Implant Preference and Clinical Outcomes of Patients with Staged Bilateral Total Knee Arthroplasty: All-Polyethylene and Contralateral Metal-Backed Tibial Components
Abstract
:1. Introduction
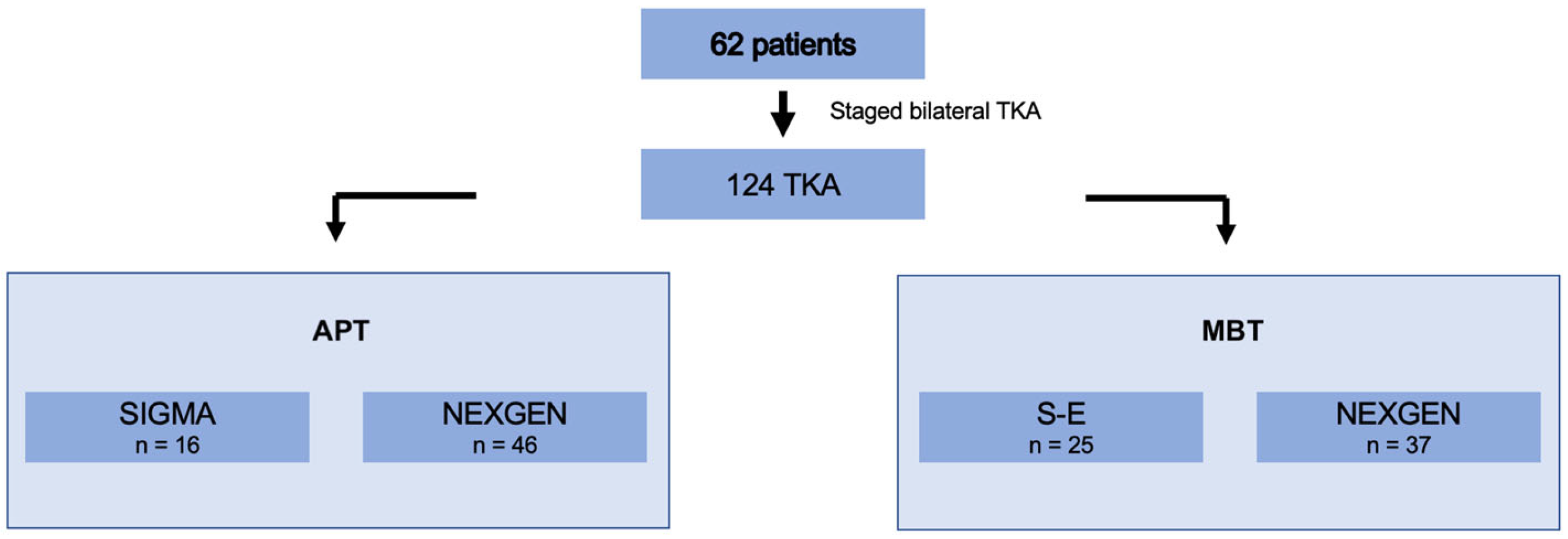
2. Materials and Methods
2.1. Sample Characteristics
2.2. Evaluation
2.3. Implant Types
2.4. Surgical Technique
2.5. Statistical Methods
3. Results
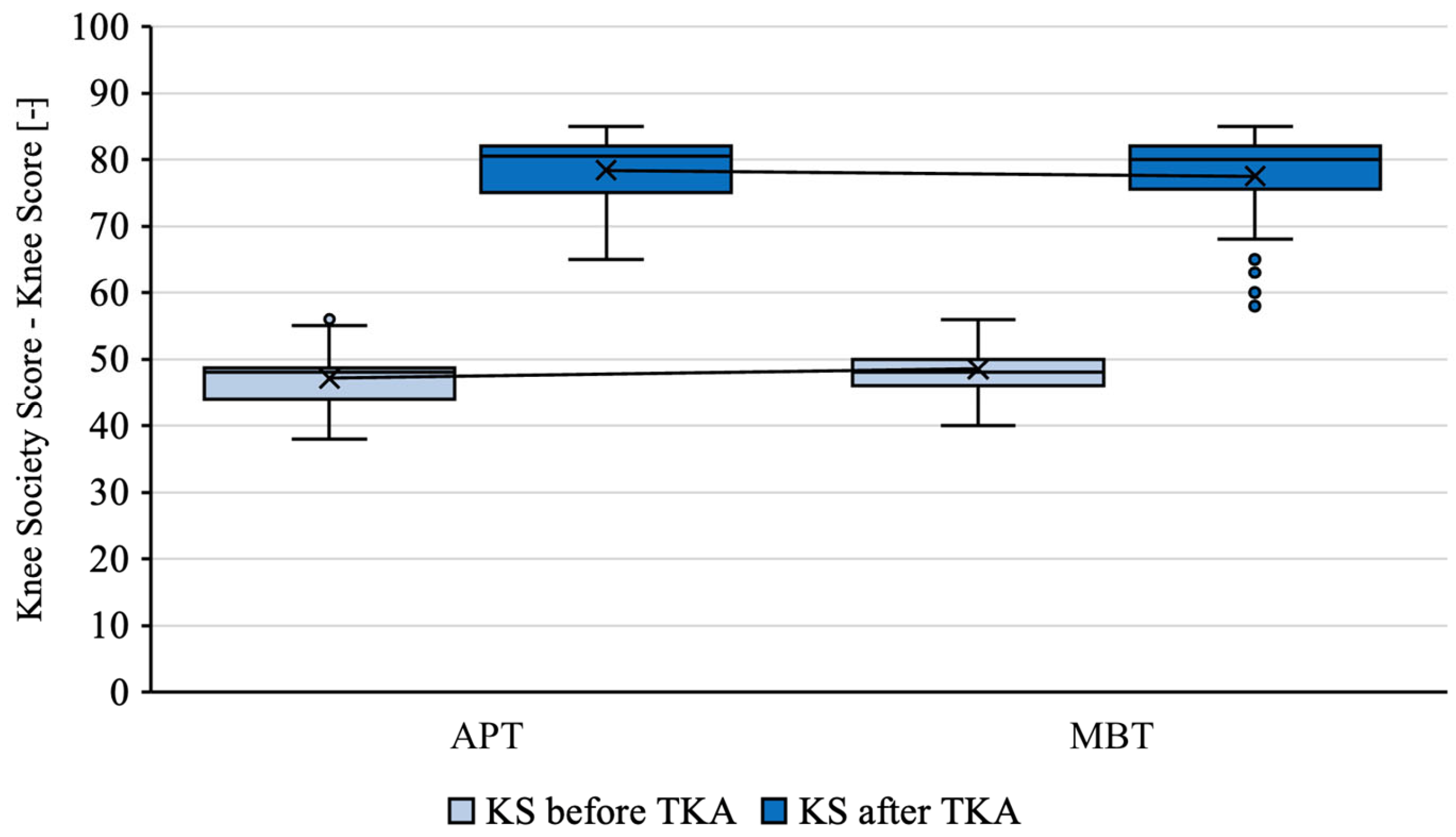
3.1. Functional Outcome
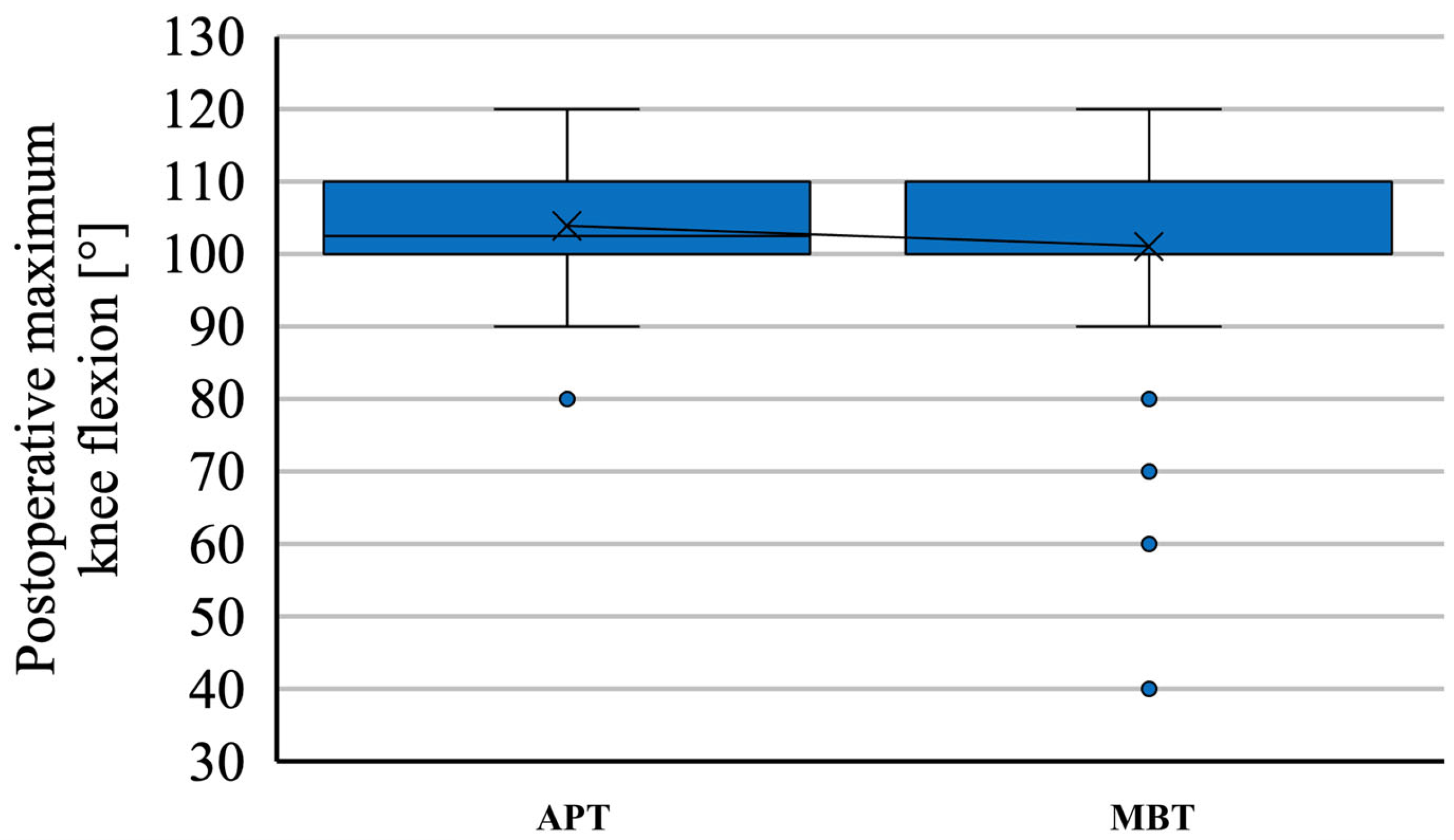
3.2. Range of Motion
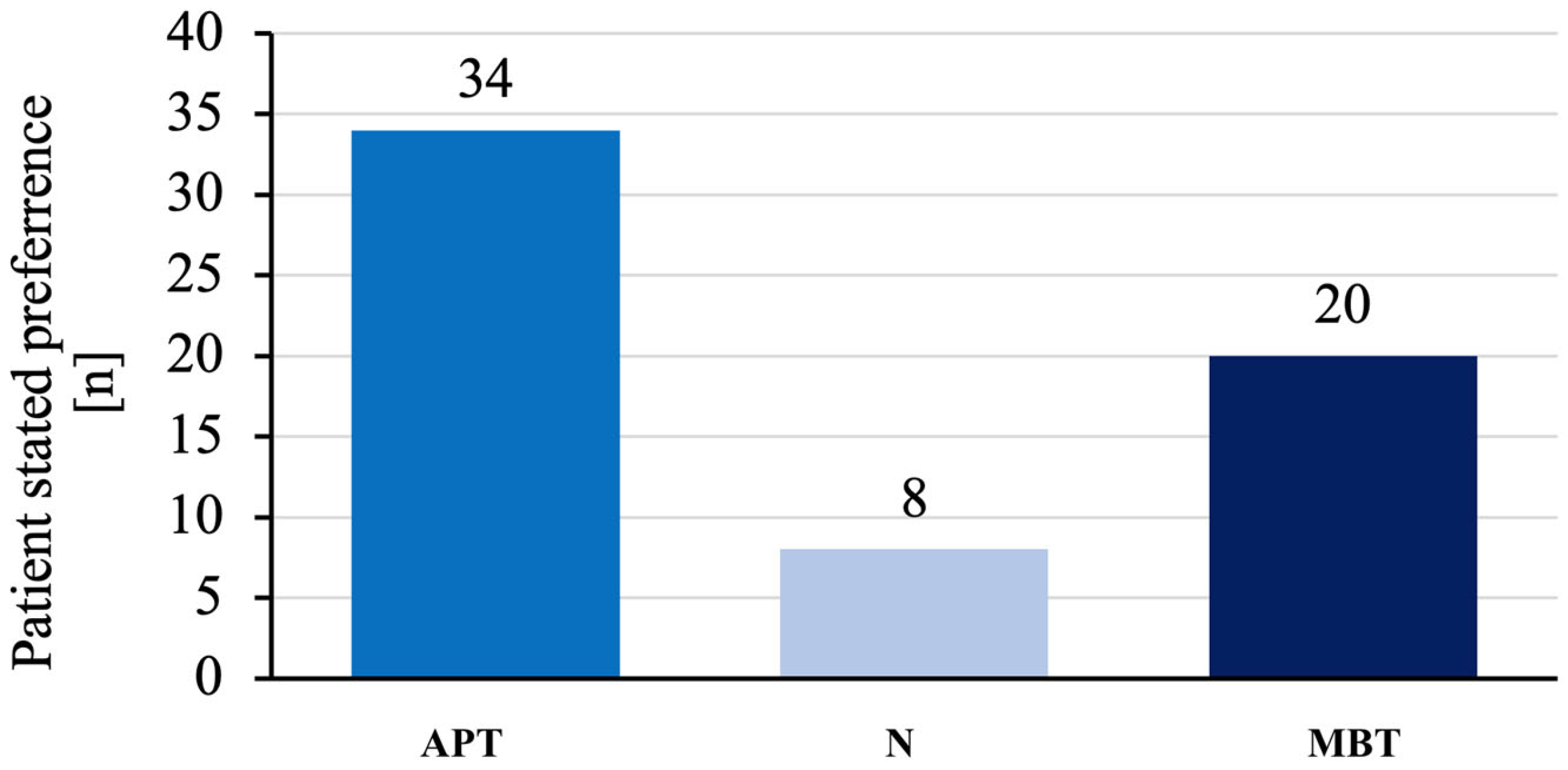
3.3. Implant Preference
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Batailler, C.; Swan, J.; Sappey Marinier, E.; Servien, E.; Lustig, S. New Technologies in Knee Arthroplasty: Current Concepts. J. Clin. Med. 2020, 10, 47. [Google Scholar] [CrossRef]
- Palazzuolo, M.; Antoniadis, A.; Mahlouly, J.; Wegrzyn, J. Total Knee Arthroplasty Improves the Quality-Adjusted Life Years in Patients Who Exceeded Their Estimated Life Expectancy. Int. Orthop. 2021, 45, 635–641. [Google Scholar] [CrossRef]
- Apostolopoulos, V.; Nachtnebl, L.; Mahdal, M.; Pazourek, L.; Boháč, P.; Janíček, P.; Tomáš, T. Clinical Outcomes and Survival Comparison between NexGen All-Poly and Its Metal-Backed Equivalent in Total Knee Arthroplasty. Int. Orthop. 2023, 47, 2207–2213. [Google Scholar] [CrossRef]
- Longo, U.G.; Ciuffreda, M.; D’Andrea, V.; Mannering, N.; Locher, J.; Denaro, V. All-Polyethylene versus Metal-Backed Tibial Component in Total Knee Arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 3620–3636. [Google Scholar] [CrossRef]
- Yassin, M.; Garti, A.; Weissbrot, M.; Ashkenazi, U.; Khatib, M.; Robinson, D. All-Polyethylene Tibial Components Are Not Inferior to Metal-Backed Tibial Components in Long-Term Follow-up of Knee Arthroplasties. Eur. J. Orthop. Surg. Traumatol. 2015, 25, 1087–1091. [Google Scholar] [CrossRef]
- Mohan, V.; Inacio, M.C.S.; Namba, R.S.; Sheth, D.; Paxton, E.W. Monoblock All-Polyethylene Tibial Components Have a Lower Risk of Early Revision than Metal-Backed Modular Components: A Registry Study of 27,657 Primary Total Knee Arthroplasties. Acta Orthop. 2013, 84, 530–536. [Google Scholar] [CrossRef]
- Voss, B.; El-Othmani, M.M.; Schnur, A.-K.; Botchway, A.; Mihalko, W.M.; Saleh, K.J. A Meta-Analysis Comparing All-Polyethylene Tibial Component to Metal-Backed Tibial Component in Total Knee Arthroplasty: Assessing Survivorship and Functional Outcomes. J. Arthroplast. 2016, 31, 2628–2636. [Google Scholar] [CrossRef]
- Ryan, S.P.; Steele, J.R.; Plate, J.F.; Attarian, D.E.; Seyler, T.M.; Bolognesi, M.P.; Wellman, S.S. All-Polyethylene Tibia: An Opportunity for Value-Based Care in Bundled Reimbursement Initiatives. Orthopedics 2021, 44, e114–e118. [Google Scholar] [CrossRef]
- Kumar, V.; Hasan, O.; Umer, M.; Baloch, N. Cemented All-Poly Tibia in Resource Constrained Country, Affordable and Cost-Effective Care. Is It Applicable at This Era? Review Article. Ann. Med. Surg. 2019, 47, 36–40. [Google Scholar] [CrossRef]
- Nachtnebl, L.; Tomáš, T.; Apostolopoulos, V.; Pazourek, L.; Mahdal, M. Long-Term Results of Total Knee Replacement Using P.F.C. Sigma System with an All-Polyethylene Tibial Component. Acta Chir. Orthop. Traumatol. Cech. 2021, 88, 412–417. [Google Scholar]
- Apostolopoulos, V.; Tomáš, T.; Boháč, P.; Marcián, P.; Mahdal, M.; Valoušek, T.; Janíček, P.; Nachtnebl, L. Biomechanical Analysis of All-Polyethylene Total Knee Arthroplasty on Periprosthetic Tibia Using the Finite Element Method. Comput. Methods Prog. Biomed. 2022, 220, 106834. [Google Scholar] [CrossRef]
- Insall, J.N.; Dorr, L.D.; Scott, R.D.; Scott, W.N. Rationale of the Knee Society Clinical Rating System. Clin. Orthop. Relat. Res. 1989, 248, 13–14. [Google Scholar]
- Australian Orthopaedic Association National Joint Replacement Registry. Annual Report. Adelaide. AOA 2020: Table KT2 10 Most Used Femoral Prostheses in Primary Total Knee Replacement. Available online: https://aoanjrr.sahmri.com/documents/10180/689619/Hip%2C+Knee+%26+Shoulder+Arthroplasty+New/6a07a3b8-8767-06cf-9069-d165dc9baca7 (accessed on 30 December 2022).
- Doran, J.; Yu, S.; Smith, D.; Iorio, R. The Role of All-Polyethylene Tibial Components in Modern TKA. J. Knee Surg. 2015, 28, 382–389. [Google Scholar] [CrossRef]
- Gustke, K.A.; Gelbke, M.K. All-Polyethylene Tibial Component Use for Elderly, Low-Demand Total Knee Arthroplasty Patients. J. Arthrop. 2017, 32, 2421–2426. [Google Scholar] [CrossRef]
- Herschmiller, T.; Bradley, K.E.; Wellman, S.S.; Attarian, D.E. Early to Midterm Clinical and Radiographic Survivorship of the All-Polyethylene Versus Modular Metal-Backed Tibia Component in Primary Total Knee Replacement. J. Surg. Orthop. Adv. 2019, 28, 108–114. [Google Scholar]
- Selvan, D.R.; Santini, A.J.A.; Davidson, J.S.; Pope, J.A. The Medium-Term Survival Analysis of an All-Polyethylene Tibia in a Single-Series Cohort of over 1000 Knees. J. Arthrop. 2020, 35, 2837–2842. [Google Scholar] [CrossRef]
- Kelley, B.; Mullen, K.; De, A.; Sassoon, A. Modular Metal-Backed Tibial Components Provide Minimal Mid-Term Survivorship Benefits Despite Increased Cost and Frequency of Use: A Retrospective Review of the American Joint Replacement Registry Database. J. Arthrop. 2022, 37, 1570–1574.e1. [Google Scholar] [CrossRef]
- Nouta, K.A.; Verra, W.C.; Pijls, B.G.; Schoones, J.W.; Nelissen, R.G.H.H. All-Polyethylene Tibial Components Are Equal to Metal-Backed Components: Systematic Review and Meta-Regression. Clin. Orthop. Relat. Res. 2012, 470, 3549–3559. [Google Scholar] [CrossRef]
- Jabbal, M.; Clement, N.; Walmsley, P.J. All-Polyethylene Tibia Components Have the Same Functional Outcomes and Survival, and Are More Cost-Effective than Metal-Backed Components in Patients 70 Years and Older Undergoing Total Knee Arthroplasty: Propensity Match Study with a Minimum Five-Year Follow-Up. Bone Jt. Open 2022, 3, 969–976. [Google Scholar] [CrossRef]
- Najfeld, M.; Kalteis, T.; Spiegler, C.; Ley, C.; Hube, R. The Safety of Bilateral Simultaneous Hip and Knee Arthroplasty versus Staged Arthroplasty in a High-Volume Center Comparing Blood Loss, Peri- and Postoperative Complications, and Early Functional Outcome. J. Clin. Med. 2021, 10, 4507. [Google Scholar] [CrossRef]
- Cammisa, E.; Sassoli, I.; La Verde, M.; Fratini, S.; Rinaldi, V.G.; Lullini, G.; Vaccari, V.; Zaffagnini, S.; Marcheggiani Muccioli, G.M. Bilateral Knee Arthroplasty in Patients Affected by Windswept Deformity: A Systematic Review. J. Clin. Med. 2022, 11, 6580. [Google Scholar] [CrossRef]
- Sugita, T.; Miyatake, N.; Aizawa, T.; Sasaki, A.; Kamimura, M.; Takahashi, A. Quality of Life after Staged Bilateral Total Knee Arthroplasty: A Minimum Five-Year Follow-up Study of Seventy-Eight Patients. Int. Orthop. 2019, 43, 2309–2314. [Google Scholar] [CrossRef]
- Schroeder, L.; Dunaway, A.; Dunaway, D. A Comparison of Clinical Outcomes and Implant Preference of Patients with Bilateral TKA: One Knee with a Patient-Specific and One Knee with an Off-the-Shelf Implant. JBJS Rev. 2022, 10, e20.00182. [Google Scholar] [CrossRef]


| Features | Bilateral TKA |
|---|---|
| Number of patients (knees) | 62 (124) |
| Age at inclusion (years) | |
| APT | 74.1 ± 3.56 (66–82) |
| MBT | 69.9 ± 3.69 (61–79) p < 0.00001 |
| Sex | |
| Female | 37 (59.7%) |
| Male | 25 (40.3%) |
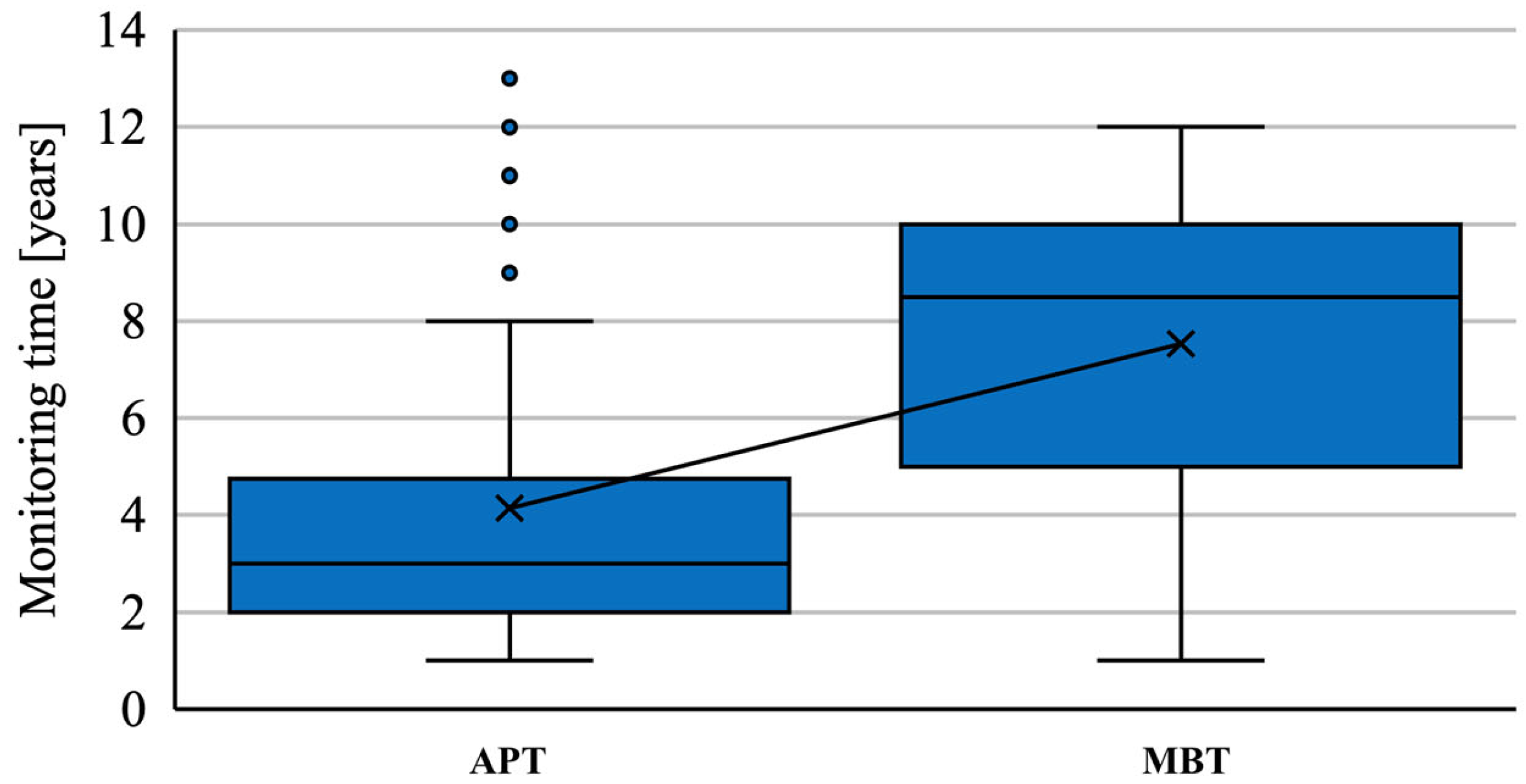
| Average follow-up (years) | |
| APT | 4.14 ± 3.19 (1–12) |
| MBT | 7.45 ± 3.01 (1–12) p < 0.00001 |
| Diagnosis | |
| Primary osteoarthritis | 124 (100%) |
| Surgical approach | |
| Medial parapatellar | 124 (100%) |
| Overall | KS: APT | KS: MBT | FS: APT | FS: MBT |
|---|---|---|---|---|
| Mean | 47.11 | 48.54 | 44.35 | 46.29 |
| Std. Dev | 4.00 | 3.56 | 4.09 | 3.83 |
| Median | 48 | 48 | 45 | 45 |
| N.Valid | 62 | 62 | 62 | 62 |
| Overall | KS: APT | KS: MBT | FS: APT | FS: MBT |
|---|---|---|---|---|
| Mean | 78.37 | 77.4 | 78.22 | 76.29 |
| Std. Dev | 5.11 | 6.87 | 4.44 | 7.06 |
| Median | 80.5 | 80 | 80 | 80 |
| N.Valid | 62 | 62 | 62 | 62 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nachtnebl, L.; Apostolopoulos, V.; Mahdal, M.; Pazourek, L.; Brančík, P.; Valoušek, T.; Boháč, P.; Tomáš, T. Implant Preference and Clinical Outcomes of Patients with Staged Bilateral Total Knee Arthroplasty: All-Polyethylene and Contralateral Metal-Backed Tibial Components. J. Clin. Med. 2023, 12, 7438. https://doi.org/10.3390/jcm12237438
Nachtnebl L, Apostolopoulos V, Mahdal M, Pazourek L, Brančík P, Valoušek T, Boháč P, Tomáš T. Implant Preference and Clinical Outcomes of Patients with Staged Bilateral Total Knee Arthroplasty: All-Polyethylene and Contralateral Metal-Backed Tibial Components. Journal of Clinical Medicine. 2023; 12(23):7438. https://doi.org/10.3390/jcm12237438
Chicago/Turabian StyleNachtnebl, Luboš, Vasileios Apostolopoulos, Michal Mahdal, Lukáš Pazourek, Pavel Brančík, Tomáš Valoušek, Petr Boháč, and Tomáš Tomáš. 2023. "Implant Preference and Clinical Outcomes of Patients with Staged Bilateral Total Knee Arthroplasty: All-Polyethylene and Contralateral Metal-Backed Tibial Components" Journal of Clinical Medicine 12, no. 23: 7438. https://doi.org/10.3390/jcm12237438
APA StyleNachtnebl, L., Apostolopoulos, V., Mahdal, M., Pazourek, L., Brančík, P., Valoušek, T., Boháč, P., & Tomáš, T. (2023). Implant Preference and Clinical Outcomes of Patients with Staged Bilateral Total Knee Arthroplasty: All-Polyethylene and Contralateral Metal-Backed Tibial Components. Journal of Clinical Medicine, 12(23), 7438. https://doi.org/10.3390/jcm12237438








