Laboratory Diagnostic of Acute Kidney Injury and Its Progression: Risk of Underdiagnosis in Female and Elderly Patients
Abstract
1. Introduction
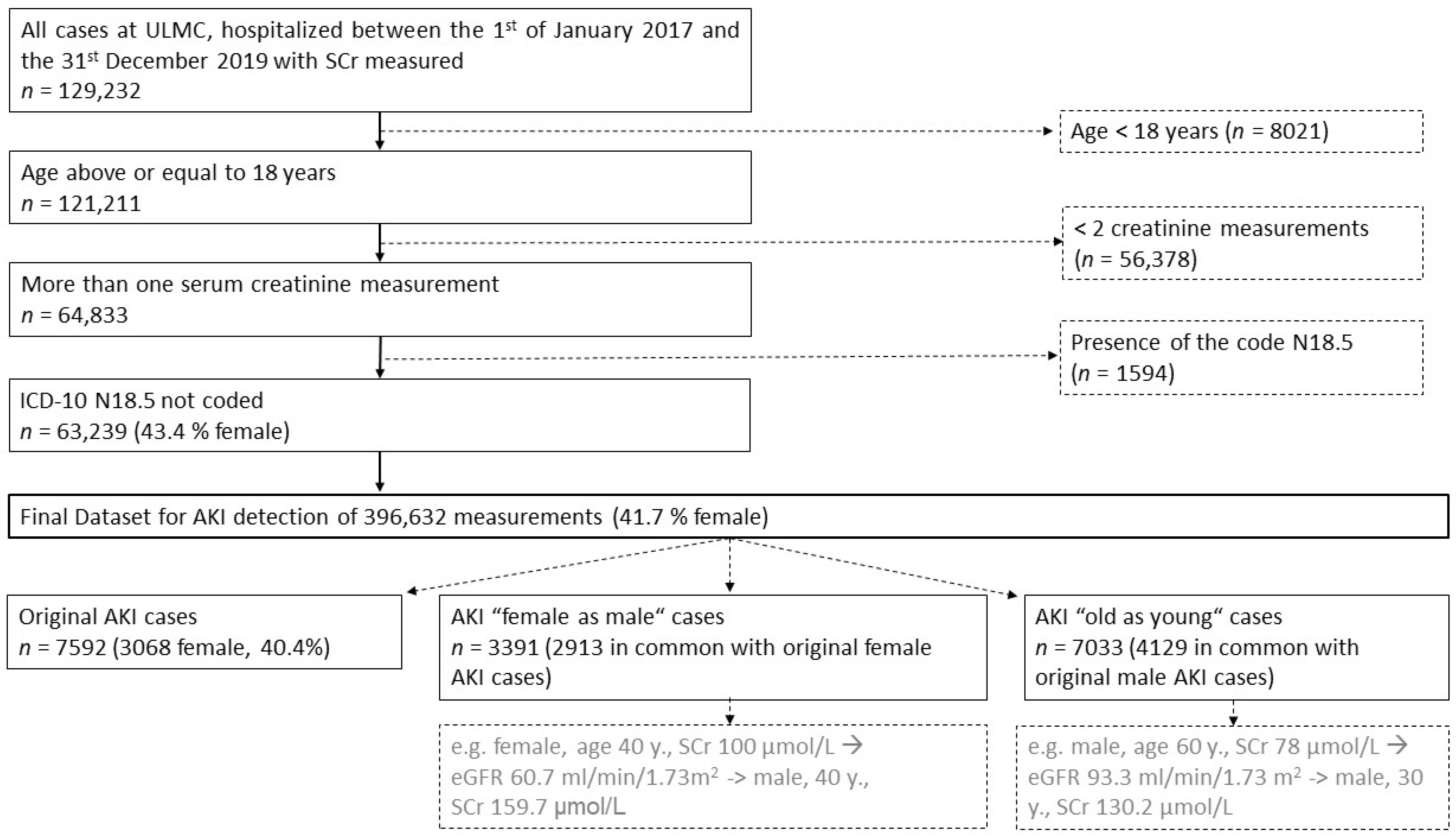
2. Materials and Methods
3. Results
3.1. Study Cohort Characteristics of Females (♀) and Males (♂) Regarding Non-Progressive and Progressive AKI
3.2. Adding Age to AKI Detection
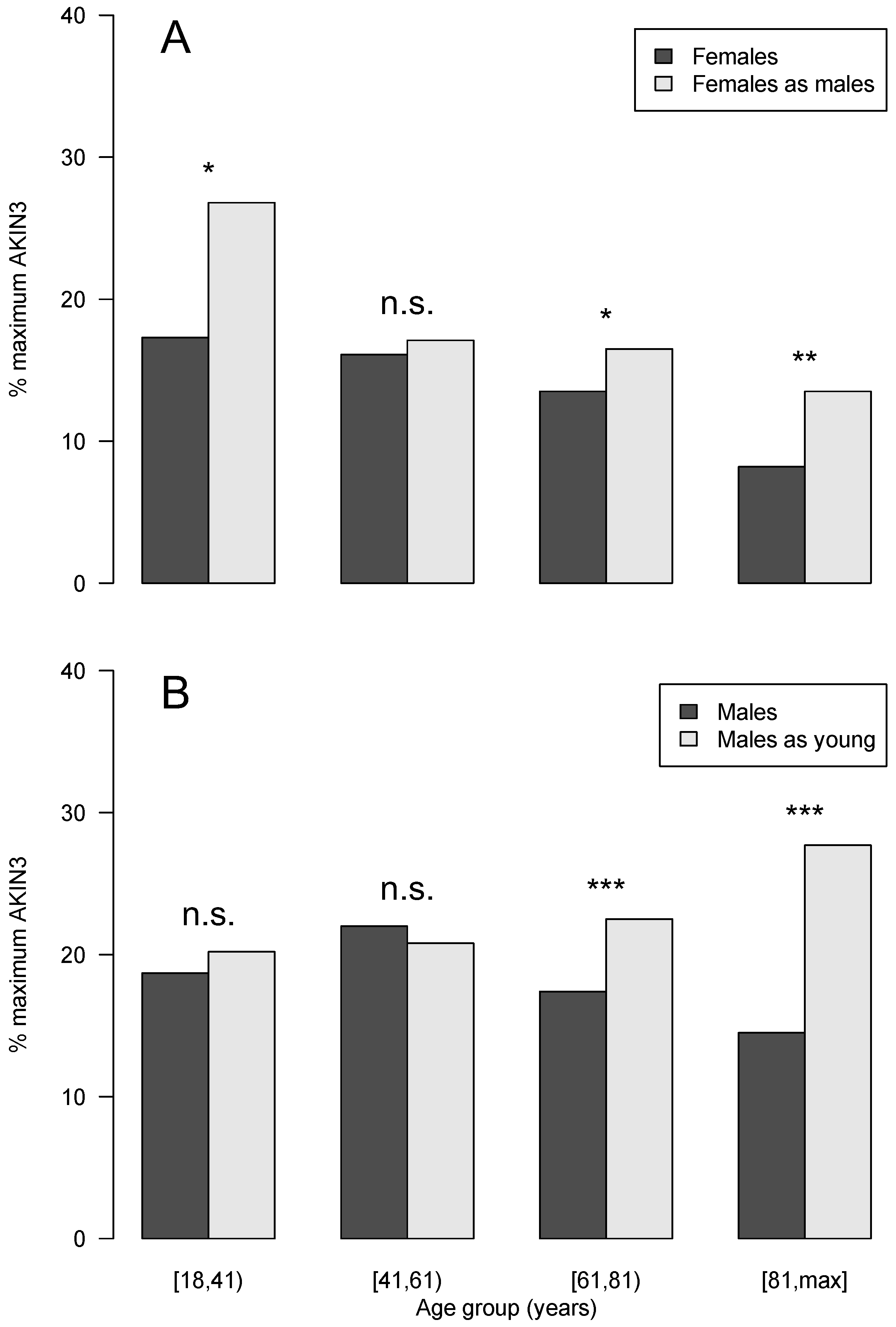
3.3. Impact of SCr Recalculation
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Khadzhynov, D.; Schmidt, D.; Hardt, J.; Rauch, G.; Gocke, P.; Eckardt, K.-U.; Schmidt-Ott, K.M. The Incidence of Acute Kidney Injury and Associated Hospital Mortality: A Retrospective Cohort Study of Over 100 000 Patients at Berlin‘s Charité Hospital. Dtsch. Ärzteblatt Int. 2019, 116, 397. [Google Scholar] [CrossRef]
- Zhao, Y.; Zheng, X.; Wang, J.; Xu, D.; Li, S.; Lv, J.; Yang, L. Effect of clinical decision support systems on clinical outcome for acute kidney injury: A systematic review and meta-analysis. BMC Nephrol. 2021, 22, 271. [Google Scholar] [CrossRef]
- Kister, T.S.; Remmler, J.; Schmidt, M.; Federbusch, M.; Eckelt, F.; Isermann, B.; Richter, H.; Wehner, M.; Krause, U.; Halbritter, J.; et al. Acute kidney injury and its progression in hospitalized patients—Results from a retrospective multicentre cohort study with a digital decision support system. PLoS ONE 2021, 16, e0254608. [Google Scholar] [CrossRef]
- Bedford, M.; Stevens, P.E.; Wheeler, T.W.; Farmer, C.K. What is the real impact of acute kidney injury? BMC Nephrol. 2014, 15, 95. [Google Scholar] [CrossRef] [PubMed]
- Bihorac, A.; Yavas, S.; Subbiah, S.; Hobson, C.E.; Schold, J.D.; Gabrielli, A.; Layon, A.J.; Segal, M.S. Long-Term Risk of Mortality and Acute Kidney Injury During Hospitalization After Major Surgery. Ann. Surg. 2009, 249, 851–858. [Google Scholar] [CrossRef] [PubMed]
- Eckelt, F.; Remmler, J.; Kister, T.; Wernsdorfer, M.; Richter, H.; Federbusch, M.; Adler, M.; Kehrer, A.; Voigt, M.; Cundius, C.; et al. Verbesserte Patientensicherheit durch „clinical decision support systems“ in der Labormedizin. Der Internist 2020, 61, 452–459. [Google Scholar] [CrossRef]
- Menon, S.; Tarrago, R.; Carlin, K.; Wu, H.; Yonekawa, K. Impact of integrated clinical decision support systems in the management of pediatric acute kidney injury: A pilot study. Pediatr. Res. 2020, 89, 1164–1170. [Google Scholar] [CrossRef]
- Selby, N.M. Electronic alerts for acute kidney injury. Curr. Opin. Nephrol. Hypertens. 2013, 22, 637–642. [Google Scholar] [CrossRef]
- Haase, M.; Kribben, A.; Zidek, W.; Floege, J.; Albert, C.; Isermann, B.; Robra, B.-P.; Haase-Fielitz, A. Electronic alerts for acute kidney injury: A systematic review. Dtsch. Ärzteblatt Int. 2017, 114, 1. [Google Scholar]
- KDIGO. Clinical Practice Guideline for Acute Kidney Injury. Kidney Int. 2012, 2, 124–138. [Google Scholar]
- Swedko, P.J.; Clark, H.D.; Paramsothy, K.; Akbari, A. Serum Creatinine Is an Inadequate Screening Test for Renal Failure in Elderly Patients. Arch. Intern. Med. 2003, 163, 356–360. [Google Scholar] [CrossRef]
- Yoo, J.-J.; Kim, S.G.; Kim, Y.D.; Lee, B.; Lee, M.H.; Jeong, S.W.; Jang, J.Y.; Lee, S.H.; Kim, H.S.; Cheon, G.J. Estimation of renal function in patients with liver cirrhosis: Impact of muscle mass and sex. J. Hepatol. 2019, 70, 847–854. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems: 10th Revision, 2nd ed.; World Health Organization: Geneva, Switzerland, 2004.
- SAP Software Solutions. Available online: https://www.sap.com/index.html (accessed on 3 May 2022).
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2019; Available online: https://www.R-project.org/ (accessed on 3 May 2022).
- Wickham, H. Reshaping Data with the reshape Package. J. Stat. Softw. 2007, 21, 1–20. [Google Scholar] [CrossRef]
- Levey, A.S.; Stevens, L.A.; Schmid, C.H.; Zhang, Y.L.; Castro, A.F., 3rd; Feldman, H.I.; Kusek, J.W.; Eggers, P.; Van Lente, F.; Greene, T.; et al. A New Equation to Estimate Glomerular Filtration Rate. Ann. Intern. Med. 2009, 150, 604–612. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.E.; Muntner, P.; Chertow, G.M.; Warnock, D.G. Acute Kidney Injury and Mortality in Hospitalized Patients. Am. J. Nephrol. 2012, 35, 349–355. [Google Scholar] [CrossRef]
- Susantitaphong, P.; Cruz, D.N.; Cerda, J.; Abulfaraj, M.; Alqahtani, F.; Koulouridis, I.; Jaber, B.L. World Incidence of AKI: A Meta-Analysis. Clin. J. Am. Soc. Nephrol. 2013, 8, 1482–1493. [Google Scholar] [CrossRef]
- Chertow, G.M.; Burdick, E.; Honour, M.; Bonventre, J.V.; Bates, D.W. Acute Kidney Injury, Mortality, Length of Stay, and Costs in Hospitalized Patients. JASN 2005, 16, 3365–3370. [Google Scholar] [CrossRef]
- Cockcroft, D.W.; Gault, H. Prediction of Creatinine Clearance from Serum Creatinine. Nephron 1976, 16, 31–41. [Google Scholar] [CrossRef]
- Perrone, R.D.; Madias, N.E.; Levey, A.S. Serum creatinine as an index of renal function: New insights into old concepts. Clin. Chem. 1992, 38, 1933–1953. [Google Scholar] [CrossRef]
- Inker, L.; Levey, A. Frequently Asked Questions about GFR Estimates. 2014. Available online: https://www.kidney.org/sites/default/files/docs/12-10-4004_abe_faqs_aboutgfrrev1b_singleb.pdf (accessed on 25 May 2021).
- Oksuzyan, A.; Juel, K.; Vaupel, J.; Christensen, K. Men: Good health and high mortality. Sex differences in health and aging. Aging Clin. Exp. Res. 2008, 20, 91–102. [Google Scholar] [CrossRef]
- Official Website of the Free State of Saxony (Germany)—Demographics. Available online: https://www.demografie.sachsen.de/Geschlechterstruktur.pdf (accessed on 25 May 2021).
- Christensen, K.; Doblhammer, G.; Rau, R.; Vaupel, J.W. Ageing populations: The challenges ahead. Lancet 2009, 374, 1196–1208. [Google Scholar] [CrossRef] [PubMed]
- Tomlinson, B.; Walton, J.; Rebeiz, J. The effects of ageing and of cachexia upon skeletal muscle A histopathological study. J. Neurol. Sci. 1969, 9, 321–346. [Google Scholar] [CrossRef] [PubMed]
- Sakuma, K.; Yamaguchi, A. Sarcopenia and Age-Related Endocrine Function. Int. J. Endocrinol. 2012, 2012, 127362. [Google Scholar] [CrossRef] [PubMed]
- Cobo, G.; Hecking, M.; Port, F.K.; Exner, I.; Lindholm, B.; Stenvinkel, P.; Carrero, J.J. Sex and gender differences in chronic kidney disease: Progression to end-stage renal disease and haemodialysis. Clin. Sci. 2016, 130, 1147–1163. [Google Scholar] [CrossRef]
- El-Khoury, J.M.; Hoenig, M.P.; Jones, G.R.D.; Lamb, E.J.; Parikh, C.R.; Tolan, N.V.; Wilson, F.P. AACC Guidance Document on Laboratory Investigation of Acute Kidney Injury. J. Appl. Lab. Med. 2021, 6, 1316–1337. [Google Scholar] [CrossRef]
- Villa, P.; Jiménez, M.; Soriano, M.-C.; Manzanares, J.; Casasnovas, P. Serum cystatin C concentration as a marker of acute renal dysfunction in critically ill patients. Crit. Care 2005, 9, R139–R143. [Google Scholar] [CrossRef]
- Coca, S.G.; Singanamala, S.; Parikh, C.R. Chronic kidney disease after acute kidney injury: A systematic review and meta-analysis. Kidney Int. 2012, 81, 442–448. [Google Scholar] [CrossRef]
- Kurzhagen, J.T.; Dellepiane, S.; Cantaluppi, V.; Rabb, H. AKI: An increasingly recognized risk factor for CKD development and progression. J. Nephrol. 2020, 33, 1171–1187. [Google Scholar] [CrossRef]
- Brar, A.; Markell, M. Impact of gender and gender disparities in patients with kidney disease. Curr. Opin. Nephrol. Hypertens. 2019, 28, 178–182. [Google Scholar] [CrossRef]
- Carrero, J.J.; Hecking, M.; Chesnaye, N.C.; Jager, K.J. Sex and gender disparities in the epidemiology and outcomes of chronic kidney disease. Nat. Rev. Nephrol. 2018, 14, 151–164. [Google Scholar] [CrossRef]
- James, M.T.; Pannu, N.; Hemmelgarn, B.R.; Austin, P.C.; Tan, Z.; McArthur, E.; Manns, B.J.; Tonelli, M.; Wald, R.; Quinn, R.R.; et al. Derivation and External Validation of Prediction Models for Advanced Chronic Kidney Disease Following Acute Kidney Injury. JAMA 2017, 318, 1787–1797. [Google Scholar] [CrossRef] [PubMed]
- Albertus, P.; Morgenstern, H.; Robinson, B.; Saran, R. Risk of ESRD in the United States. Am. J. Kidney Dis. 2016, 68, 862–872. [Google Scholar] [CrossRef] [PubMed]
| Stage | Serum Creatinine | Urine Output |
|---|---|---|
| AKIN1 | 1.5–1.9 times baseline, OR ≥0.3 mg/dL (≥26.5 μmol/L) increase | <0.5 mL/kg/h for 6–12 h |
| AKIN2 | 2.0–2.9 times baseline | <0.5 mL/kg/h for ≥12 h |
| AKIN3 | 3.0 times baseline, OR increase in serum creatinine to ≥4.0 mg/dL (≥353.6 μmol/L), OR initiation of renal replacement therapy, OR in patients <18 years, decrease in eGFR to <35 mL/min per 1.73 m2 | <0.3 mL/kg/h for ≥24 h, OR anuria for ≥12 h |
| All AKI Cases, n = 7592 | Progressive AKI Cases, n = 1458 | |||||
|---|---|---|---|---|---|---|
| Female | Male | p-Value | Female Progression | Male Progression | p-Value | |
| Incidence proportion, n, % | 3068, 40.4 | 4524, 59.6 | 554, 18.1 | 904, 20.0 | 0.039 | |
| Basic patient characteristics | ||||||
| Age (years) | 72.0 [60.4–80.9] | 67.7 [57.9–77.8] | <0.001 | 70.7 [59.0–79.5] | 66.0 [57.0–75.9] | <0.001 |
| Total length of hospitalization (days) | 16.2 [9.1–29.6] | 17.6 [9.1–31.6] | 0.038 | 24.7 [14.2–43.1] | 26.3 [14.9–42.6] | 0.491 |
| First eGFR (mL/min/1.73 m²) | 59.9 [36–85.4] | 63.4 [39.3–88.2] | <0.001 | 58.0 [36.1–85.1] | 61.9 [37.7–88.1] | 0.177 |
| Last eGFR (mL/min/1.73 m²) | 53.2 [32.7–82.2] | 55.9 [35.7–84.5] | <0.001 | 44.9 [25.2–74.4] | 46.0 [25.7–75.7] | 0.502 |
| Time to first AKI during hospitalization (days) | 4.7 [1.9–10.8] | 4.5 [1.8–9.9] | 0.073 | 4.9 [1.9–11.9] | 4.5 [1.8–9.4] | 0.037 |
| In-hospital mortality | 22.0 | 23.0 | 0.310 | 45.5 | 45.0 | 0.905 |
| Comorbidities | ||||||
| I10.—Hypertension | 48.2 | 46.4 | 0.129 | 47.7 | 46.9 | 0.822 |
| E11.—Diabetes mellitus | 31.8 | 34.4 | 0.022 | 31.4 | 35.2 | 0.156 |
| E86.—Exsiccosis | 4.8 | 4.4 | 0.466 | 6.0 | 3.4 | 0.031 |
| R57.—Shock | 17.2 | 22.3 | <0.001 | 37.9 | 44.3 | 0.020 |
| I25.—Coronary heart disease | 13.5 | 23.4 | <0.001 | 11.2 | 23.5 | <0.001 |
| I21.—Myocardial infarction | 3.2 | 4.9 | 0.001 | 3.4 | 6.2 | 0.028 |
| I50.—Cardiac insufficiency | 28.9 | 28.0 | 0.435 | 33.9 | 34.6 | 0.832 |
| A41.—Sepsis | 19.9 | 24.9 | <0.001 | 38.8 | 41.9 | 0.263 |
| K74.—Liver cirrhosis | 5.1 | 5.1 | 0.993 | 8.7 | 9.0 | 0.865 |
| Age Group | All AKI (n = 7592, 12.0%) | Female (n = 3068, 11.2%) | Male (n = 4524, 12.6%) |
|---|---|---|---|
| [18–41) * | 470, 5.2% | 202, 4.7% | 268, 5.8% |
| [41–61) *** | 1765, 10.4% | 596, 9.0% | 1169, 11.2% |
| [61–81) n.s. | 3902, 14.0% | 1519, 13.5% | 2383, 14.3% |
| [81–max] *** | 1455, 15.6% | 751, 14.3% | 704, 17.4% |
| Age Group | Total Progressive AKI (n = 1458, 19.2%) * | Female (n = 554, 7.3%) | Male (n = 904, 11.9%) |
|---|---|---|---|
| [18–41) n.s | 85, 18.1% | 36, 17.8% | 49, 18.3% |
| [41–61) n.s | 389, 22.0% | 124, 20.8% | 265, 22.7% |
| [61–81) n.s | 748, 19.2% | 281, 18.5% | 467, 19.6% |
| [81–max] n.s | 236, 16.2% | 113, 15.0% | 123, 17.5% |
| Criteria Feature | AKIN1, n, % | AKIN3, n, % | ||||
|---|---|---|---|---|---|---|
| Female (n = 6011) | Male (n = 9365) | p-Value | Female (n = 1032) | Male (n = 1984) | p-Value | |
| Absolute | 1214, 20.2% | 2750, 29.4% | <0.001 | 138, 13.4% | 302, 15.2% | 0.190 |
| Both | 1450, 24.1% | 2510, 26.8% | <0.001 | 294, 28.5% | 936, 47.2% | <0.001 |
| Relative | 3347, 55.7% | 4105, 43.8% | <0.001 | 600, 58.1% | 746, 37.6% | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kister, T.S.; Schmidt, M.; Heuft, L.; Federbusch, M.; Haase, M.; Kaiser, T. Laboratory Diagnostic of Acute Kidney Injury and Its Progression: Risk of Underdiagnosis in Female and Elderly Patients. J. Clin. Med. 2023, 12, 1092. https://doi.org/10.3390/jcm12031092
Kister TS, Schmidt M, Heuft L, Federbusch M, Haase M, Kaiser T. Laboratory Diagnostic of Acute Kidney Injury and Its Progression: Risk of Underdiagnosis in Female and Elderly Patients. Journal of Clinical Medicine. 2023; 12(3):1092. https://doi.org/10.3390/jcm12031092
Chicago/Turabian StyleKister, Thea Sophie, Maria Schmidt, Lara Heuft, Martin Federbusch, Michael Haase, and Thorsten Kaiser. 2023. "Laboratory Diagnostic of Acute Kidney Injury and Its Progression: Risk of Underdiagnosis in Female and Elderly Patients" Journal of Clinical Medicine 12, no. 3: 1092. https://doi.org/10.3390/jcm12031092
APA StyleKister, T. S., Schmidt, M., Heuft, L., Federbusch, M., Haase, M., & Kaiser, T. (2023). Laboratory Diagnostic of Acute Kidney Injury and Its Progression: Risk of Underdiagnosis in Female and Elderly Patients. Journal of Clinical Medicine, 12(3), 1092. https://doi.org/10.3390/jcm12031092








