Total Ankle Replacement Infections: A Systematic Review of the Literature
Abstract
1. Introduction
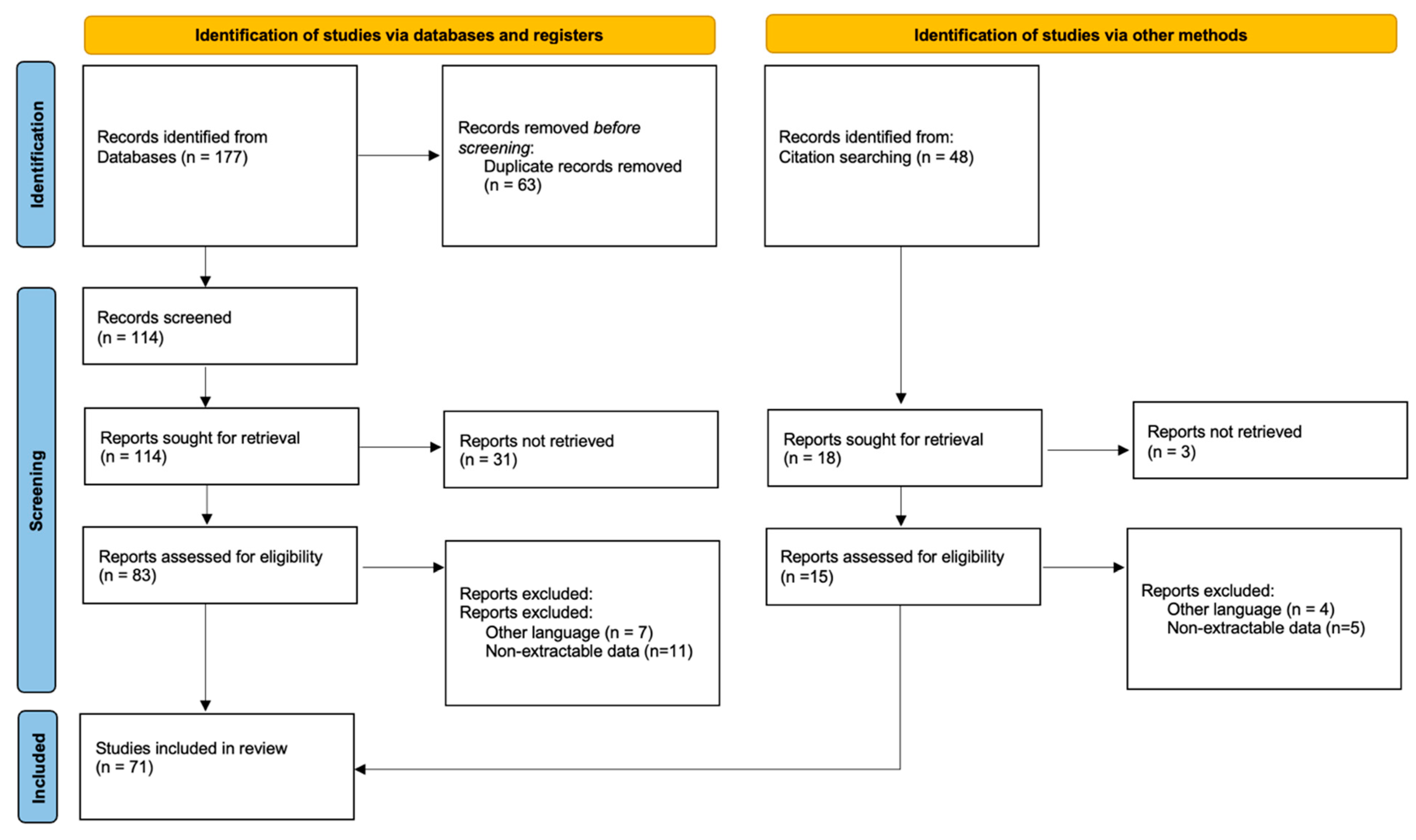
2. Methods
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Glazebrook, M.; Daniels, T.; Younger, A.; Foote, C.J.; Penner, M.; Wing, K.; Lau, J.; Leighton, R.; Dunbar, M. Comparison of health-related quality of life between patients with end-stage ankle and hip arthrosis. J. Bone Jt. Surg. Am. 2008, 90, 499–505. [Google Scholar] [CrossRef]
- Haddad, S.L.; Coetzee, J.C.; Estok, R.; Fahrbach, K.; Banel, D.; Nalysnyk, L. Intermediate and long-term outcomes of total ankle arthroplasty and ankle arthrodesis. A systematic review of the literature. J. Bone Jt. Surg. Am. 2007, 89, 1899–1905. [Google Scholar] [CrossRef]
- Terrell, R.D.; Montgomery, S.R.; Pannell, W.C.; Sandlin, M.I.; Inoue, H.; Wang, J.C.; SooHoo, N.F. Comparison of practice patterns in total ankle replacement and ankle fusion in the United States. Foot Ankle Int. 2013, 34, 1486–1492. [Google Scholar] [CrossRef] [PubMed]
- Jordan, R.W.; Chahal, G.S.; Chapman, A. Is end-stage ankle arthrosis best managed with total ankle replacement or arthrodesis? A systematic review. Adv. Orthop. 2014, 2014, 986285. [Google Scholar] [CrossRef] [PubMed]
- SooHoo, N.F.; Zingmond, D.S.; Ko, C.Y. Comparison of reoperation rates following ankle arthrodesis and total ankle arthroplasty. J. Bone Jt. Surg. Am. 2007, 89, 2143–2149. [Google Scholar] [CrossRef]
- Hintermann, B.; Zwicky, L.; Knupp, M.; Henninger, H.B.; Barg, A. HINTEGRA revision arthroplasty for failed total ankle prostheses. J. Bone Jt. Surg. Am. 2013, 95, 1166–1174. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Akoh, C.C.; Kadakia, R.; Somerson, J.S.; Easley, M.E.; Adams, S.B.; DeOrio, J.K.; Nunley, J.A. Analysis of 408 Total Ankle Arthroplasty Adverse Events Reported to the US Food and Drug Administration From 2015 to 2018. Foot Ankle Spec. 2021, 14, 393–400. [Google Scholar] [CrossRef] [PubMed]
- Clough, T.M.; Alvi, F.; Majeed, H. Total ankle arthroplasty: What are the risks?: A guide to surgical consent and a review of the literature. Bone Jt. J. 2018, 100-B, 1352–1358. [Google Scholar] [CrossRef]
- Gougoulias, N.; Khanna, A.; Maffulli, N. How successful are current ankle replacements?: A systematic review of the literature. Clin. Orthop. Relat. Res. 2010, 468, 199–208. [Google Scholar] [CrossRef]
- Mazzotti, A.; Geraci, G.; Panciera, A.; Perna, F.; Stefanini, N.; Pilla, F.; Ruffilli, A.; Faldini, C. Trends in surgical management of the infected total ankle arthroplasty. Eur. Rev. Med. Pharmacol. Sci. 2019, 23, 159–172. [Google Scholar] [CrossRef]
- Kessler, B.; Knupp, M.; Graber, P.; Zwicky, L.; Hintermann, B.; Zimmerli, W.; Sendi, P. The treatment and outcome of peri-prosthetic infection of the ankle: A single cohort-centre experience of 34 cases. Bone Jt. J. 2014, 96-B, 772–777. [Google Scholar] [CrossRef] [PubMed]
- Kessler, B.; Sendi, P.; Graber, P.; Knupp, M.; Zwicky, L.; Hintermann, B.; Zimmerli, W. Risk factors for periprosthetic ankle joint infection: A case-control study. J. Bone Jt. Surg. Am. 2012, 94, 1871–1876. [Google Scholar] [CrossRef] [PubMed]
- van der Heide, H.J.; Schutte, B.; Louwerens, J.W.; van den Hoogen, F.H.; Malefijt, M.C. Total ankle prostheses in rheumatoid arthropathy: Outcome in 52 patients followed for 1–9 years. Acta Orthop. 2009, 80, 440–444. [Google Scholar] [CrossRef] [PubMed]
- Doets, H.C.; Brand, R.; Nelissen, R.G. Total ankle arthroplasty in inflammatory joint disease with use of two mobile-bearing designs. J. Bone Jt. Surg. Am. 2006, 88, 1272–1284. [Google Scholar] [CrossRef] [PubMed]
- Santos, A.L.; Demange, M.K.; Prado, M.P.; Fernandes, T.D.; Giglio, P.N.; Hintermann, B. Cartilage lesions and ankle osteoarthrosis: Review of the literature and treatment algorithm. Rev. Bras. Ortop. 2014, 49, 565–572. [Google Scholar] [CrossRef][Green Version]
- Walley, K.C.; Arena, C.B.; Juliano, P.J.; Aynardi, M.C. Diagnostic Criteria and Treatment of Acute and Chronic Periprosthetic Joint Infection of Total Ankle Arthroplasty. Foot Ankle Orthop. 2019, 4, 2473011419841000. [Google Scholar] [CrossRef]
- Page, M.J.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. BMJ 2021, 372, n160. [Google Scholar] [CrossRef]
- Myerson, M.S.; Shariff, R.; Zonno, A.J. The management of infection following total ankle replacement: Demographics and treatment. Foot Ankle Int. 2014, 35, 855–862. [Google Scholar] [CrossRef]
- Patton, D.; Kiewiet, N.; Brage, M. Infected total ankle arthroplasty: Risk factors and treatment options. Foot Ankle Int. 2015, 36, 626–634. [Google Scholar] [CrossRef]
- Carlsson, A.S.; Montgomery, F.; Besjakov, J. Arthrodesis of the ankle secondary to replacement. Foot Ankle Int. 1998, 19, 240–245. [Google Scholar] [CrossRef]
- Kotnis, R.; Pasapula, C.; Anwar, F.; Cooke, P.H.; Sharp, R.J. The management of failed ankle replacement. J. Bone Jt. Surg. Br. 2006, 88, 1039–1047. [Google Scholar] [CrossRef]
- Wood, P.L.; Deakin, S. Total ankle replacement. The results in 200 ankles. J. Bone Jt. Surg. Br. 2003, 85, 334–341. [Google Scholar] [CrossRef]
- Lee, K.B.; Cho, S.G.; Hur, C.I.; Yoon, T.R. Perioperative complications of HINTEGRA total ankle replacement: Our initial 50 cases. Foot Ankle Int. 2008, 29, 978–984. [Google Scholar] [CrossRef]
- Saltzman, C.L.; Amendola, A.; Anderson, R.; Coetzee, J.C.; Gall, R.J.; Haddad, S.L.; Herbst, S.; Lian, G.; Sanders, R.W.; Scioli, M.; et al. Surgeon training and complications in total ankle arthroplasty. Foot Ankle Int. 2003, 24, 514–518. [Google Scholar] [CrossRef]
- Schutte, B.G.; Louwerens, J.W. Short-term results of our first 49 Scandanavian total ankle replacements (STAR). Foot Ankle Int. 2008, 29, 124–127. [Google Scholar] [CrossRef]
- Young, J.L.; May, M.M.; Haddad, S.L. Infected total ankle arthroplasty following routine dental procedure. Foot Ankle Int. 2009, 30, 252–257. [Google Scholar] [CrossRef] [PubMed]
- Henricson, A.; Knutson, K.; Lindahl, J.; Rydholm, U. The AES total ankle replacement: A mid-term analysis of 93 cases. Foot Ankle Surg. 2010, 16, 61–64. [Google Scholar] [CrossRef] [PubMed]
- Reuver, J.M.; Dayerizadeh, N.; Burger, B.; Elmans, L.; Hoelen, M.; Tulp, N. Total ankle replacement outcome in low volume centers: Short-term followup. Foot Ankle Int. 2010, 31, 1064–1068. [Google Scholar] [CrossRef]
- Devries, J.G.; Berlet, G.C.; Lee, T.H.; Hyer, C.F.; Deorio, J.K. Revision total ankle replacement: An early look at agility to INBONE. Foot Ankle Spec. 2011, 4, 235–244. [Google Scholar] [CrossRef] [PubMed]
- Ferrao, P.; Myerson, M.S.; Schuberth, J.M.; McCourt, M.J. Cement spacer as definitive management for postoperative ankle infection. Foot Ankle Int. 2012, 33, 173–178. [Google Scholar] [CrossRef] [PubMed]
- McCoy, T.H.; Goldman, V.; Fragomen, A.T.; Rozbruch, S.R. Circular external fixator-assisted ankle arthrodesis following failed total ankle arthroplasty. Foot Ankle Int. 2012, 33, 947–955. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues-Pinto, R.; Muras, J.; Martín Oliva, X.; Amado, P. Functional results and complication analysis after total ankle replacement: Early to medium-term results from a Portuguese and Spanish prospective multicentric study. Foot Ankle Surg. 2013, 19, 222–228. [Google Scholar] [CrossRef] [PubMed]
- Oliver, S.M.; Coetzee, J.C.; Nilsson, L.J.; Samuelson, K.M.; Stone, R.M.; Fritz, J.E.; Giveans, M.R. Early Patient Satisfaction Results on a Modern Generation Fixed-Bearing Total Ankle Arthroplasty. Foot Ankle Int. 2016, 37, 938–943. [Google Scholar] [CrossRef]
- Richter, D.; Krähenbühl, N.; Susdorf, R.; Barg, A.; Ruiz, R.; Hintermann, B. What Are the Indications for Implant Revision in Three-component Total Ankle Arthroplasty? Clin. Orthop. Relat. Res. 2021, 479, 601–609. [Google Scholar] [CrossRef] [PubMed]
- Brunner, S.; Barg, A.; Knupp, M.; Zwicky, L.; Kapron, A.L.; Valderrabano, V.; Hintermann, B. The Scandinavian total ankle replacement: Long-term, eleven to fifteen-year, survivorship analysis of the prosthesis in seventy-two consecutive patients. J. Bone Jt. Surg. Am. 2013, 95, 711–718. [Google Scholar] [CrossRef] [PubMed]
- Clough, T.; Bodo, K.; Majeed, H.; Davenport, J.; Karski, M. Survivorship and long-term outcome of a consecutive series of 200 Scandinavian Total Ankle Replacement (STAR) implants. Bone Jt. J. 2019, 101-B, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Adams, S.B.; Demetracopoulos, C.A.; Queen, R.M.; Easley, M.E.; DeOrio, J.K.; Nunley, J.A. Early to mid-term results of fixed-bearing total ankle arthroplasty with a modular intramedullary tibial component. J. Bone Jt. Surg. Am. 2014, 96, 1983–1989. [Google Scholar] [CrossRef] [PubMed]
- Bennett, A.; Ramaskandhan, J.; Siddique, M. Total Ankle Replacement for Osteoarthritis Following Pilon Fracture of the Tibia. Foot Ankle Int. 2018, 39, 1008–1018. [Google Scholar] [CrossRef]
- Berlet, G.C.; Brandão, R.A.; Consul, D.; Ebaugh, P.; Hyer, C.F. Short- to Midterm Follow-up of Cemented Total Ankle Replacement Using the INBONE II: A Retrospective Chart Review. Foot Ankle Spec. 2021, 14, 302–311. [Google Scholar] [CrossRef] [PubMed]
- Bianchi, A.; Martinelli, N.; Sartorelli, E.; Malerba, F. The Bologna-Oxford total ankle replacement: A mid-term follow-up study. J. Bone Jt. Surg. Br. 2012, 94, 793–798. [Google Scholar] [CrossRef]
- Borenstein, T.R.; Anand, K.; Li, Q.; Charlton, T.P.; Thordarson, D.B. A Review of Perioperative Complications of Outpatient Total Ankle Arthroplasty. Foot Ankle Int. 2018, 39, 143–148. [Google Scholar] [CrossRef]
- Bouchard, M.; Amin, A.; Pinsker, E.; Khan, R.; Deda, E.; Daniels, T.R. The impact of obesity on the outcome of total ankle replacement. J. Bone Jt. Surg. Am. 2015, 97, 904–910. [Google Scholar] [CrossRef] [PubMed]
- Lewis, J.S.; Green, C.L.; Adams, S.B.; Easley, M.E.; DeOrio, J.K.; Nunley, J.A. Comparison of First- and Second-Generation Fixed-Bearing Total Ankle Arthroplasty Using a Modular Intramedullary Tibial Component. Foot Ankle Int. 2015, 36, 881–890. [Google Scholar] [CrossRef] [PubMed]
- Loewy, E.M.; Sanders, T.H.; Walling, A.K. Intermediate-term Experience With the STAR Total Ankle in the United States. Foot Ankle Int. 2019, 40, 268–275. [Google Scholar] [CrossRef] [PubMed]
- Mann, J.A.; Mann, R.A.; Horton, E. STAR™ ankle: Long-term results. Foot Ankle Int. 2011, 32, S473–S484. [Google Scholar] [CrossRef]
- Muir, D.; Aoina, J.; Hong, T.; Mason, R. The outcome of the Mobility total ankle replacement at a mean of four years: Can poor outcomes be predicted from pre- and post-operative analysis? Bone Jt. J. 2013, 95-B, 1366–1371. [Google Scholar] [CrossRef]
- Mosca, M.; Caravelli, S.; Vocale, E.; Maitan, N.; Grassi, A.; Massimi, S.; Fuiano, M.; Zaffagnini, S. Clinical-radiological outcomes and complications after total ankle replacement through a lateral transfibular approach: A retrospective evaluation at a mid-term follow-up. Int. Orthop. 2021, 45, 437–443. [Google Scholar] [CrossRef] [PubMed]
- Buechel, F.F.; Pappas, M.J. Ten-year evaluation of cementless Buechel-Pappas meniscal bearing total ankle replacement. Foot Ankle Int. 2003, 24, 462–472. [Google Scholar] [CrossRef] [PubMed]
- Claridge, R.J.; Sagherian, B.H. Intermediate term outcome of the agility total ankle arthroplasty. Foot Ankle Int. 2009, 30, 824–835. [Google Scholar] [CrossRef]
- Lachman, J.R.; Ramos, J.A.; DeOrio, J.K.; Easley, M.E.; Nunley, J.A.; Adams, S.B. Outcomes of Acute Hematogenous Periprosthetic Joint Infection in Total Ankle Arthroplasty Treated With Irrigation, Debridement, and Polyethylene Exchange. Foot Ankle Int. 2018, 39, 1266–1271. [Google Scholar] [CrossRef]
- Wagener, J.; Gross, C.E.; Schweizer, C.; Lang, T.H.; Hintermann, B. Custom-made total ankle arthroplasty for the salvage of major talar bone loss. Bone Jt. J. 2017, 99-B, 231–236. [Google Scholar] [CrossRef] [PubMed]
- Usuelli, F.G.; Indino, C.; Maccario, C.; Manzi, L.; Liuni, F.M.; Vulcano, E. Infections in primary total ankle replacement: Anterior approach versus lateral transfibular approach. Foot Ankle Surg. 2019, 25, 19–23. [Google Scholar] [CrossRef] [PubMed]
- Tan, E.W.; Maccario, C.; Talusan, P.G.; Schon, L.C. Early Complications and Secondary Procedures in Transfibular Total Ankle Replacement. Foot Ankle Int. 2016, 37, 835–841. [Google Scholar] [CrossRef] [PubMed]
- Strauss, A.C.; Goldmann, G.; Wessling, M.; Gravius, S.; Müller, M.C.; Wimmer, M.D.; Wirtz, D.C.; Oldenburg, J.; Pennekamp, P.H. Total ankle replacement in patients with haemophilia and virus infections—A safe alternative to ankle arthrodesis? Haemophilia 2014, 20, 702–708. [Google Scholar] [CrossRef] [PubMed]
- Cody, E.A.; Taylor, M.A.; Nunley, J.A.; Parekh, S.G.; DeOrio, J.K. Increased Early Revision Rate With the INFINITY Total Ankle Prosthesis. Foot Ankle Int. 2019, 40, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Cody, E.A.; Bejarano-Pineda, L.; Lachman, J.R.; Taylor, M.A.; Gausden, E.B.; DeOrio, J.K.; Easley, M.E.; Nunley, J.A. Risk Factors for Failure of Total Ankle Arthroplasty With a Minimum Five Years of Follow-up. Foot Ankle Int. 2019, 40, 249–258. [Google Scholar] [CrossRef]
- Daniels, T.R.; Younger, A.S.; Penner, M.; Wing, K.; Dryden, P.J.; Wong, H.; Glazebrook, M. Intermediate-term results of total ankle replacement and ankle arthrodesis: A COFAS multicenter study. J. Bone Jt. Surg. Am. 2014, 96, 135–142. [Google Scholar] [CrossRef]
- Nieuwe Weme, R.A.; van Solinge, G.; N Doornberg, J.; Sierevelt, I.; Haverkamp, D.; Doets, H.C. Total ankle replacement for posttraumatic arthritis. Similar outcome in postfracture and instability arthritis: A comparison of 90 ankles. Acta Orthop. 2015, 86, 401–406. [Google Scholar] [CrossRef]
- Noelle, S.; Egidy, C.C.; Cross, M.B.; Gebauer, M.; Klauser, W. Complication rates after total ankle arthroplasty in one hundred consecutive prostheses. Int. Orthop. 2013, 37, 1789–1794. [Google Scholar] [CrossRef]
- Pangrazzi, G.J.; Baker, E.A.; Shaheen, P.J.; Okeagu, C.N.; Fortin, P.T. Single-Surgeon Experience and Complications of a Fixed-Bearing Total Ankle Arthroplasty. Foot Ankle Int. 2018, 39, 46–58. [Google Scholar] [CrossRef]
- Pedersen, E.; Pinsker, E.; Younger, A.S.; Penner, M.J.; Wing, K.J.; Dryden, P.J.; Glazebrook, M.; Daniels, T.R. Outcome of total ankle arthroplasty in patients with rheumatoid arthritis and noninflammatory arthritis. A multicenter cohort study comparing clinical outcome and safety. J. Bone Jt. Surg. Am. 2014, 96, 1768–1775. [Google Scholar] [CrossRef]
- Demetracopoulos, C.A.; Adams, S.B.; Queen, R.M.; DeOrio, J.K.; Nunley, J.A.; Easley, M.E. Effect of Age on Outcomes in Total Ankle Arthroplasty. Foot Ankle Int. 2015, 36, 871–880. [Google Scholar] [CrossRef] [PubMed]
- Demetracopoulos, C.A.; Cody, E.A.; Adams, S.B.; DeOrio, J.K.; Nunley, J.A.; Easley, M.E. Outcomes of Total Ankle Arthroplasty in Moderate and Severe Valgus Deformity. Foot Ankle Spec. 2019, 12, 238–245. [Google Scholar] [CrossRef] [PubMed]
- Di Iorio, A.; Viste, A.; Fessy, M.H.; Besse, J.L. The AES total ankle arthroplasty analysis of failures and survivorship at ten years. Int. Orthop. 2017, 41, 2525–2533. [Google Scholar] [CrossRef] [PubMed]
- Faber, F.W.M.; Mastboom, M.J.L.; van Vliet-Koppert, S.T.; Bouman, I.C.E.; van Kampen, P.M. Outcome after 52 Salto Ankle Prostheses Implanted by a Single Surgeon. Adv. Orthop. 2018, 2018, 2735634. [Google Scholar] [CrossRef]
- Giannini, S.; Romagnoli, M.; Barbadoro, P.; Marcheggiani Muccioli, G.M.; Cadossi, M.; Grassi, A.; Zaffagnini, S. Results at a minimum follow-up of 5 years of a ligaments-compatible total ankle replacement design. Foot Ankle Surg. 2017, 23, 116–121. [Google Scholar] [CrossRef]
- Gross, C.E.; Hamid, K.S.; Green, C.; Easley, M.E.; DeOrio, J.K.; Nunley, J.A. Operative Wound Complications Following Total Ankle Arthroplasty. Foot Ankle Int. 2017, 38, 360–366. [Google Scholar] [CrossRef] [PubMed]
- Harston, A.; Lazarides, A.L.; Adams, S.B.; DeOrio, J.K.; Easley, M.E.; Nunley, J.A. Midterm Outcomes of a Fixed-Bearing Total Ankle Arthroplasty With Deformity Analysis. Foot Ankle Int. 2017, 38, 1295–1300. [Google Scholar] [CrossRef]
- Heida, K.A.; Waterman, B.; Tatro, E.; Bader, J.; McCoy, A.C.; Rensing, N.; Orr, J. Short-Term Perioperative Complications and Mortality After Total Ankle Arthroplasty in the United States. Foot Ankle Spec. 2018, 11, 123–132. [Google Scholar] [CrossRef]
- Henricson, A.; Carlsson, Å. Survival Analysis of the Single- and Double-Coated STAR Ankle up to 20 Years: Long-Term Follow-up of 324 Cases From the Swedish Ankle Registry. Foot Ankle Int. 2015, 36, 1156–1160. [Google Scholar] [CrossRef]
- Hurowitz, E.J.; Gould, J.S.; Fleisig, G.S.; Fowler, R. Outcome analysis of agility total ankle replacement with prior adjunctive procedures: Two to six year followup. Foot Ankle Int. 2007, 28, 308–312. [Google Scholar] [CrossRef]
- Jung, H.G.; Shin, M.H.; Lee, S.H.; Eom, J.S.; Lee, D.O. Comparison of the outcomes between two 3-component total ankle implants. Foot Ankle Int. 2015, 36, 656–663. [Google Scholar] [CrossRef]
- Karantana, A.; Hobson, S.; Dhar, S. The scandinavian total ankle replacement: Survivorship at 5 and 8 years comparable to other series. Clin. Orthop. Relat. Res. 2010, 468, 951–957. [Google Scholar] [CrossRef] [PubMed]
- Kerkhoff, Y.R.A.; Kosse, N.M.; Louwerens, J.W.K. Short term results of the Mobility Total Ankle System: Clinical and radiographic outcome. Foot Ankle Surg. 2016, 22, 152–157. [Google Scholar] [CrossRef]
- Koivu, H.; Kohonen, I.; Mattila, K.; Loyttyniemi, E.; Tiusanen, H. Long-term Results of Scandinavian Total Ankle Replacement. Foot Ankle Int. 2017, 38, 723–731. [Google Scholar] [CrossRef] [PubMed]
- Koo, K.; Liddle, A.D.; Pastides, P.S.; Rosenfeld, P.F. The Salto total ankle arthroplasty—Clinical and radiological outcomes at five years. Foot Ankle Surg. 2019, 25, 523–528. [Google Scholar] [CrossRef]
- Kraal, T.; van der Heide, H.J.; van Poppel, B.J.; Fiocco, M.; Nelissen, R.G.; Doets, H.C. Long-term follow-up of mobile-bearing total ankle replacement in patients with inflammatory joint disease. Bone Jt. J. 2013, 95-B, 1656–1661. [Google Scholar] [CrossRef]
- Lagaay, P.M.; Schuberth, J.M. Analysis of ankle range of motion and functional outcome following total ankle arthoplasty. J. Foot Ankle Surg. 2010, 49, 147–151. [Google Scholar] [CrossRef] [PubMed]
- Halverson, A.L.; Goss, D.A.; Berlet, G.C. Ankle Arthrodesis With Structural Grafts Can Work for the Salvage of Failed Total Ankle Arthroplasty. Foot Ankle Spec. 2020, 13, 132–137. [Google Scholar] [CrossRef]
- Kamrad, I.; Henricsson, A.; Karlsson, M.K.; Magnusson, H.; Nilsson, J.; Carlsson, Å.; Rosengren, B.E. Poor prosthesis survival and function after component exchange of total ankle prostheses. Acta Orthop. 2015, 86, 407–411. [Google Scholar] [CrossRef]
- Rahm, S.; Klammer, G.; Benninger, E.; Gerber, F.; Farshad, M.; Espinosa, N. Inferior results of salvage arthrodesis after failed ankle replacement compared to primary arthrodesis. Foot Ankle Int. 2015, 36, 349–359. [Google Scholar] [CrossRef]
- Berkowitz, M.J.; Clare, M.P.; Walling, A.K.; Sanders, R. Salvage of failed total ankle arthroplasty with fusion using structural allograft and internal fixation. Foot Ankle Int. 2011, 32, S493–S502. [Google Scholar] [CrossRef]
- Bai, L.B.; Lee, K.B.; Song, E.K.; Yoon, T.R.; Seon, J.K. Total ankle arthroplasty outcome comparison for post-traumatic and primary osteoarthritis. Foot Ankle Int. 2010, 31, 1048–1056. [Google Scholar] [CrossRef]
- Najefi, A.; Malhotra, K.; Chan, O.; Cullen, N.; Goldberg, A. The Bologna-Oxford ankle replacement: A case series of clinical and radiological outcomes. Int. Orthop. 2019, 43, 2333–2339. [Google Scholar] [CrossRef]
- Spirt, A.A.; Assal, M.; Hansen, S.T. Complications and failure after total ankle arthroplasty. J. Bone Jt. Surg. Am. 2004, 86, 1172–1178. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.S.; Ahn, J.Y.; Lee, J.S.; Lee, J.Y.; Jeong, J.J.; Choi, Y.R. Cement arthroplasty for ankle joint destruction. J. Bone Jt. Surg. Am. 2014, 96, 1468–1475. [Google Scholar] [CrossRef] [PubMed]
- Zaidi, R.; Cro, S.; Gurusamy, K.; Siva, N.; Macgregor, A.; Henricson, A.; Goldberg, A. The outcome of total ankle replacement: A systematic review and meta-analysis. Bone Jt. J. 2013, 95-B, 1500–1507. [Google Scholar] [CrossRef] [PubMed]
- McKenna, B.J.; Cook, J.; Cook, E.A.; Crafton, J.; Knabel, M.; Swenson, E.; Miner, S.; Manning, E.; Basile, P. Total Ankle Arthroplasty Survivorship: A Meta-analysis. J. Foot Ankle Surg. 2020, 59, 1040–1048. [Google Scholar] [CrossRef] [PubMed]
- Jämsen, E.; Huhtala, H.; Puolakka, T.; Moilanen, T. Risk factors for infection after knee arthroplasty. A register-based analysis of 43,149 cases. J. Bone Jt. Surg. Am. 2009, 91, 38–47. [Google Scholar] [CrossRef]
- Romanò, C.; Logoluso, N.; Drago, L.; Peccati, A.; Romanò, D. Role for irrigation and debridement in periprosthetic infections. J. Knee Surg. 2014, 27, 267–272. [Google Scholar] [CrossRef]
- Kunutsor, S.K.; Beswick, A.D.; Whitehouse, M.R.; Wylde, V.; Blom, A.W. Debridement, antibiotics and implant retention for periprosthetic joint infections: A systematic review and meta-analysis of treatment outcomes. J. Infect. 2018, 77, 479–488. [Google Scholar] [CrossRef] [PubMed]
- D’Errico, M.; Morelli, I.; Castellini, G.; Gianola, S.; Logoluso, N.; Romanò, D.; Scarponi, S.; Pellegrini, A. Is debridement really the best we can do for periprosthetic joint infections following total ankle replacements? A systematic review and meta-analysis. Foot Ankle Surg. 2022, 28, 697–708. [Google Scholar] [CrossRef] [PubMed]
- Zimmerli, W.; Trampuz, A.; Ochsner, P.E. Prosthetic-joint infections. N. Engl. J. Med. 2004, 351, 1645–1654. [Google Scholar] [CrossRef]
- Doets, H.C.; Zürcher, A.W. Salvage arthrodesis for failed total ankle arthroplasty. Acta Orthop. 2010, 81, 142–147. [Google Scholar] [CrossRef] [PubMed]
- Henricson, A.; Rydholm, U. Use of a trabecular metal implant in ankle arthrodesis after failed total ankle replacement. Acta Orthop. 2010, 81, 745–747. [Google Scholar] [CrossRef] [PubMed]
- Gross, C.; Erickson, B.J.; Adams, S.B.; Parekh, S.G. Ankle arthrodesis after failed total ankle replacement: A systematic review of the literature. Foot Ankle Spec. 2015, 8, 143–151. [Google Scholar] [CrossRef] [PubMed]
- Alrashidi, Y.; Galhoum, A.E.; Wiewiorski, M.; Herrera-Pérez, M.; Hsu, R.Y.; Barg, A.; Valderrabano, V. How To Diagnose and Treat Infection in Total Ankle Arthroplasty. Foot Ankle Clin. 2017, 22, 405–423. [Google Scholar] [CrossRef]
- Horisberger, M.; Henninger, H.B.; Valderrabano, V.; Barg, A. Bone augmentation for revision total ankle arthroplasty with large bone defects. Acta Orthop. 2015, 86, 412–414. [Google Scholar] [CrossRef]
- Bullens, P.; de Waal Malefijt, M.; Louwerens, J.W. Conversion of failed ankle arthroplasty to an arthrodesis. Technique using an arthrodesis nail and a cage filled with morsellized bone graft. Foot Ankle Surg. 2010, 16, 101–104. [Google Scholar] [CrossRef]
- Culpan, P.; Le Strat, V.; Piriou, P.; Judet, T. Arthrodesis after failed total ankle replacement. J. Bone Jt. Surg. Br. 2007, 89, 1178–1183. [Google Scholar] [CrossRef]
- Thomason, K.; Eyres, K.S. A technique of fusion for failed total replacement of the ankle: Tibio-allograft-calcaneal fusion with a locked retrograde intramedullary nail. J. Bone Jt. Surg. Br. 2008, 90, 885–888. [Google Scholar] [CrossRef]
- Kitaoka, H.B. Salvage of nonunion following ankle arthrodesis for failed total ankle arthroplasty. Clin. Orthop. Relat. Res. 1991, 268, 37–43. [Google Scholar]
- Kitaoka, H.B.; Romness, D.W. Arthrodesis for failed ankle arthroplasty. J. Arthroplast. 1992, 7, 277–284. [Google Scholar] [CrossRef]
- Mulhern, J.L.; Protzman, N.M.; White, A.M.; Brigido, S.A. Salvage of Failed Total Ankle Replacement Using a Custom Titanium Truss. J. Foot Ankle Surg. 2016, 55, 868–873. [Google Scholar] [CrossRef] [PubMed]
- Kharwadkar, N.; Harris, N.J. Revision of STAR total ankle replacement to hybrid AES-STAR total ankle replacement-a report of two cases. Foot Ankle Surg. 2009, 15, 101–105. [Google Scholar] [CrossRef] [PubMed]
- Myerson, M.S.; Won, H.Y. Primary and revision total ankle replacement using custom-designed prostheses. Foot Ankle Clin. 2008, 13, 521–538. [Google Scholar] [CrossRef] [PubMed]
- Anagnostakos, K.; Wilmes, P.; Schmitt, E.; Kelm, J. Elution of gentamicin and vancomycin from polymethylmethacrylate beads and hip spacers in vivo. Acta Orthop. 2009, 80, 193–197. [Google Scholar] [CrossRef] [PubMed]
| Study | Patients (n) | PJI (n) | Incidence (%) | Age, Years (Mean) | Follow-Up, Months (Mean) | Type of Infection | |||
|---|---|---|---|---|---|---|---|---|---|
| Early | Late | Acute Hematogenous | NR | ||||||
| Myerson et al. [18] | 613 | 19 | 3.10% | 57 | 19 | 3 | 15 | 1 | _ |
| Kessler et al. [11] | 511 | 34 | 6.65% | 62 | 31 | 19 | 15 | _ | _ |
| Patton et al. [19] | 966 | 29 | 3.00% | 55 | 55 | 14 | 7 | _ | 8 |
| Carlsson et al. [20] | 100 | 4 | 4.00% | 69 | 40 | _ | 4 | _ | _ |
| Kotnis et al. [21] | 16 | 2 | 12.50% | 56 | 12 | _ | 2 | _ | _ |
| Doets et al. [14] | 93 | 5 | 5.38% | 58 | 84 | 3 | 2 | _ | _ |
| Wood et al. [22] | 200 | 1 | 0.50% | 60 | 46 | _ | 1 | _ | _ |
| Lee et al. [23] | 50 | 1 | 2.00% | 59 | 12 | _ | 1 | _ | _ |
| Saltzman et al. [24] | 90 | 3 | 3.33% | 63 | 6 | _ | 3 | _ | _ |
| Schutte et al. [25] | 49 | 4 | 8.16% | 57 | 28 | _ | _ | 4 | _ |
| V. D. Heide et al. [13] | 58 | 6 | 10.34% | 55 | 30 | _ | 6 | _ | _ |
| Young et al. [26] | 1 | 1 | NA | 58 | 16 | _ | 1 | _ | _ |
| Henricson et al. [27] | 93 | 4 | 4.30% | 57 | 42 | _ | 4 | _ | _ |
| Reuver et al. [28] | 64 | 3 | 4.69% | 57 | 36 | _ | 3 | _ | _ |
| Devries et al. [29] | 5 | 1 | NA | 67 | 17 | _ | 1 | _ | _ |
| Ferrao et al. [30] | 6 | 6 | NA | 63 | 62 | _ | 6 | _ | _ |
| McCoy et al. [31] | 7 | 3 | NA | 59 | 58 | _ | 3 | _ | _ |
| Rodrigues-Pinto et al. [32] | 119 | 2 | 1.68% | 56 | 35 | _ | 2 | _ | _ |
| Hintermann et al. [6] | 117 | 9 | 7.69% | 55 | 72 | _ | 9 | _ | _ |
| Oliver et al. [33] | 245 | 4 | 1.63% | 66 | 39 | _ | 4 | _ | _ |
| Richter et al. [34] | 935 | 11 | 1.18% | 62 | 110 | _ | _ | _ | 11 |
| Brunner et al. [35] | 77 | 1 | 1.30% | 47 | 85 | _ | 1 | _ | _ |
| Clough et al. [36] | 200 | 1 | 0.50% | 60 | 85 | _ | 1 | _ | _ |
| Adams et al. [37] | 194 | 5 | 2.58% | 64 | 4 | 2 | 3 | _ | _ |
| Bennett et al. [38] | 173 | 3 | 1.73% | 60 | 24 | 1 | 2 | _ | _ |
| Berlet et al. [39] | 121 | 3 | 2.48% | 62 | 12 | _ | 3 | _ | _ |
| Bianchi et al. [40] | 62 | 1 | 1.61% | 57 | 42 | _ | 1 | _ | _ |
| Borenstein et al. [41] | 65 | 1 | 1.54% | 64 | 16 | 1 | _ | _ | _ |
| Bouchard et al. [42] | 87 | 1 | 1.15% | 62 | 3.8 | _ | 1 | _ | _ |
| Lewis et al. [43] | 249 | 5 | 2.01% | 60 | 40 | _ | 5 | _ | _ |
| Loewy et al. [44] | 138 | 4 | 2.90% | 62 | 100 | _ | 4 | _ | _ |
| Mann et al. [45] | 84 | 3 | 3.57% | 61 | 108 | 3 | _ | _ | _ |
| Muir et al. [46] | 178 | 3 | 1.69% | 64 | 48 | _ | _ | _ | 3 |
| Mosca et al. [47] | 73 | 1 | 1.37% | 62 | 31 | _ | 1 | _ | _ |
| Buechel et al. [48] | 50 | 2 | 4.00% | 49 | 60 | 1 | 1 | _ | _ |
| Claridge et al. [49] | 28 | 4 | 14.29% | 65 | 45 | _ | 4 | _ | _ |
| Lachmann et al. [50] | 1600 | 14 | 0.88% | 61 | 34 | _ | _ | 14 | _ |
| Wagener et al. [51] | 13 | 1 | 7.69% | 60 | 84 | _ | _ | _ | 1 |
| Usuelli et al. [52] | 150 | 4 | 2.67% | 53 | 12 | _ | 3 | 1 | _ |
| Tan et al. [53] | 20 | 1 | 5.00% | 64 | 18 | _ | _ | _ | 1 |
| Strauss et al. [54] | 11 | 2 | NA | 57 | 30 | 2 | _ | _ | _ |
| Cody et al. [55] | 159 | 6 | 3.77% | 63 | 20 | _ | _ | _ | 6 |
| Cody et al. [56] | 538 | 5 | 0.93% | 62 | 60 | _ | _ | _ | 5 |
| Daniels et al. [57] | 229 | 3 | 1.31% | 62 | 108 | _ | _ | _ | 3 |
| Nieuwe Weme et al. [58] | 88 | 1 | 1.14% | 57 | 60 | _ | 1 | _ | _ |
| Noelle et al. [59] | 97 | 4 | 4.12% | 63 | 36 | _ | _ | _ | 4 |
| Pangrazzi et al. [60] | 104 | 3 | 2.88% | 65 | 46 | _ | _ | _ | 3 |
| Pedersen et al. [61] | 100 | 1 | 1.00% | 59 | 65 | _ | 1 | _ | _ |
| Demetracopoulos et al. [62] | 395 | 3 | 0.76% | 62 | 40 | _ | 3 | _ | _ |
| Demetracopoulos et al. [63] | 80 | 1 | 1.25% | 67 | 40 | _ | 1 | _ | _ |
| Di Iorio et al. [64] | 44 | 2 | 4.55% | 56 | 120 | _ | _ | _ | 2 |
| Faber et al. [65] | 51 | 1 | 1.96% | 70 | 50 | _ | _ | _ | 1 |
| Giannini et al. [66] | 76 | 1 | 1.32% | 62 | 24 | _ | 1 | _ | _ |
| Gross et al. [67] | 762 | 8 | 1.05% | 63 | 13 | _ | 8 | _ | _ |
| Harston et al. [68] | 149 | 1 | 0.67% | 63 | 48 | _ | _ | _ | 1 |
| Heida et al. [69] | 404 | 1 | 0.25% | 65 | NR | _ | _ | _ | 1 |
| Henricson et al. [70] | 324 | 14 | 4.32% | NR | NR | _ | _ | _ | 14 |
| Hurowitz et al. [71] | 62 | 3 | 4.84% | 55 | 40 | _ | 3 | _ | _ |
| Jung et al. [72] | 54 | 3 | 5.56% | 63 | 30 | _ | 3 | _ | _ |
| Karantana et al. [73] | 52 | 1 | 1.92% | 62 | 80 | _ | 1 | _ | _ |
| Kerkhoff et al. [74] | 67 | 2 | 2.99% | 63 | 40 | 1 | 1 | _ | _ |
| Koivu et al. [75] | 34 | 3 | 8.82% | 56 | 159 | _ | 3 | _ | _ |
| Koo et al. [76] | 55 | 1 | 1.82% | 70 | 60 | _ | 1 | _ | _ |
| Kraal et al. [77] | 93 | 3 | 3.23% | 58 | 120 | 1 | 1 | _ | 1 |
| Lagaay et al. [78] | 94 | 1 | 1.06% | 59 | 30 | 1 | _ | _ | _ |
| Halverson et al. [79] | 5 | 1 | NA | 63 | 60 | 1 | _ | _ | _ |
| Kamrad et al. [80] | 73 | 2 | 2.74% | 55 | NR | _ | 2 | _ | _ |
| Rahm et al. [81] | 23 | 6 | 26.09% | 62 | 25 | _ | 6 | _ | _ |
| Berkowitz et al. [82] | 24 | 2 | 8.33% | 62 | 42 | _ | _ | _ | 2 |
| Bai et al. [83] | 67 | 1 | 1.49% | 56 | 38 | _ | 1 | _ | _ |
| Najefi et al. [84] | 34 | 2 | 5.88% | 58 | 58 | _ | _ | 2 | _ |
| Study | Patients | PJI | Timing of PJI, Months (Mean) | Treatment | Final Treatment | PJI Recurrence (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| DAIR | One Stage | Two Stage | Antibiotic | NR | Amputation | Prosthesis | Arthrodesis | Cement Spacer | NR | |||||
| Myerson et al. [18] | 613 | 19 | 18 | 4 | 5 | 10 | _ | _ | 4 | 3 | 6 | 6 | _ | 4 Recurrences (21%) 3 Reinfections (15.7%) |
| Kessler et al. [11] | 511 | 34 | NR | 21 | 4 | 9 | _ | _ | 1 | 26 | 7 | _ | _ | 4 Recurrences (11.7%) 3 Reinfections (8.8%) |
| Patton et al. [19] | 966 | 29 | 18 | 5 | 7 | 17 | _ | _ | 6 | 18 | 3 | 2 | _ | 5 Recurrences (17.2%) |
| Carlsson et al. [20] | 100 | 4 | 59 | _ | 4 | _ | _ | _ | _ | _ | 4 | _ | _ | _ |
| Kotnis et al. [21] | 16 | 2 | 24 | _ | 2 | _ | _ | _ | 1 | _ | 1 | _ | _ | _ |
| Doets et al. [14] | 93 | 5 | NR | 4 | _ | 1 | _ | _ | _ | 4 | 1 | _ | _ | _ |
| Wood et al. [22] | 200 | 1 | NR | _ | 1 | _ | _ | _ | _ | _ | 1 | _ | _ | _ |
| Lee et al. [23] | 50 | 1 | 3 | _ | _ | 1 | _ | _ | _ | 1 | _ | _ | _ | _ |
| Saltzman et al. [24] | 90 | 3 | NR | _ | 2 | 1 | _ | _ | _ | _ | 2 | 1 | _ | 1 Recurrence (33.3%) |
| Schutte et al. [25] | 49 | 4 | NR | _ | 3 | 1 | _ | _ | _ | 1 | 3 | _ | _ | _ |
| V. D. Heide et al. [13] | 58 | 6 | 25 | 3 | 3 | _ | _ | _ | 1 | 3 | 2 | _ | _ | _ |
| Young et al. [26] | 1 | 1 | 42 | _ | _ | 1 | _ | _ | _ | 1 | _ | _ | _ | _ |
| Henricson et al. [27] | 93 | 4 | NR | 1 | 1 | 1 | 1 | _ | _ | 3 | 1 | _ | _ | _ |
| Reuver et al. [28] | 64 | 3 | NR | 1 | 2 | _ | _ | _ | _ | 1 | 2 | _ | _ | _ |
| Devries et al. [29] | 5 | 1 | 48 | _ | _ | 1 | _ | _ | _ | _ | 1 | _ | _ | 1 Recurrence (20%) |
| Ferrao et al. [30] | 6 | 6 | NR | _ | _ | 6 | _ | _ | _ | _ | _ | 6 | _ | _ |
| McCoy et al. [31] | 7 | 3 | 72 | _ | 3 | _ | _ | _ | _ | _ | 3 | _ | _ | _ |
| Rodrigues-Pinto et al. [32] | 119 | 2 | 10 | _ | 1 | 1 | _ | _ | _ | 1 | 1 | _ | _ | _ |
| Hintermann et al. [6] | 117 | 9 | 52 | _ | _ | 9 | _ | _ | _ | 7 | 2 | _ | _ | _ |
| Oliver et al. [33] | 245 | 4 | 20 | _ | 4 | _ | _ | _ | _ | _ | 4 | _ | _ | _ |
| Richter et al. [34] | 935 | 11 | NR | _ | _ | 11 | _ | _ | _ | 11 | _ | _ | _ | _ |
| Brunner et al. [35] | 77 | 1 | 96 | _ | 1 | _ | _ | _ | _ | _ | 1 | _ | _ | _ |
| Clough et al. [36] | 200 | 1 | 80 | _ | 1 | _ | _ | _ | _ | _ | 1 | _ | _ | _ |
| Adams et al. [37] | 194 | 5 | NR | 2 | _ | 3 | _ | _ | 1 | 3 | 1 | _ | _ | _ |
| Bennett et al. [38] | 173 | 3 | NR | 1 | _ | 2 | _ | _ | _ | 3 | _ | _ | _ | _ |
| Berlet et al. [39] | 121 | 3 | NR | _ | _ | 3 | _ | _ | _ | 3 | _ | _ | _ | _ |
| Bianchi et al. [40] | 62 | 1 | 9 | _ | _ | 1 | _ | _ | _ | 1 | _ | _ | _ | _ |
| Borenstein et al. [41] | 65 | 1 | NR | 1 | _ | _ | _ | _ | _ | 1 | _ | _ | _ | _ |
| Bouchard et al. [42] | 87 | 1 | NR | _ | _ | 1 | _ | _ | _ | 1 | _ | _ | _ | _ |
| Lewis et al. [43] | 249 | 5 | NR | 2 | 2 | 1 | _ | _ | 1 | 3 | 1 | _ | _ | _ |
| Loewy et al. [44] | 138 | 4 | 17 | _ | 2 | 2 | _ | _ | _ | 2 | 2 | _ | _ | _ |
| Mann et al. [45] | 84 | 3 | 13 | 3 | _ | _ | _ | _ | _ | 3 | _ | _ | _ | _ |
| Muir et al. [46] | 178 | 3 | NR | _ | _ | 3 | _ | _ | _ | 3 | _ | _ | _ | _ |
| Mosca et al. [47] | 73 | 1 | 3 | _ | _ | 1 | _ | _ | _ | 1 | _ | _ | _ | _ |
| Buechel et al. [48] | 50 | 2 | 3 | _ | _ | _ | _ | 2 | _ | _ | _ | _ | 2 | _ |
| Claridge et al. [49] | 28 | 4 | NR | 2 | _ | 2 | _ | _ | _ | 4 | _ | _ | _ | _ |
| Lachmann et al. [50] | 1600 | 14 | 43 | 14 | _ | _ | _ | _ | 1 | 9 | 4 | _ | _ | 1 Recurrence (7.14%) |
| Wagener et al. [51] | 13 | 1 | 48 | _ | 1 | _ | _ | _ | _ | _ | 1 | _ | _ | _ |
| Usuelli et al. [52] | 150 | 4 | NR | 2 | _ | _ | 2 | _ | _ | 4 | _ | _ | _ | |
| Tan et al. [53] | 20 | 1 | NR | 1 | _ | _ | _ | _ | _ | 1 | _ | _ | _ | _ |
| Strauss et al. [54] | 11 | 2 | 1 | _ | 2 | _ | _ | _ | _ | _ | 2 | _ | _ | _ |
| Cody et al. [55] | 159 | 6 | 13 | _ | _ | _ | _ | 6 | _ | _ | _ | _ | 6 | _ |
| Cody et al. [56] | 538 | 5 | NR | _ | _ | _ | _ | 5 | 3 | _ | _ | _ | 2 | _ |
| Daniels et al. [57] | 229 | 3 | NR | _ | _ | _ | 3 | _ | _ | _ | _ | 3 | _ | |
| Nieuwe Weme et al. [58] | 88 | 1 | NR | _ | _ | _ | _ | 1 | _ | _ | _ | _ | 1 | _ |
| Noelle et al. [59] | 97 | 4 | NR | _ | 1 | 3 | _ | _ | _ | 3 | 1 | _ | _ | |
| Pangrazzi et al. [60] | 104 | 3 | NR | 2 | _ | _ | 1 | _ | _ | 3 | _ | _ | _ | |
| Pedersen et al. [61] | 100 | 1 | 49 | _ | _ | 1 | _ | _ | _ | 1 | _ | _ | _ | _ |
| Demetracopoulos et al. [62] | 395 | 3 | NR | _ | 1 | 2 | _ | _ | 1 | 1 | 1 | _ | _ | _ |
| Demetracopoulos et al. [63] | 80 | 1 | NR | _ | _ | 1 | _ | _ | _ | 1 | _ | _ | _ | _ |
| Di Iorio et al. [64] | 44 | 2 | NR | _ | _ | _ | _ | 2 | _ | _ | _ | _ | 2 | _ |
| Faber et al. [65] | 51 | 1 | NR | _ | _ | _ | _ | 1 | _ | _ | _ | _ | 1 | _ |
| Giannini et al. [66] | 76 | 1 | NR | _ | _ | 1 | _ | _ | _ | 1 | _ | _ | _ | _ |
| Gross et al. [67] | 762 | 8 | NR | 4 | 2 | 2 | _ | _ | 2 | 6 | _ | _ | _ | 1 Recurrence (12.5%) |
| Harston et al. [68] | 149 | 1 | NR | _ | _ | _ | _ | 1 | _ | _ | _ | _ | 1 | _ |
| Heida et al. [69] | 404 | 1 | NR | _ | _ | _ | _ | 1 | _ | _ | _ | _ | 1 | _ |
| Henricson et al. [70] | 324 | 14 | NR | _ | _ | _ | _ | 14 | _ | _ | _ | _ | 14 | _ |
| Hurowitz et al. [71] | 62 | 3 | NR | _ | _ | 2 | _ | 1 | _ | 2 | _ | _ | 1 | _ |
| Jung et al. [72] | 54 | 3 | 20 | 1 | _ | 2 | _ | _ | _ | 3 | _ | _ | _ | _ |
| Karantana et al. [73] | 52 | 1 | NR | _ | 1 | _ | _ | _ | _ | _ | 1 | _ | _ | _ |
| Kerkhoff et al. [74] | 67 | 2 | NR | 1 | _ | 1 | _ | _ | _ | 2 | _ | _ | _ | _ |
| Koivu et al. [75] | 34 | 3 | 53 | _ | _ | _ | _ | 3 | _ | _ | _ | _ | 3 | _ |
| Koo et al. [76] | 55 | 1 | 30 | _ | 1 | _ | _ | _ | _ | _ | 1 | _ | _ | _ |
| Kraal et al. [77] | 93 | 3 | NR | _ | 1 | 1 | _ | 1 | _ | 1 | 1 | _ | 1 | _ |
| Lagaay et al. [78] | 94 | 1 | NR | _ | _ | _ | 1 | _ | _ | 1 | _ | _ | _ | _ |
| Halverson et al. [79] | 5 | 1 | NR | 1 | _ | _ | _ | _ | _ | 1 | _ | _ | _ | 1 Recurrence (100%) |
| Kamrad et al. [80] | 73 | 2 | NR | _ | _ | 2 | _ | _ | _ | 1 | 1 | _ | _ | _ |
| Rahm et al. [81] | 23 | 6 | 33 | _ | 6 | _ | _ | _ | _ | _ | 6 | _ | _ | _ |
| Berkowitz et al. [82] | 24 | 2 | NR | _ | 2 | _ | _ | _ | _ | _ | 2 | _ | _ | _ |
| Bai et al. [83] | 67 | 1 | 6 | _ | 1 | _ | _ | _ | _ | 1 | _ | _ | _ | _ |
| Najefi et al. [84] | 34 | 2 | 26 | 1 | 1 | _ | _ | _ | _ | 1 | 1 | _ | _ | _ |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zunarelli, R.; Fiore, M.; Lonardo, G.; Pace, A.; Persiani, V.; De Paolis, M.; Sambri, A. Total Ankle Replacement Infections: A Systematic Review of the Literature. J. Clin. Med. 2023, 12, 7711. https://doi.org/10.3390/jcm12247711
Zunarelli R, Fiore M, Lonardo G, Pace A, Persiani V, De Paolis M, Sambri A. Total Ankle Replacement Infections: A Systematic Review of the Literature. Journal of Clinical Medicine. 2023; 12(24):7711. https://doi.org/10.3390/jcm12247711
Chicago/Turabian StyleZunarelli, Renato, Michele Fiore, Gianluca Lonardo, Andrea Pace, Valentina Persiani, Massimiliano De Paolis, and Andrea Sambri. 2023. "Total Ankle Replacement Infections: A Systematic Review of the Literature" Journal of Clinical Medicine 12, no. 24: 7711. https://doi.org/10.3390/jcm12247711
APA StyleZunarelli, R., Fiore, M., Lonardo, G., Pace, A., Persiani, V., De Paolis, M., & Sambri, A. (2023). Total Ankle Replacement Infections: A Systematic Review of the Literature. Journal of Clinical Medicine, 12(24), 7711. https://doi.org/10.3390/jcm12247711








