Imaging in Third Molar Surgery: A Clinical Update
Abstract
:1. Introduction
2. Imaging Modalities in Third Molar Surgery
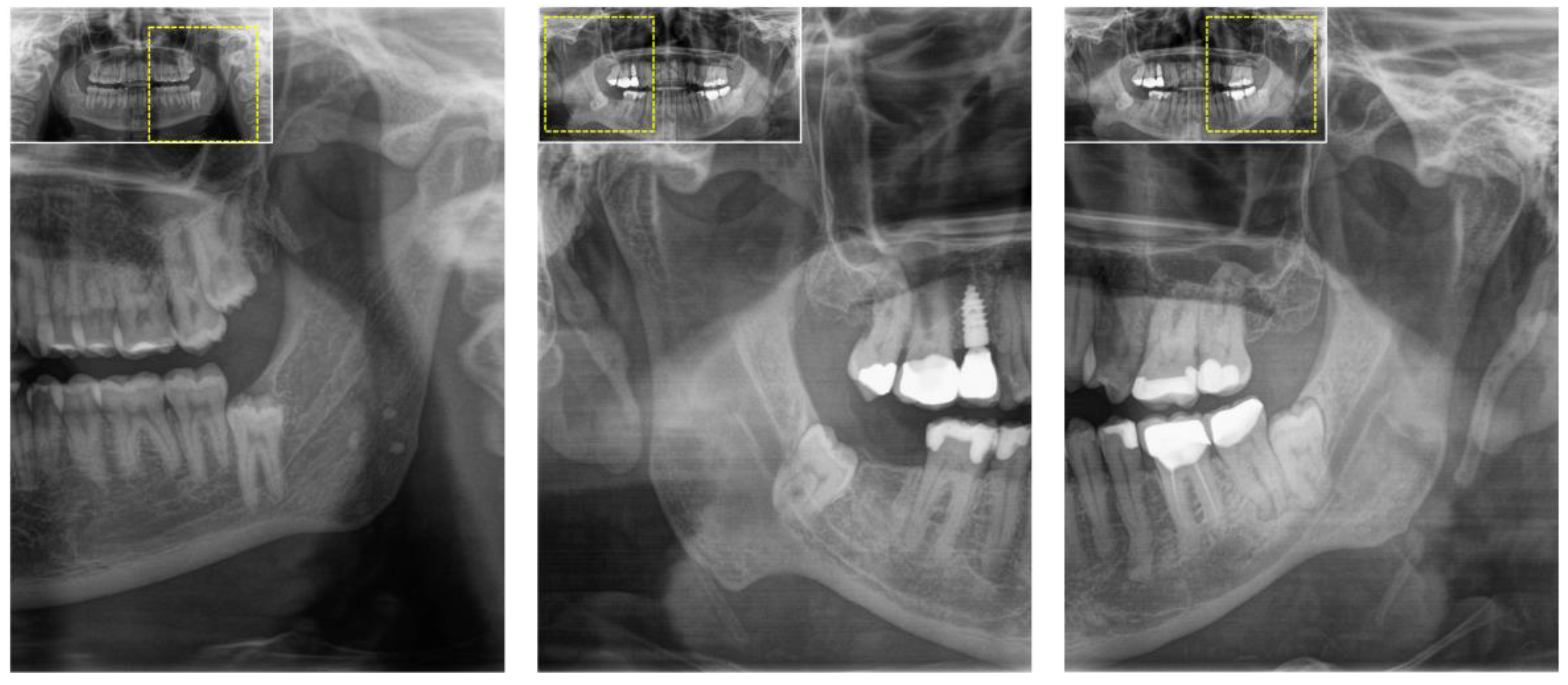
2.1. Orthopantomography (OPG)
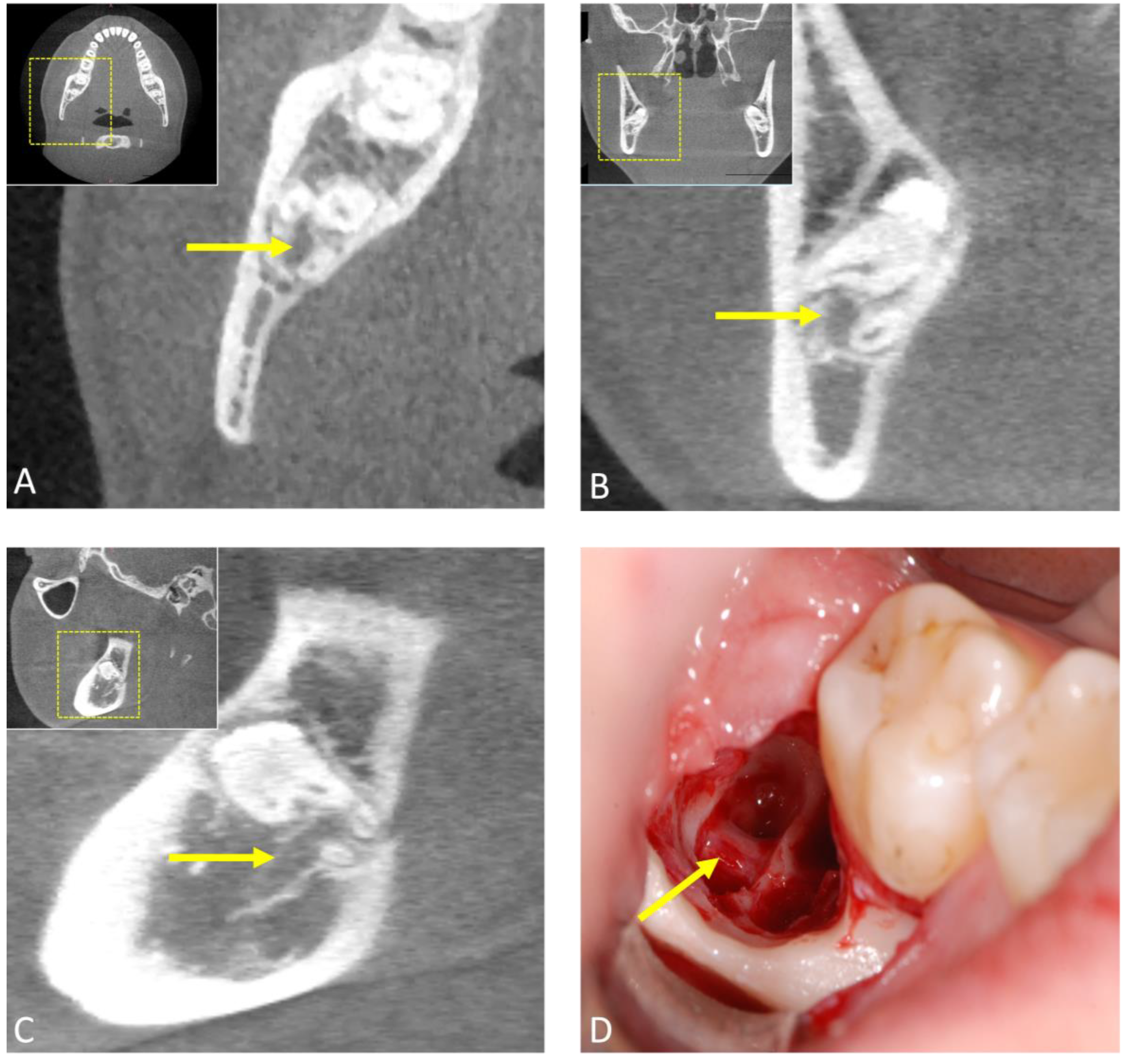
2.2. Computed Tomography (CT)
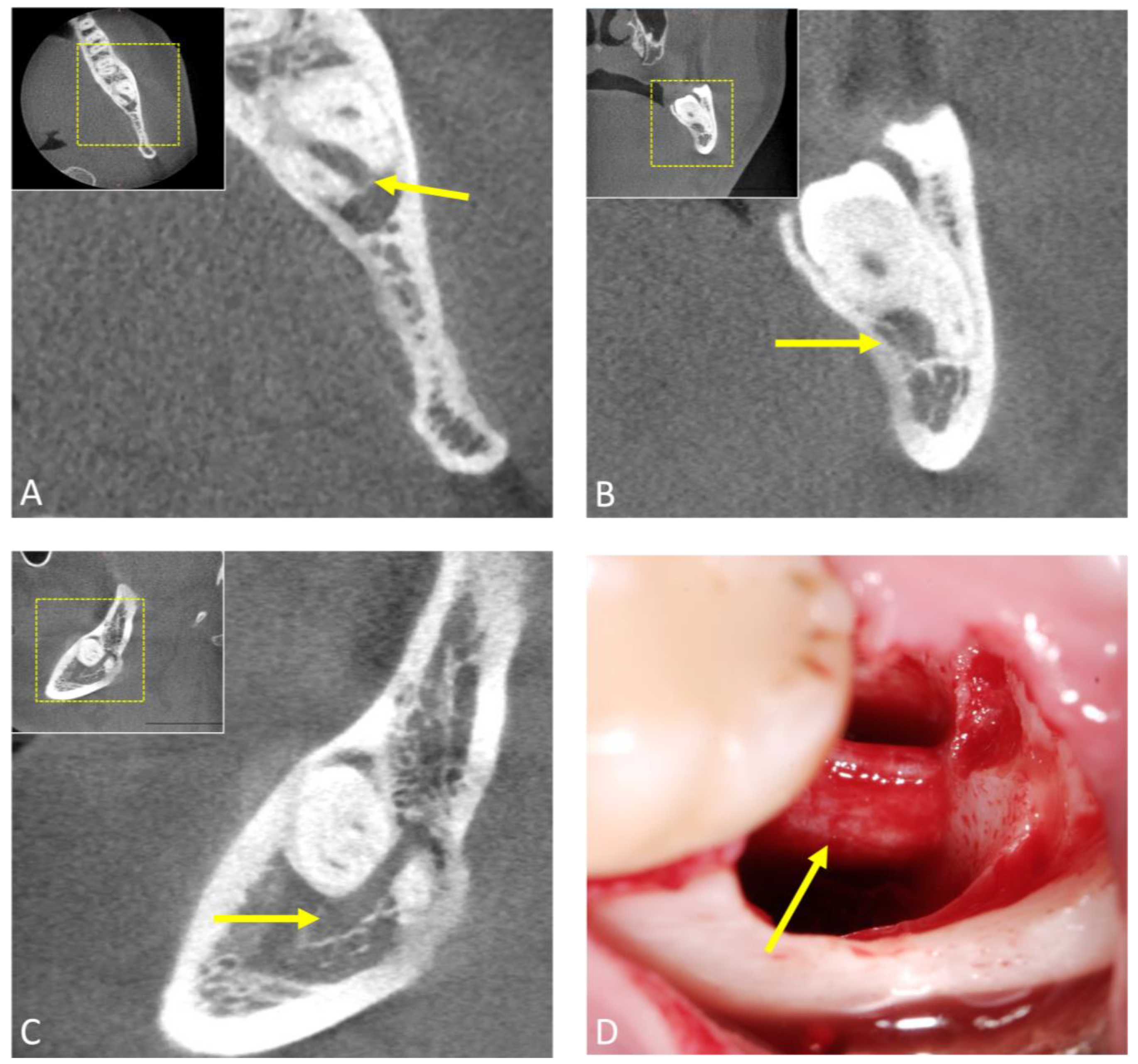
2.3. Cone-Beam Computed Tomography (CBCT)
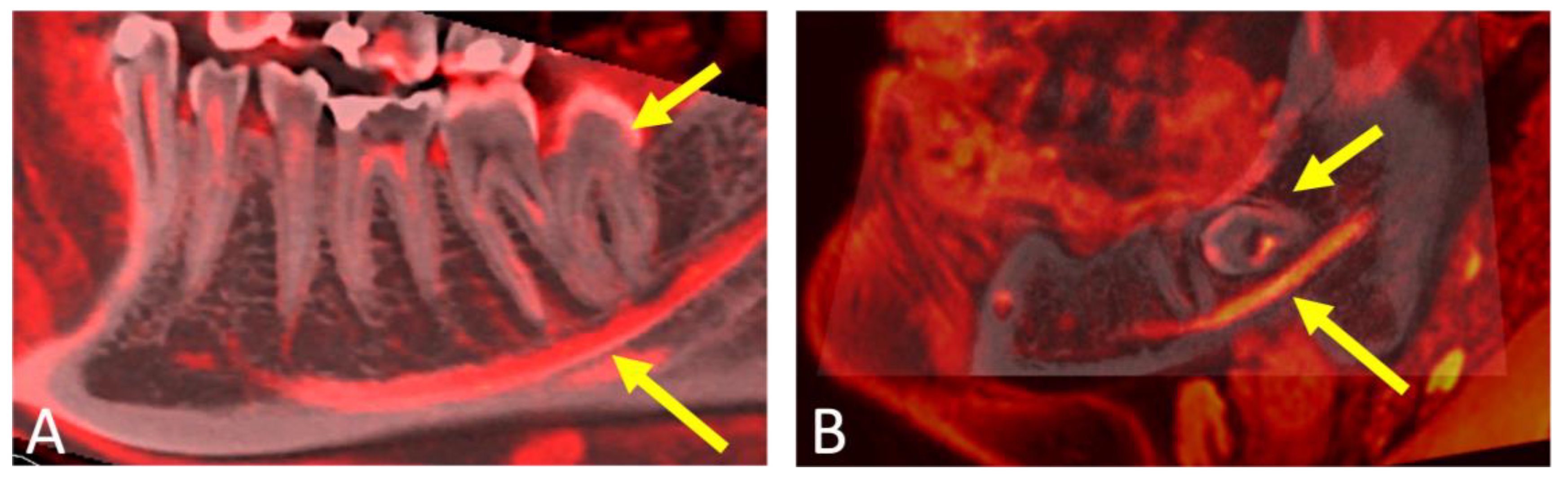
2.4. Photon-Counting Computed Tomography (PCCT)
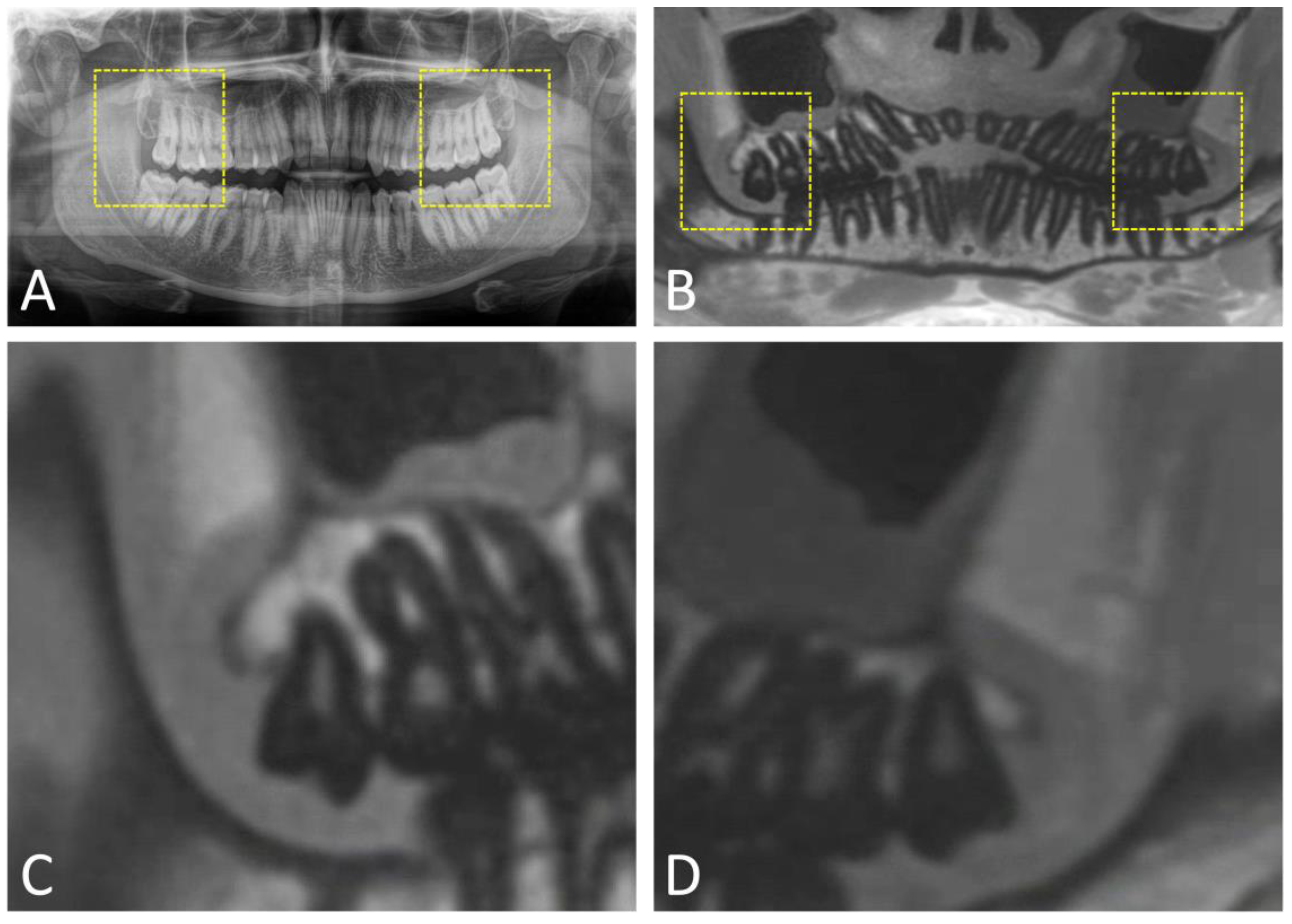
2.5. Magnetic Resonance Imaging (MRI)
3. Artificial Intelligence and Machine Learning in Third Molar Surgery
4. Clinical Recommendations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bailey, E.; Kashbour, W.; Shah, N.; Worthington, H.V.; Renton, T.F.; Coulthard, P. Surgical techniques for the removal of mandibular wisdom teeth. Cochrane Database Syst. Rev. 2020, 7, CD004345. [Google Scholar] [CrossRef] [PubMed]
- Brasileiro, B.F.; de Bragança, R.M.; Van Sickels, J.E. An evaluation of patients’ knowledge about perioperative information for third molar removal. J. Oral Maxillofac. Surg. 2012, 70, 12–18. [Google Scholar] [CrossRef] [PubMed]
- Menchini-Fabris, G.B.; Toti, P.; Crespi, R.; Crespi, G.; Cosola, S.; Covani, U. A Retrospective Digital Analysis of Contour Changing after Tooth Extraction with or without Using Less Traumatic Surgical Procedures. J. Clin. Med. 2022, 11, 922. [Google Scholar] [CrossRef] [PubMed]
- Flygare, L.; Ohman, A. Preoperative imaging procedures for lower wisdom teeth removal. Clin. Oral Investig. 2008, 12, 291–302. [Google Scholar] [CrossRef] [PubMed]
- Steed, M.B. The indications for third-molar extractions. J. Am. Dent. Assoc. 2014, 145, 570–573. [Google Scholar] [CrossRef] [PubMed]
- Jerjes, W.; Swinson, B.; Moles, D.R.; El-Maaytah, M.; Banu, B.; Upile, T.; Kumar, M.; Al Khawalde, M.; Vourvachis, M.; Hadi, H.; et al. Permanent sensory nerve impairment following third molar surgery: A prospective study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2006, 102, e1–e7. [Google Scholar] [CrossRef] [PubMed]
- Qi, W.; Lei, J.; Liu, Y.N.; Li, J.N.; Pan, J.; Yu, G.Y. Evaluating the risk of post-extraction inferior alveolar nerve injury through the relative position of the lower third molar root and inferior alveolar canal. Int. J. Oral Maxillofac. Surg. 2019, 48, 1577–1583. [Google Scholar] [CrossRef] [PubMed]
- Pippi, R.; Spota, A.; Santoro, M. Prevention of Lingual Nerve Injury in Third Molar Surgery: Literature Review. J. Oral Maxillofac. Surg. 2017, 75, 890–900. [Google Scholar] [CrossRef]
- Bouloux, G.F.; Steed, M.B.; Perciaccante, V.J. Complications of third molar surgery. Oral. Maxillofac. Surg. Clin. N. Am. 2007, 19, 117–128. [Google Scholar] [CrossRef]
- Haug, R.H.; Perrott, D.H.; Gonzalez, M.L.; Talwar, R.M. The American Association of Oral and Maxillofacial Surgeons Age-Related Third Molar Study. J. Oral Maxillofac. Surg. 2005, 63, 1106–1114. [Google Scholar] [CrossRef]
- Baqain, Z.H.; Karaky, A.A.; Sawair, F.; Khraisat, A.; Duaibis, R.; Rajab, L.D. Frequency estimates and risk factors for postoperative morbidity after third molar removal: A prospective cohort study. J. Oral Maxillofac. Surg. 2008, 66, 2276–2283. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.C.; Choi, S.S.; Wang, S.J.; Kim, S.G. Minor complications after mandibular third molar surgery: Type, incidence, and possible prevention. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2006, 102, e4–e11. [Google Scholar] [CrossRef] [PubMed]
- Rushton, V.E.; Horner, K. The use of panoramic radiology in dental practice. J. Dent. 1996, 24, 185–201. [Google Scholar] [CrossRef] [PubMed]
- Dula, K.; Bornstein, M.M.; Buser, D.; Dagassan-Berndt, D.; Ettlin, D.A.; Filippi, A.; Gabioud, F.; Katsaros, C.; Krastl, G.; Lambrecht, J.T.; et al. SADMFR guidelines for the use of Cone-Beam Computed Tomography/Digital Volume Tomography. Swiss Dent. J. 2014, 124, 1169–1183. [Google Scholar] [PubMed]
- Schneider, T.; Filo, K.; Kruse, A.L.; Locher, M.; Grätz, K.W.; Lübbers, H.T. Variations in the anatomical positioning of impacted mandibular wisdom teeth and their practical implications. Swiss Dent. J. 2014, 124, 520–538. [Google Scholar]
- Eyrich, G.; Seifert, B.; Matthews, F.; Matthiessen, U.; Heusser, C.K.; Kruse, A.L.; Obwegeser, J.A.; Lübbers, H.T. 3-Dimensional imaging for lower third molars: Is there an implication for surgical removal? J. Oral Maxillofac. Surg. 2011, 69, 1867–1872. [Google Scholar] [CrossRef] [PubMed]
- Vanden Broeke, L.; Grillon, M.; Yeung, A.W.K.; Wu, W.; Tanaka, R.; Vardhanabhuti, V. Feasibility of photon-counting spectral CT in dental applications—A comparative qualitative analysis. BDJ Open 2021, 7, 4. [Google Scholar] [CrossRef] [PubMed]
- Tortora, M.; Gemini, L.; D’Iglio, I.; Ugga, L.; Spadarella, G.; Cuocolo, R. Spectral Photon-Counting Computed Tomography: A Review on Technical Principles and Clinical Applications. J. Imaging 2022, 8, 112. [Google Scholar] [CrossRef]
- Jacobs, R.; Salmon, B.; Codari, M.; Hassan, B.; Bornstein, M.M. Cone beam computed tomography in implant dentistry: Recommendations for clinical use. BMC Oral Health 2018, 18, 88. [Google Scholar] [CrossRef]
- Tsapaki, V. Radiation protection in dental radiology—Recent advances and future directions. Phys. Med. 2017, 44, 222–226. [Google Scholar] [CrossRef]
- Jaju, P.P.; Jaju, S.P. Cone-beam computed tomography: Time to move from ALARA to ALADA. Imaging Sci. Dent. 2015, 45, 263–265. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, T. Dental MRI: A road beyond CBCT. Eur. Radiol. 2020, 30, 6389–6391. [Google Scholar] [CrossRef] [PubMed]
- Al-Haj Husain, A.; Stadlinger, B.; Winklhofer, S.; Piccirelli, M.; Valdec, S. Magnetic resonance imaging for preoperative diagnosis in third molar surgery: A systematic review. Oral Radiol. 2023, 9, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Pakravan, A.H.; Aghamiri, S.M.; Bamdadian, T.; Gholami, M.; Moshfeghi, M. Dosimetry of Occupational Radiation around Panoramic X-ray Apparatus. J. Biomed. Phys. Eng. 2019, 9, 525–532. [Google Scholar] [CrossRef] [PubMed]
- Atieh, M.A. Diagnostic accuracy of panoramic radiography in determining relationship between inferior alveolar nerve and mandibular third molar. J. Oral Maxillofac. Surg. 2010, 68, 74–82. [Google Scholar] [CrossRef] [PubMed]
- Nakagawa, Y.; Ishii, H.; Nomura, Y.; Watanabe, N.Y.; Hoshiba, D.; Kobayashi, K.; Ishibashi, K. Third molar position: Reliability of panoramic radiography. J. Oral Maxillofac. Surg. 2007, 65, 1303–1308. [Google Scholar] [CrossRef] [PubMed]
- Sifuentes-Cervantes, J.S.; Carrillo-Morales, F.; Castro-Núñez, J.; Cunningham, L.L.; Van Sickels, J.E. Third molar surgery: Past, present, and the future. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2021, 132, 523–531. [Google Scholar] [CrossRef] [PubMed]
- Al-Haj Husain, A.; Schönegg, D.; Bosshard, F.A.; Valdec, S. Bilateral supernumerary maxillary fourth and fifth molars: A clinical case report and literature review. Imaging Sci. Dent. 2022, 52, 429–434. [Google Scholar] [CrossRef]
- Nakamori, K.; Tomihara, K.; Noguchi, M. Clinical significance of computed tomography assessment for third molar surgery. World J. Radiol. 2014, 6, 417–423. [Google Scholar] [CrossRef]
- Susarla, S.M.; Dodson, T.B. Preoperative computed tomography imaging in the management of impacted mandibular third molars. J. Oral Maxillofac. Surg. 2007, 65, 83–88. [Google Scholar] [CrossRef]
- Xu, G.Z.; Yang, C.; Fan, X.D.; Yu, C.Q.; Cai, X.Y.; Wang, Y.; He, D. Anatomic relationship between impacted third mandibular molar and the mandibular canal as the risk factor of inferior alveolar nerve injury. Br. J. Oral Maxillofac. Surg. 2013, 51, e215–e219. [Google Scholar] [CrossRef] [PubMed]
- Tack, D.; Widelec, J.; De Maertelaer, V.; Bailly, J.M.; Delcour, C.; Gevenois, P.A. Comparison between low-dose and standard-dose multidetector CT in patients with suspected chronic sinusitis. AJR Am. J. Roentgenol. 2003, 181, 939–944. [Google Scholar] [CrossRef] [PubMed]
- Ohman, A.; Kull, L.; Andersson, J.; Flygare, L. Radiation doses in examination of lower third molars with computed tomography and conventional radiography. Dentomaxillofac. Radiol. 2008, 37, 445–452. [Google Scholar] [CrossRef] [PubMed]
- Kaeppler, G. Applications of cone beam computed tomography in dental and oral medicine. Int. J. Comput. Dent. 2010, 13, 203–219. [Google Scholar] [PubMed]
- Nasseh, I.; Al-Rawi, W. Cone Beam Computed Tomography. Dent. Clin. N. Am. 2018, 62, 361–391. [Google Scholar] [CrossRef] [PubMed]
- Ludlow, J.B.; Timothy, R.; Walker, C.; Hunter, R.; Benavides, E.; Samuelson, D.B.; Scheske, M.J. Effective dose of dental CBCT-a meta analysis of published data and additional data for nine CBCT units. Dentomaxillofac. Radiol. 2015, 44, 20140197. [Google Scholar] [CrossRef] [PubMed]
- Scarfe, W.C.; Farman, A.G.; Sukovic, P. Clinical applications of cone-beam computed tomography in dental practice. J. Can. Dent. Assoc. 2006, 72, 75–80. [Google Scholar]
- Leung, Y.Y.; Hung, K.F.; Li, D.T.S.; Yeung, A.W.K. Application of Cone Beam Computed Tomography in Risk Assessment of Lower Third Molar Surgery. Diagnostics 2023, 13, 919. [Google Scholar] [CrossRef]
- Ohman, A.; Kivijärvi, K.; Blombäck, U.; Flygare, L. Pre-operative radiographic evaluation of lower third molars with computed tomography. Dentomaxillofac. Radiol. 2006, 35, 30–35. [Google Scholar] [CrossRef]
- Lübbers, H.T.; Matthews, F.; Damerau, G.; Kruse, A.L.; Obwegeser, J.A.; Grätz, K.W.; Eyrich, G.K. Anatomy of impacted lower third molars evaluated by computerized tomography: Is there an indication for 3-dimensional imaging? Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2011, 111, 547–550. [Google Scholar] [CrossRef]
- de Toledo Telles-Araújo, G.; Peralta-Mamani, M.; Caminha, R.D.G.; de Fatima Moraes-da-Silva, A.; Rubira, C.M.F.; Honório, H.M.; Rubira-Bullen, I.R.F. CBCT does not reduce neurosensory disturbances after third molar removal compared to panoramic radiography: A systematic review and meta-analysis. Clin. Oral Investig. 2020, 24, 1137–1149. [Google Scholar] [CrossRef] [PubMed]
- García, A.G.; Sampedro, F.G.; Rey, J.G.; Vila, P.G.; Martin, M.S. Pell-Gregory classification is unreliable as a predictor of difficulty in extracting impacted lower third molars. Br. J. Oral Maxillofac. Surg. 2000, 38, 585–587. [Google Scholar] [CrossRef] [PubMed]
- Renton, T.; McGurk, M. Evaluation of factors predictive of lingual nerve injury in third molar surgery. Br. J. Oral Maxillofac. Surg. 2001, 39, 423–428. [Google Scholar] [CrossRef] [PubMed]
- Renton, T.; Smeeton, N.; McGurk, M. Factors predictive of difficulty of mandibular third molar surgery. Br. Dent. J. 2001, 190, 607–610. [Google Scholar] [CrossRef] [PubMed]
- Gbotolorun, O.M.; Arotiba, G.T.; Ladeinde, A.L. Assessment of factors associated with surgical difficulty in impacted mandibular third molar extraction. J. Oral Maxillofac. Surg. 2007, 65, 1977–1983. [Google Scholar] [CrossRef] [PubMed]
- Glera-Suárez, P.; Soto-Peñaloza, D.; Peñarrocha-Oltra, D.; Peñarrocha-Diago, M. Patient morbidity after impacted third molar extraction with different flap designs. A systematic review and meta-analysis. Med. Oral Patol. Oral Cir. Bucal 2020, 25, e233–e239. [Google Scholar] [CrossRef] [PubMed]
- Cosola, S.; Kim, Y.S.; Park, Y.M.; Giammarinaro, E.; Covani, U. Coronectomy of Mandibular Third Molar: Four Years of Follow-Up of 130 Cases. Medicina 2020, 56, 654. [Google Scholar] [CrossRef]
- Matzen, L.H.; Berkhout, E. Cone beam CT imaging of the mandibular third molar: A position paper prepared by the European Academy of DentoMaxilloFacial Radiology (EADMFR). Dentomaxillofac. Radiol. 2019, 48, 20190039. [Google Scholar] [CrossRef]
- Yeung, A.W.K.; Jacobs, R.; Bornstein, M.M. Novel low-dose protocols using cone beam computed tomography in dental medicine: A review focusing on indications, limitations, and future possibilities. Clin. Oral Investig. 2019, 23, 2573–2581. [Google Scholar] [CrossRef]
- Al-Haj Husain, A.; Döbelin, Q.; Giacomelli-Hiestand, B.; Wiedemeier, D.B.; Stadlinger, B.; Valdec, S. Diagnostic Accuracy of Cystic Lesions Using a Pre-Programmed Low-Dose and Standard-Dose Dental Cone-Beam Computed Tomography Protocol: An Ex Vivo Comparison Study. Sensors 2021, 21, 7402. [Google Scholar] [CrossRef]
- Ruetters, M.; Sen, S.; Gehrig, H.; Bruckner, T.; Kim, T.S.; Lux, C.J.; Schlemmer, H.P.; Heinze, S.; Maier, J.; Kachelrieß, M.; et al. Dental imaging using an ultra-high resolution photon-counting CT system. Sci. Rep. 2022, 12, 7125. [Google Scholar] [CrossRef] [PubMed]
- Rajendran, K.; Petersilka, M.; Henning, A.; Shanblatt, E.; Marsh, J.; Thorne, J.; Schmidt, B.; Flohr, T.; Fletcher, J.; McCollough, C.; et al. Full field-of-view, high-resolution, photon-counting detector CT: Technical assessment and initial patient experience. Phys. Med. Biol. 2021, 66, 205019. [Google Scholar] [CrossRef] [PubMed]
- Schlemmer, H.P. The Eye of the CT Scanner: The story of learning to see the invisible or from the fluorescent screen to the photon-counting detector. Rofo 2021, 193, 1034–1049. [Google Scholar] [CrossRef] [PubMed]
- Gahleitner, A.; Solar, P.; Nasel, C.; Homolka, P.; Youssefzadeh, S.; Ertl, L.; Schick, S. Magnetic resonance tomography in dental radiology (dental MRI). Radiologe 1999, 39, 1044–1050. [Google Scholar] [CrossRef] [PubMed]
- Miloro, M.; Halkias, L.E.; Slone, H.W.; Chakeres, D.W. Assessment of the lingual nerve in the third molar region using magnetic resonance imaging. J. Oral Maxillofac. Surg. 1997, 55, 134–137. [Google Scholar] [CrossRef] [PubMed]
- Al-Haj Husain, A.; Solomons, M.; Stadlinger, B.; Pejicic, R.; Winklhofer, S.; Piccirelli, M.; Valdec, S. Visualization of the Inferior Alveolar Nerve and Lingual Nerve Using MRI in Oral and Maxillofacial Surgery: A Systematic Review. Diagnostics 2021, 11, 1657. [Google Scholar] [CrossRef] [PubMed]
- Al-Haj Husain, A.; Stadlinger, B.; Winklhofer, S.; Müller, M.; Piccirelli, M.; Valdec, S. Mandibular Third Molar Surgery: Intraosseous Localization of the Inferior Alveolar Nerve Using 3D Double-Echo Steady-State MRI (3D-DESS). Diagnostics 2021, 11, 1245. [Google Scholar] [CrossRef] [PubMed]
- Fujii, H.; Fujita, A.; Yang, A.; Kanazawa, H.; Buch, K.; Sakai, O.; Sugimoto, H. Visualization of the Peripheral Branches of the Mandibular Division of the Trigeminal Nerve on 3D Double-Echo Steady-State with Water Excitation Sequence. AJNR Am. J. Neuroradiol. 2015, 36, 1333–1337. [Google Scholar] [CrossRef]
- Al-Haj Husain, A.; Valdec, S.; Stadlinger, B.; Rucker, M.; Piccirelli, M.; Winklhofer, S. Preoperative visualization of the lingual nerve by 3D double-echo steady-state MRI in surgical third molar extraction treatment. Clin. Oral Investig. 2022, 26, 2043–2053. [Google Scholar] [CrossRef]
- Valdec, S.; Al-Haj Husain, A.; Winklhofer, S.; Müller, M.; Piccirelli, M.; Stadlinger, B. Comparison of Preoperative Cone-Beam Computed Tomography and 3D-Double Echo Steady-State MRI in Third Molar Surgery. J. Clin. Med. 2021, 10, 4768. [Google Scholar] [CrossRef]
- Burian, E.; Probst, F.A.; Weidlich, D.; Cornelius, C.P.; Maier, L.; Robl, T.; Zimmer, C.; Karampinos, D.C.; Ritschl, L.M.; Probst, M. MRI of the inferior alveolar nerve and lingual nerve-anatomical variation and morphometric benchmark values of nerve diameters in healthy subjects. Clin. Oral Investig. 2020, 24, 2625–2634. [Google Scholar] [CrossRef] [PubMed]
- Du, J.; Bydder, G.M. Qualitative and quantitative ultrashort-TE MRI of cortical bone. NMR Biomed. 2013, 26, 489–506. [Google Scholar] [CrossRef] [PubMed]
- Stumpf, K.; Kaye, E.; Paul, J.; Wundrak, S.; Pauly, J.M.; Rasche, V. Two-dimensional UTE overview imaging for dental application. Magn. Reson. Med. 2020, 84, 2616–2624. [Google Scholar] [CrossRef] [PubMed]
- Al-Haj Husain, A.; Schmidt, V.; Valdec, S.; Stadlinger, B.; Winklhofer, S.; Schönegg, D.; Sommer, S.; Özcan, M.; Al-Haj Husain, N.; Piccirelli, M. MR-orthopantomography in operative dentistry and oral and maxillofacial surgery: A proof of concept study. Sci. Rep. 2023, 13, 6228. [Google Scholar] [CrossRef] [PubMed]
- Gray, C.F.; Redpath, T.W.; Smith, F.W.; Staff, R.T. Advanced imaging: Magnetic resonance imaging in implant dentistry. Clin. Oral Implants Res. 2003, 14, 18–27. [Google Scholar] [CrossRef] [PubMed]
- Ludwig, U.; Eisenbeiss, A.K.; Scheifele, C.; Nelson, K.; Bock, M.; Hennig, J.; von Elverfeldt, D.; Herdt, O.; Flügge, T.; Hövener, J.B. Dental MRI using wireless intraoral coils. Sci. Rep. 2016, 6, 23301. [Google Scholar] [CrossRef] [PubMed]
- Prager, M.; Heiland, S.; Gareis, D.; Hilgenfeld, T.; Bendszus, M.; Gaudino, C. Dental MRI using a dedicated RF-coil at 3 Tesla. J. Craniomaxillofac Surg. 2015, 43, 2175–2182. [Google Scholar] [CrossRef]
- Al-Haj Husain, A.; Sekerci, E.; Schönegg, D.; Bosshard, F.A.; Stadlinger, B.; Winklhofer, S.; Piccirelli, M.; Valdec, S. Dental MRI of Oral Soft-Tissue Tumors-Optimized Use of Black Bone MRI Sequences and a 15-Channel Mandibular Coil. J. Imaging 2022, 8, 146. [Google Scholar] [CrossRef]
- Sedaghatfar, M.; August, M.A.; Dodson, T.B. Panoramic radiographic findings as predictors of inferior alveolar nerve exposure following third molar extraction. J. Oral Maxillofac. Surg. 2005, 63, 3–7. [Google Scholar] [CrossRef]
- Choi, E.; Lee, S.; Jeong, E.; Shin, S.; Park, H.; Youm, S.; Son, Y.; Pang, K. Artificial intelligence in positioning between mandibular third molar and inferior alveolar nerve on panoramic radiography. Sci. Rep. 2022, 12, 2456. [Google Scholar] [CrossRef]
- Lo Casto, A.; Spartivento, G.; Benfante, V.; Di Raimondo, R.; Ali, M.; Di Raimondo, D.; Tuttolomondo, A.; Stefano, A.; Yezzi, A.; Comelli, A. Artificial Intelligence for Classifying the Relationship between Impacted Third Molar and Mandibular Canal on Panoramic Radiographs. Life 2023, 13, 1441. [Google Scholar] [CrossRef] [PubMed]
- Kempers, S.; van Lierop, P.; Hsu, T.H.; Moin, D.A.; Bergé, S.; Ghaeminia, H.; Xi, T.; Vinayahalingam, S. Positional assessment of lower third molar and mandibular canal using explainable artificial intelligence. J. Dent. 2023, 133, 104519. [Google Scholar] [CrossRef] [PubMed]
- Zhu, T.; Chen, D.; Wu, F.; Zhu, F.; Zhu, H. Artificial Intelligence Model to Detect Real Contact Relationship between Mandibular Third Molars and Inferior Alveolar Nerve Based on Panoramic Radiographs. Diagnostics 2021, 11, 1664. [Google Scholar] [CrossRef] [PubMed]
- Sukegawa, S.; Tanaka, F.; Hara, T.; Yoshii, K.; Yamashita, K.; Nakano, K.; Takabatake, K.; Kawai, H.; Nagatsuka, H.; Furuki, Y. Deep learning model for analyzing the relationship between mandibular third molar and inferior alveolar nerve in panoramic radiography. Sci. Rep. 2022, 12, 16925. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, J.S.; Lotz, M.; Rubi, L.; Unger, S.; Pfister, T.; Buhmann, J.M.; Stadlinger, B. Preinterventional Third-Molar Assessment Using Robust Machine Learning. J. Dent. Res. 2023, 102, 1452–1459. [Google Scholar] [CrossRef] [PubMed]
- Vranckx, M.; Van Gerven, A.; Willems, H.; Vandemeulebroucke, A.; Ferreira Leite, A.; Politis, C.; Jacobs, R. Artificial Intelligence (AI)-Driven Molar Angulation Measurements to Predict Third Molar Eruption on Panoramic Radiographs. Int. J. Environ. Res. Public Health 2020, 17, 3716. [Google Scholar] [CrossRef] [PubMed]
- Yoo, J.H.; Yeom, H.G.; Shin, W.; Yun, J.P.; Lee, J.H.; Jeong, S.H.; Lim, H.J.; Lee, J.; Kim, B.C. Deep learning based prediction of extraction difficulty for mandibular third molars. Sci. Rep. 2021, 11, 1954. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Li, J.; Li, Z.B.; Li, Z. Predicting postoperative facial swelling following impacted mandibular third molars extraction by using artificial neural networks evaluation. Sci. Rep. 2018, 8, 12281. [Google Scholar] [CrossRef]
- Rasteau, S.; Ernenwein, D.; Savoldelli, C.; Bouletreau, P. Artificial intelligence for oral and maxillo-facial surgery: A narrative review. J. Stomatol. Oral Maxillofac. Surg. 2022, 123, 276–282. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Haj Husain, A.; Stadlinger, B.; Winklhofer, S.; Bosshard, F.A.; Schmidt, V.; Valdec, S. Imaging in Third Molar Surgery: A Clinical Update. J. Clin. Med. 2023, 12, 7688. https://doi.org/10.3390/jcm12247688
Al-Haj Husain A, Stadlinger B, Winklhofer S, Bosshard FA, Schmidt V, Valdec S. Imaging in Third Molar Surgery: A Clinical Update. Journal of Clinical Medicine. 2023; 12(24):7688. https://doi.org/10.3390/jcm12247688
Chicago/Turabian StyleAl-Haj Husain, Adib, Bernd Stadlinger, Sebastian Winklhofer, Fabienne A. Bosshard, Valérie Schmidt, and Silvio Valdec. 2023. "Imaging in Third Molar Surgery: A Clinical Update" Journal of Clinical Medicine 12, no. 24: 7688. https://doi.org/10.3390/jcm12247688
APA StyleAl-Haj Husain, A., Stadlinger, B., Winklhofer, S., Bosshard, F. A., Schmidt, V., & Valdec, S. (2023). Imaging in Third Molar Surgery: A Clinical Update. Journal of Clinical Medicine, 12(24), 7688. https://doi.org/10.3390/jcm12247688





