The Outcome of under 10 mm Single-Incision Surgery Using a Non-Specialized Volar Plate in Distal Radius Fractures: A Retrospective Comparative Study
Abstract
:1. Introduction
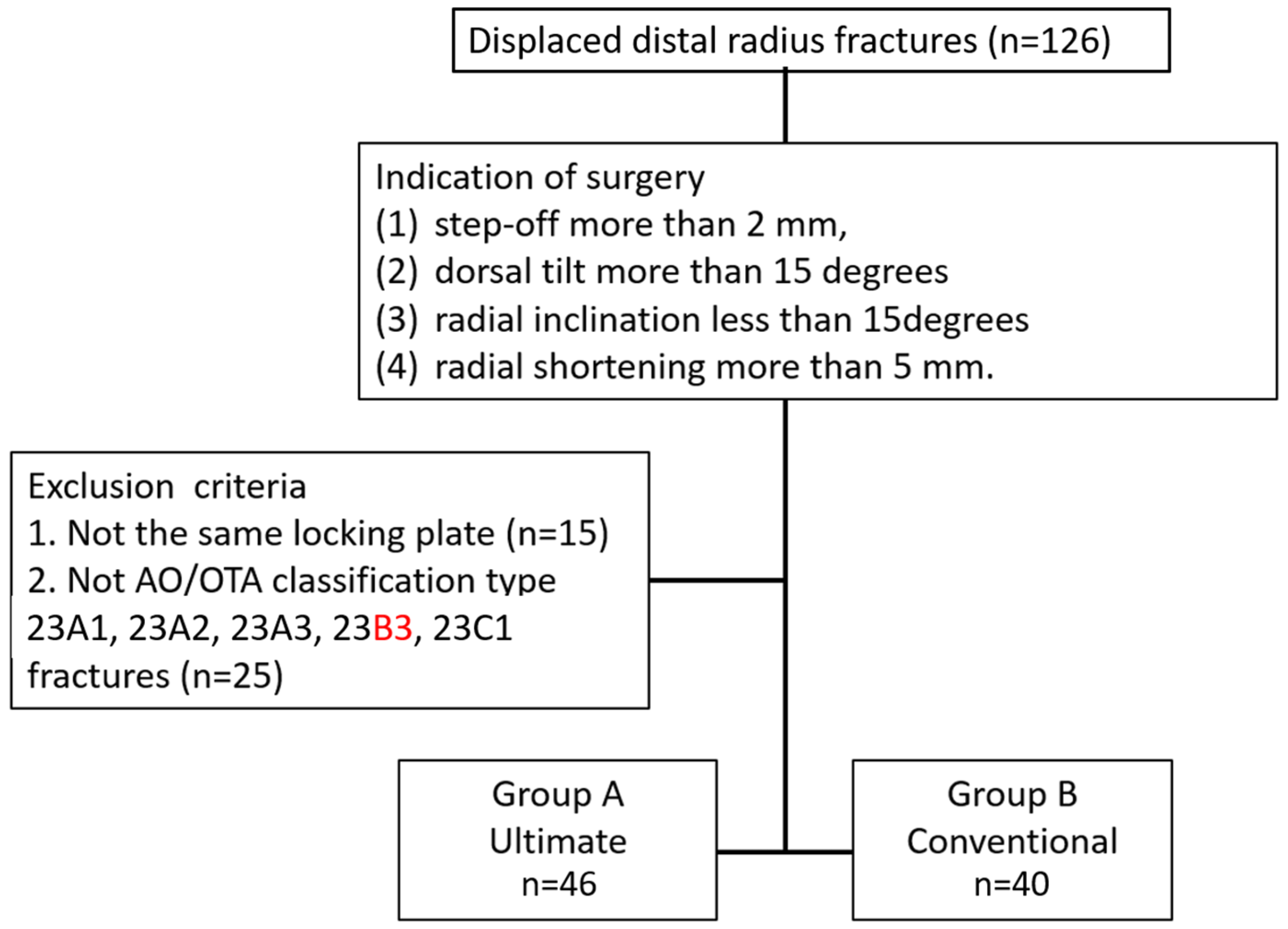
2. Materials and Methods
2.1. Patients
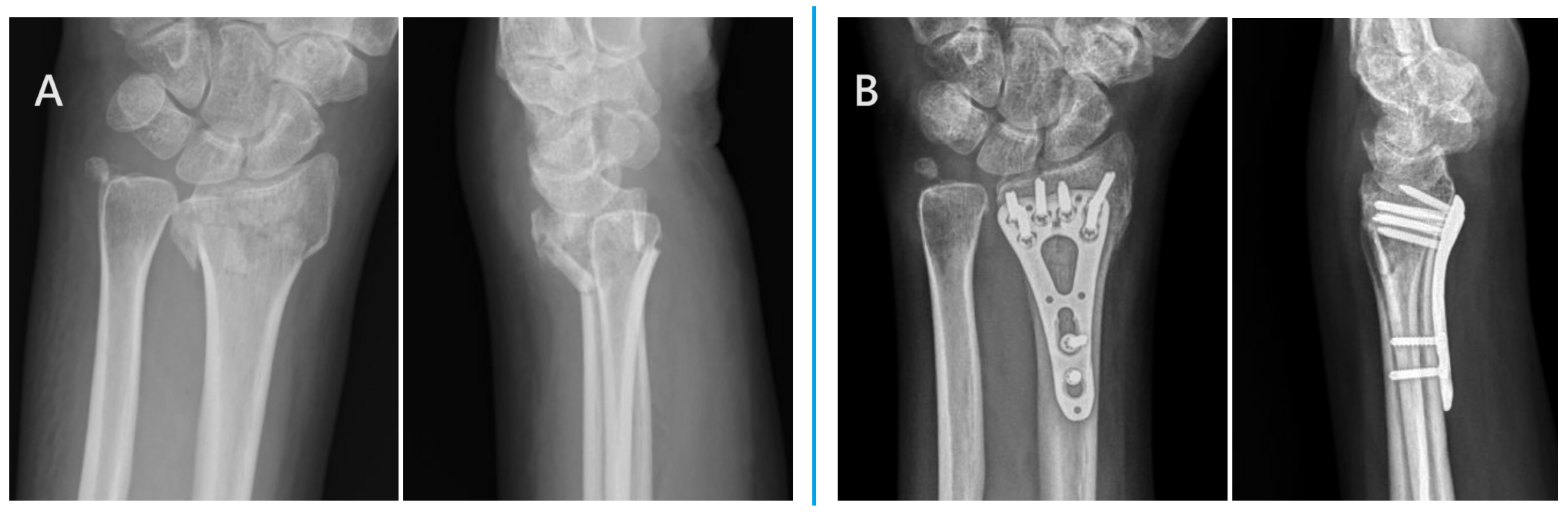
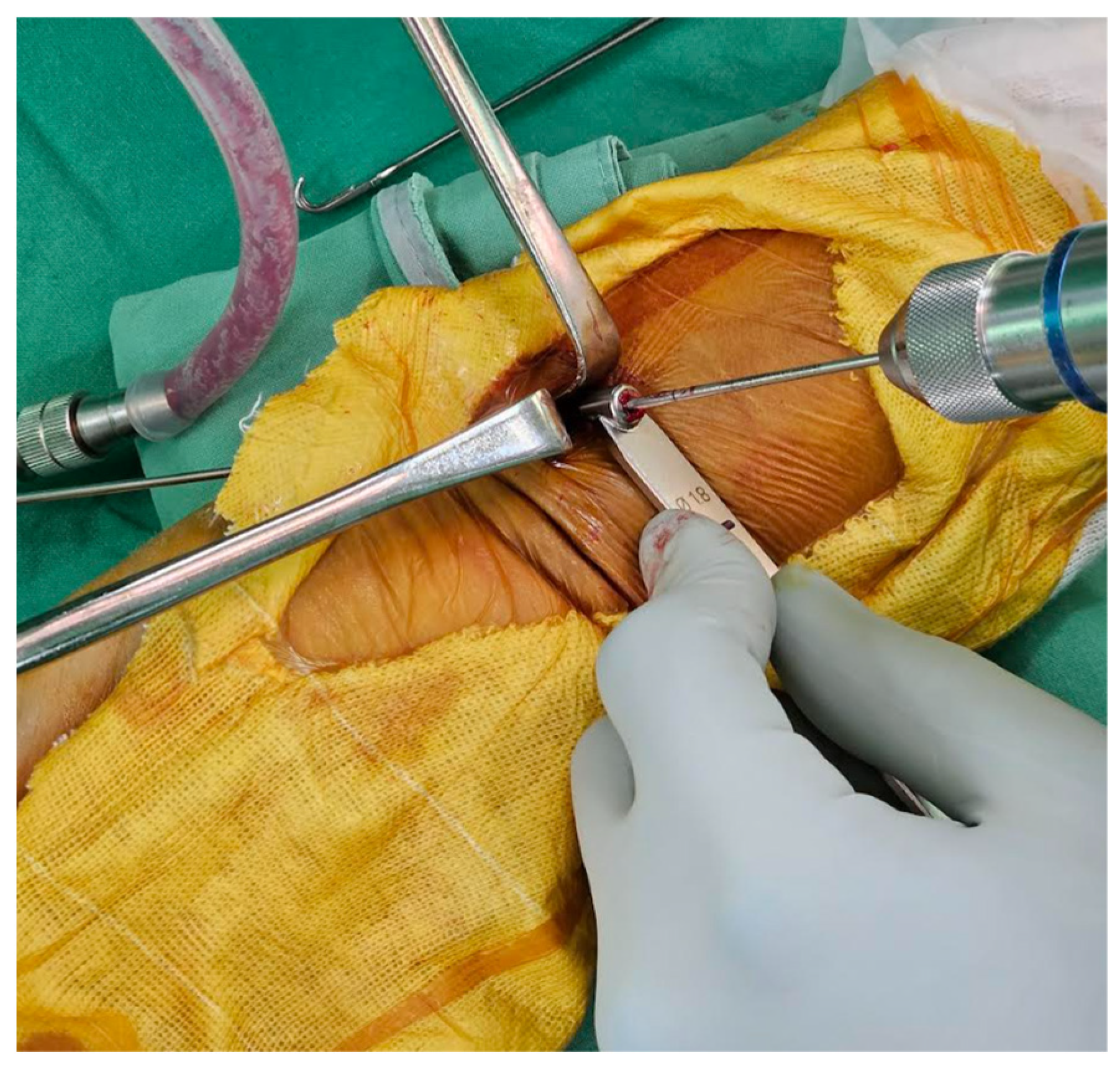
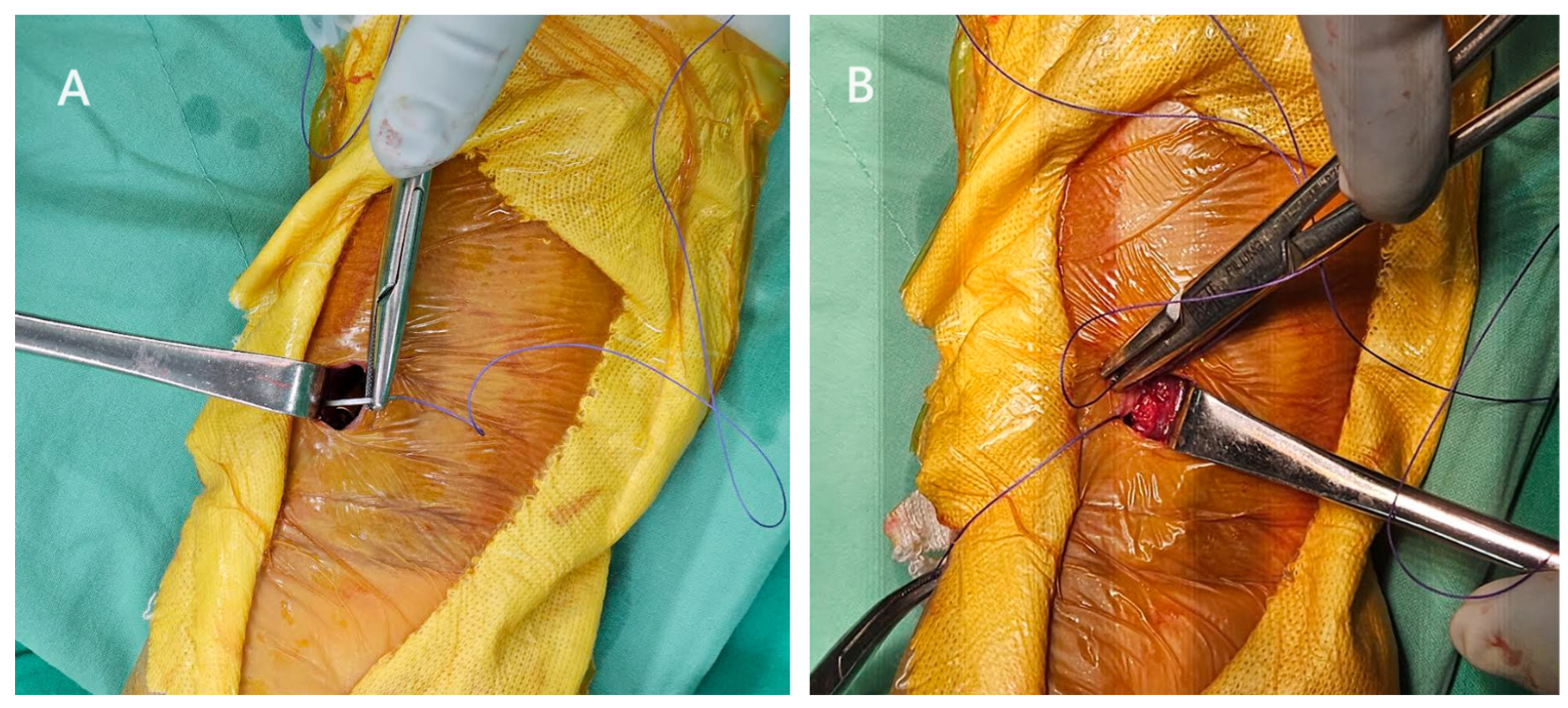
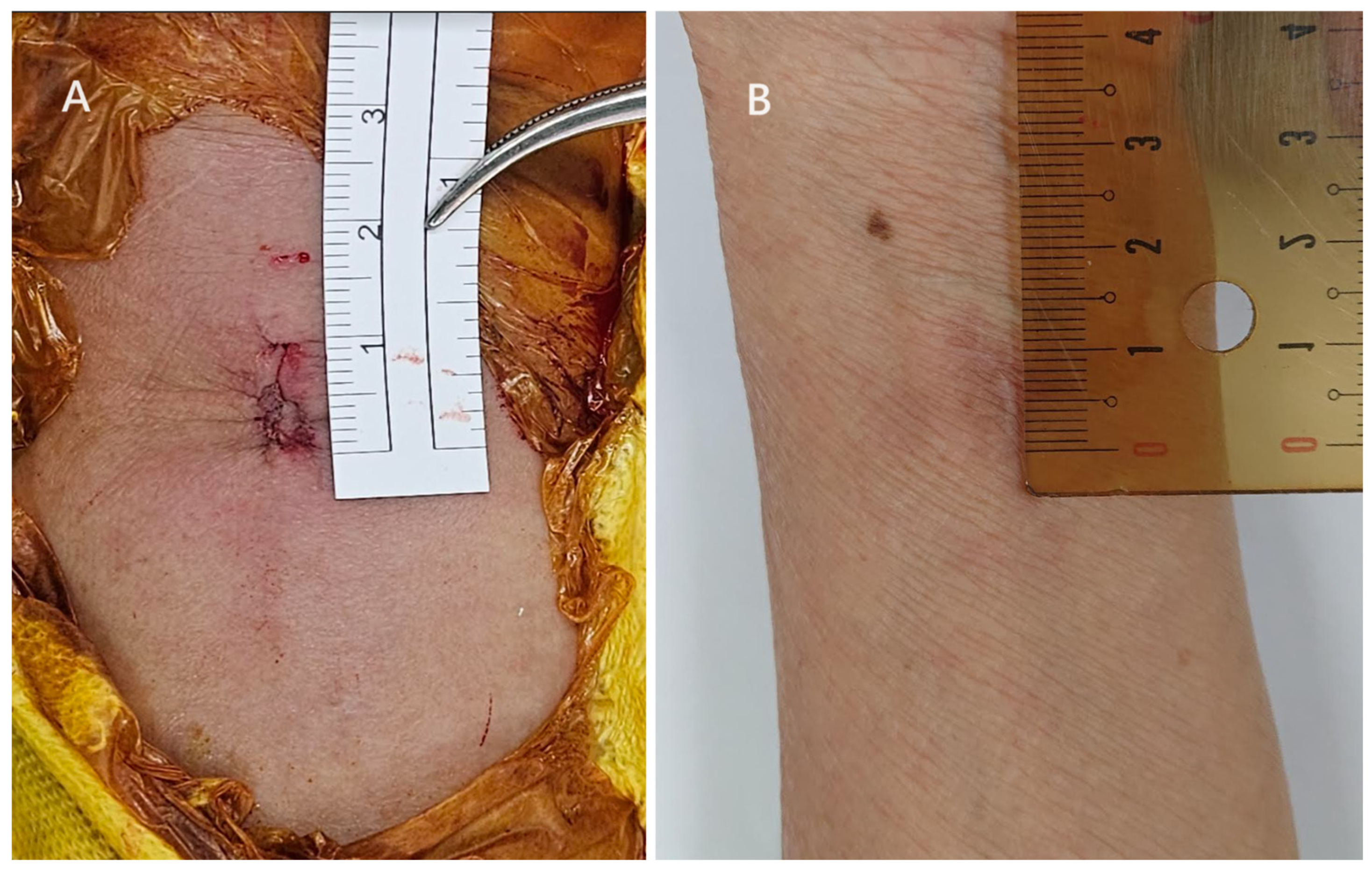
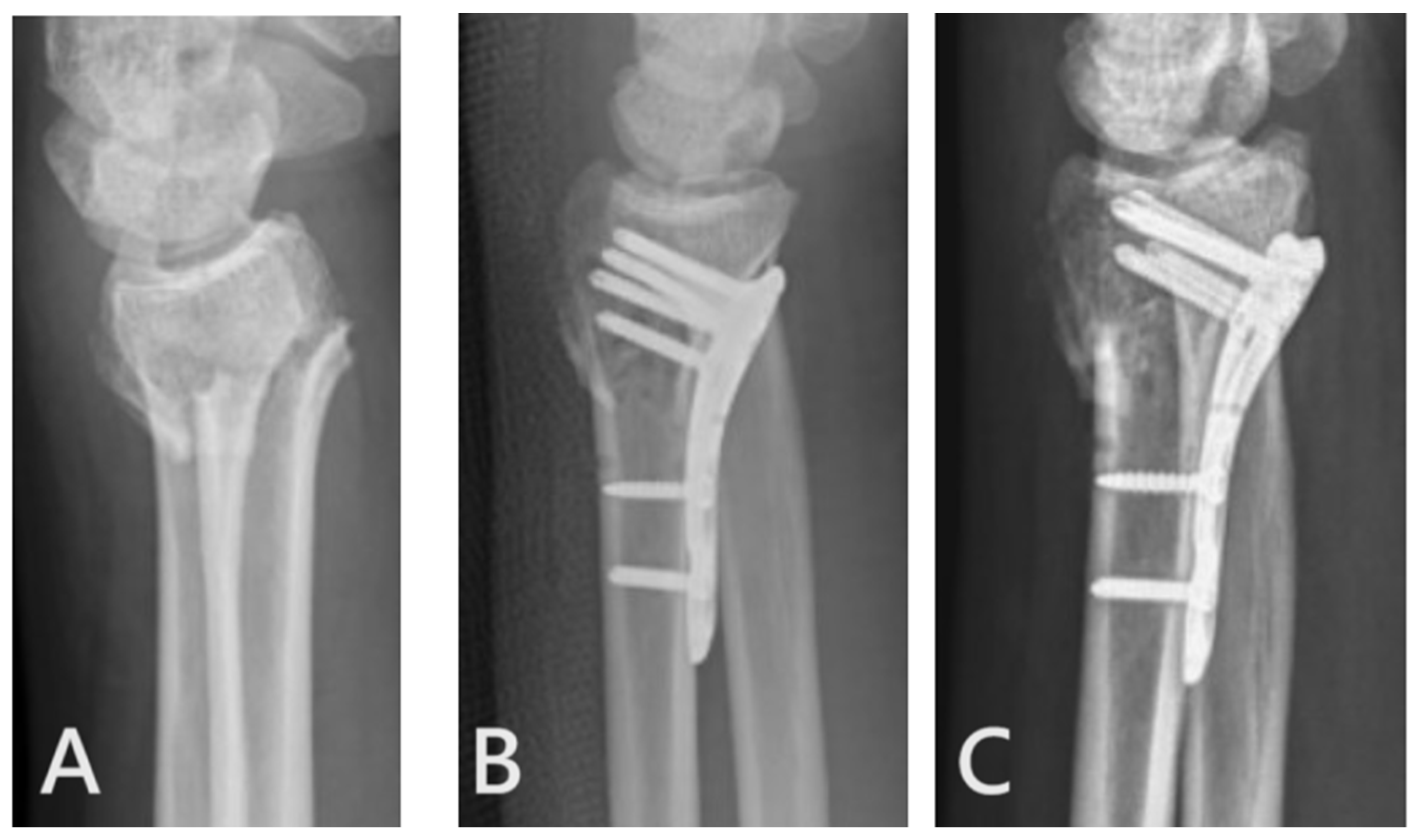
2.2. Surgical Techniques of Ultimate Incision Surgery
2.3. Surgical Techniques of Conventional Incision Surgery
2.4. Outcome Evaluations
2.5. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Radiographic Outcome
3.3. Clinical Outcome
3.4. Complications
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Patel, D.; Kamal, R. Enhanced Approaches to the Treatment of Distal Radius Fractures. Hand Clin. 2023, 39, 515–521. [Google Scholar] [CrossRef] [PubMed]
- van Delft, E.A.K.; van Bruggen, S.G.J.; van Stralen, K.J.; Bloemers, F.W.; Sosef, N.L.; Schep, N.W.L.; Vermeulen, J. Four weeks versus six weeks of immobilization in a cast following closed reduction for displaced distal radial fractures in adult patients: A multicentre randomized controlled trial. Bone Jt. J. 2023, 105, 993–999. [Google Scholar] [CrossRef] [PubMed]
- Yang, Q.; Cai, G.; Liu, J.; Wang, X.; Zhu, D. Efficacy of cast immobilization versus surgical treatment for distal radius fractures in adults: A systematic review and meta-analysis. Osteoporos. Int. 2023, 34, 659–669. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.T.; Chou, S.H.; Huang, H.T.; Fu, Y.C.; Jupiter, J.B.; Liu, W.C. Comparison of distal radius fracture plating surgery under wide-awake local anesthesia no tourniquet technique and balanced anesthesia: A retrospective cohort study. J. Orthop. Surg. Res. 2023, 18, 746. [Google Scholar] [CrossRef] [PubMed]
- Joo, P.Y.; Halperin, S.J.; Dhodapkar, M.M.; Adeclat, G.J.; Elaydi, A.; Wilhelm, C.; Grauer, J.N. Racial Disparities in Surgical Versus Nonsurgical Management of Distal Radius Fractures in a Medicare Population. Hand 2023, 15589447231198267. [Google Scholar] [CrossRef] [PubMed]
- Doering, T.A.; Mauck, B.M.; Calandruccio, J.H. Hot Topics in Hand and Wrist Surgery. Orthop. Clin. N. Am. 2021, 52, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Ensrud, K.E. Epidemiology of fracture risk with advancing age. J. Gerontol. A Biol. Sci. Med. Sci. 2013, 68, 1236–1242. [Google Scholar] [CrossRef] [PubMed]
- Dempster, D.W. Osteoporosis and the burden of osteoporosis-related fractures. Am. J. Manag. Care 2011, 17 (Suppl. S6), S164–S169. [Google Scholar]
- Nellans, K.W.; Kowalski, E.; Chung, K.C. The epidemiology of distal radius fractures. Hand Clin. 2012, 28, 113–125. [Google Scholar] [CrossRef]
- Oldrini, L.M.; Feltri, P.; Albanese, J.; Lucchina, S.; Filardo, G.; Candrian, C. Volar locking plate vs cast immobilization for distal radius fractures: A systematic review and meta-analysis. EFORT Open Rev. 2022, 7, 644–652. [Google Scholar] [CrossRef]
- Nana, A.D.; Joshi, A.; Lichtman, D.M. Plating of the distal radius. J. Am. Acad. Orthop. Surg. 2005, 13, 159–171. [Google Scholar] [CrossRef] [PubMed]
- Chaudhry, H.; Kleinlugtenbelt, Y.V.; Mundi, R.; Ristevski, B.; Goslings, J.C.; Bhandari, M. Are Volar Locking Plates Superior to Percutaneous K-wires for Distal Radius Fractures? A Meta-analysis. Clin. Orthop. Relat. Res. 2015, 473, 3017–3027. [Google Scholar] [CrossRef] [PubMed]
- Zong, S.L.; Kan, S.L.; Su, L.X.; Wang, B. Meta-analysis for dorsally displaced distal radius fracture fixation: Volar locking plate versus percutaneous Kirschner wires. J. Orthop. Surg. Res. 2015, 10, 108. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, E.; Campanholi, G.; Acherboim, M.; Ruggiero, G.M. Mini-Invasive Surgery for Distal Radius Fractures: A Double Incision under 12 mm. J. Wrist Surg. 2021, 10, 136–143. [Google Scholar] [CrossRef] [PubMed]
- Lebailly, F.; Zemirline, A.; Facca, S.; Gouzou, S.; Liverneaux, P. Distal radius fixation through a mini-invasive approach of 15 mm. PART 1: A series of 144 cases. Eur. J. Orthop. Surg. Traumatol. 2014, 24, 877–890. [Google Scholar] [CrossRef] [PubMed]
- Zemirline, A.; Naito, K.; Lebailly, F.; Facca, S.; Liverneaux, P. Distal radius fixation through a mini-invasive approach of 15 mm. Part 1: Feasibility study. Eur. J. Orthop. Surg. Traumatol. 2014, 24, 1031–1037. [Google Scholar] [CrossRef] [PubMed]
- Zemirline, A.; Taleb, C.; Facca, S.; Liverneaux, P. Minimally invasive surgery of distal radius fractures: A series of 20 cases using a 15 mm anterior approach and arthroscopy. Chir. Main 2014, 33, 263–271. [Google Scholar] [CrossRef]
- Naito, K.; Zemirline, A.; Sugiyama, Y.; Obata, H.; Liverneaux, P.; Kaneko, K. Possibility of Fixation of a Distal Radius Fracture With a Volar Locking Plate Through a 10 mm Approach. Tech. Hand Up. Extrem. Surg. 2016, 20, 71–76. [Google Scholar] [CrossRef]
- Soong, M.; Earp, B.E.; Bishop, G.; Leung, A.; Blazar, P. Volar locking plate implant prominence and flexor tendon rupture. J. Bone Jt. Surg. Am. 2011, 93, 328–335. [Google Scholar] [CrossRef]
- Kleinlugtenbelt, Y.V.; Krol, R.G.; Bhandari, M.; Goslings, J.C.; Poolman, R.W.; Scholtes, V.A.B. Are the patient-rated wrist evaluation (PRWE) and the disabilities of the arm, shoulder and hand (DASH) questionnaire used in distal radial fractures truly valid and reliable? Bone Jt. Res. 2018, 7, 36–45. [Google Scholar] [CrossRef]
- Asmar, G.; Bellity, J.; Falcone, M.O. Surgical comfort and clinical outcomes of MIPO with an extra-short plate designed for distal radius fractures. Eur. J. Orthop. Surg. Traumatol. 2021, 31, 481–490. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.; Meyer, M.A.; Earp, B.E.; Blazar, P. Role of Pronator Quadratus Repair in Volar Locking Plate Treatment of Distal Radius Fractures. J. Am. Acad. Orthop. Surg. 2022, 30, 696–702. [Google Scholar] [CrossRef] [PubMed]
- Shi, F.; Ren, L. Is pronator quadratus repair necessary to improve outcomes after volar plate fixation of distal radius fractures? A systematic review and meta-analysis. Orthop. Traumatol. Surg. Res. 2020, 106, 1627–1635. [Google Scholar] [CrossRef] [PubMed]
- Mulders, M.A.M.; Walenkamp, M.M.J.; Bos, F.; Schep, N.W.L.; Goslings, J.C. Repair of the pronator quadratus after volar plate fixation in distal radius fractures: A systematic review. Strategies Trauma Limb Reconstr. 2017, 12, 181–188. [Google Scholar] [PubMed]
- Husain, T.M.; Jabbour, J.I.; Sudduth, J.D.; Lessard, A.S.; Patete, C.L.; Panthaki, Z.J.; Salloum, G.E. Pronator Quadratus Muscle Flap for Prevention of Flexor Tendon Rupture after Distal Radius Volar Plating. Plast. Reconstr. Surg. Glob. Open 2023, 11, e5227. [Google Scholar] [CrossRef] [PubMed]
- Falk, S.S.I.; Maksimow, A.; Mittlmeier, T.; Gradl, G. Does access through the pronator quadratus influence pronation strength in palmar plate fixation of distal radius fractures in elderly patients? Arch. Orthop. Trauma Surg. 2023, 143, 5445–5454. [Google Scholar] [CrossRef]
- Thalhammer, G.; Hruby, L.A.; Dangl, T.; Liebe, J.; Erhart, J.; Haider, T. Does the pronator-sparing approach improve functional outcome, compared to a standard volar approach, in volar plating of distal radius fractures? A prospective, randomized controlled trial. J. Orthop. Traumatol. 2023, 24, 16. [Google Scholar] [CrossRef]
- Maniglio, M.; Truong, V.; Zumstein, M.; Bolliger, L.; McGarry, M.H.; Lee, T.Q. Should We Repair the Pronator Quadratus in a Distal Radius Fracture with an Ulnar Styloid Base Fracture? A Biomechanical Study. J. Wrist Surg. 2021, 10, 407–412. [Google Scholar] [CrossRef]
- Turley, L.P.; Hurley, E.T.; White-Gibson, A.; Clesham, K.; Lyons, F. Pronator quadratus repair after volar plating for distal radius fractures: A systematic review and meta-analysis of randomized controlled trials. Acta Orthop. Traumatol. Turc. 2023, 57, 176–182. [Google Scholar] [CrossRef]
- Lee, J.H.; Lee, J.K.; Park, J.S.; Kim, D.H.; Baek, J.H.; Kim, Y.J.; Yoon, K.T.; Song, S.H.; Gwak, H.G.; Ha, C.; et al. Complications associated with volar locking plate fixation for distal radius fractures in 1955 cases: A multicentre retrospective study. Int. Orthop. 2020, 44, 2057–2067. [Google Scholar] [CrossRef]
- Azzi, A.J.; Aldekhayel, S.; Boehm, K.S.; Zadeh, T. Tendon Rupture and Tenosynovitis following Internal Fixation of Distal Radius Fractures: A Systematic Review. Plast. Reconstr. Surg. 2017, 139, 717e–724e. [Google Scholar] [CrossRef] [PubMed]
- Sato, K.; Murakami, K.; Mimata, Y.; Doita, M. Incidence of tendon rupture following volar plate fixation of distal radius fractures: A survey of 2787 cases. J. Orthop. 2018, 15, 236–238. [Google Scholar] [CrossRef] [PubMed]
- Thorninger, R.; Madsen, M.L.; Wæver, D.; Borris, L.C.; Duedal Rölfing, J.H. Complications of volar locking plating of distal radius fractures in 576 patients with 3.2 years follow-up. Injury 2017, 48, 1104–1109. [Google Scholar] [CrossRef] [PubMed]
- Vasara, H.; Tarkiainen, P.; Stenroos, A.; Kosola, J.; Anttila, T.; Aavikko, A.; Nordback, P.H.; Aspinen, S. Higher Soong grade predicts flexor tendon issues after volar plating of distal radius fractures—A retrospective cohort study. BMC Musculoskelet. Disord. 2023, 24, 271. [Google Scholar] [CrossRef]



| Conventional | Ultimate Incision | p-Value | |
|---|---|---|---|
| Number of patients | 40 | 46 | |
| Age, mean ± standard deviation (SD) | 63.4 ± 16.0 | 60.7 ± 15.2 | 0.530 |
| Sex (male/female) | 12/28 | 8/38 | 0.167 |
| Body mass index (BMI) | 27.6 ± 2.1 | 26.5 ± 2.3 | 0.684 |
| Laterality (right/left) | 19/21 | 19/27 | 0.564 |
| AO/OTA classification (A/B3/C1) | 27/4/9 | 38/1/7 | 0.099 |
| Conventional | Ultimate Incision | p-Value | |
|---|---|---|---|
| Pre-operative parameter (mean ± SD) | |||
| Volar tilt angle (°) | −13.1 ± 16.3 | −14.6 ± 18.6 | 0.652 |
| Radial inclination angle (°) | 13.8 ± 9.8 | 15.0 ± 9.6 | 0.774 |
| Ulna variance (mm) | 3.1 ± 1.3 | 2.9 ± 1.5 | 0.446 |
| Immediate post-operative parameter (mean ± SD) | |||
| Volar tilt angle (°) | 9.6 ± 5.0 | 9.0 ± 5.2 | 0.762 |
| Radial inclination angle (°) | 21.7 ± 4.2 | 21.9 ± 2.9 | 0.986 |
| Ulna variance (mm) | 0.5 ± 1.2 | 0.9 ± 1.2 | 0.166 |
| Soong grade (grade 0/1/2) | 20/18/2 | 29/14/3 | 0.378 |
| Parameters (Mean ± SD) | Conventional | Ultimate Incision | p-Value |
|---|---|---|---|
| Pain VAS | 0.7 ± 0.8 | 0.6 ± 0.7 | 0.684 |
| Q-DASH | 9.26 ± 10.6 | 5.42 ± 7.67 | 0.080 |
| PRWE | 12.2 ± 4.3 | 10.3 ± 4.1 | 0.134 |
| Cosmetic NRS | 1.93 ± 1.57 | 0.68 ± 0.87 | <0.001 |
| Surgical duration (min) | 76.3 ± 22.4 | 59.8 ± 12.6 | <0.001 |
| Pearls | Pitfalls | |
|---|---|---|
| Fracture type | Metaphysis and/or simple articular fractures | Avoid comminuted articular fractures. |
| Fracture reduction |
| Difficult to insert traditional reduction forceps into the ultimate incision. |
| Plate insertion |
| Avoid using retractors when inserting the plate. |
| Screw insertion |
| Avoid forceful wound retraction. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, C.-Y.; Lee, C.-C.; Chen, C.-W.; Hu, M.-H.; Wu, K.-W.; Wang, T.-M.; Wang, J.-H.; Tseng, T.-H. The Outcome of under 10 mm Single-Incision Surgery Using a Non-Specialized Volar Plate in Distal Radius Fractures: A Retrospective Comparative Study. J. Clin. Med. 2023, 12, 7670. https://doi.org/10.3390/jcm12247670
Huang C-Y, Lee C-C, Chen C-W, Hu M-H, Wu K-W, Wang T-M, Wang J-H, Tseng T-H. The Outcome of under 10 mm Single-Incision Surgery Using a Non-Specialized Volar Plate in Distal Radius Fractures: A Retrospective Comparative Study. Journal of Clinical Medicine. 2023; 12(24):7670. https://doi.org/10.3390/jcm12247670
Chicago/Turabian StyleHuang, Chang-Yu, Chia-Che Lee, Chih-Wei Chen, Ming-Hsiao Hu, Kuan-Wen Wu, Ting-Ming Wang, Jyh-Horng Wang, and Tzu-Hao Tseng. 2023. "The Outcome of under 10 mm Single-Incision Surgery Using a Non-Specialized Volar Plate in Distal Radius Fractures: A Retrospective Comparative Study" Journal of Clinical Medicine 12, no. 24: 7670. https://doi.org/10.3390/jcm12247670
APA StyleHuang, C.-Y., Lee, C.-C., Chen, C.-W., Hu, M.-H., Wu, K.-W., Wang, T.-M., Wang, J.-H., & Tseng, T.-H. (2023). The Outcome of under 10 mm Single-Incision Surgery Using a Non-Specialized Volar Plate in Distal Radius Fractures: A Retrospective Comparative Study. Journal of Clinical Medicine, 12(24), 7670. https://doi.org/10.3390/jcm12247670






