Incidence and Timing of Immune-Related Adverse Events in Immune-Checkpoint Inhibitor-Treated Patients: A Retrospective Observational Study
Abstract
:1. Introduction
2. Materials and Methods
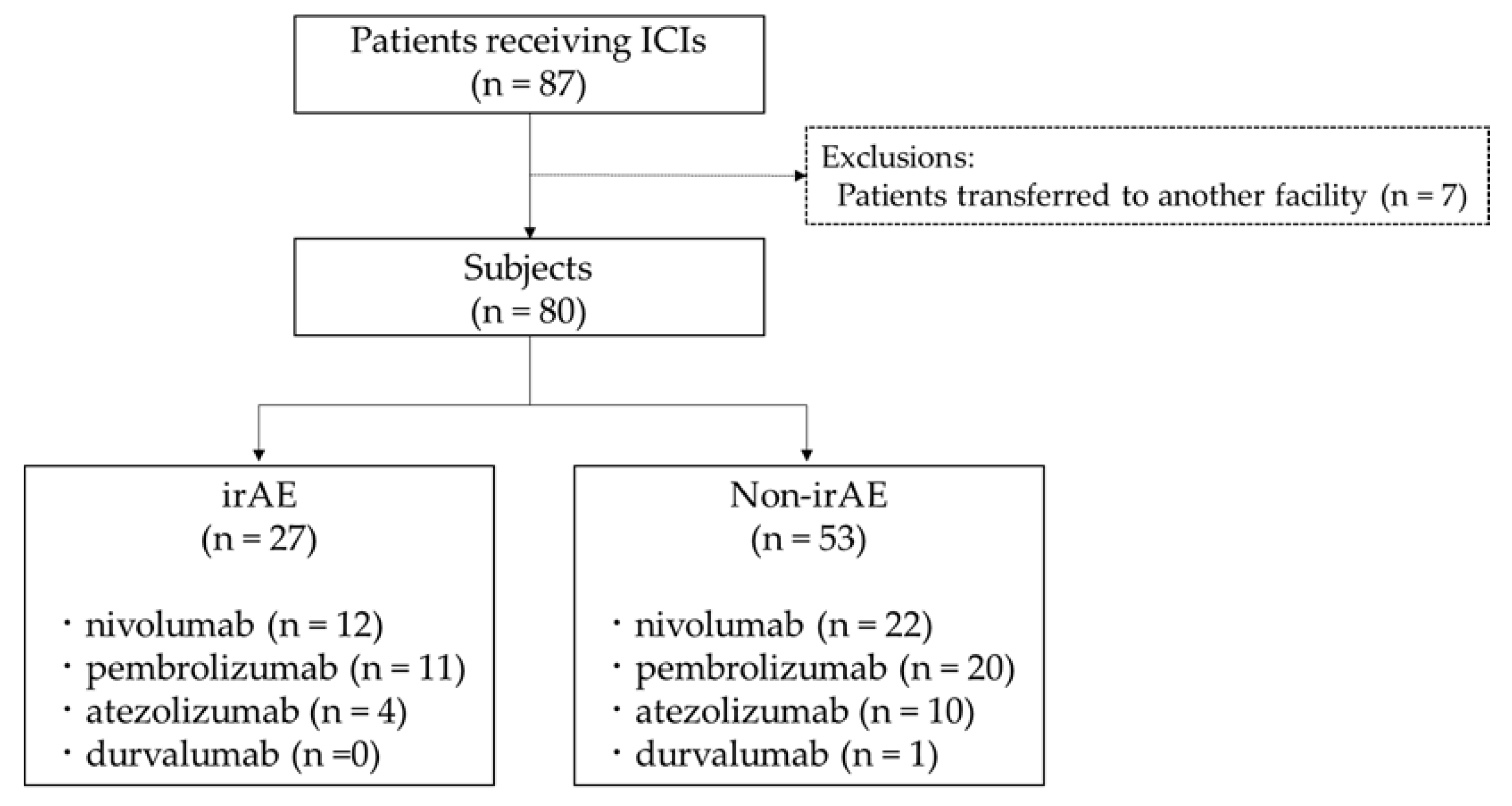
2.1. Study Patients
2.2. Clinical Characteristics
2.3. Definitions
2.4. Statistical Analysis
3. Results
3.1. Incidence of irAEs
3.2. Patterns of irAE Manifestation
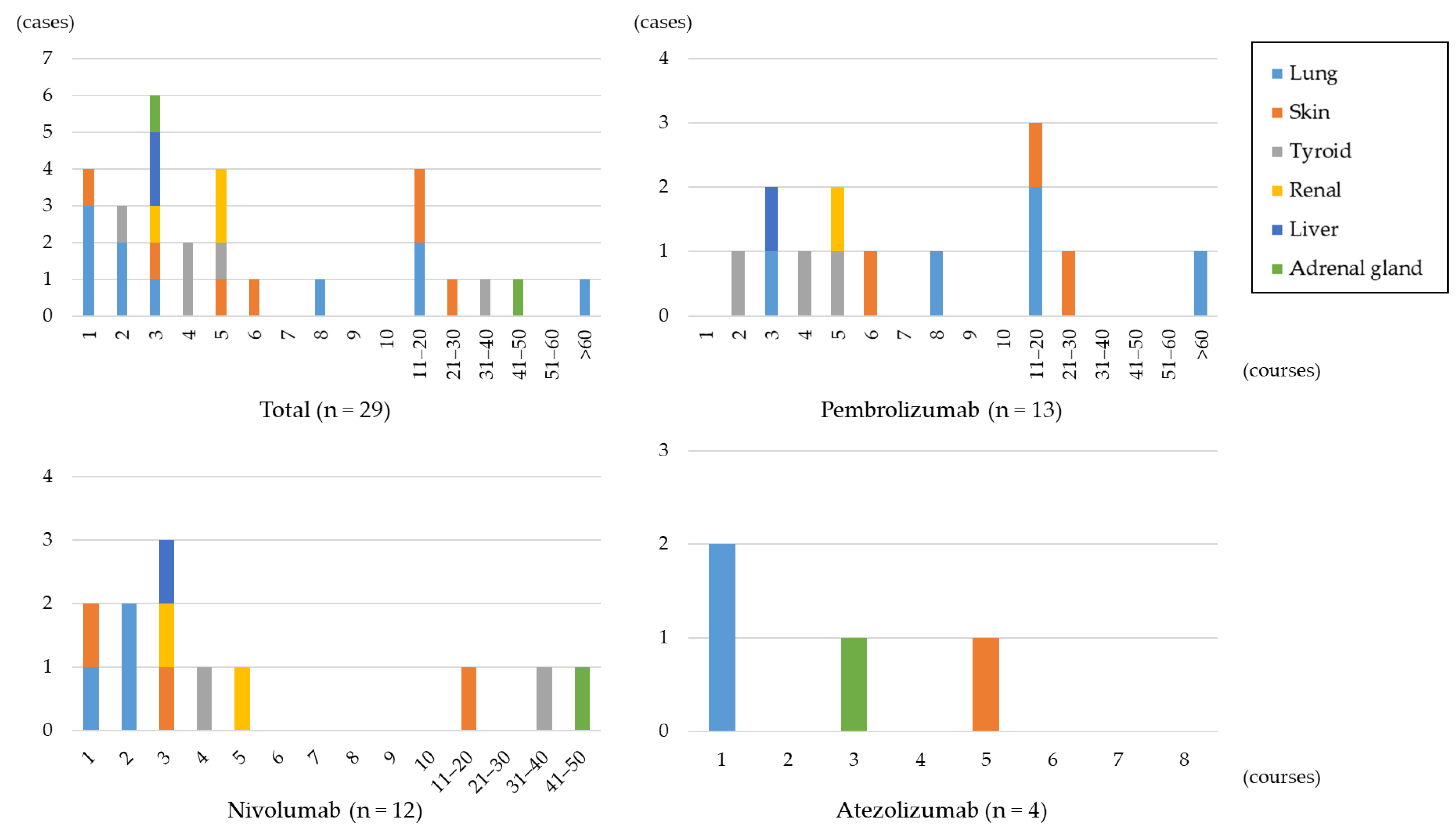
3.3. Timing of irAEs
3.4. Clinical Characteristics between irAE Group and Non-irAE Group
3.5. Grade of irAEs, Treatment for irAEs, and Subsequent Cancer Therapy for irAE Group
4. Discussion
4.1. Incidence Rate and Timing of irAE
4.2. Symptoms of irAEs
4.2.1. Pneumonitis
4.2.2. Thyroid Dysfunction
4.2.3. Dermatologic Adverse Event
4.2.4. Hepatitis
4.2.5. Acute Kidney Injury
4.2.6. Adrenal Insufficiency
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Japanese Society of Medical Oncology. JSMO Cancer Immunotherapy Guidelines, 3rd ed.; Kanehara-Shuppan: Tokyo, Japan, 2023. [Google Scholar]
- Kadono, T. Immune-related adverse events by immune checkpoint inhibitors. Nihon Rinsho Meneki Gakkai Kaishi 2017, 40, 83–89. [Google Scholar] [CrossRef] [PubMed]
- Aimono, Y.; Kamoshida, T.; Kikuchi, S.; Kamata, E.; Abe, H.; Ogawa, T.; Suzuki, S.; Saitou, Y.; Aoyama, Y. Evaluation of Risk Factors for Immune-Related Adverse Events Associated with Treatment with Immune Checkpoint Inhibitors. Gan Kagaku Ryoho 2021, 48, 57–61. [Google Scholar]
- Wei, S.C.; Levine, J.H.; Cogdill, A.P.; Zhao, Y.; Anang, N.A.S.; Andrews, M.C.; Sharma, P.; Wang, J.; Wargo, J.A.; Pe’er, D.; et al. Distinct Cellular Mechanisms Underlie Anti-CTLA-4 and Anti-PD-1 Checkpoint Blockade. Cell 2017, 170, 1120–1133.e17. [Google Scholar] [CrossRef]
- Maruyama, M.; Umemura, M.; Sadamori, M. Frequency of Adverse Events Related to Immune Checkpoint Inhibitors (ICIs) and Causes for Treatment Discontinuation. Bull. Gifu Univ. Med. Sci. 2021, 15, 7–14. [Google Scholar]
- Kobayashi, T.; Iwama, S.; Yasuda, Y.; Okada, N.; Tsunekawa, T.; Onoue, T.; Takagi, H.; Hagiwara, D.; Ito, Y.; Morishita, Y.; et al. Patients with Antithyroid Antibodies Are Prone to Develop Destructive Thyroiditis by Nivolumab: A Prospective Study. J. Endocr. Soc. 2018, 2, 241–251. [Google Scholar] [CrossRef] [PubMed]
- Chen, D.S.; Mellman, I. Oncology meets immunology: The cancer-immunity cycle. Immunity 2013, 39, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Sharma, P.; Allison, J.P. The future of immune checkpoint therapy. Science 2015, 348, 56–61. [Google Scholar] [CrossRef] [PubMed]
- Pardoll, D.M. The blockade of immune checkpoints in cancer immunotherapy. Nat. Rev. Cancer 2012, 12, 252–264. [Google Scholar] [CrossRef]
- Postow, M.A. Managing immune checkpoint-blocking antibody side effects. Am. Soc. Clin. Oncol. Educ. Book 2015, 35, 76–83. [Google Scholar] [CrossRef]
- Xu, C.; Chen, Y.P.; Du, X.J.; Liu, J.Q.; Huang, C.L.; Chen, L.; Zhou, G.Q.; Li, W.F.; Mao, Y.P.; Hsu, C.; et al. Comparative safety of immune checkpoint inhibitors in cancer: Systematic review and network meta-analysis. BMJ 2018, 363, k4226. [Google Scholar] [CrossRef]
- Tang, S.Q.; Tang, L.L.; Mao, Y.P.; Li, W.F.; Chen, L.; Zhang, Y.; Guo, Y.; Liu, Q.; Sun, Y.; Xu, C.; et al. The Pattern of Time to Onset and Resolution of Immune-Related Adverse Events Caused by Immune Checkpoint Inhibitors in Cancer: A Pooled Analysis of 23 Clinical Trials and 8436 Patients. Cancer Res. Treat. 2021, 53, 339–354. [Google Scholar] [CrossRef] [PubMed]
- Khunger, M.; Rakshit, S.; Pasupuleti, V.; Hernandez, A.V.; Mazzone, P.; Stevenson, J.; Pennell, N.A.; Velcheti, V. Incidence of Pneumonitis With Use of Programmed Death 1 and Programmed Death-Ligand 1 Inhibitors in Non-Small Cell Lung Cancer: A Systematic Review and Meta-Analysis of Trials. Chest 2017, 152, 271–281. [Google Scholar] [CrossRef] [PubMed]
- Nishino, M.; Giobbie-Hurder, A.; Hatabu, H.; Ramaiya, N.H.; Hodi, F.S. Incidence of Programmed Cell Death 1 Inhibitor-Related Pneumonitis in Patients With Advanced Cancer: A Systematic Review and Meta-analysis. JAMA Oncol. 2016, 2, 1607–1616. [Google Scholar] [CrossRef] [PubMed]
- Postow, M.A.; Chesney, J.; Pavlick, A.C.; Robert, C.; Grossmann, K.; McDermott, D.; Linette, G.P.; Meyer, N.; Giguere, J.K.; Agarwala, S.S.; et al. Nivolumab and ipilimumab versus ipilimumab in untreated melanoma. N. Engl. J. Med. 2015, 372, 2006–2017. [Google Scholar] [CrossRef] [PubMed]
- Naidoo, J.; Wang, X.; Woo, K.M.; Iyriboz, T.; Halpenny, D.; Cunningham, J.; Chaft, J.E.; Segal, N.H.; Callahan, M.K.; Lesokhin, A.M.; et al. Pneumonitis in Patients Treated With Anti-Programmed Death-1/Programmed Death Ligand 1 Therapy. J. Clin. Oncol. 2017, 35, 709–717. [Google Scholar] [CrossRef]
- Kubo, K.; Azuma, A.; Kanazawa, M.; Kameda, H.; Kusumoto, M.; Genma, A.; Saijo, Y.; Sakai, F.; Sugiyama, Y.; Tatsumi, K.; et al. Consensus statement for the diagnosis and treatment of drug-induced lung injuries. Respir. Investig. 2013, 51, 260–277. [Google Scholar] [CrossRef]
- Socinski, M.A.; Jotte, R.M.; Cappuzzo, F.; Orlandi, F.; Stroyakovskiy, D.; Nogami, N.; Rodríguez-Abreu, D.; Moro-Sibilot, D.; Thomas, C.A.; Barlesi, F.; et al. Atezolizumab for First-Line Treatment of Metastatic Nonsquamous NSCLC. N. Engl. J. Med. 2018, 378, 2288–2301. [Google Scholar] [CrossRef]
- de Filette, J.; Andreescu, C.E.; Cools, F.; Bravenboer, B.; Velkeniers, B. A Systematic Review and Meta-Analysis of Endocrine-Related Adverse Events Associated with Immune Checkpoint Inhibitors. Horm. Metab. Res. 2019, 51, 145–156. [Google Scholar] [CrossRef]
- de Filette, J.; Jansen, Y.; Schreuer, M.; Everaert, H.; Velkeniers, B.; Neyns, B.; Bravenboer, B. Incidence of Thyroid-Related Adverse Events in Melanoma Patients Treated With Pembrolizumab. J. Clin. Endocrinol. Metab. 2016, 101, 4431–4439. [Google Scholar] [CrossRef]
- Cukier, P.; Santini, F.C.; Scaranti, M.; Hoff, A.O. Endocrine side effects of cancer immunotherapy. Endocr. Relat. Cancer 2017, 24, T331–T347. [Google Scholar] [CrossRef]
- Geisler, A.N.; Phillips, G.S.; Barrios, D.M.; Wu, J.; Leung, D.Y.M.; Moy, A.P.; Kern, J.A.; Lacouture, M.E. Immune checkpoint inhibitor-related dermatologic adverse events. J. Am. Acad. Dermatol. 2020, 83, 1255–1268. [Google Scholar] [CrossRef]
- Coleman, E.L.; Olamiju, B.; Leventhal, J.S. The life-threatening eruptions of immune checkpoint inhibitor therapy. Clin. Dermatol. 2020, 38, 94–104. [Google Scholar] [CrossRef]
- Paz-Ares, L.; Ciuleanu, T.E.; Cobo, M.; Schenker, M.; Zurawski, B.; Menezes, J.; Richardet, E.; Bennouna, J.; Felip, E.; Juan-Vidal, O.; et al. First-line nivolumab plus ipilimumab combined with two cycles of chemotherapy in patients with non-small-cell lung cancer (CheckMate 9LA): An international, randomised, open-label, phase 3 trial. Lancet Oncol. 2021, 22, 198–211. [Google Scholar] [CrossRef]
- McDermott, D.F.; Sosman, J.A.; Sznol, M.; Massard, C.; Gordon, M.S.; Hamid, O.; Powderly, J.D.; Infante, J.R.; Fassò, M.; Wang, Y.V.; et al. Atezolizumab, an Anti-Programmed Death-Ligand 1 Antibody, in Metastatic Renal Cell Carcinoma: Long-Term Safety, Clinical Activity, and Immune Correlates From a Phase Ia Study. J. Clin. Oncol. 2016, 34, 833–842. [Google Scholar] [CrossRef]
- Postow, M.A.; Sidlow, R.; Hellmann, M.D. Immune-Related Adverse Events Associated with Immune Checkpoint Blockade. N. Engl. J. Med. 2018, 378, 158–168. [Google Scholar] [CrossRef]
- Sibaud, V. Dermatologic Reactions to Immune Checkpoint Inhibitors: Skin Toxicities and Immunotherapy. Am. J. Clin. Dermatol. 2018, 19, 345–361. [Google Scholar] [CrossRef]
- Reynolds, K.; Thomas, M.; Dougan, M. Diagnosis and Management of Hepatitis in Patients on Checkpoint Blockade. Oncologist 2018, 23, 991–997. [Google Scholar] [CrossRef]
- Cortazar, F.B.; Marrone, K.A.; Troxell, M.L.; Ralto, K.M.; Hoenig, M.P.; Brahmer, J.R.; Le, D.T.; Lipson, E.J.; Glezerman, I.G.; Wolchok, J.; et al. Clinicopathological features of acute kidney injury associated with immune checkpoint inhibitors. Kidney Int. 2016, 90, 638–647. [Google Scholar] [CrossRef]
- Seethapathy, H.; Zhao, S.; Chute, D.F.; Zubiri, L.; Oppong, Y.; Strohbehn, I.; Cortazar, F.B.; Leaf, D.E.; Mooradian, M.J.; Villani, A.C.; et al. The Incidence, Causes, and Risk Factors of Acute Kidney Injury in Patients Receiving Immune Checkpoint Inhibitors. Clin. J. Am. Soc. Nephrol. 2019, 14, 1692–1700. [Google Scholar] [CrossRef]
- Cortazar, F.B.; Kibbelaar, Z.A.; Glezerman, I.G.; Abudayyeh, A.; Mamlouk, O.; Motwani, S.S.; Murakami, N.; Herrmann, S.M.; Manohar, S.; Shirali, A.C.; et al. Clinical Features and Outcomes of Immune Checkpoint Inhibitor-Associated AKI: A Multicenter Study. J. Am. Soc. Nephrol. 2020, 31, 435–446. [Google Scholar] [CrossRef]
- Grouthier, V.; Lebrun-Vignes, B.; Moey, M.; Johnson, D.B.; Moslehi, J.J.; Salem, J.E.; Bachelot, A. Immune Checkpoint Inhibitor-Associated Primary Adrenal Insufficiency: WHO VigiBase Report Analysis. Oncologist 2020, 25, 696–701. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, A.; Saito, Y.; Okamoto, K.; Narumi, K.; Furugen, A.; Takekuma, Y.; Sugawara, M.; Kobayashi, M. Preexisting autoimmune disease is a risk factor for immune-related adverse events: A meta-analysis. Support Care Cancer 2021, 29, 7747–7753. [Google Scholar] [CrossRef] [PubMed]

| irAE | Non-irAE | p-Value | ||||
|---|---|---|---|---|---|---|
| Clinical Characteristics | n = 27 | n = 53 | ||||
| Male gender | 21 | (77.8) | 40 | (75.5) | 0.819 | |
| Age (years) a | 68 | (65–78) | 71 | (65–76) | 0.963 | |
| BMI (kg/m2) a | 20.9 | (17.8–23.8) | 20.1 | (17.4–22.6) | 0.274 | |
| History of ILD | 3 | (11.1) | 4 | (7.6) | 0.683 | |
| History of COPD | 3 | (11.1) | 7 | (13.2) | >0.999 | |
| History of autoimmune disease | 1 | (3.7) | 1 | (1.9) | >0.999 | |
| PPI b | 6 | (22.2) | 15 | (28.3) | 0.559 | |
| Concomitant use of ipilimumab | 4 | (14.8) | 0 | (0) | 0.011 | |
| Anti-TPO antibody | 13 | (48.2) | 9 | (17.0) | 0.003 | |
| Anti-Tg antibody | 11 | (40.7) | 9 | (17.0) | 0.020 | |
| Laboratory data a | ||||||
| WBC (103/µL) | 6.6 | (5.1–8.6) | 6.7 | (5.4–9.9) | 0.665 | |
| RBC (104/µL) | 417 | (347–444) | 382 | (335–428) | 0.105 | |
| Hb (g/dL) | 12.3 | (10.2–14.0) | 11.2 | (10.0–12.6) | 0.100 | |
| PLT (104/µL) | 25.3 | (19.8–35.4) | 25.6 | (18.7–35.4) | 0.947 | |
| CCr (mL/min) | 60.9 | (46.5–85.2) | 53.5 | (41.9–71.5) | 0.114 | |
| eGFR (mL/min) | 69.6 | (50.9–85.0) | 63.7 | (47.4–76.2) | 0.255 | |
| T-Bil (mg/dL) | 0.6 | (0.5–1.0) | 0.6 | (0.4–0.8) | 0.201 | |
| AST (U/L) | 23 | (20–28) | 22 | (18–37) | 0.988 | |
| ALT (U/L) | 17 | (13–22) | 16 | (10–31) | 0.760 | |
| Patient ID a | Age | Gender | ICI | irAE (Organ) | Grade | Hospitalization Due to irAE | Discontinuation of ICI Treatment | Treatment for irAE | Subsequent Cancer Therapy |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 67 | M | NIVO | Lung | 3 | YES | YES | Prednisolone | None |
| 2 | 72 | M | NIVO | Lung | 2 | NO | YES | Prednisolone | None |
| 3 | 79 | M | NIVO | Lung | 2 | NO | YES | Prednisolone | Other chemotherapy |
| 4 | 67 | M | NIVO | Skin | 3 | NO | NO | Prednisolone | Continuation of NIVO |
| 5 | 77 | M | NIVO | Skin | 2 | NO | NO | Antihistamines | Continuation of NIVO |
| 6 | 66 | M | NIVO | Skin | 2 | NO | NO | Antihistamines | Continuation of NIVO |
| 7 | 77 | M | NIVO | Thyroid | 2 | NO | YES | Levothyroxine | None |
| 8 | 84 | M | NIVO | Thyroid | 2 | NO | YES | Levothyroxine | None |
| 9 | 28 | M | NIVO | Renal | 3 | YES | YES | Prednisolone | Resuming NIVO |
| 10 | 82 | F | NIVO | Renal | 2 | YES | YES | Ringer’s acetate solution | None |
| 11 | 66 | M | NIVO | Liver | 2 | NO | YES | UDCA | Resuming NIVO |
| 12 | 50 | F | NIVO | Adrenal gland | 1 | NO | NO | Hydrocortisone | Continuation of NIVO |
| 13 | 81 | M | PEMBRO | Lung | 3 | YES | YES | None | Changed to ATEZO |
| 14 | 78 | M | PEMBRO | Lung | 3 | YES | YES | Prednisolone | None |
| 15-2 | 62 | F | PEMBRO | Lung | 3 | YES | YES | Prednisolone | None |
| 16-2 | 58 | M | PEMBRO | Lung | 2 | YES | YES | Prednisolone | Other chemotherapy |
| 17 | 76 | F | PEMBRO | Lung | 2 | YES | YES | Prednisolone | None |
| 18 | 66 | M | PEMBRO | Skin | 2 | NO | NO | Topical steroids | Continuation of PEMBRO |
| 19 | 81 | M | PEMBRO | Skin | 2 | NO | NO | None | Continuation of PEMBRO |
| 20 | 67 | M | PEMBRO | Skin | 2 | NO | NO | Antihistamines | Continuation of PEMBRO |
| 21 | 63 | M | PEMBRO | Thyroid | 2 | NO | NO | Levothyroxine | Continuation of PEMBRO |
| 16-1 | 58 | M | PEMBRO | Thyroid | 2 | NO | NO | Levothyroxine | Continuation of PEMBRO |
| 15-1 | 62 | F | PEMBRO | Thyroid | 1 | NO | NO | None | Continuation of PEMBRO |
| 22 | 68 | F | PEMBRO | Renal | 2 | NO | YES | None | Resuming PEMBRO |
| 23 | 92 | M | PEMBRO | Liver | 2 | NO | YES | UDCA | None |
| 24 | 69 | M | ATEZO | Lung | 3 | YES | YES | Prednisolone | None |
| 25 | 65 | F | ATEZO | Lung | 2 | YES | YES | Prednisolone | Other chemotherapy |
| 26 | 72 | M | ATEZO | Skin | 1 | NO | YES | Topical steroids | Other chemotherapy |
| 27 | 62 | M | ATEZO | Adrenal gland | 1 | NO | YES | Hydrocortisone | None |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Masaki, K.; Miyazaki, M.; Kakimoto, H.; Fukiage, Y.; Fukue, H.; Nakashima, A.; Imakyure, O. Incidence and Timing of Immune-Related Adverse Events in Immune-Checkpoint Inhibitor-Treated Patients: A Retrospective Observational Study. J. Clin. Med. 2023, 12, 7564. https://doi.org/10.3390/jcm12247564
Masaki K, Miyazaki M, Kakimoto H, Fukiage Y, Fukue H, Nakashima A, Imakyure O. Incidence and Timing of Immune-Related Adverse Events in Immune-Checkpoint Inhibitor-Treated Patients: A Retrospective Observational Study. Journal of Clinical Medicine. 2023; 12(24):7564. https://doi.org/10.3390/jcm12247564
Chicago/Turabian StyleMasaki, Kou, Motoyasu Miyazaki, Hideki Kakimoto, Yuma Fukiage, Haruka Fukue, Akio Nakashima, and Osamu Imakyure. 2023. "Incidence and Timing of Immune-Related Adverse Events in Immune-Checkpoint Inhibitor-Treated Patients: A Retrospective Observational Study" Journal of Clinical Medicine 12, no. 24: 7564. https://doi.org/10.3390/jcm12247564
APA StyleMasaki, K., Miyazaki, M., Kakimoto, H., Fukiage, Y., Fukue, H., Nakashima, A., & Imakyure, O. (2023). Incidence and Timing of Immune-Related Adverse Events in Immune-Checkpoint Inhibitor-Treated Patients: A Retrospective Observational Study. Journal of Clinical Medicine, 12(24), 7564. https://doi.org/10.3390/jcm12247564






