Chronic Stress in Pregnancy Is Associated with Low Birth Weight: A Meta-Analysis
Abstract
:1. Introduction
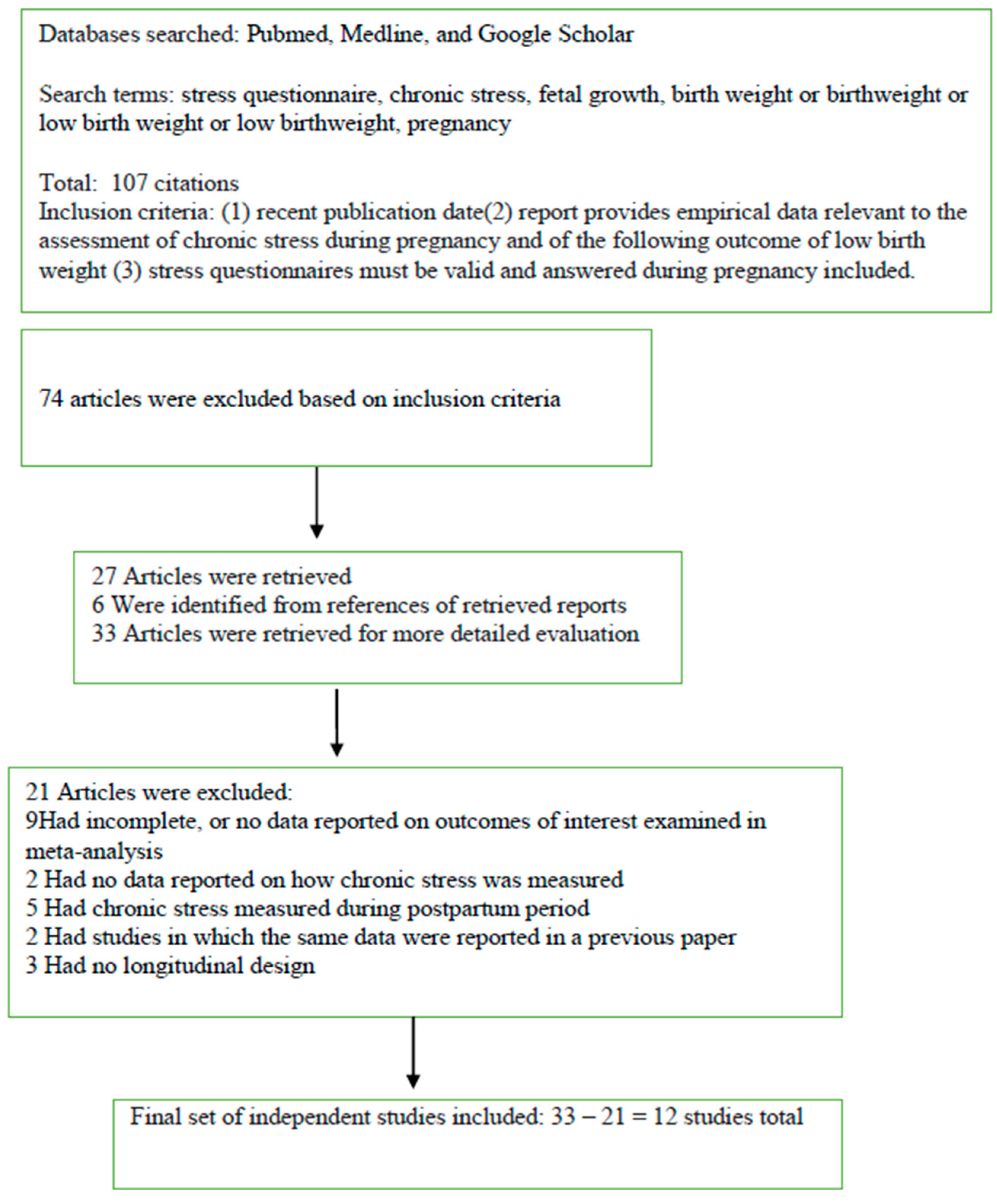
2. Materials and Methods
3. Results
4. Discussion and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Latendresse, G. The interaction between chronic stress and pregnancy: Preterm birth from a biobehavioral perspective. J. Midwifery Women’s Health 2009, 54, 8–17. [Google Scholar] [CrossRef]
- Cohen, S.; Kessler, R.C.; Gordon, L.U. Measuring Stress: A Guide for Health and Social Scientists; Oxford University Press: New York, NY, USA, 1995. [Google Scholar]
- Lazarus, R.S. From psychological stress to the emotions: A history of changing outlooks. Annu. Rev. Psychol. 1993, 44, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Aschbacher, K.; Kornfeld, S.; Picard, M.; Puterman, E.; Havel, P.; Stanhope, K.; Lustig, R.; Epel, E. Chronic stress increase vulnerabilityto diet related abdominal fat, oxidative stress and metabolic risk. Psychoneuroendocrinology 2014, 46, 14–22. [Google Scholar] [CrossRef] [PubMed]
- Katsuhara, S.; Yokkomoto-Umakoshi, M.; Matsuda, Y.; Iwahashi, N.; Kaneko, H.; Ogata, M.; Fukumoto, T.; Terada, E.; Sakamoto, R.; Ogawa, Y. Impact of cortisol on reduction in muscle strength and mass: A Mendelian Randomization Study. J. Clin. Endocrinol. Metab. 2022, 107, 1477–1487. [Google Scholar] [CrossRef]
- Tsigos, C.; Chrousos, G.P. Hypothalamic-pituitary-adrenal axis, neuroendocrine factors and stress. J. Psychosom. Res. 2002, 53, 865–871. [Google Scholar] [CrossRef] [PubMed]
- Kelly, R.H.; Russo, J.; Holt, V.L.; Danielsen, B.H.; Zatzick, D.F.; Walker, E.; Katon, W. Psychiatric and substance use disorders as risk factors for low birth weight and preterm delivery. Obs. Gynecol. 2002, 100, 297–304. [Google Scholar] [CrossRef]
- Kalil, K.M.; Gruber, J.E.; Conley, J.G.; LaGrandeur, R.M. Relationships among Stress, Anxiety, Type A, and Pregnancy-Related Complications. J. Prenat. Perinat. Psychol. Health 1995, 9, 221. [Google Scholar]
- Bussières, E.-L.; Tarabulsy, G.M.; Pearson, J.; Tessier, R.; Forest, J.-C.; Giguère, Y. Maternal prenatal stress and infant birth weight and gestational age: A meta-analysis of prospective studies. Dev. Rev. 2015, 36, 179–199. [Google Scholar] [CrossRef]
- Szegda, K.; Bertone-Johnson, E.R.; Pekow, P.; Powers, S.; Markenson, G.; Dole, N.; Chasan-Taber, L. Prenatal Perceived Stress and Adverse Birth Outcomes Among Puerto Rican Women. J. Womens Health 2018, 27, 699–708. [Google Scholar] [CrossRef]
- Andersson, N.W.; Li, Q.; Mills, C.W.; Ly, J.; Nomura, Y.; Chen, J. Influence of prenatal maternal stress on umbilical cord blood cytokine levels. Arch. Women’s Ment Health 2016, 19, 761–767. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B. Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA 1999, 282, 1737–1744. [Google Scholar] [CrossRef] [PubMed]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Radloff, L.S. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Ware, J.E., Jr. SF-36 health survey update. Spine 2000, 25, 3130–3139. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A Global Measure of Perceived Stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef]
- Cox, J.L.; Holden, J.M.; Sagovsky, R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br. J. Psychiatry 1987, 150, 782–786. [Google Scholar] [CrossRef]
- Spielberger, C.D.; Gonzalez-Reigosa, F.; Martinez-Urrutia, A.; Natalicio, L.F.; Natalicio, D.S. The state-trait anxiety inventory. Rev. Interam. De Psicol. Interam. J. Psychol. 1971, 5, 22–27. [Google Scholar]
- Goldberg, D.P.; Hillier, V.F. A scaled version of the General Health Questionnaire. Psychol. Med. 1979, 9, 139–145. [Google Scholar] [CrossRef]
- Beck, A.T.; Ward, C.H.; Mendelson, M.; Mock, J.; Erbaugh, J. An inventory for measuring depression. Arch. Gen. Psychiatry 1961, 4, 561–571. [Google Scholar] [CrossRef]
- Derogatis, L.R.; Melisaratos, N. The Brief Symptom Inventory: An introductory report. Psychol. Med. 1983, 13, 595–605. [Google Scholar] [CrossRef]
- Mathews, T.J.; Menacker, F.; MacDorman, M.F. Infant mortality statistics from the 2002 period: Linked birth/infant death data set. Natl. Vital. Stat. Rep. 2004, 53, 1–29. [Google Scholar]
- Lau, Y. The effect of maternal stress and health-related quality of life on birth outcomes among Macao Chinese pregnant women. J. Perinat. Neonatal. Nurs. 2013, 27, 14–24. [Google Scholar] [CrossRef] [PubMed]
- Rondó, P.H.; Ferreira, R.F.; Nogueira, F.; Ribeiro, M.C.; Lobert, H.; Artes, R. Maternal psychological stress and distress as predictors of low birth weight, prematurity and intrauterine growth retardation. Eur. J. Clin. Nutr. 2003, 57, 266–272. [Google Scholar] [CrossRef] [PubMed]
- Evans, J.; Heron, J.; Patel, R.R.; Wiles, N. Depressive symptoms during pregnancy and low birth weight at term: Longitudinal study. Br. J. Psychiatry 2007, 191, 84–85. [Google Scholar] [CrossRef] [PubMed]
- Berle, J.; Mykletun, A.; Daltveit, A.K.; Rasmussen, S.; Holsten, F.; Dahl, A.A. Neonatal outcomes in offspring of women with anxiety and depression during pregnancy. A linkage study from The Nord-Trøndelag Health Study (HUNT) and Medical Birth Registry of Norway. Arch. Women’s Ment. Health 2005, 8, 181–189. [Google Scholar] [CrossRef]
- Krabbendam, L.; Smits, L.; de Bie, R.; Bastiaanssen, J.; Stelma, F.; van Os, J. The impact of maternal stress on pregnancy outcome in a well-educated Caucasian population. Paediatr. Perinat. Epidemiol. 2005, 19, 421–425. [Google Scholar] [CrossRef] [PubMed]
- Borders, A.E.; Grobman, W.A.; Amsden, L.B.; Holl, J.L. Chronic stress and low birth weight neonates in a low-income population of women. Obs. Gynecol 2007, 109, 331–338. [Google Scholar] [CrossRef]
- Steer, R.A.; Scholl, T.O.; Hediger, M.L.; Fischer, R.L. Self-reported depression and negative pregnancy outcomes. J. Clin. Epidemiol. 1992, 45, 1093–1099. [Google Scholar] [CrossRef] [PubMed]
- Henrichs, J.; Schenk, J.J.; Roza, S.J.; van den Berg, M.P.; Schmidt, H.G.; Steegers, E.A.; Hofman, A.; Jaddoe, V.W.; Verhulst, F.C.; Tiemeier, H. Maternal psychological distress and fetal growth trajectories: The Generation R Study. Psychol. Med. 2010, 40, 633–643. [Google Scholar] [CrossRef]
- Broekman, B.F.; Chan, Y.H.; Chong, Y.S.; Kwek, K.; Cohen, S.S.; Haley, C.L.; Chen, H.; Chee, C.; Rifkin-Graboi, A.; Gluckman, P.D.; et al. The influence of anxiety and depressive symptoms during pregnancy on birth size. Paediatr. Perinat. Epidemiol. 2014, 28, 116–126. [Google Scholar] [CrossRef]
- Dancause, K.N.; Laplante, D.P.; Oremus, C.; Fraser, S.; Brunet, A.; King, S. Disaster-related prenatal maternal stress influences birth outcomes: Project Ice Storm. Early Hum. Dev. 2011, 87, 813–820. [Google Scholar] [CrossRef] [PubMed]
- Pritchard, C.W.; Teo, P.Y. Preterm birth, low birthweight and the stressfulness of the household role for pregnant women. Soc. Sci. Med. 1994, 38, 89–96. [Google Scholar] [CrossRef] [PubMed]
- Glynn, L.; Schetter, C. Stress in pregnancy: Empirical evidence and theoretical issues to guide interdisciplinary research. Handb. Stress Sci. Biol. Psychol. Health 2010, 321–343. [Google Scholar] [CrossRef]
- Mancuso, R.A.; Schetter, C.D.; Rini, C.M.; Roesch, S.C.; Hobel, C.J. Maternal prenatal anxiety and corticotropin-releasing hormone associated with timing of delivery. Psychosom. Med. 2004, 66, 762–769. [Google Scholar] [CrossRef] [PubMed]
- Huizink, A.C.; Mulder, E.J.; Robles de Medina, P.G.; Visser, G.H.; Buitelaar, J.K. Is pregnancy anxiety a distinctive syndrome? Early Hum. Dev. 2004, 79, 81–91. [Google Scholar] [CrossRef]
- Magyar, D.M.; Fridshal, D.; Elsner, C.W.; Glatz, T.; Eliot, J.; Klein, A.H.; Lowe, K.C.; Buster, J.E.; Nathanielsz, P.W. Time-trend analysis of plasma cortisol concentrations in the fetal sheep in relation to parturition. Endocrinology 1980, 107, 155–159. [Google Scholar] [CrossRef]
- Chapman, K.; Holmes, M.; Seckl, J. 11β-hydroxysteroid dehydrogenases: Intracellular gate-keepers of tissue glucocorticoid action. Physiol. Rev. 2013, 93, 1139–1206. [Google Scholar] [CrossRef]
- Schlotz, W.; Schulz, P.; Hellhammer, J.; Stone, A.A.; Hellhammer, D.H. Trait anxiety moderates the impact of performance pressure on salivary cortisol in everyday life. Psychoneuroendocrinology 2006, 31, 459–472. [Google Scholar] [CrossRef]
| Name of Scale | Description of Scale |
|---|---|
| Primary Care Evaluation of Mental Disorders (PRIME-MD) [12] | A 2-stage system: the patient first completes a 26-item self-administered questionnaire that screens for 5 of the most common groups of disorders in primary care: anxiety depressive, somatoform, alcohol and eating disorders. |
| Hospital Anxiety and Depression Rating Scale (HADS) [13] | A total of 14 items developed for the hospital setting: 7 items for symptoms of depression (HADS-D) and 7 items for symptoms of anxiety (HADS-A) experienced during the previous 7 days. |
| Center for Epidemiological Studies Depression Scale (CES-D) [14] | A total of 20 items which measure symptoms of depression and their frequencies in the past week in the general population; cutoff for depression is a score of 16. |
| SF-36 Health Survey [15] | Indicates the health status of populations, helps with service planning and measures the impact of clinical and social interventions. |
| Perceived Stress Scale (PSS) [16] | A total of 14 items measure the degree to which lives are unpredictable, uncontrollable, and overloading in the last 30 days. |
| Edinburgh Postnatal Depression Scale (EPDS) [17] | A total of 10 items initially developed for measuring the severity of postpartum depression symptoms, which have been validated for use in non-postpartum women. |
| State—Trait Anxiety Inventories, (STAI) [18] | The 20-item scale measures state or transitory anxiety experienced at that moment only and the other 20-item scale measures trait anxiety, or propensity towards anxiety based on personality. |
| General Health Questionnaire (GHQ) [19] | Screening tool for detecting psychiatric illness through items regarding disruptions in performing daily activities and feelings of subjective distress; 12-, 28-, 30-, and 60-item versions. |
| Beck Depression Inventory (BDI) [20] | A total of 21 items that measure the severity of behavioral manifestations of depression, including mood, pessimism, sense of failure, lack of satisfaction, guilt, self-dislike, punishment, self- accusation, crying, irritability, suicidal ideation social withdrawal, indecisiveness, body image, work, sleep disturbance, fatigue, loss of appetite, weight loss, somatic symptoms, and libido. |
| Brief Symptom Inventory (BSI) [21] | A self-report questionnaire with 53 items that assesses anxious and depressive symptoms. These items define a spectrum of psychiatric symptoms in the preceding seven days. |
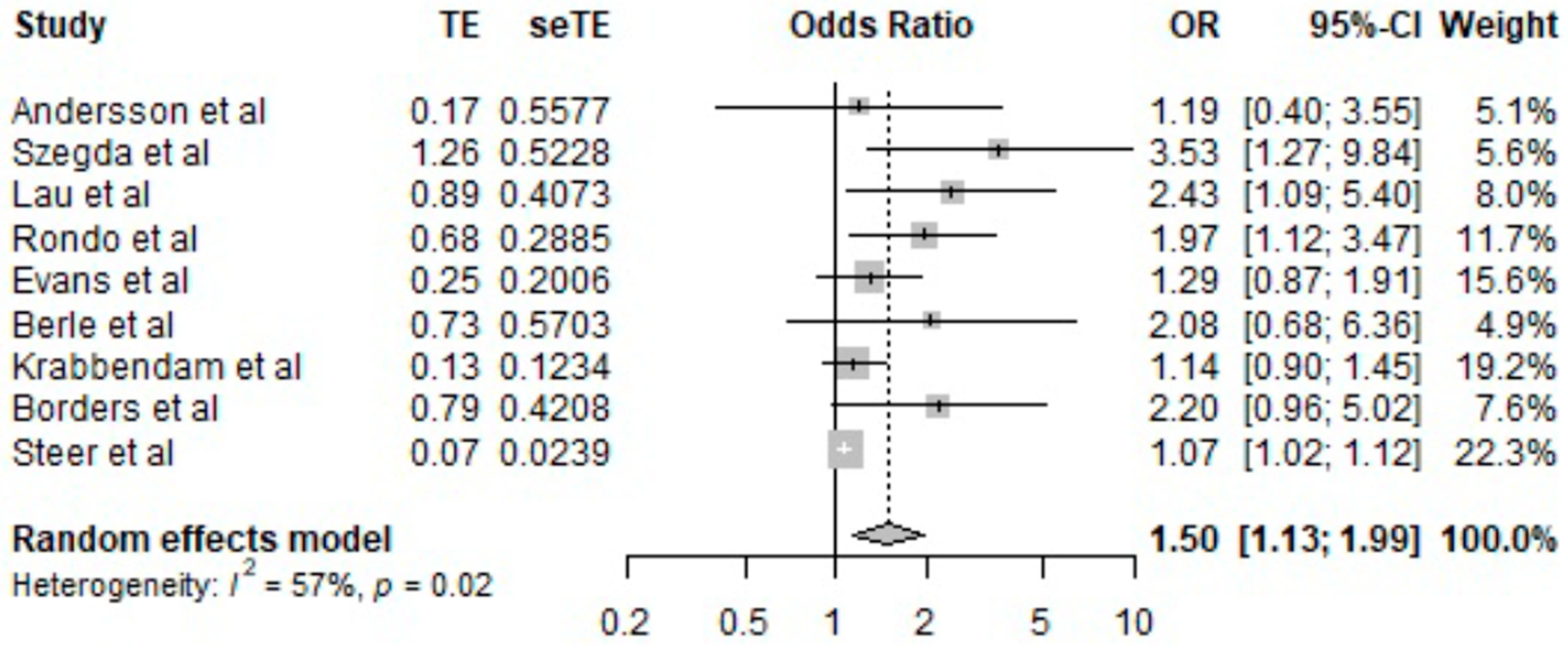
| Source | Sample Size | Questionnaire | OR (95% CI) |
|---|---|---|---|
| [11] | 1465 | PRIME-MD | 1.19 (0.40, 3.55) |
| [10] | 1267 | PSS | 3.53 (1.27, 9.84) |
| [23] | 581 | PSS | 2.43 (1.09, 5.40) |
| [24] | 865 | GHQ | 1.97 (1.12, 3.47) |
| [25] | 10,967 | EPDS | 1.29 (0.87, 1.91) |
| [26] | 680 | HADS | 2.08 (0.68, 6.36) |
| [27] | 5511 | PSS | 1.14 (0.90, 1.45) |
| [28] | 294 | CES-D | 2.20 (0.96, 5.02) |
| [29] | 712 | BDI | 1.07 (1.02, 1.12) |
| [11] | 1465 | PRIME-MD | 1.19 (0.40, 3.55) |
| [10] | 1267 | PSS | 3.53 (1.27, 9.84) |
| [23] | 581 | PSS | 2.43 (1.09, 5.40) |
| [24] | 865 | GHQ | 1.97 (1.12, 3.47) |
| [25] | 10,967 | EPDS | 1.29 (0.87, 1.91) |
| [26] | 680 | HADS | 2.08 (0.68, 6.36) |
| Source | Sample Size | Questionnaire | OR (95% CI) |
|---|---|---|---|
| [30] | 6313 | BSI | −22.42 (−53.05; 8.21) |
| [31] | 946 | BDI | −3.30 (−31.30; 24.70) |
| [32] | 172 | GHQ | 4.57 (2.99; 12.13) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Matsas, A.; Panopoulou, P.; Antoniou, N.; Bargiota, A.; Gryparis, A.; Vrachnis, N.; Mastorakos, G.; Kalantaridou, S.N.; Panoskaltsis, T.; Vlahos, N.F.; et al. Chronic Stress in Pregnancy Is Associated with Low Birth Weight: A Meta-Analysis. J. Clin. Med. 2023, 12, 7686. https://doi.org/10.3390/jcm12247686
Matsas A, Panopoulou P, Antoniou N, Bargiota A, Gryparis A, Vrachnis N, Mastorakos G, Kalantaridou SN, Panoskaltsis T, Vlahos NF, et al. Chronic Stress in Pregnancy Is Associated with Low Birth Weight: A Meta-Analysis. Journal of Clinical Medicine. 2023; 12(24):7686. https://doi.org/10.3390/jcm12247686
Chicago/Turabian StyleMatsas, Alkis, Panagiota Panopoulou, Neofyta Antoniou, Alexandra Bargiota, Alexandros Gryparis, Nikolaos Vrachnis, George Mastorakos, Sophia N. Kalantaridou, Theodoros Panoskaltsis, Nikos F. Vlahos, and et al. 2023. "Chronic Stress in Pregnancy Is Associated with Low Birth Weight: A Meta-Analysis" Journal of Clinical Medicine 12, no. 24: 7686. https://doi.org/10.3390/jcm12247686
APA StyleMatsas, A., Panopoulou, P., Antoniou, N., Bargiota, A., Gryparis, A., Vrachnis, N., Mastorakos, G., Kalantaridou, S. N., Panoskaltsis, T., Vlahos, N. F., & Valsamakis, G. (2023). Chronic Stress in Pregnancy Is Associated with Low Birth Weight: A Meta-Analysis. Journal of Clinical Medicine, 12(24), 7686. https://doi.org/10.3390/jcm12247686