The Impact of Regional Nerve Blocks on Postoperative Delirium or Cognitive Dysfunction following Thoracic Surgery: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Methods
2.1. Eligible Criteria
2.2. Search Strategy
2.3. Study Selection
2.4. Data Extraction
2.5. Assessment of the Risk of Bias
2.6. Outcome Measures
2.7. Statistical Analysis
3. Results
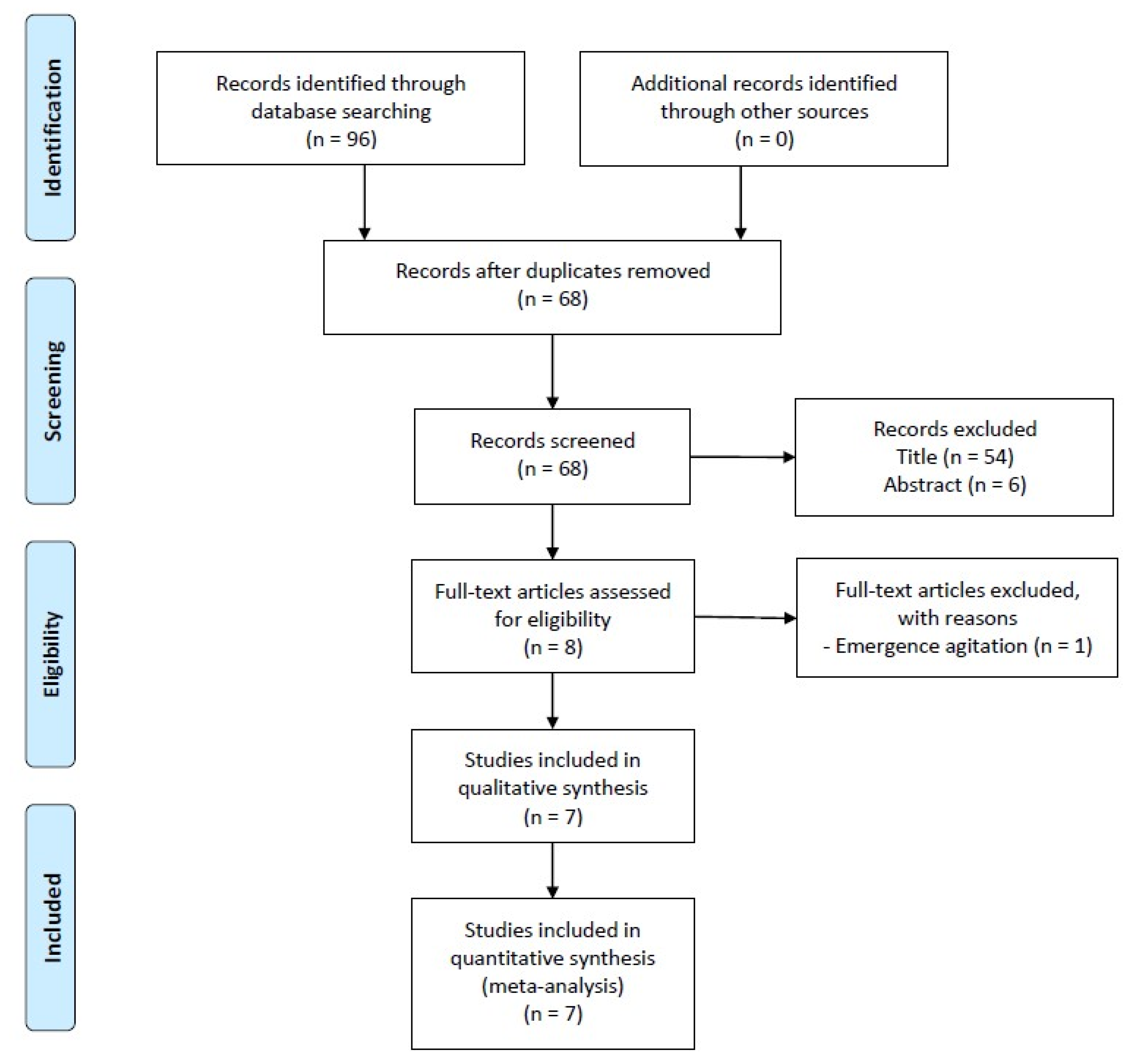
3.1. Study Selection
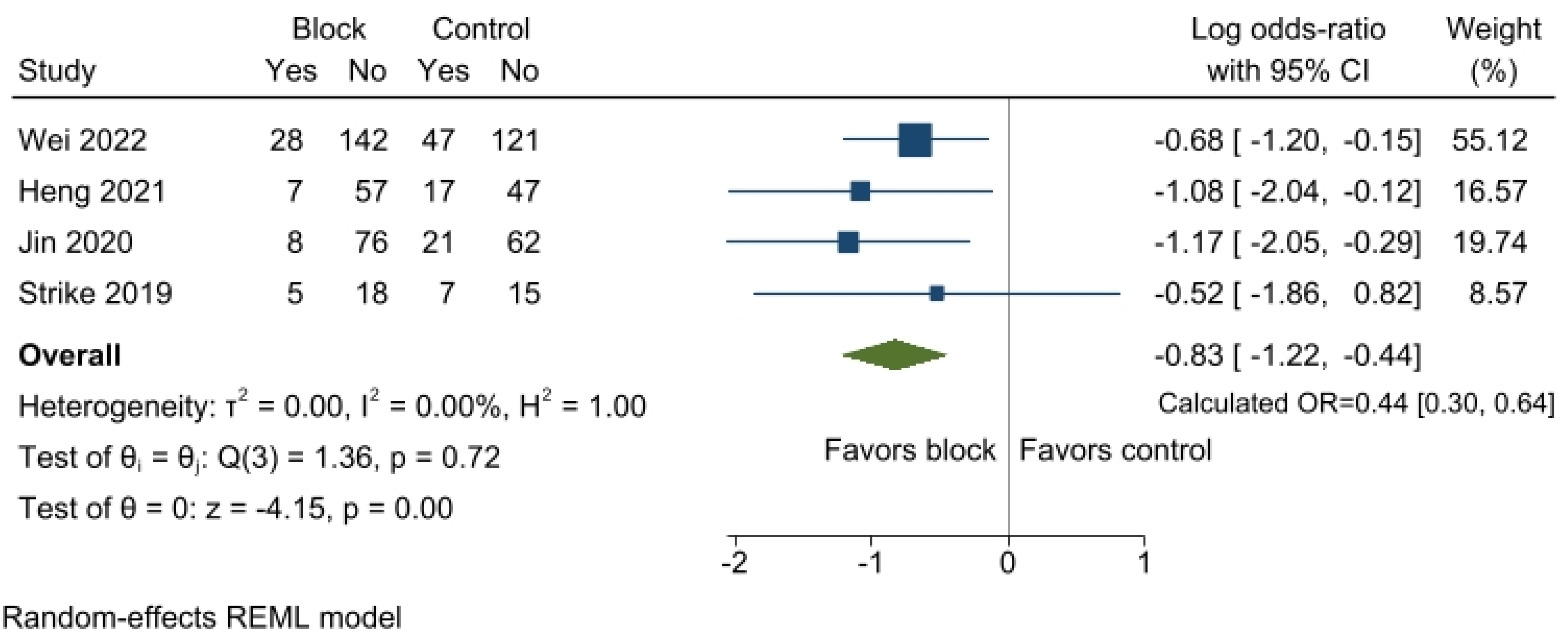
3.2. Postoperative Delirium
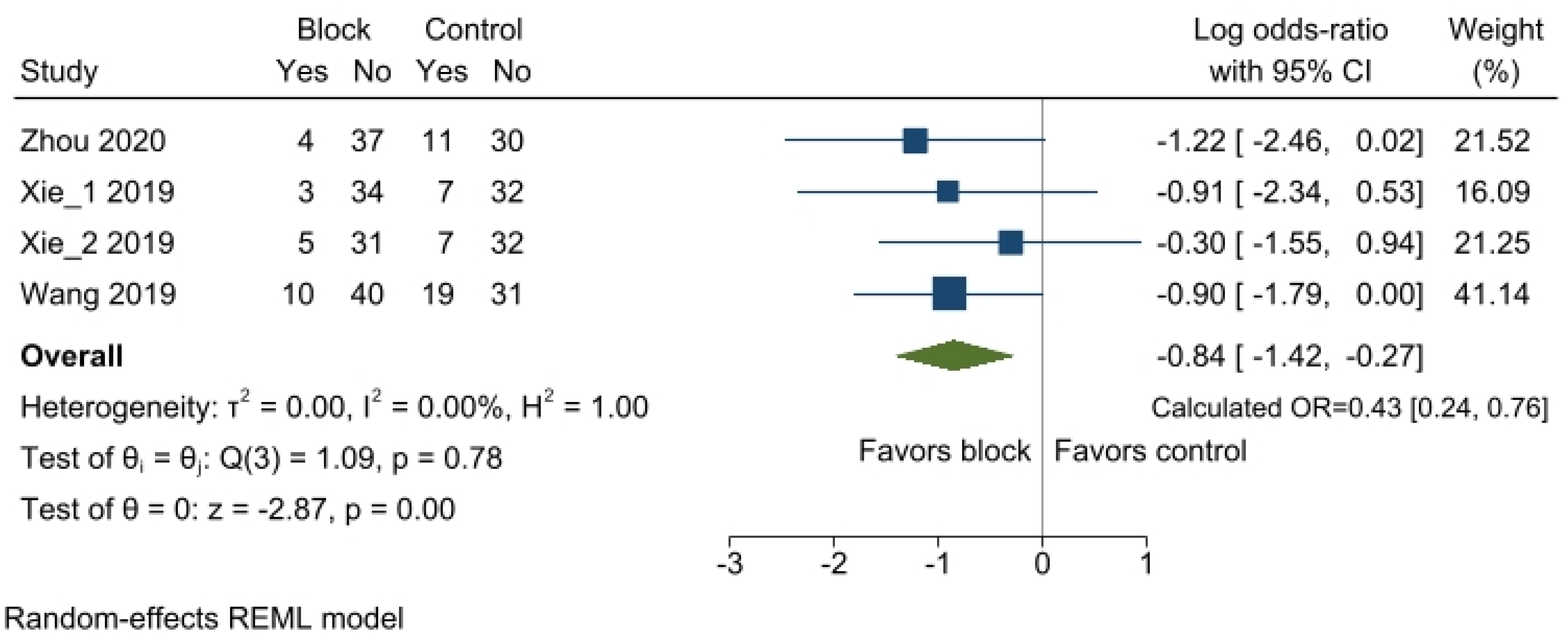
3.3. Postoperative Cognitive Dysfunction
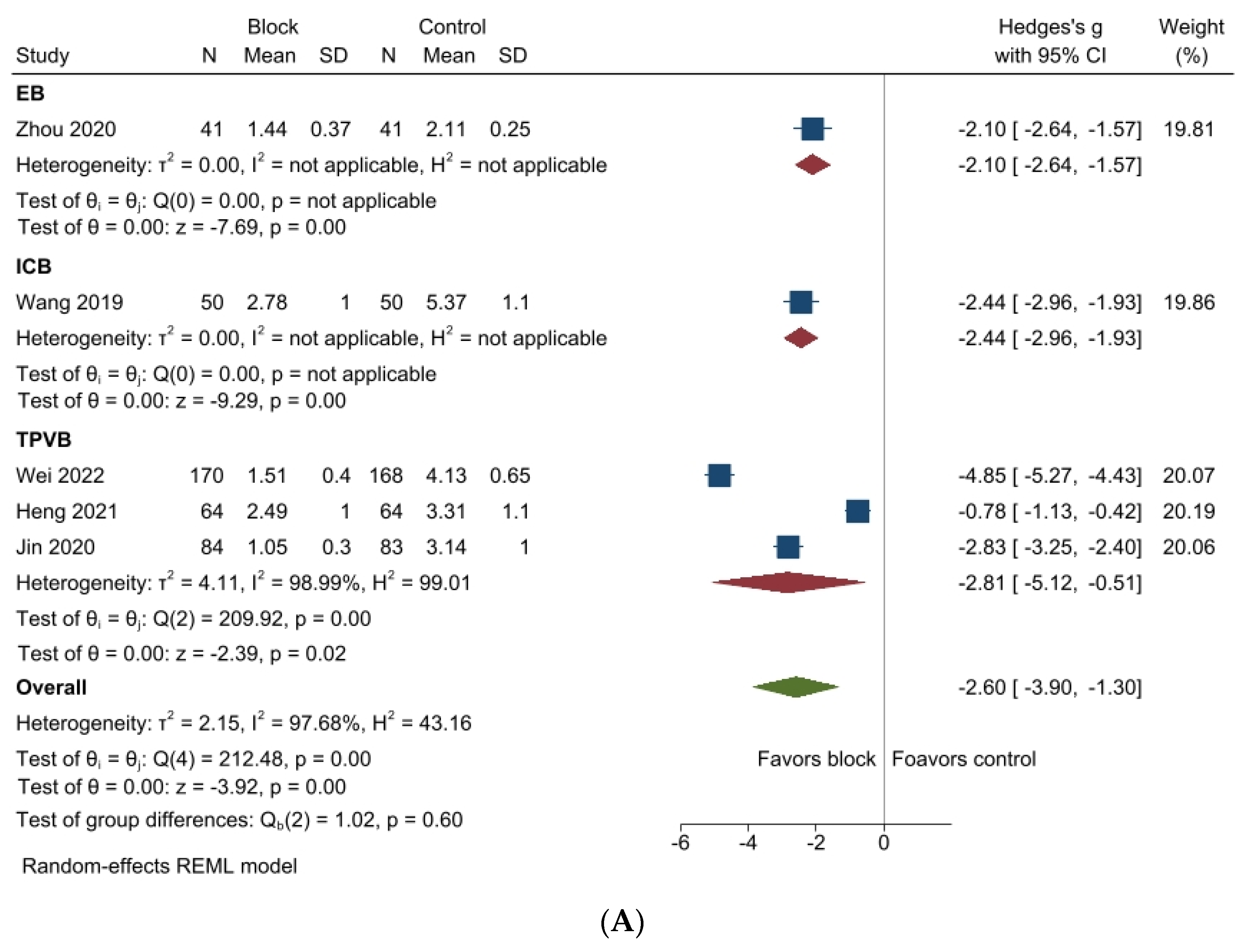
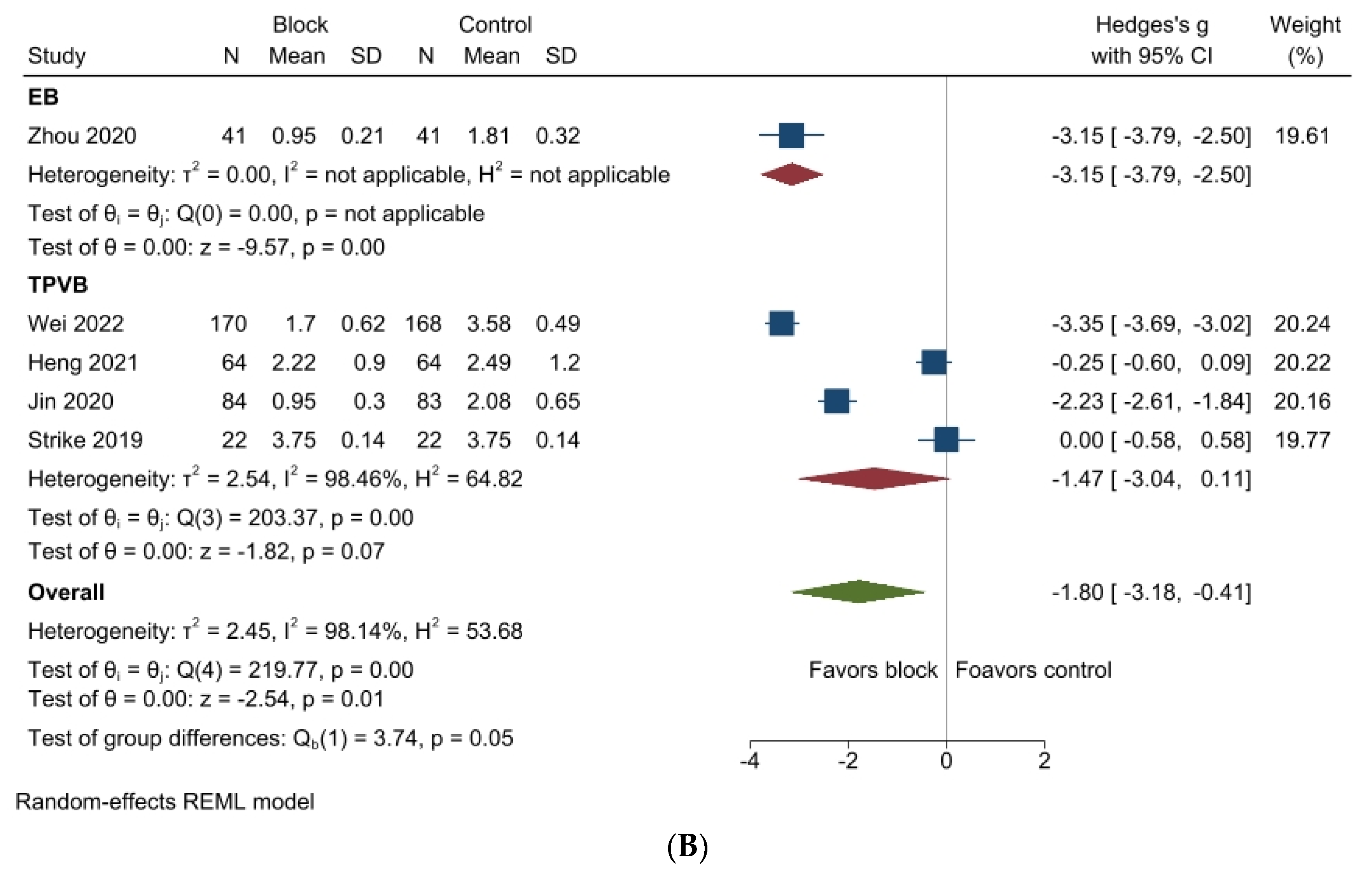
3.4. Pain Scores
4. Risk of Bias
5. Certainty of Evidence
6. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vacas, S.; Cole, D.J.; Cannesson, M. Cognitive Decline Associated With Anesthesia and Surgery in Older Patients. JAMA 2021, 326, 863–864. [Google Scholar] [CrossRef]
- Robinson, T.N.; Raeburn, C.D.; Tran, Z.V.; Angles, E.M.; Brenner, L.A.; Moss, M. Postoperative delirium in the elderly: Risk factors and outcomes. Ann. Surg. 2009, 249, 173–178. [Google Scholar] [CrossRef]
- Park, E.A.; Kim, M.Y. Postoperative Delirium is Associated with Negative Outcomes and Long-Term Mortality in Elderly Koreans: A Retrospective Observational Study. Medicina 2019, 55, 618. [Google Scholar] [CrossRef] [PubMed]
- Bramley, P.; McArthur, K.; Blayney, A.; McCullagh, I. Risk factors for postoperative delirium: An umbrella review of systematic reviews. Int. J. Surg. 2021, 93, 106063. [Google Scholar] [CrossRef] [PubMed]
- Jin, Z.; Hu, J.; Ma, D. Postoperative delirium: Perioperative assessment, risk reduction, and management. Br. J. Anaesth. 2020, 125, 492–504. [Google Scholar] [CrossRef]
- Vaurio, L.E.; Sands, L.P.; Wang, Y.; Mullen, E.A.; Leung, J.M. Postoperative delirium: The importance of pain and pain management. Anesth. Analg. 2006, 102, 1267–1273. [Google Scholar] [CrossRef]
- Jin, F.; Chung, F. Multimodal analgesia for postoperative pain control. J. Clin. Anesth. 2001, 13, 524–539. [Google Scholar] [CrossRef]
- Wei, W.; Zheng, X.; Gu, Y.; Fu, W.; Tang, C.; Yao, Y. Effect of general anesthesia with thoracic paravertebral block on postoperative delirium in elderly patients undergoing thoracoscopic lobectomy: A randomized-controlled trial. BMC Anesthesiol. 2022, 22, 1. [Google Scholar] [CrossRef] [PubMed]
- Strike, E.; Arklina, B.; Stradins, P.; Cusimano, R.J.; Osten, M.; Horlick, E.; Styra, R.; Poonawala, H.; Carroll, J.; Djaiani, G. Postoperative Pain Management Strategies and Delirium After Transapical Aortic Valve Replacement: A Randomized Controlled Trial. J. Cardiothorac. Vasc. Anesth. 2019, 33, 1668–1672. [Google Scholar] [CrossRef]
- Guerra-Londono, C.E.; Privorotskiy, A.; Cozowicz, C.; Hicklen, R.S.; Memtsoudis, S.G.; Mariano, E.R.; Cata, J.P. Assessment of Intercostal Nerve Block Analgesia for Thoracic Surgery: A Systematic Review and Meta-analysis. JAMA Netw. Open 2021, 4, e2133394. [Google Scholar] [CrossRef]
- Jack, J.; McLellan, E.; Versyck, B.; Englesakis, M.; Chin, K. The role of serratus anterior plane and pectoral nerves blocks in cardiac surgery, thoracic surgery and trauma: A qualitative systematic review. Anaesthesia 2020, 75, 1372–1385. [Google Scholar] [CrossRef]
- Turhan, Ö.; Sivrikoz, N.; Sungur, Z.; Duman, S.; Özkan, B.; Şentürk, M. Thoracic Paravertebral Block Achieves Better Pain Control Than Erector Spinae Plane Block and Intercostal Nerve Block in Thoracoscopic Surgery: A Randomized Study. J. Cardiothorac. Vasc. Anesth. 2021, 35, 2920–2927. [Google Scholar] [CrossRef] [PubMed]
- Khan, B.A.; Perkins, A.J.; Campbell, N.L.; Gao, S.; Khan, S.H.; Wang, S.; Fuchita, M.; Weber, D.J.; Zarzaur, B.L.; Boustani, M.A. Preventing postoperative delirium after major noncardiac thoracic surgery—A randomized clinical trial. J. Am. Geriatr. Soc. 2018, 66, 2289–2297. [Google Scholar] [CrossRef]
- Van Norden, J.; Spies, C.; Borchers, F.; Mertens, M.; Kurth, J.; Heidgen, J.; Pohrt, A.; Mueller, A. The effect of peri-operative dexmedetomidine on the incidence of postoperative delirium in cardiac and non-cardiac surgical patients: A randomised, double-blind placebo-controlled trial. Anaesthesia 2021, 76, 1342–1351. [Google Scholar] [CrossRef] [PubMed]
- Shen, L.; Chen, J.-Q.; Yang, X.-L.; Hu, J.-C.; Gao, W.; Chai, X.-Q.; Wang, D. Flurbiprofen used in one-lung ventilation improves intraoperative regional cerebral oxygen saturation and reduces the incidence of postoperative delirium. Front. Psychiatry 2022, 13, 889637. [Google Scholar] [CrossRef] [PubMed]
- Aiello, G.; Cuocina, M.; La Via, L.; Messina, S.; Attaguile, G.A.; Cantarella, G.; Sanfilippo, F.; Bernardini, R. Melatonin or Ramelteon for Delirium Prevention in the Intensive Care Unit: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Clin. Med. 2023, 12, 435. [Google Scholar] [CrossRef]
- Fellous, S.; Dubost, B.; Cambriel, A.; Bonnet, M.-P.; Verdonk, F. Perioperative ketamine administration to prevent delirium and neurocognitive disorders after surgery: A systematic review and meta-analysis. Int. J. Surg. 2023, 109, 3555–3565. [Google Scholar] [CrossRef]
- Duning, T.; Ilting-Reuke, K.; Beckhuis, M.; Oswald, D. Postoperative delirium—Treatment and prevention. Curr. Opin. Anesthesiol. 2021, 34, 27–32. [Google Scholar] [CrossRef]
- Kim, S.Y.; Jo, H.Y.; Na, H.-S.; Han, S.-H.; Do, S.-H.; Shin, H.-J. The Effect of Peripheral Nerve Block on Postoperative Delirium in Older Adults Undergoing Hip Surgery: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Clin. Med. 2023, 12, 2459. [Google Scholar] [CrossRef]
- Li, T.; Dong, T.; Cui, Y.; Meng, X.; Dai, Z. Effect of regional anesthesia on the postoperative delirium: A systematic review and meta-analysis of randomized controlled trials. Front. Surg. 2022, 9, 937293. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. J. Clin. Epidemiol. 2009, 62, 1006–1012. [Google Scholar] [CrossRef]
- Wan, X.; Wang, W.; Liu, J.; Tong, T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med. Res. Methodol. 2014, 14, 135. [Google Scholar] [CrossRef]
- Higgins, J.P.; Altman, D.G.; Gotzsche, P.C.; Juni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.; et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef]
- Shim, J.G.; Ryu, K.H.; Kim, P.O.; Cho, E.A.; Ahn, J.H.; Yeon, J.E.; Lee, S.H.; Kang, D.Y. Evaluation of ultrasound-guided erector spinae plane block for postoperative management of video-assisted thoracoscopic surgery: A prospective, randomized, controlled clinical trial. J. Thorac. Dis. 2020, 12, 4174–4182. [Google Scholar] [CrossRef] [PubMed]
- Heng, L.; Wang, M.; Wang, M.; Li, L.; Zhu, S. Thoracic Paravertebral Block Ameliorates Postoperative Delirium in Geriatric Patients. Thorac. Cardiovasc. Surg. 2021, 70, 439–444. [Google Scholar] [CrossRef] [PubMed]
- Jin, L.; Yao, R.; Heng, L.; Pang, B.; Sun, F.G.; Shen, Y.; Zhong, J.F.; Zhao, P.P.; Wu, C.Y.; Li, B.P. Ultrasound-guided continuous thoracic paravertebral block alleviates postoperative delirium in elderly patients undergoing esophagectomy: A randomized controlled trial. Medicine 2020, 99, e19896. [Google Scholar] [CrossRef] [PubMed]
- Zhou, W.; Wang, B.; Cai, X.; Xu, Z. Effects of epidural block anesthesia combined with general anesthesia on cognitive function and analgesic effect after thoracoscopic surgery. Int. J. Clin. Exp. Med. 2020, 13, 8966–8973. [Google Scholar]
- Xie, H.; Zhou, J.; Du, W.; Zhang, S.; Huang, R.; Han, Q.; Guo, Q. Impact of thoracic paravertebral block combined with general anesthesia on postoperative cognitive function and serum adiponectin levels in elderly patients undergoing lobectomy. Videosurg. Other Miniinvasive Tech. 2019, 14, 538–544. [Google Scholar] [CrossRef]
- Wang, Y.; Cheng, J.; Yang, L.; Wang, J.; Liu, H.; Lv, Z. Ropivacaine for Intercostal Nerve Block Improves Early Postoperative Cognitive Dysfunction in Patients Following Thoracotomy for Esophageal Cancer. Med. Sci. Monit. 2019, 25, 460–465. [Google Scholar] [CrossRef]
- Silverstein, J.H.; Deiner, S.G. Perioperative delirium and its relationship to dementia. Prog. Neuropsychopharmacol. Biol. Psychiatry 2013, 43, 108–115. [Google Scholar] [CrossRef]
- Liang, C.K.; Chu, C.L.; Chou, M.Y.; Lin, Y.T.; Lu, T.; Hsu, C.J.; Chen, L.K. Interrelationship of postoperative delirium and cognitive impairment and their impact on the functional status in older patients undergoing orthopaedic surgery: A prospective cohort study. PLoS ONE 2014, 9, e110339. [Google Scholar] [CrossRef]
- Cerejeira, J.; Firmino, H.; Vaz-Serra, A.; Mukaetova-Ladinska, E.B. The neuroinflammatory hypothesis of delirium. Acta Neuropathol. 2010, 119, 737–754. [Google Scholar] [CrossRef]
- Campos, A.C.P.; Antunes, G.F.; Matsumoto, M.; Pagano, R.L.; Martinez, R.C.R. Neuroinflammation, Pain and Depression: An Overview of the Main Findings. Front. Psychol. 2020, 11, 1825. [Google Scholar] [CrossRef]
- Bagry, H.; de la Cuadra Fontaine, J.C.; Asenjo, J.F.; Bracco, D.; Carli, F. Effect of a continuous peripheral nerve block on the inflammatory response in knee arthroplasty. Reg. Anesth. Pain. Med. 2008, 33, 17–23. [Google Scholar] [CrossRef]
- Mejia-Terrazas, G.E.; Ruiz-Suarez, M.; Vadillo-Ortega, F.; Franco, Y.B.R.E.; Lopez-Munoz, E. Effect of interscalene nerve block on the inflammatory response in shoulder surgery: A randomized trial. J. Shoulder Elb. Surg. 2019, 28, e291–e303. [Google Scholar] [CrossRef]
- Wang, H.; Zhang, L.; Zhang, Z.; Li, Y.; Luo, Q.; Yuan, S.; Yan, F. Perioperative Sleep Disturbances and Postoperative Delirium in Adult Patients: A Systematic Review and Meta-Analysis of Clinical Trials. Front. Psychiatry 2020, 11, 570362. [Google Scholar] [CrossRef] [PubMed]
- He, E.; Dong, Y.; Jia, H.; Yu, L. Relationship of sleep disturbance and postoperative delirium: A systematic review and meta-analysis. Gland. Surg. 2022, 11, 1192–1203. [Google Scholar] [CrossRef] [PubMed]
- Olofsson, K.; Alling, C.; Lundberg, D.; Malmros, C. Abolished circadian rhythm of melatonin secretion in sedated and artificially ventilated intensive care patients. Acta Anaesthesiol. Scand. 2004, 48, 679–684. [Google Scholar] [CrossRef] [PubMed]
- Herrero Babiloni, A.; De Koninck, B.P.; Beetz, G.; De Beaumont, L.; Martel, M.O.; Lavigne, G.J. Sleep and pain: Recent insights, mechanisms, and future directions in the investigation of this relationship. J. Neural Transm. 2020, 127, 647–660. [Google Scholar] [CrossRef] [PubMed]
- Yang, D.-F.; Huang, W.-C.; Wu, C.W.; Huang, C.-Y.; Yang, Y.-C.S.H.; Tung, Y.-T. Acute sleep deprivation exacerbates systemic inflammation and psychiatry disorders through gut microbiota dysbiosis and disruption of circadian rhythms. Microbiol. Res. 2023, 268, 127292. [Google Scholar] [CrossRef] [PubMed]
- van der Woude, M.C.; Bormans, L.; van der Horst, R.P.; Sosef, M.N.; Belgers, H.J.; Hemmes, S.N.; Tuip-de Boer, A.; de Abreu, M.G.; Pelosi, P.; Spronk, P.E. Pulmonary levels of biomarkers for inflammation and lung injury in protective versus conventional one-lung ventilation for oesophagectomy: A randomised clinical trial. Eur. J. Anaesthesiol. 2020, 37, 1040–1049. [Google Scholar] [CrossRef] [PubMed]
- Verdonk, F.; Einhaus, J.; Tsai, A.S.; Hedou, J.; Choisy, B.; Gaudilliere, D.; Kin, C.; Aghaeepour, N.; Angst, M.S.; Gaudilliere, B. Measuring the human immune response to surgery: Multiomics for the prediction of postoperative outcomes. Curr. Opin. Crit. Care 2021, 27, 717–725. [Google Scholar] [CrossRef]
- Sommer, C.; Leinders, M.; Üçeyler, N. Inflammation in the pathophysiology of neuropathic pain. Pain 2018, 159, 595–602. [Google Scholar] [CrossRef] [PubMed]
- Rahbar, E.; Cardenas, J.C.; Baimukanova, G.; Usadi, B.; Bruhn, R.; Pati, S.; Ostrowski, S.R.; Johansson, P.I.; Holcomb, J.B.; Wade, C.E. Endothelial glycocalyx shedding and vascular permeability in severely injured trauma patients. J. Transl. Med. 2015, 13, 117. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.-Y.; Li, M.; Wang, P.; Fang, P. Goal-directed therapy based on rScO2 monitoring in elderly patients with one-lung ventilation: A randomized trial on perioperative inflammation and postoperative delirium. Trials 2022, 23, 687. [Google Scholar] [CrossRef] [PubMed]
- Devinney, M.J.; Wong, M.K.; Wright, M.C.; Marcantonio, E.R.; Terrando, N.; Browndyke, J.N.; Whitson, H.E.; Cohen, H.J.; Nackley, A.G.; Klein, M.E.; et al. Role of Blood–Brain Barrier Dysfunction in Delirium following Non-cardiac Surgery in Older Adults. Ann. Neurol. 2023, 94, 1024–1035. [Google Scholar] [CrossRef]
- Campos, M.G.; Peixoto, A.R.; Fonseca, S.; Santos, F.; Pinho, C.; Leite, D. Assessment of main complications of regional anesthesia recorded in an acute pain unit in a tertiary care university hospital: A retrospective cohort. Braz. J. Anesthesiol. 2022, 72, 605–613. [Google Scholar] [CrossRef]
- Niesen, A.D.; Jacob, A.K.; Law, L.A.; Sviggum, H.P.; Johnson, R.L. Complication rate of ultrasound-guided paravertebral block for breast surgery. Reg. Anesth. Pain. Med. 2020, 45, 813–817. [Google Scholar] [CrossRef]
- Manassero, A.; Bossolasco, M.; Carrega, M.; Coletta, G. Postoperative Thoracic Epidural Analgesia: Adverse Events from a Single-Center Series of 3126 Patients. Local Reg. Anesth. 2020, 13, 111–119. [Google Scholar] [CrossRef]
- Sanfilippo, F.; La Via, L.; Tigano, S.; Morgana, A.; Rosa, V.; Astuto, M. Trial Sequential Analysis: The evaluation of the robustness of meta-analyses findings and the need for further research. EuroMediterranean Biomed. J. 2021, 16, 104–107. [Google Scholar] [CrossRef]
- De Cassai, A.; Pasin, L.; Boscolo, A.; Salvagno, M.; Navalesi, P. Trial sequential analysis: Plain and simple. Korean J. Anesthesiol. 2020, 74, 363–365. [Google Scholar] [CrossRef] [PubMed]
| Author (Year) | Group | N (Block/Control) | Nerve Block | Control Arm | Age (Block/Control) | Diagnosis | Diagnostic Tool of Cognitive Function | Types of Surgery | Pain Score | Postoperative Pain Control |
|---|---|---|---|---|---|---|---|---|---|---|
| Wei (2022) [8] | 2 | 50/50 | US-TPVB | No block | 76.2/73.5 | Delirium | CAM | VATS | VAS | IV-PCA |
| Heng (2021) [25] | 2 | 64/64 | US-TPVB | No block | 70.3/69.7 | Delirium | NDSS | VATS | VAS | IV-PCA |
| Jin (2020) [26] | 2 | 90/90 | US-TPVB | No block | 70.8/71.4 | Delirium | CAM | Thoracotomy for esophageal cancer | NRS | IV-PCA |
| Strike (2019) [9] | 2 | 22/22 | US-TPVB | No block | 82.3/81.7 | Delirium | CAM | Thoracotomy for TAVR | VAS | IV-PCA |
| Zhou (2020) [27] | 2 | 41/41 | EB | No block | 56.7/56.3 | POCD | MMSE | VATS | VAS | No information |
| Xie (2019) [28] | 3 | 37/39 36/39 | US-TPVB EB | No block No block | 75.1/76.6 76.1/76.6 | POCD | MMSE | VATS | VAS | IV-PCA IV-PCA |
| Wang (2019) [29] | 2 | 50/50 | ICNB | No block | 45.3/44.9 | POCD | MMSE | Thoracotomy for esophageal cancer | VAS | No information |
| Author (Year) | Nerve Block | Block Technique | Local Anesthetics | Volume of Local Anesthetics | Injected Adjuncts of Block | Method of Block Confirmation | Postoperative Pain Control |
|---|---|---|---|---|---|---|---|
| Wei (2022) [8] | US-TPVB | Continuous | 0.2% Ropivacaine | 2 mL/h | None | Ultrasound-guided | IV-PCA |
| Heng (2021) [25] | US-TPVB | Continuous | 0.5% Ropivacaine | 20 mL 2 mL/h | None | Ultrasound-guided | IV-PCA |
| Jin (2020) [26] | US-TPVB | Continuous | 0.375% Ropivacaine | 15–20 mL 10 mL/6 h | 10 ug of sufentanil | Ultrasound-guided | IV-PCA |
| Strike (2019) [9] | US-TPVB | Continuous | 0.2% Ropivacaine or 0.125% Bupivacaine | 5–8 mL 5–10 mL/h | None | Ultrasound-guided | IV-PCA |
| Zhou (2020) [27] | EB | Continuous | 0.75% Ropivacaine | 0.12 mL/kg | 3 mL of 2% lidocaine | 15 min of observation | No information |
| Xie (2019) [28] | US-TPVB EB | Single shot Single shot | 0.25% Ropivacaine 0.375% Ropivacaine | 20 mL 8–15 mL | None | Ultrasound-guided | IV-PCA IV-PCA |
| Wang (2019) [29] | ICNB | Single shot | 0.5% Ropivacaine | 15 mL | None | No information | No information |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.Y.; Lee, J.; Na, H.-S.; Koo, B.-W.; Lee, K.O.; Shin, H.-J. The Impact of Regional Nerve Blocks on Postoperative Delirium or Cognitive Dysfunction following Thoracic Surgery: A Systematic Review and Meta-Analysis. J. Clin. Med. 2023, 12, 7576. https://doi.org/10.3390/jcm12247576
Kim SY, Lee J, Na H-S, Koo B-W, Lee KO, Shin H-J. The Impact of Regional Nerve Blocks on Postoperative Delirium or Cognitive Dysfunction following Thoracic Surgery: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2023; 12(24):7576. https://doi.org/10.3390/jcm12247576
Chicago/Turabian StyleKim, Su Yeon, Jiyoun Lee, Hyo-Seok Na, Bon-Wook Koo, Keum O Lee, and Hyun-Jung Shin. 2023. "The Impact of Regional Nerve Blocks on Postoperative Delirium or Cognitive Dysfunction following Thoracic Surgery: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 12, no. 24: 7576. https://doi.org/10.3390/jcm12247576
APA StyleKim, S. Y., Lee, J., Na, H.-S., Koo, B.-W., Lee, K. O., & Shin, H.-J. (2023). The Impact of Regional Nerve Blocks on Postoperative Delirium or Cognitive Dysfunction following Thoracic Surgery: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 12(24), 7576. https://doi.org/10.3390/jcm12247576





