Enhancing Precision and Efficiency in Knee Arthroplasty: A Comparative Analysis of Computer-Assisted Measurements with a Novel Software Tool versus Manual Measurements for Lower Leg Geometry
Abstract
:1. Introduction
2. Materials and Methods
2.1. Manual Measurements
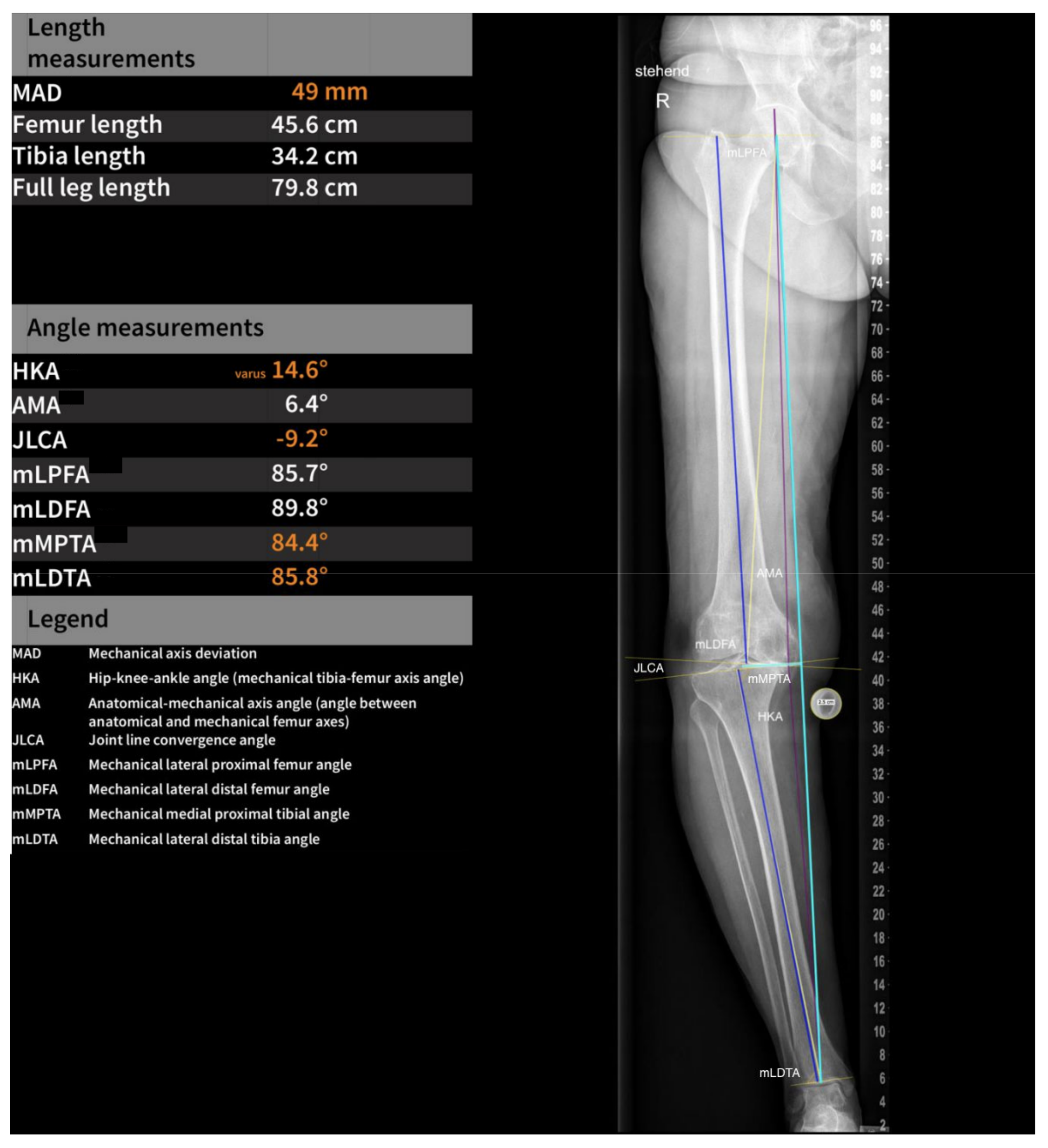
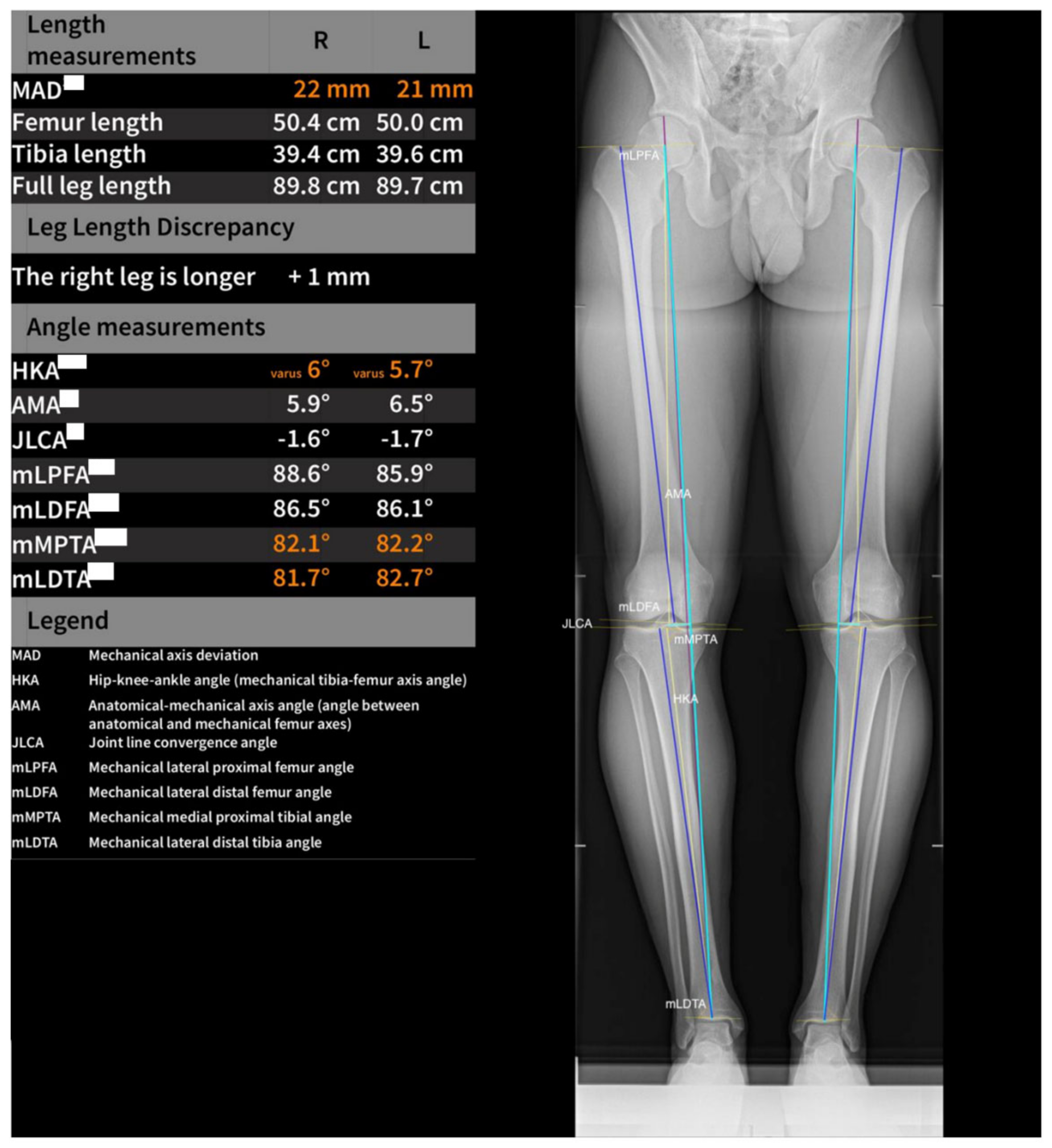
2.2. Software Measurements
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Berend, M.E.; Small, S.R.; Ritter, M.A.; Buckley, C.A.; Merk, J.C.; Dierking, W.K. Effects of femoral component size on proximal tibial strain with anatomic graduated components total knee arthroplasty. J. Arthroplast. 2010, 25, 58–63. [Google Scholar] [CrossRef]
- Ritter, M.A.; Faris, P.M.; Keating, E.M.; Meding, J.B. Postoperative alignment of total knee replacement. Its effect on survival. Clin. Orthop. Relat. Res. 1994, 299, 153–156. [Google Scholar] [CrossRef]
- Kinzel, V.; Scaddan, M.; Bradley, B.; Shakespeare, D. Varus/valgus alignment of the femur in total knee arthroplasty. Can accuracy be improved by pre-operative CT scanning? Knee 2004, 11, 197–201. [Google Scholar] [CrossRef] [PubMed]
- Kniesel, B.; Konstantinidis, L.; Hirschmüller, A.; Südkamp, N.; Helwig, P. Digital templating in total knee and hip replacement: An analysis of planning accuracy. Int. Orthop. 2014, 38, 733–739. [Google Scholar] [CrossRef] [PubMed]
- Schroer, W.C.; Berend, K.R.; Lombardi, A.V.; Barnes, C.L.; Bolognesi, M.P.; Berend, M.E.; Ritter, M.A.; Nunley, R.M. Why are total knees failing today? Etiology of total knee revision in 2010 and 2011. J. Arthroplast. 2013, 28, 116–119. [Google Scholar] [CrossRef]
- Goyal, N.; Stulberg, S.D. Evaluating the Precision of Preoperative Planning in Patient Specific Instrumentation: Can a Single MRI Yield Different Preoperative Plans? J. Arthroplast. 2015, 30, 1250–1253. [Google Scholar] [CrossRef]
- Hirschmann, M.T.; Konala, P.; Amsler, F.; Iranpour, F.; Friederich, N.F.; Cobb, J.P. The position and orientation of total knee replacement components: A comparison of conventional radiographs, transverse 2D-CT slices and 3D-CT reconstruction. J. Bone Jt. Surg. Br. 2011, 93, 629–633. [Google Scholar] [CrossRef]
- Tiefenboeck, S.; Sesselmann, S.; Taylor, D.; Forst, R.; Seehaus, F. Preoperative planning of total knee arthroplasty: Reliability of axial alignment using a three-dimensional planning approach. Acta Radiol. 2022, 63, 1051–1061. [Google Scholar] [CrossRef]
- The, B.; Diercks, R.L.; van Ooijen, P.M.A.; van Horn, J.R. Comparison of analog and digital preoperative planning in total hip and knee arthroplasties. A prospective study of 173 hips and 65 total knees. Acta Orthop. 2005, 76, 78–84. [Google Scholar] [CrossRef]
- Hsu, A.R.; Kim, J.D.; Bhatia, S.; Levine, B.R. Effect of training level on accuracy of digital templating in primary total hip and knee arthroplasty. Orthopedics 2012, 35, e179–e183. [Google Scholar] [CrossRef]
- Kobayashi, A.; Ishii, Y.; Takeda, M.; Noguchi, H.; Higuchi, H.; Toyabe, S. Comparison of analog 2D and digital 3D preoperative templating for predicting implant size in total knee arthroplasty. Comput. Aided Surg. 2012, 17, 96–101. [Google Scholar] [CrossRef]
- Ettinger, M.; Claassen, L.; Paes, P.; Calliess, T. 2D versus 3D templating in total knee arthroplasty. Knee 2016, 23, 149–151. [Google Scholar] [CrossRef] [PubMed]
- Jazrawi, L.M.; Birdzell, L.; Kummer, F.J.; Di Cesare, P.E. The accuracy of computed tomography for determining femoral and tibial total knee arthroplasty component rotation. J. Arthroplast. 2000, 15, 761–766. [Google Scholar] [CrossRef] [PubMed]
- Konigsberg, B.; Hess, R.; Hartman, C.; Smith, L.; Garvin, K.L. Inter- and intraobserver reliability of two-dimensional CT scan for total knee arthroplasty component malrotation. Clin. Orthop. Relat. Res. 2014, 472, 212–217. [Google Scholar] [CrossRef] [PubMed]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Hankemeier, S.; Gosling, T.; Richter, M.; Hufner, T.; Hochhausen, C.; Krettek, C. Computer-assisted analysis of lower limb geometry: Higher intraobserver reliability compared to conventional method. Comput. Aided Surg. 2006, 11, 81–86. [Google Scholar] [CrossRef]
- Schröter, S.; Ihle, C.; Mueller, J.; Lobenhoffer, P.; Stöckle, U.; van Heerwaarden, R. Digital planning of high tibial osteotomy. Interrater reliability by using two different software. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 189–196. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.S.; Kim, M.K.; Byun, H.W.; Kim, S.B.; Kim, J.G. Reliability of the imaging software in the preoperative planning of the open-wedge high tibial osteotomy. Knee Surg. Sports Traumatol. Arthrosc. 2015, 23, 846–851. [Google Scholar] [CrossRef]
- Moreland, J.R. Mechanisms of failure in total knee arthroplasty. Clin. Orthop. Relat. Res. 1988, 226, 49–64. [Google Scholar] [CrossRef]
- Gopurathingal, A.A.; Bhonsle, S. Inter-Observer and Intra-Observer Reliability of 2D Radiograph-Based Valgus Cut Angle Measurement in Preoperative Planning for Primary Total Knee Arthroplasty. Cureus 2021, 13, e12788. [Google Scholar] [CrossRef]
- Swanson, K.E.; Stocks, G.W.; Warren, P.D.; Hazel, M.R.; Janssen, H.F. Does axial limb rotation affect the alignment measurements in deformed limbs? Clin. Orthop. Relat. Res. 2000, 371, 246–252. [Google Scholar] [CrossRef] [PubMed]
- Pagano, S.; Müller, K.; Götz, J.; Reinhard, J.; Schindler, M.; Grifka, J.; Maderbacher, G. The Role and Efficiency of an AI-Powered Software in the Evaluation of Lower Limb Radiographs before and after Total Knee Arthroplasty. J. Clin. Med. 2023, 12, 5498. [Google Scholar] [CrossRef] [PubMed]
- Miura, M.; Hagiwara, S.; Nakamura, J.; Wako, Y.; Kawarai, Y.; Ohtori, S. Interobserver and Intraobserver Reliability of Computed Tomography-Based Three-Dimensional Preoperative Planning for Primary Total Knee Arthroplasty. J. Arthroplast. 2018, 33, 1572–1578. [Google Scholar] [CrossRef] [PubMed]
- Kastner, N.; Aigner, B.A.; Meikl, T.; Friesenbichler, J.; Wolf, M.; Glehr, M.; Gruber, G.; Leithner, A.; Sadoghi, P. Gender-specific outcome after implantation of low-contact-stress mobile-bearing total knee arthroplasty with a minimum follow-up of ten years. Int. Orthop. 2014, 38, 2489–2493. [Google Scholar] [CrossRef]
- Kastner, N.; Sternbauer, S.; Friesenbichler, J.; Vielgut, I.; Wolf, M.; Glehr, M.; Leithner, A.; Sadoghi, P. Impact of the tibial slope on range of motion after low-contact-stress, mobile-bearing, total knee arthroplasty. Int. Orthop. 2014, 38, 291–295. [Google Scholar] [CrossRef]
- Neubauer, M.; Moser, L.; Neugebauer, J.; Raudner, M.; Wondrasch, B.; Führer, M.; Emprechtinger, R.; Dammerer, D.; Ljuhar, R.; Salzlechner, C.; et al. Artificial-Intelligence-Aided Radiographic Diagnostic of Knee Osteoarthritis Leads to a Higher Association of Clinical Findings with Diagnostic Ratings. J. Clin. Med. 2023, 12, 744. [Google Scholar] [CrossRef]

| Manual d1 | Manual d15 | Software d1 | Software d15 | |
|---|---|---|---|---|
| mLPFA | 90.3 (SD: 4.7) | 89.7 (SD: 3.9) | 91.7 (SD: 4.8) | 91.8 (SD: 4.8) |
| mLDFA | 89.2 (SD: 4.1) | 88.0 (SD: 3.9) | 88.1 (SD: 2.9) | 88.2 (SD: 2.9) |
| JLCA | 3.3 (SD: 3.7) | 3.3 (SD: 3.9) | 2.4 (SD: 4.0) | 2.5 (SD: 4.0) |
| mMPTA | 89.5 (SD: 3.3) | 88.9 (SD: 3.4) | 87.8 (SD: 2.8) | 87.8 (SD: 2.8) |
| mLPTA | 88.5 (SD: 3.5) | 87.9 (SD: 3.2) | 86.2 (SD: 3.8) | 86.1 (SD: 3.8) |
| HKA | 2.6 (SD: 7.1) | 2.8 (SD: 7.6) | 2.6 (SD: 7.6) | 2.7 (SD: 7.6) |
| AMA | 6.7 (SD: 1.1) | 7.0 (SD: 1.6) | 6.9 (SD: 1.1) | 6.9 (SD: 1.1) |
| Knee Angles | Intra-Observer Variability (Manual) | Intra-Observer Variability (Software) | Inter-Observer Variability d1 | Inter-Observer Variability d15 |
|---|---|---|---|---|
| mLPFA | p = 0.285 | p = 0.320 | p = 0.026 | p < 0.001 |
| mLDFA | p = 0.012 | p = 0.320 | p = 0.035 | p = 0.741 |
| JLCA | p = 0.822 | p = 0.435 | p = 0.114 | p = 0.103 |
| mMPTA | p = 0.164 | p = 0.320 | p < 0.001 | p = 0.010 |
| mLPTA | p = 0.097 | p = 0.276 | p < 0.001 | p < 0.001 |
| HKA | p = 0.726 | p = 0.320 | p = 0.934 | p = 0.943 |
| AMA | p = 0.030 | p = 0.320 | p = 0.087 | p = 0.594 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wittig, U.; Koutp, A.; Reinbacher, P.; Hütter, K.; Leithner, A.; Sadoghi, P. Enhancing Precision and Efficiency in Knee Arthroplasty: A Comparative Analysis of Computer-Assisted Measurements with a Novel Software Tool versus Manual Measurements for Lower Leg Geometry. J. Clin. Med. 2023, 12, 7581. https://doi.org/10.3390/jcm12247581
Wittig U, Koutp A, Reinbacher P, Hütter K, Leithner A, Sadoghi P. Enhancing Precision and Efficiency in Knee Arthroplasty: A Comparative Analysis of Computer-Assisted Measurements with a Novel Software Tool versus Manual Measurements for Lower Leg Geometry. Journal of Clinical Medicine. 2023; 12(24):7581. https://doi.org/10.3390/jcm12247581
Chicago/Turabian StyleWittig, Ulrike, Amir Koutp, Patrick Reinbacher, Konstanze Hütter, Andreas Leithner, and Patrick Sadoghi. 2023. "Enhancing Precision and Efficiency in Knee Arthroplasty: A Comparative Analysis of Computer-Assisted Measurements with a Novel Software Tool versus Manual Measurements for Lower Leg Geometry" Journal of Clinical Medicine 12, no. 24: 7581. https://doi.org/10.3390/jcm12247581
APA StyleWittig, U., Koutp, A., Reinbacher, P., Hütter, K., Leithner, A., & Sadoghi, P. (2023). Enhancing Precision and Efficiency in Knee Arthroplasty: A Comparative Analysis of Computer-Assisted Measurements with a Novel Software Tool versus Manual Measurements for Lower Leg Geometry. Journal of Clinical Medicine, 12(24), 7581. https://doi.org/10.3390/jcm12247581







