Being Underweight Is Associated with Increased Risk of Sudden Cardiac Death in People with Diabetes Mellitus
Abstract
:1. Introduction
2. Patients and Methods
2.1. Nationwide Database
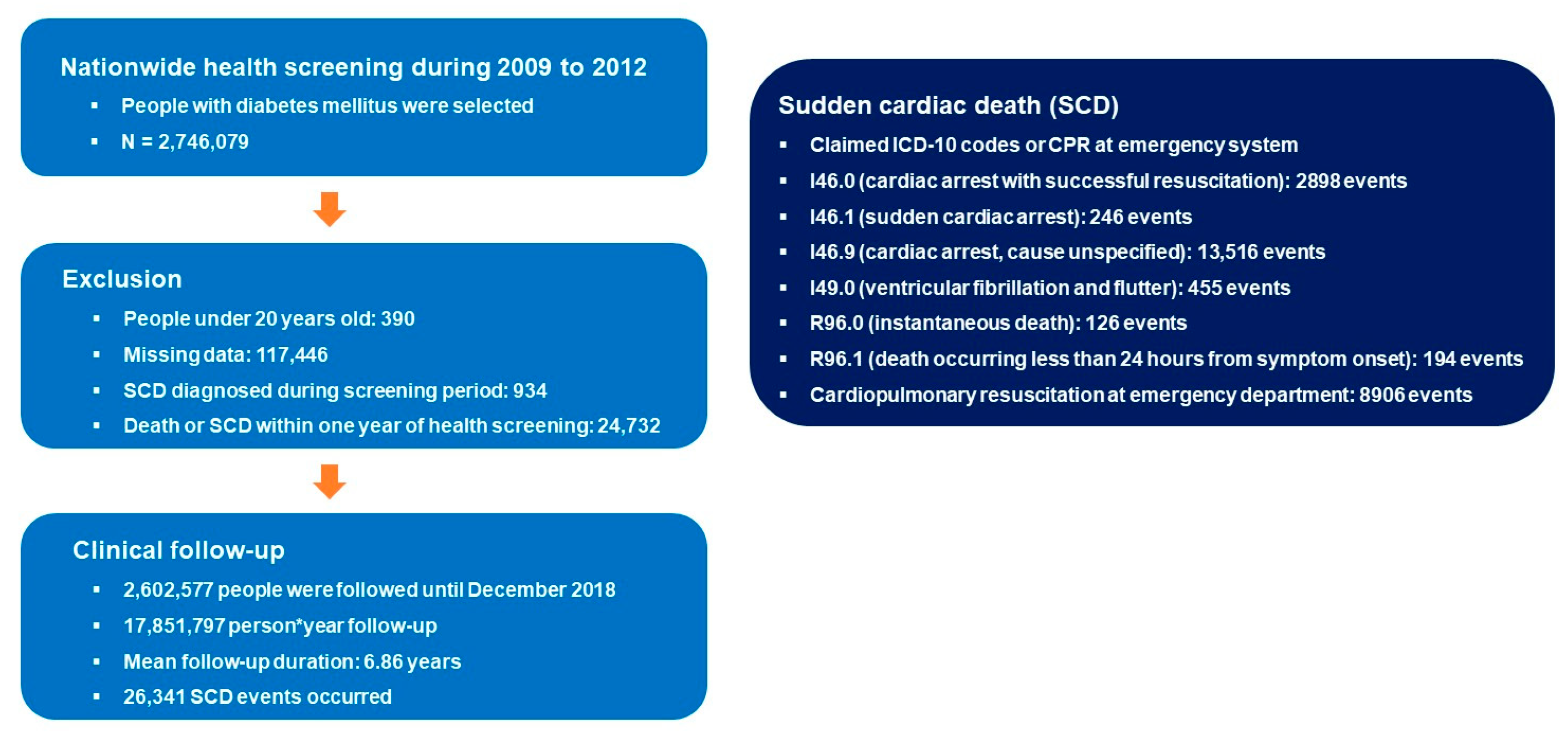
2.2. Participants
2.3. Sudden Cardiac Death
2.4. Definitions
2.5. Statistical Analysis
2.6. Data Availability Statement
3. Results
3.1. Study Population
3.2. Risk of Sudden Cardiac Death
3.3. Subgroup Analysis
4. Discussion
4.1. Obesity and SCD
4.2. Being Underweight and SCD
4.3. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Ackerman, M.; Atkins, D.L.; Triedman, J.K. Sudden Cardiac Death in the Young. Circulation 2016, 133, 1006–1026. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hemingway, H.; Malik, M.; Marmot, M. Social and psychosocial influences on sudden cardiac death, ventricular arrhythmia and cardiac autonomic function. Eur. Heart J. 2001, 22, 1082–1101. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hasselqvist-Ax, I.; Riva, G.; Herlitz, J.; Rosenqvist, M.; Hollenberg, J.; Nordberg, P.; Ringh, M.; Jonsson, M.; Axelsson, C.; Lindqvist, J.; et al. Early cardiopulmonary resuscitation in out-of-hospital cardiac arrest. N. Engl. J. Med. 2015, 372, 2307–2315. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eisenberg, M.S.; Hallstrom, A.; Bergner, L. Long-term survival after out-of-hospital cardiac arrest. N. Engl. J. Med. 1982, 306, 1340–1343. [Google Scholar] [CrossRef]
- Blewer, A.L.; Ho, A.F.W.; Shahidah, N.; White, A.E.; Pek, P.P.; Ng, Y.Y.; Mao, D.R.; Tiah, L.; Chia, M.Y.; Leong, B.S.; et al. Impact of bystander-focused public health interventions on cardiopulmonary resuscitation and survival: A cohort study. Lancet Public Health 2020, 5, e428–e436. [Google Scholar] [CrossRef]
- Berdowski, J.; Berg, R.A.; Tijssen, J.G.; Koster, R.W. Global incidences of out-of-hospital cardiac arrest and survival rates: Systematic review of 67 prospective studies. Resuscitation 2010, 81, 1479–1487. [Google Scholar] [CrossRef]
- El-Battrawy, I.; Pilsinger, C.; Liebe, V.; Lang, S.; Kuschyk, J.; Zhou, X.; Borggrefe, M.; Röger, S.; Akin, I. Impact of sacubitril/valsartan on the long-term incidence of ventricular arrhythmias in chronic heart failure patients. J. Clin. Med. 2019, 8, 1582. [Google Scholar] [CrossRef] [Green Version]
- Myat, A.; Song, K.-J.; Rea, T. Out-of-hospital cardiac arrest: Current concepts. Lancet 2018, 391, 970–979. [Google Scholar] [CrossRef]
- Pannone, L.; Falasconi, G.; Cianfanelli, L.; Baldetti, L.; Moroni, F.; Spoladore, R.; Vergara, P. Sudden cardiac death in patients with heart disease and preserved systolic function: Current options for risk stratification. J. Clin. Med. 2021, 10, 1823. [Google Scholar] [CrossRef]
- Jouven, X.; Lemaître, R.N.; Rea, T.D.; Sotoodehnia, N.; Empana, J.-P.; Siscovick, D.S. Diabetes, glucose level, and risk of sudden cardiac death. Eur. Heart J. 2005, 26, 2142–2147. [Google Scholar] [CrossRef]
- Lynge, T.H.; Svane, J.; Pedersen-Bjergaard, U.; Gislason, G.; Torp-Pedersen, C.; Banner, J.; Risgaard, B.; Winkel, B.G.; Tfelt-Hansen, J. Sudden cardiac death among persons with diabetes aged 1–49 years: A 10-year nationwide study of 14294 deaths in Denmark. Eur. Heart J. 2020, 41, 2699–2706. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, Y.G.; Roh, S.Y.; Han, K.-D.; Jeong, J.H.; Choi, Y.Y.; Min, K.; Shim, J.; Choi, J.-I.; Kim, Y.-H. Hypertension and diabetes including their earlier stage are associated with increased risk of sudden cardiac arrest. Sci. Rep. 2022, 12, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Calle, E.E.; Thun, M.J.; Petrelli, J.M.; Rodriguez, C.; Heath, C.W., Jr. Body-mass index and mortality in a prospective cohort of U.S. adults. N. Engl. J. Med. 1999, 341, 1097–1105. [Google Scholar] [CrossRef] [PubMed]
- Jee, S.H.; Sull, J.W.; Park, J.; Lee, S.-Y.; Ohrr, H.; Guallar, E.; Samet, J.M. Body-mass index and mortality in Korean men and women. N. Engl. J. Med. 2006, 355, 779–787. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Twig, G.; Yaniv, G.; Levine, H.; Leiba, A.; Goldberger, N.; Derazne, E.; Ben-Ami Shor, D.; Tzur, D.; Afek, A.; Shamiss, A. Body-mass index in 2.3 million adolescents and cardiovascular death in adulthood. N. Engl. J. Med. 2016, 374, 2430–2440. [Google Scholar] [CrossRef]
- Rozen, G.; Elbaz-Greener, G.; Margolis, G.; Marai, I.; Heist, E.K.; Ruskin, J.N.; Carasso, S.; Roguin, A.; Birati, E.Y.; Amir, O. The Obesity Paradox in Real-World Nation-Wide Cohort of Patients Admitted for a Stroke in the US. J. Clin. Med. 2022, 11, 1678. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.-W.; Li, Y.-H.; Hsieh, C.-H.; Liu, P.-Y.; Lin, G.-M. Association of body mass index with all-cause mortality in patients with diabetes: A systemic review and meta-analysis. Cardiovasc. Diagn. Ther. 2016, 6, 109. [Google Scholar] [CrossRef] [Green Version]
- Sairenchi, T.; Iso, H.; Irie, F.; Fukasawa, N.; Ota, H.; Muto, T. Underweight as a predictor of diabetes in older adults: A large cohort study. Diabetes Care 2008, 31, 583–584. [Google Scholar] [CrossRef] [Green Version]
- Kim, Y.G.; Han, K.D.; Choi, J.I.; Choi, Y.Y.; Choi, H.Y.; Boo, K.Y.; Kim, D.Y.; Lee, K.N.; Shim, J.; Kim, J.S.; et al. Non-genetic risk factors for atrial fibrillation are equally important in both young and old age: A nationwide population-based study. Eur. J. Prev. Cardiol. 2021, 28, 666–676. [Google Scholar] [CrossRef]
- Kim, Y.G.; Han, K.D.; Kim, D.Y.; Choi, Y.Y.; Choi, H.Y.; Roh, S.Y.; Shim, J.; Kim, J.S.; Choi, J.I.; Kim, Y.H. Different Influence of Blood Pressure on New-Onset Atrial Fibrillation in Pre- and Postmenopausal Women: A Nationwide Population-Based Study. Hypertension 2021, 77, 1500–1509. [Google Scholar] [CrossRef]
- Kim, Y.G.; Han, K.D.; Choi, J.I.; Choi, Y.Y.; Choi, H.Y.; Shim, J.; Kim, Y.H. Premature ventricular contraction is associated with increased risk of atrial fibrillation: A nationwide population-based study. Sci. Rep. 2021, 11, 1601. [Google Scholar] [CrossRef]
- Roh, S.Y.; Choi, J.I.; Kim, M.S.; Cho, E.Y.; Kim, Y.G.; Lee, K.N.; Shim, J.; Kim, J.S.; Kim, Y.H. Incidence and etiology of sudden cardiac arrest in Koreans: A cohort from the national health insurance service database. PLoS ONE 2020, 15, e0242799. [Google Scholar] [CrossRef]
- Kim, Y.G.; Han, K.D.; Choi, J.I.; Yung Boo, K.; Kim, D.Y.; Oh, S.K.; Lee, K.N.; Shim, J.; Kim, J.S.; Kim, Y.H. Impact of the Duration and Degree of Hypertension and Body Weight on New-Onset Atrial Fibrillation: A Nationwide Population-Based Study. Hypertension 2019, 74, e45–e51. [Google Scholar] [CrossRef]
- Kim, Y.G.; Oh, S.K.; Choi, H.Y.; Choi, J.I. Inherited arrhythmia syndrome predisposing to sudden cardiac death. Korean J. Intern. Med. 2021, 36, 527–538. [Google Scholar] [CrossRef]
- Kim, Y.G.; Han, K.; Jeong, J.H.; Roh, S.Y.; Choi, Y.Y.; Min, K.; Shim, J.; Choi, J.I.; Kim, Y.H. Metabolic Syndrome, Gamma-Glutamyl Transferase, and Risk of Sudden Cardiac Death. J. Clin. Med. 2022, 11, 1781. [Google Scholar] [CrossRef]
- Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N. Engl. J. Med. 2002, 346, 549–556. [CrossRef]
- de Vreede-Swagemakers, J.J.; Gorgels, A.P.; Dubois-Arbouw, W.I.; van Ree, J.W.; Daemen, M.J.; Houben, L.G.; Wellens, H.J. Out-of-hospital cardiac arrest in the 1990’s: A population-based study in the Maastricht area on incidence, characteristics and survival. J. Am. Coll. Cardiol. 1997, 30, 1500–1505. [Google Scholar] [CrossRef] [Green Version]
- Culley, L.L.; Rea, T.D.; Murray, J.A.; Welles, B.; Fahrenbruch, C.E.; Olsufka, M.; Eisenberg, M.S.; Copass, M.K. Public access defibrillation in out-of-hospital cardiac arrest: A community-based study. Circulation 2004, 109, 1859–1863. [Google Scholar] [CrossRef] [Green Version]
- Kim, C.; Fahrenbruch, C.E.; Cobb, L.A.; Eisenberg, M.S. Out-of-hospital cardiac arrest in men and women. Circulation 2001, 104, 2699–2703. [Google Scholar] [CrossRef] [Green Version]
- Haffner, S.; Taegtmeyer, H. Epidemic obesity and the metabolic syndrome. Circulation 2003, 108, 1541–1545. [Google Scholar] [CrossRef]
- Empana, J.P.; Duciemetiere, P.; Balkau, B.; Jouven, X. Contribution of the metabolic syndrome to sudden death risk in asymptomatic men: The Paris Prospective Study I. Eur. Heart J. 2007, 28, 1149–1154. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hess, P.L.; Al-Khalidi, H.R.; Friedman, D.J.; Mulder, H.; Kucharska-Newton, A.; Rosamond, W.R.; Lopes, R.D.; Gersh, B.J.; Mark, D.B.; Curtis, L.H.; et al. The Metabolic Syndrome and Risk of Sudden Cardiac Death: The Atherosclerosis Risk in Communities Study. J. Am. Heart Assoc. 2017, 6, e006103. [Google Scholar] [CrossRef] [PubMed]
- Perry, J.R.; Voight, B.F.; Yengo, L.; Amin, N.; Dupuis, J.; Ganser, M.; Grallert, H.; Navarro, P.; Li, M.; Qi, L. Stratifying type 2 diabetes cases by BMI identifies genetic risk variants in LAMA1 and enrichment for risk variants in lean compared to obese cases. PLoS Genet. 2012, 8, e1002741. [Google Scholar] [CrossRef]


| Body-Mass Index (BMI) | ||||||||
|---|---|---|---|---|---|---|---|---|
| BMI < 18.5 | 18.5 ≤ BMI < 23 | 23 ≤ BMI < 25 | 25 ≤ BMI < 30 | BMI ≥ 30 | p Value | BMI ≥ 18.5 | p Value (<18.5 vs. ≥18.5) | |
| n | 41,598 | 648,206 | 645,444 | 1,066,439 | 200,890 | 2,560,979 | ||
| Age, years | 59.7 ± 16.1 | 58.6 ± 12.9 | 58.3 ± 11.7 | 57.0 ± 11.8 | 53.0 ± 13.0 | <0.001 | 57.4 ± 12.3 | <0.001 |
| Age groups | <0.001 | <0.001 | ||||||
| <40 | 5172 (12.4%) | 47,580 (7.3%) | 35,757 (5.5%) | 76,107 (7.1%) | 32,037 (16.0%) | 191,481 (7.5%) | ||
| 40 ≤ age < 65 | 18,663 (44.9%) | 378,603 (58.4%) | 406,130 (62.9%) | 690,485 (64.8%) | 126,645 (63.0%) | 1,601,863 (62.6%) | ||
| ≥65 | 17,763 (42.7%) | 222,023 (34.3%) | 203,557 (31.5%) | 299,847 (28.1%) | 42,208 (21.0%) | 767,635 (30.0%) | ||
| Sex | <0.001 | <0.001 | ||||||
| Male | 23,765 (57.1%) | 382,404 (59.0%) | 403,135 (62.5%) | 653,020 (61.2%) | 99,974 (49.8%) | 1,538,533 (60.1%) | ||
| Female | 17,833 (42.9%) | 265,802 (41.0%) | 242,309 (37.5%) | 413,419 (38.8%) | 100,916 (50.2%) | 1,022,446 (39.9%) | ||
| Income (lowest quartile) | 10,377 (25.0%) | 142,184 (21.9%) | 132,778 (20.6%) | 217,179 (20.4%) | 43,936 (21.9%) | <0.001 | 536,077 (20.9%) | <0.001 |
| Smoking | <0.001 | <0.001 | ||||||
| Non | 22,586 (54.3%) | 360,640 (55.6%) | 352,969 (54.7%) | 589,443 (55.3%) | 122,660 (61.1%) | 1,425,712 (55.7%) | ||
| Ex | 4865 (11.7%) | 103,684 (16.0%) | 126,303 (19.6%) | 215,921 (20.3%) | 30,257 (15.1%) | 476,165 (18.6%) | ||
| Current | 14,147 (34.0%) | 183,882 (28.4%) | 166,172 (25.8%) | 261,075 (24.5%) | 47,973 (23.9%) | 659,102 (25.7%) | ||
| Drinking | <0.001 | <0.001 | ||||||
| Non | 26,504 (63.7%) | 383,752 (59.2%) | 365,192 (56.6%) | 595,316 (55.8%) | 120,730 (60.1%) | 1,464,990 (57.2%) | ||
| Mild | 11,386 (27.4%) | 205,557 (31.7%) | 217,857 (33.8%) | 357,372 (33.5%) | 59,925 (29.8%) | 840,711 (32.8%) | ||
| Heavy | 3708 (8.9%) | 58,897 (9.1%) | 62,395 (9.7%) | 113,751 (10.7%) | 20,235 (10.1%) | 255,278 (10.0%) | ||
| Regular exercise | 6065 (14.6%) | 134,781 (20.8%) | 142,392 (22.1%) | 219,627 (20.6%) | 33,160 (16.5%) | <0.001 | 529,960 (20.7%) | <0.001 |
| Hypertension | 15,965 (38.4%) | 301,988 (46.6%) | 352,520 (54.6%) | 664,559 (62.3%) | 143,015 (71.2%) | <0.001 | 1,462,082 (57.1%) | <0.001 |
| Dyslipidemia | 9092 (21.9%) | 223,499 (34.5%) | 268,170 (41.6%) | 490,648 (46.0%) | 99,901 (49.7%) | <0.001 | 1,082,218 (42.3%) | <0.001 |
| DM duration, ≥5 years | 12,806 (30.8%) | 227,952 (35.2%) | 214,249 (33.2%) | 307,177 (28.8%) | 47,331 (23.6%) | <0.001 | 796,709 (31.1%) | 0.156 |
| On Insulin | 5983 (14.4%) | 68,633 (10.6%) | 55,762 (8.6%) | 82,799 (7.8%) | 14,764 (7.4%) | <0.001 | 221,958 (8.7%) | <0.001 |
| Oran antidiabetics, ≥3 | 6144 (14.8%) | 102,545 (15.8%) | 95,288 (14.8%) | 146,073 (13.7%) | 27,257 (13.6%) | <0.001 | 371,163 (14.5%) | 0.112 |
| BMI (kg/m2) | 17.4 ± 0.9 | 21.4 ± 1.2 | 24.0 ± 0.6 | 26.9 ± 1.3 | 32.3 ± 2.4 | <0.001 | 25.2 ± 3.3 | <0.001 |
| Waist circumference (cm) | 70.0 ± 6.4 | 78.0 ± 6.0 | 83.5 ± 5.4 | 89.2 ± 6.1 | 98.7 ± 7.8 | <0.001 | 85.7 ± 8.5 | <0.001 |
| Systolic BP (mmHg) | 122.3 ± 17.4 | 126.1 ± 16.1 | 128.5 ± 15.5 | 130.6 ± 15.3 | 133.7 ± 15.9 | <0.001 | 129.2 ± 15.8 | <0.001 |
| Diastolic BP (mmHg) | 75.3 ± 10.8 | 76.9 ± 10.2 | 78.5 ± 10.0 | 80.2 ± 10.1 | 82.6 ± 10.7 | <0.001 | 79.1 ± 10.3 | <0.001 |
| Fasting glucose (mg/dL) | 152.1 ± 65.5 | 146.4 ± 51.7 | 144.3 ± 46.4 | 143.6 ± 43.8 | 145.7 ± 45.2 | <0.001 | 144.7 ± 46.7 | <0.001 |
| Total cholesterol (mg/dL) | 183.0 ± 41.7 | 191.6 ± 41.9 | 196.2 ± 42.6 | 199.1 ± 43.0 | 202.6 ± 43.4 | <0.001 | 196.7 ± 42.8 | <0.001 |
| HDL (mg/dL) | 59.1 ± 28.5 | 54.6 ± 25.5 | 51.9 ± 23.5 | 50.6 ± 22.9 | 50.2 ± 22.0 | <0.001 | 51.9 ± 23.7 | <0.001 |
| LDL (mg/dL) | 101.4 ± 41.5 | 108.8 ± 40.2 | 111.4 ± 40.8 | 112.2 ± 41.6 | 114.0 ± 41.9 | <0.001 | 111.3 ± 41.1 | <0.001 |
| Triglyceride (mg/dL) | 101.5 (100.9–102.0) | 123.6 (123.5–123.8) | 144.8 (144.6–145.0) | 160.7 (160.6–160.9) | 171.4 (171.0–171.8) | <0.001 | 147.2 (147.1–147.3) | <0.001 |
| N | SCD | Follow-Up Duration (Person-Years) | Incidence | Hazard Ratio with 95% Confidence Interval | |||
|---|---|---|---|---|---|---|---|
| Non-Adjusted | Model 1 | Model 2 | |||||
| Underweight | |||||||
| No (BMI ≥ 18.5) | 2,560,979 | 25,259 | 17,604,724 | 1.43 | 1 (reference) | 1 (reference) | 1 (reference) |
| Yes (BMI < 18.5) | 41,598 | 1082 | 247,073 | 4.38 | 3.11 (2.93–3.31) | 2.56 (2.41–2.72) | 2.40 (2.26–2.56) |
| BMI value | |||||||
| BMI < 18.5 | 41,598 | 1082 | 247,073 | 4.38 | 2.29 (2.15–2.44) | 2.01 (1.94–2.20) | 2.01 (1.88–2.14) |
| 18.5 ≤ BMI < 23 | 648,206 | 8491 | 4,355,959 | 1.95 | 1 (reference) | 1 (reference) | 1 (reference) |
| 23 ≤ BMI < 25 | 645,444 | 6401 | 4,457,801 | 1.44 | 0.73 (0.71–0.76) | 0.75 (0.73–0.78) | 0.77 (0.75–0.80) |
| 25 ≤ BMI < 30 | 1,066,439 | 8844 | 7,408,578 | 1.19 | 0.61 (0.59–0.63) | 0.69 (0.67–0.71) | 0.71 (0.69–0.74) |
| BMI ≥ 30 | 200,890 | 1523 | 1,382,385 | 1.10 | 0.57 (0.54–0.60) | 0.89 (0.84–0.94) | 0.89 (0.84–0.94) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, Y.G.; Han, K.-D.; Roh, S.-Y.; Jeong, J.H.; Choi, Y.Y.; Min, K.; Shim, J.; Choi, J.-I.; Kim, Y.-H. Being Underweight Is Associated with Increased Risk of Sudden Cardiac Death in People with Diabetes Mellitus. J. Clin. Med. 2023, 12, 1045. https://doi.org/10.3390/jcm12031045
Kim YG, Han K-D, Roh S-Y, Jeong JH, Choi YY, Min K, Shim J, Choi J-I, Kim Y-H. Being Underweight Is Associated with Increased Risk of Sudden Cardiac Death in People with Diabetes Mellitus. Journal of Clinical Medicine. 2023; 12(3):1045. https://doi.org/10.3390/jcm12031045
Chicago/Turabian StyleKim, Yun Gi, Kyung-Do Han, Seung-Young Roh, Joo Hee Jeong, Yun Young Choi, Kyongjin Min, Jaemin Shim, Jong-Il Choi, and Young-Hoon Kim. 2023. "Being Underweight Is Associated with Increased Risk of Sudden Cardiac Death in People with Diabetes Mellitus" Journal of Clinical Medicine 12, no. 3: 1045. https://doi.org/10.3390/jcm12031045
APA StyleKim, Y. G., Han, K.-D., Roh, S.-Y., Jeong, J. H., Choi, Y. Y., Min, K., Shim, J., Choi, J.-I., & Kim, Y.-H. (2023). Being Underweight Is Associated with Increased Risk of Sudden Cardiac Death in People with Diabetes Mellitus. Journal of Clinical Medicine, 12(3), 1045. https://doi.org/10.3390/jcm12031045






