Health-Related Quality of Life after Pediatric Traumatic Brain Injury: A Quantitative Comparison between Children’s and Parents’ Perspectives of the QOLIBRI-KID/ADO Questionnaire
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Sample
2.2. Measures and Data Collection
2.3. Ethical Approval
2.4. Data Analyses
2.4.1. Internal Consistency
2.4.2. Parent–Child Agreement for the QOLIBRI-KID/ADO
2.4.3. Factors Associated with Parent–Child Agreement Concerning HRQoL
3. Results
3.1. Study Sample
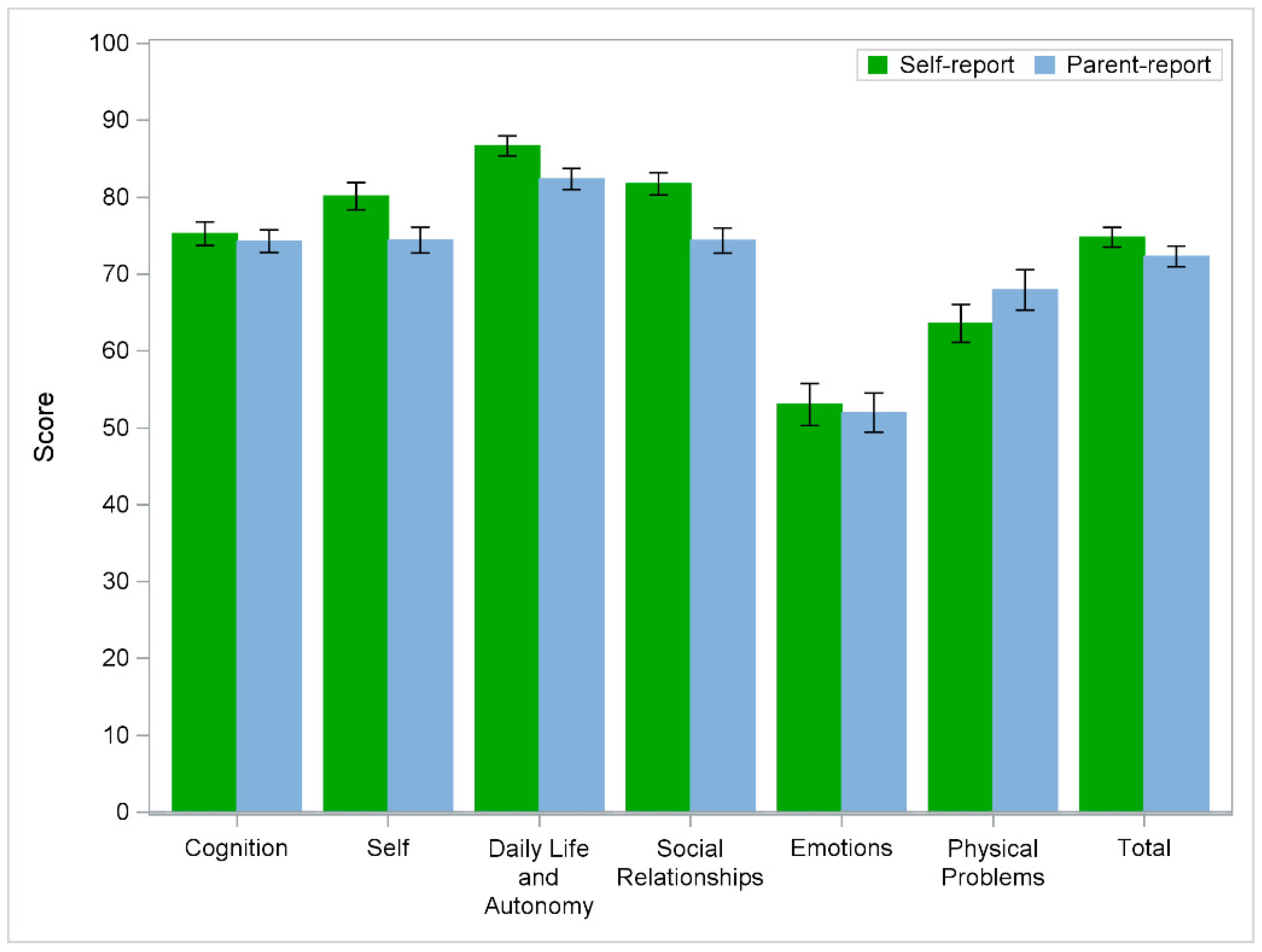
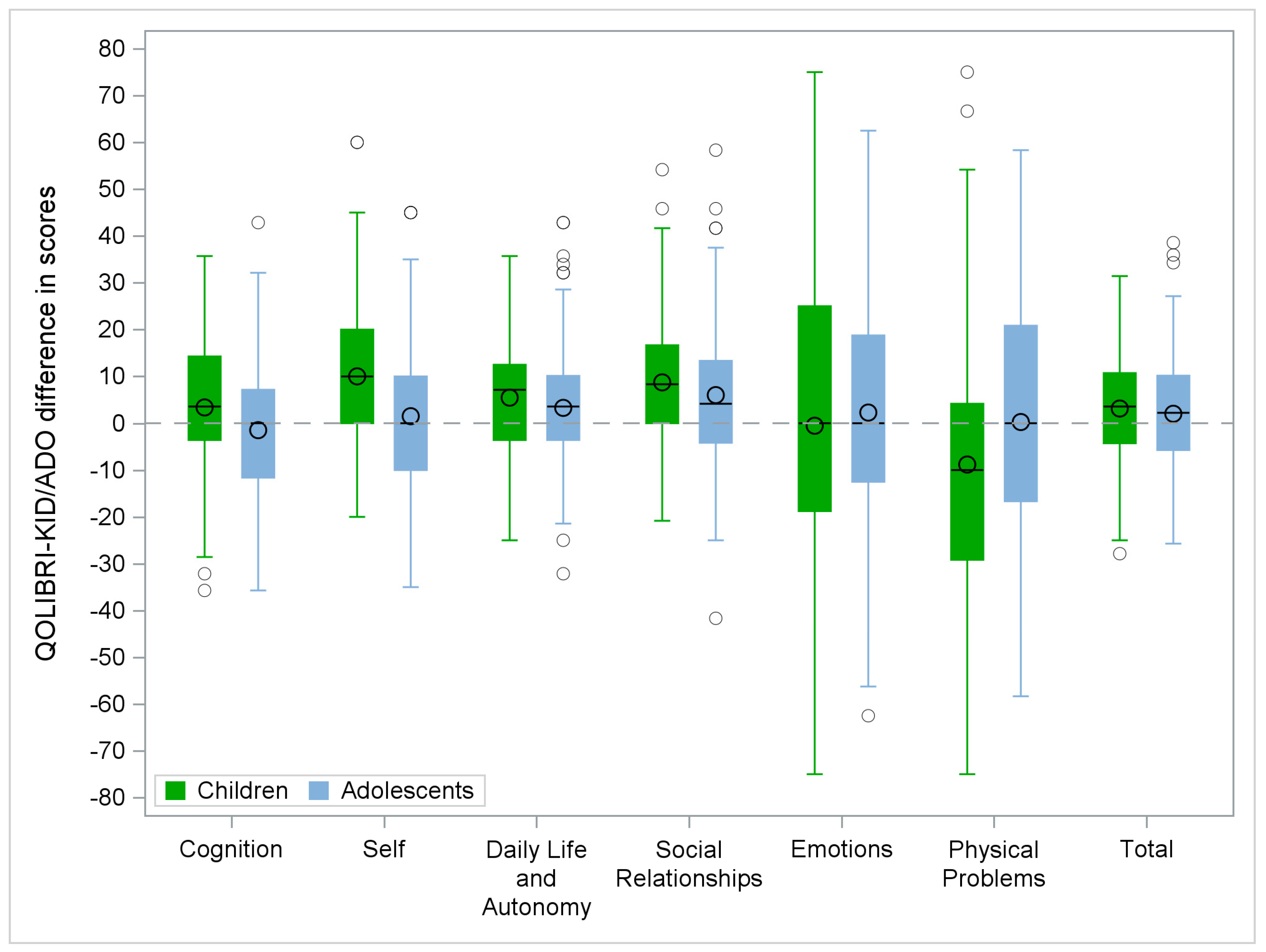
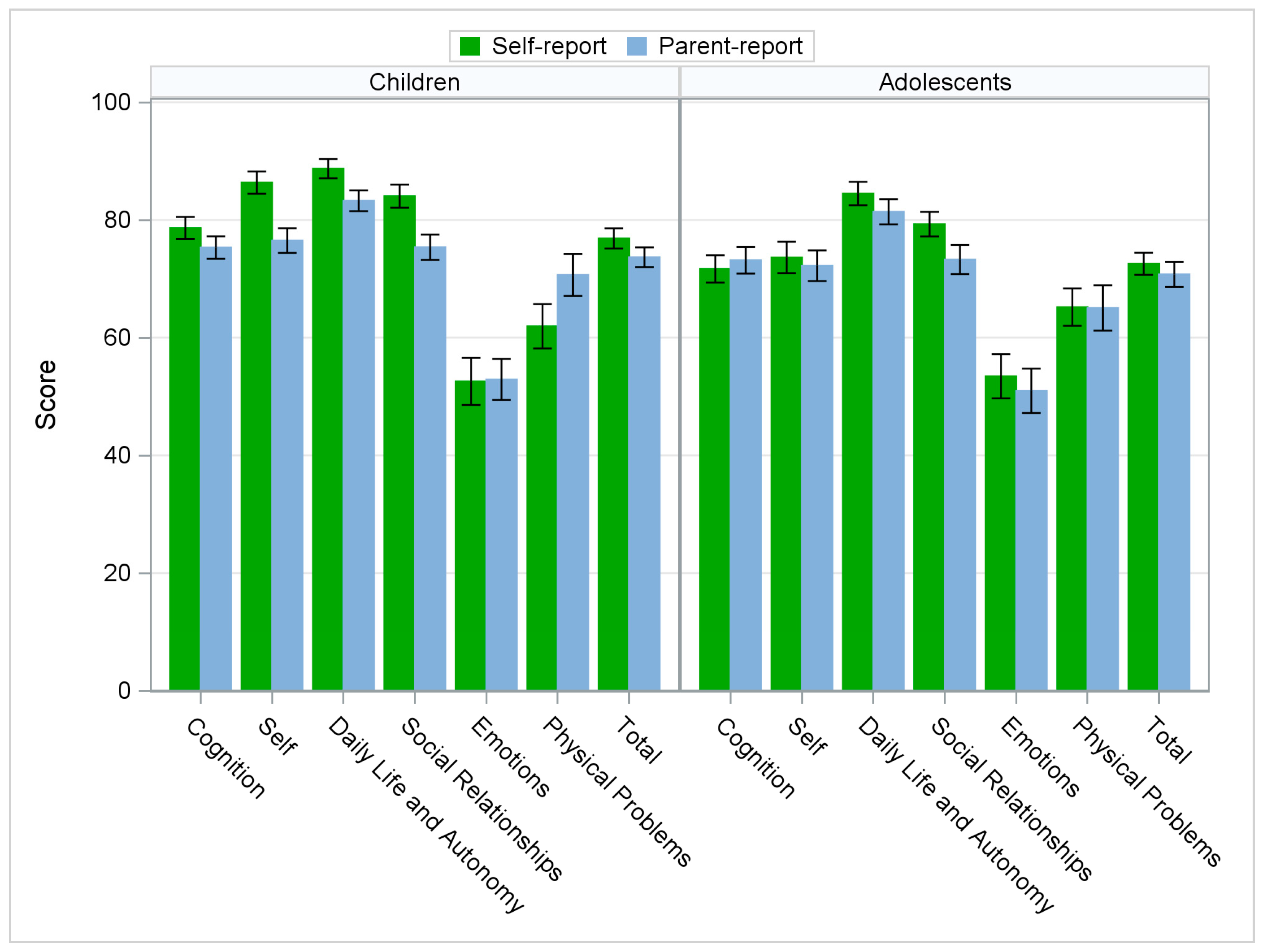
3.2. Descriptive Statistics of the QOLIBRI-KID/ADO Questionnaire
3.3. Data Analyses
3.3.1. Internal Consistency
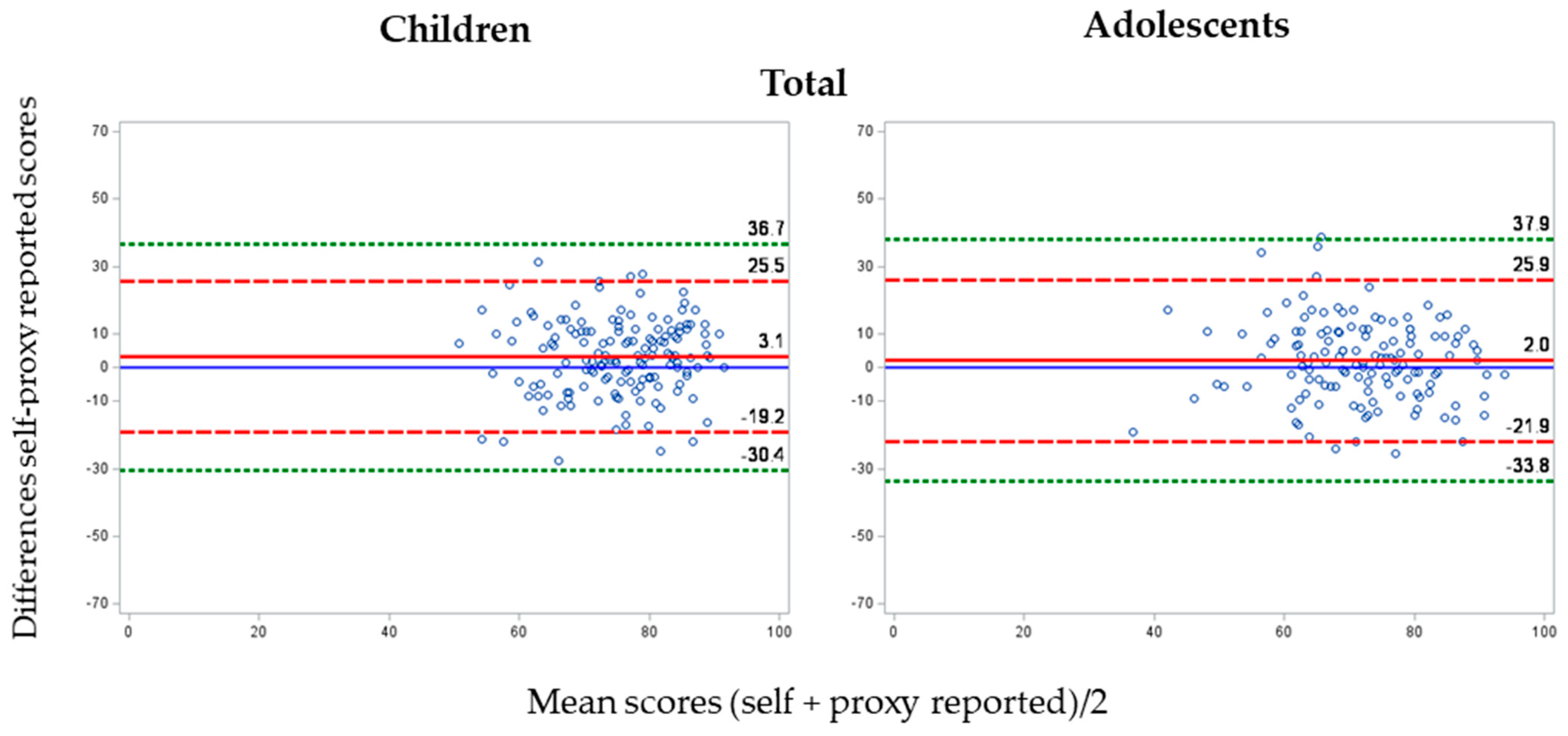
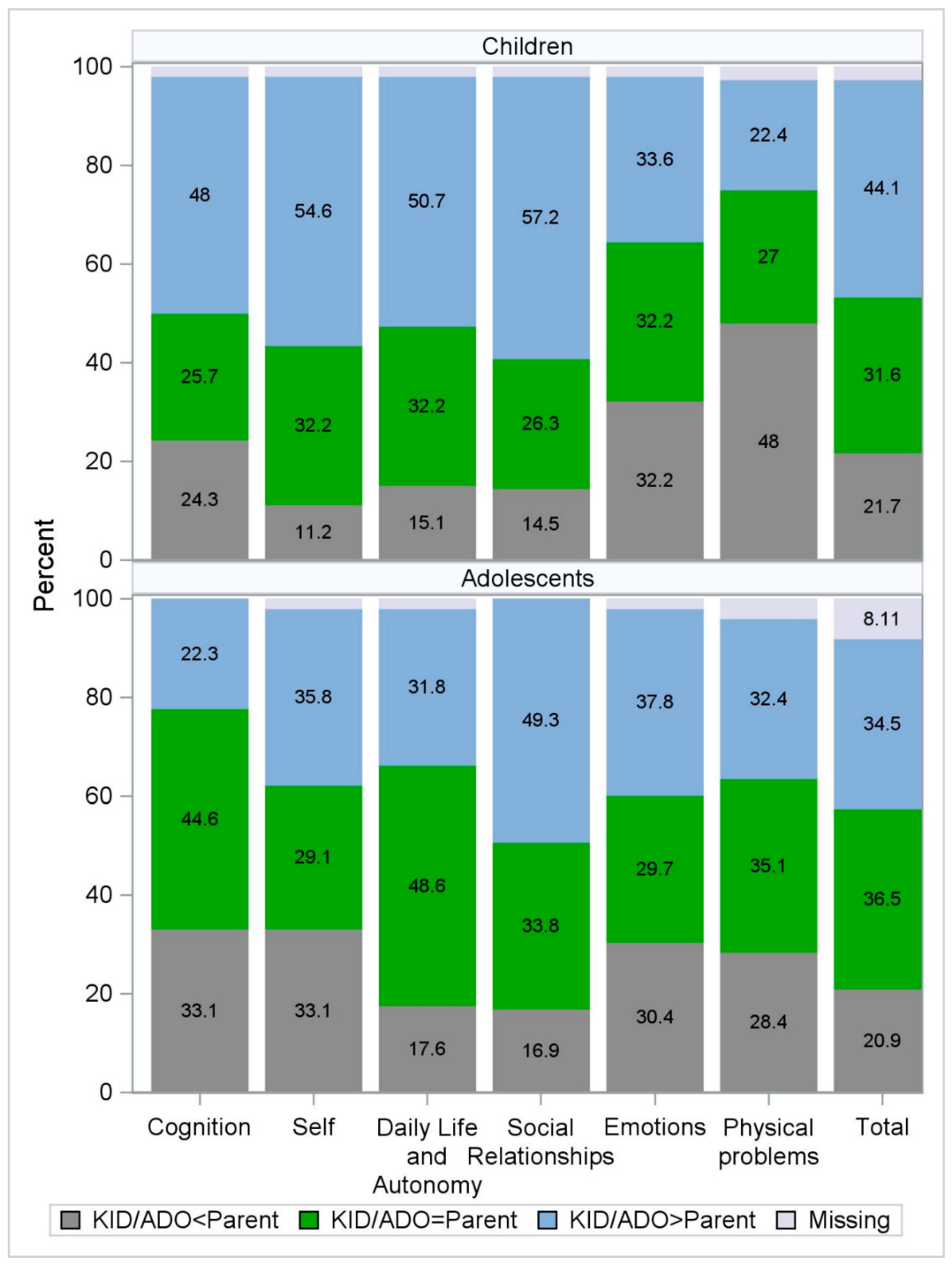
3.3.2. Parent–Child Agreement of the QOLIBRI-KID/ADO
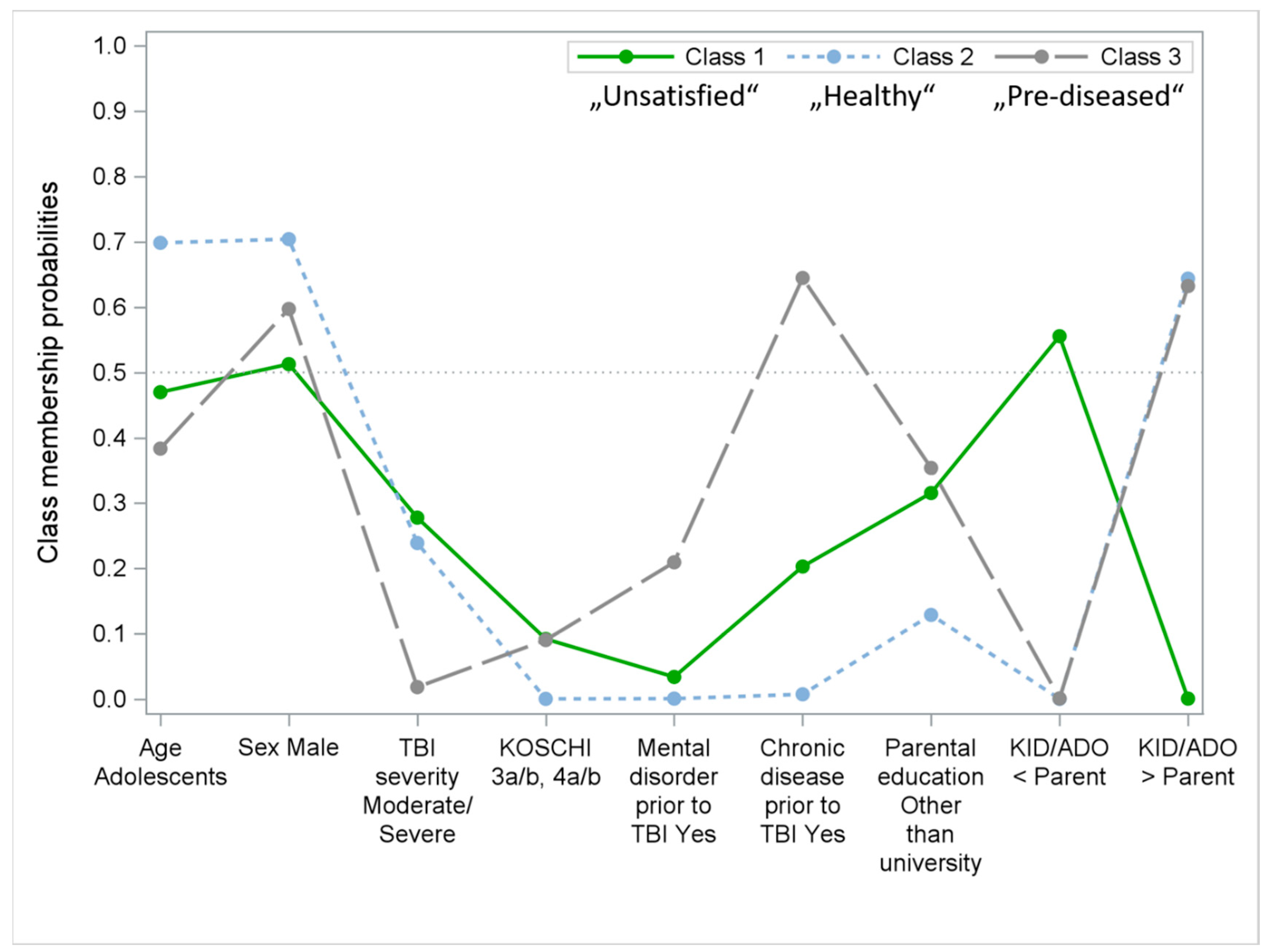
3.3.3. Factors Associated with Parent–Child Agreement Concerning HRQoL
4. Discussion
4.1. Strengths and Limitations
4.2. Recommendations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Self-Report | Parent Report | |||
|---|---|---|---|---|
| Mean (SD) | Missing | Mean (SD) | Missing | |
| Children (n = 152) | ||||
| Cognition | 78.6 (11.64) | 0 | 75.3 (11.77) | 3 |
| Self | 86.3 (11.83) | 0 | 76.5 (12.94) | 3 |
| Daily Life and Autonomy | 88.7 (10.20) | 0 | 83.3 (10.89) | 3 |
| Social Relationships | 84.0 (12.24) | 0 | 75.4 (13.29) | 3 |
| Emotions | 52.6 (25.02) | 0 | 52.9 (21.56) | 3 |
| Physical Problems | 61.9 (23.47) | 0 | 70.7 (22.00) | 4 |
| Total | 76.9 (10.71) | 0 | 73.7 (10.33) | 4 |
| Adolescents (n = 148) | ||||
| Cognition | 71.7 (14.29) | 0 | 73.1 (13.88) | 0 |
| Self | 73.6 (16.41) | 1 | 72.2 (15.91) | 2 |
| Daily Life and Autonomy | 84.5 (12.24) | 2 | 81.4 (13.09) | 1 |
| Social Relationships | 79.3 (12.85) | 0 | 73.3 (15.17) | 0 |
| Emotions | 53.4 (23.08) | 0 | 51.0 (22.94) | 3 |
| Physical Problems | 65.2 (19.58) | 0 | 65.0 (23.25) | 6 |
| Total | 72.6 (11.46) | 3 | 70.8 (12.61) | 9 |
Appendix B
| QOLIBRI-KID/ADO Scale | Children and Adolescents | Parents | ||||
|---|---|---|---|---|---|---|
| (n Items) | n | α | ω | n | A | ω |
| Cognition (7) | 293 | 0.70 | 0.71 | 290 | 0.76 | 0.75 |
| Self (4) | 294 | 0.78 | 0.80 | 284 | 0.75 | 0.75 |
| Daily Life and Autonomy (7) | 284 | 0.70 | 0.71 | 276 | 0.74 | 0.75 |
| Social Relationships (6) | 296 | 0.73 | 0.72 | 283 | 0.78 | 0.77 |
| Emotions (4) | 295 | 0.72 | 0.72 | 289 | 0.72 | 0.72 |
| Physical Problems (6) | 288 | 0.73 | 0.73 | 270 | 0.77 | 0.76 |
| Total (35) | 266 | 0.89 | 0.88 | 235 | 0.91 | 0.90 |
| Children | Parents | |||||
| n | α | ω | n | A | ω | |
| Cognition (7) | 152 | 0.64 | 0.63 | 146 | 0.71 | 0.73 |
| Self (4) | 151 | 0.68 | 0.68 | 145 | 0.69 | 0.66 |
| Daily Life and Autonomy (7) | 148 | 0.66 | 0.65 | 140 | 0.71 | 0.70 |
| Social Relationships (6) | 152 | 0.75 | 0.75 | 141 | 0.76 | 0.75 |
| Emotions (4) | 150 | 0.74 | 0.74 | 146 | 0.70 | 0.70 |
| Physical Problems (6) | 146 | 0.77 | 0.77 | 136 | 0.78 | 0.77 |
| Total (35) | 140 | 0.88 | 0.87 | 119 | 0.88 | 0.87 |
| Adolescents | Parents | |||||
| n | α | ω | n | A | ω | |
| Cognition (7) | 141 | 0.72 | 0.73 | 144 | 0.78 | 0.78 |
| Self (4) | 143 | 0.78 | 0.79 | 139 | 0.78 | 0.79 |
| Daily Life and Autonomy (7) | 136 | 0.73 | 0.74 | 136 | 0.77 | 0.78 |
| Social Relationships (6) | 144 | 0.68 | 0.68 | 142 | 0.79 | 0.78 |
| Emotions (4) | 145 | 0.70 | 0.71 | 143 | 0.73 | 0.73 |
| Physical Problems (6) | 142 | 0.68 | 0.65 | 134 | 0.76 | 0.75 |
| Total (35) | 126 | 0.89 | 0.88 | 116 | 0.92 | 0.91 |
Bland–Altman Plots


| QOLIBRI-KID/ADO Scales | Item | Children | Adolescents | ||
|---|---|---|---|---|---|
| Item Level Value (95% CI) | Scale Value (95% CI) | Item Level Value (95% CI) | Scale Value (95% CI) | ||
| Cognition | Concentration | 0.21 (0.094, 0.317) * | 0.23 (0.19, 0.277) * | 0.44 (0.333, 0.547) * | 0.31 (0.268, 0.352) * |
| Talking to others | 0.19 (0.064, 0.313) | 0.27 (0.159, 0.372) * | |||
| Remembering | 0.14 (0.032, 0.247) | 0.21 (0.106, 0.323) * | |||
| Thinking speed | 0.16 (0.045, 0.266) | 0.19 (0.073, 0.305) | |||
| Planning | 0.11 (0.007, 0.214) | 0.13 (0.025, 0.235) | |||
| Orientation | 0.22 (0.079, 0.366) | 0.27 (0.12, 0.418) * | |||
| Decision between two things | 0.05 (−0.054, 0.146) | 0.13 (0.02, 0.25) | |||
| Self | Appearance | 0.13 (0.016, 0.249) | 0.14 (0.089, 0.194) * | 0.15 (0.033, 0.276) | 0.26 (0.202, 0.311) * |
| Self-esteem | 0.15 (0.036, 0.267) | 0.17 (0.048, 0.297) | |||
| Accomplishment | 0.01 (−0.103, 0.128) | 0.13 (−0.003, 0.254) | |||
| Future | 0.1 (−0.024, 0.233) | 0.27 (0.151, 0.396) * | |||
| Energy | 0.18 (0.072, 0.283) | 0.33 (0.208, 0.448) * | |||
| Daily Life and Autonomy | Manage at school | 0.26 (0.143, 0.381) * | 0.23 (0.183, 0.282) * | 0.38 (0.267, 0.503)* | 0.32 (0.272, 0.367) * |
| Decision making | 0.1 (−0.008, 0.201) | 0.1 (−0.012, 0.221) | |||
| Daily independence | 0 (−0.134, 0.127) | 0.25 (0.067, 0.433)* | |||
| Getting out and about | 0.18 (0.018, 0.34) | 0.09 (−0.036, 0.22) | |||
| Social activities | 0.21 (0.087, 0.34) * | 0.31 (0.184, 0.436) * | |||
| Support from others | 0.1 (−0.018, 0.225) | 0.17 (0.051, 0.287) | |||
| Ability to move | 0.2 (0.059, 0.343) | 0.29 (0.147, 0.44) * | |||
| Social Relation-ships | Family relationship | 0.17 (0.048, 0.284) | 0.2 (0.152, 0.246) * | 0.25 (0.139, 0.364) * | 0.24 (0.197, 0.287) * |
| Relationship with friends | 0.24 (0.128, 0.354) * | 0.22 (0.094, 0.353) | |||
| Attitudes from others | 0.25 (0.124, 0.369) * | 0.19 (0.081, 0.302) | |||
| Friendships | 0.09 (−0.019, 0.199) | 0.14 (0.011, 0.278) | |||
| Open up to others | 0.1 (−0.019, 0.228) | 0.13 (0.025, 0.23) | |||
| Demands from others | 0.07 (−0.031, 0.165) | 0.23 (0.128, 0.338) * | |||
| Emotions | Anger | 0.13 (0.019, 0.239) | 0.14 (0.087, 0.198) * | 0.21 (0.1, 0.324) * | 0.14 (0.087, 0.202) * |
| Anxiety | 0.12 (0.01, 0.223) | 0.14 (0.022, 0.248) | |||
| Sadness | 0.13 (0.031, 0.235) | 0.03 (−0.077, 0.14) | |||
| Loneliness | 0.11 (−0.012, 0.223) | 0.15 (0.027, 0.27) | |||
| Physical Problems | TBI effects | 0.22 (0.11, 0.334) * | 0.21 (0.166, 0.259) * | 0.3 (0.179, 0.425) * | 0.27 (0.223, 0.318) * |
| Headaches | 0.13 (0.013, 0.244) | 0.25 (0.132, 0.366) * | |||
| Pain | 0.05 (−0.063, 0.155) | 0.1 (−0.007, 0.21) | |||
| Clumsiness | 0.08 (−0.029, 0.183) | 0.12 (0.013, 0.231) | |||
| Seeing/hearing | 0.22 (0.086, 0.352) | 0.27 (0.158, 0.389) * | |||
| Other injuries | 0.21 (0.09, 0.339) * | 0.25 (0.113, 0.39) * | |||
| Total Score | 0.09 (0.067, 0.106) * | 0.11 (0.095, 0.134) * | |||
Appendix C
| Variable p-Value 1 Unadjusted OR (95% CI) | QOLIBRI-KID/ADO Scales | ||||||
|---|---|---|---|---|---|---|---|
| Cognition | Self | Daily Life and Autonomy | Social Relationships | Emotions | Physical Problems | Total Score | |
| Age | 0.001 | 0.004 | |||||
| Children vs. Adolescents | 0.44 (0.27, 0.72) | 1.16 (0.71, 1.90) | 0.50 (0.31, 0.80) | 0.72 (0.44, 1.18) | 1.13 (0.69, 1.84) | 0.66 (0.40, 1.09) | 0.73 (0.45, 1.19) |
| Sex | |||||||
| Female vs. Male | 1.12 (0.69, 1.82) | 0.94 (0.57, 1.56) | 0.78 (0.49, 1.26) | 1.14 (0.69, 1.88) | 1.57 (0.96, 2.59) | 1.33 (0.81, 2.19) | 0.82 (0.50, 1.35) |
| TBI severity | |||||||
| Moderate or severe vs. Mild | 1.27 (0.75, 2.14) | 0.84 (0.48, 1.46) | 0.90 (0.54, 1.50) | 0.64 (0.36, 1.14) | 1.20 (0.70, 2.06) | 0.69 (0.39, 1.22) | 0.69 (0.40, 1.20) |
| KOSCHI | |||||||
| 3a/b, 4a/b vs. 5a/b | 1.01 (0.46, 2.19) | 0.89 (0.39, 2.01) | 1.04 (0.49, 2.20) | 0.64 (0.27, 1.55) | 0.73 (0.31, 1.70) | 0.90 (0.39, 2.05) | 0.51 (0.21, 1.23) |
| Chronic disease | |||||||
| Yes vs. No | 1.05 (0.60, 1.81) | 0.75 (0.42, 1.35) | 0.87 (0.51, 1.51) | 1.25 (0.71, 2.19) | 0.60 (0.33, 1.11) | 0.93 (0.52, 1.66) | 0.83 (0.47, 1.48) |
| Pre-TBI mental disorder | |||||||
| Yes vs. No | 0.81 (0.34, 1.92) | 0.50 (0.18, 1.38) | 0.90 (0.40, 2.07) | 1.02 (0.43, 2.44) | 0.78 (0.31, 1.92) | 1.44 (0.62, 3.34) | 0.67 (0.27, 1.66) |
References
- Giza, C.C.; Mink, R.B.; Madikians, A. Pediatric Traumatic Brain Injury: Not Just Little Adults. Curr. Opin. Crit. Care 2007, 13, 143–152. [Google Scholar] [CrossRef] [PubMed]
- Bruns, N.; Trocchi, P.; Felderhoff-Müser, U.; Dohna-Schwake, C.; Stang, A. Hospitalization and Morbidity Rates After Pediatric Traumatic Brain Injury: A Nation-Wide Population-Based Analysis. Front. Pediatr. 2021, 9, 747743. [Google Scholar] [CrossRef]
- Di Battista, A.; Soo, C.; Catroppa, C.; Anderson, V. Quality of Life in Children and Adolescents Post-TBI: A Systematic Review and Meta-Analysis. J. Neurotrauma 2012, 29, 1717–1727. [Google Scholar] [CrossRef] [PubMed]
- Matza, L.S.; Swensen, A.R.; Flood, E.M.; Secnik, K.; Leidy, N.K. Assessment of Health-Related Quality of Life in Children: A Review of Conceptual, Methodological, and Regulatory Issues. Value Health 2004, 7, 79–92. [Google Scholar] [CrossRef] [PubMed]
- Burd, R.; Jensen, A.R.; VanBuren, J.M.; Alvey, J.S.; Richards, R.; Holubkov, R.; Pollack, M. Long-Term Outcomes after Pediatric Injury: Results of the Assessment of Functional Outcomes and Health-Related Quality of Life after Pediatric Trauma Study. J. Am. Coll. Surg. 2021, 233, 666–675e2. [Google Scholar] [CrossRef] [PubMed]
- Ramos-Usuga, D.; Benito-Sánchez, I.; Pérez-Delgadillo, P.; Valdivia-Tangarife, R.; Villaseñor-Cabrera, T.; Olabarrieta-Landa, L.; Arango-Lasprilla, J.C. Trajectories of Neuropsychological Functioning in Mexican Children with Traumatic Brain Injury over the First Year after Injury. NeuroRehabilitation 2019, 45, 295–309. [Google Scholar] [CrossRef]
- Lendt, M.; Müller, K. Langfristige psychosoziale Entwicklung nach schwerem Schädel-Hirn-Trauma im Kindesalter. Monatsschrift Kinderheilkd. 2014, 162, 420–427. [Google Scholar] [CrossRef]
- Babikian, T.; Merkley, T.; Savage, R.C.; Giza, C.C.; Levin, H. Chronic Aspects of Pediatric Traumatic Brain Injury: Review of the Literature. J. Neurotrauma 2015, 32, 1849–1860. [Google Scholar] [CrossRef]
- Martinez, A.P.; Scherer, M.J.; Tozser, T. Traumatic Brain Injury (TBI) in School-Based Populations: Common Sequelae and Assistive Technology Interventions. Adv. Neurodev. Disord. 2018, 2, 310–321. [Google Scholar] [CrossRef]
- Bullinger, M.; Ravens-Sieberer, U. Lebensqualität Und Chronische Krankheit: Die Perspektive von Kindern und Jugendlichen in Der Rehabilitation. Prax. Kinderpsychol. Kinderpsychiatr. 2006, 55, 23–35. [Google Scholar]
- Ravens-Sieberer, U.; Patrick, P.D.; Benz, B.; Calaminus, G.; Flechtner, H.; Melchers, P.; Patrick, P.; Schäfer, B.; Suhr, L.; Schrod, L.; et al. Quality of Life in Children with Traumatic Brain Injury--Basic Issues, Assessment, and Recommendations. Restor. Neurol. Neurosci. 2002, 20, 151–159. [Google Scholar] [PubMed]
- von Steinbüchel-Rheinwall, N.; Backhaus, J. Erhebung gesundheitsbezogener Lebensqualität: Gegenwärtiger Stand und Perspektiven. Z. Epileptol. 2015, 28, 102–110. [Google Scholar] [CrossRef]
- von Steinbuechel, N.; Petersen, C.; Bullinger, M.; The QOLIBRI Group. Assessment of Health-Related Quality of Life in Persons after Traumatic Brain Injury—Development of the Qolibri, a Specific Measure. Acta Neurochir. Suppl. 2005, 93, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Solans, M.; Pane, S.; Estrada, M.-D.; Serra-Sutton, V.; Berra, S.; Herdman, M.; Alonso, J.; Rajmil, L. Health-Related Quality of Life Measurement in Children and Adolescents: A Systematic Review of Generic and Disease-Specific Instruments. Value Health 2008, 11, 742–764. [Google Scholar] [CrossRef]
- Upton, P.; Lawford, J.; Eiser, C. Parent–Child Agreement across Child Health-Related Quality of Life Instruments: A Review of the Literature. Qual. Life Res. 2008, 17, 895–913. [Google Scholar] [CrossRef]
- Von Steinbuechel, N.; Zeldovich, M.; Greving, S.; Olabarrieta-Landa, L.; Krenz, U.; Timmermann, D.; Koerte, I.K.; Bonfert, M.V.; Berweck, S.; Kieslich, M.; et al. Quality of Life after Brain Injury in Children and Adolescents (QOLIBRI-KID/ADO)—The First Disease-Specific Self-Report Questionnaire after Traumatic Brain Injury. JCM 2023, 12, 4898. [Google Scholar] [CrossRef] [PubMed]
- Eiser, C.; Morse, R. A Review of Measures of Quality of Life for Children with Chronic Illness. Arch. Dis. Child. 2001, 84, 205–211. [Google Scholar] [CrossRef]
- Lam, C.L.K. Subjective Quality of Life Measures—General Principles and Concepts. In Handbook of Disease Burdens and Quality of Life Measures; Preedy, V.R., Watson, R.R., Eds.; Springer: New York, NY, USA, 2010; pp. 381–399. [Google Scholar]
- Eiser, C.; Morse, R. Can Parents Rate Their Child’s Health-Related Quality of Life? Results of a Systematic Review. Qual. Life Res. 2001, 10, 347–357. [Google Scholar] [CrossRef]
- Pieper, P.; Garvan, C. Concordance of Child and Parent Reports of Health-Related Quality of Life in Children With Mild Traumatic Brain or Non-Brain Injuries and in Uninjured Children: Longitudinal Evaluation. J. Pediatr. Health Care 2015, 29, 343–351. [Google Scholar] [CrossRef]
- Pickard, A.S.; Knight, S.J. Proxy Evaluation of Health-Related Quality of Life: A Conceptual Framework for Understanding Multiple Proxy Perspectives. Med. Care 2005, 43, 493–499. [Google Scholar] [CrossRef]
- Varni, J.W.; Seid, M.; Kurtin, P.S. PedsQLTM 4.0: Reliability and Validity of the Pediatric Quality of Life InventoryTM Version 4.0 Generic Core Scales in Healthy and Patient Populations. Med. Care 2001, 39, 800–812. [Google Scholar] [CrossRef] [PubMed]
- Varni, J.W.; Limbers, C.A.; Burwinkle, T.M. How Young Can Children Reliably and Validly Self-Report Their Health-Related Quality of Life?: An Analysis of 8,591 Children across Age Subgroups with the PedsQLTM 4.0 Generic Core Scales. Health Qual. Life Outcomes 2007, 5, 1. [Google Scholar] [CrossRef] [PubMed]
- Khanna, D.; Khadka, J.; Mpundu-Kaambwa, C.; Lay, K.; Russo, R.; Ratcliffe, J. The Quality of Life in Kids: Key Evidence to Strengthen Decisions in Australia (QUOKKA) Project Team; Devlin, N.; Norman, R.; Viney, R.; et al. Are We Agreed? Self- Versus Proxy-Reporting of Paediatric Health-Related Quality of Life (HRQoL) Using Generic Preference-Based Measures: A Systematic Review and Meta-Analysis. PharmacoEconomics 2022, 40, 1043–1067. [Google Scholar] [CrossRef] [PubMed]
- Agnihotri, K.; Awasthi, S.; Singh, U.; Chandra, H.; Thakur, S. A Study of Concordance between Adolescent Self-Report and Parent-Proxy Report of Health-Related Quality of Life in School-Going Adolescents. J. Psychosom. Res. 2010, 69, 525–532. [Google Scholar] [CrossRef] [PubMed]
- Câmara-Costa, H.; Opatowski, M.; Francillette, L.; Toure, H.; Brugel, D.; Laurent-Vannier, A.; Meyer, P.; Watier, L.; Dellatolas, G.; Chevignard, M. Self- and Parent-Reported Quality of Life 7 Years after Severe Childhood Traumatic Brain Injury in the Traumatisme Grave de l’Enfant Cohort: Associations with Objective and Subjective Factors and Outcomes. Qual. Life Res. 2020, 29, 515–528. [Google Scholar] [CrossRef]
- van Markus-Doornbosch, F.; van der Holst, M.; de Kloet, A.J.; Vliet Vlieland, T.P.M.; Meesters, J.J.L. Fatigue, Participation and Quality of Life in Adolescents and Young Adults with Acquired Brain Injury in an Outpatient Rehabilitation Cohort. Dev. Neurorehabilit. 2020, 23, 328–335. [Google Scholar] [CrossRef]
- Green, L.; Godfrey, C.; Soo, C.; Anderson, V.; Catroppa, C. Agreement between Parent-adolescent Ratings on Psychosocial Outcome and Quality-of-life Following Childhood Traumatic Brain Injury. Dev. Neurorehabilit. 2012, 15, 105–113. [Google Scholar] [CrossRef]
- Sluys, K.P.; Lannge, M.; Iselius, L.; Eriksson, L.E. Six Years beyond Pediatric Trauma: Child and Parental Ratings of Children’s Health-Related Quality of Life in Relation to Parental Mental Health. Qual. Life Res. 2015, 24, 2689–2699. [Google Scholar] [CrossRef] [PubMed]
- Cremeens, J.; Eiser, C.; Blades, M. Factors Influencing Agreement between Child Self-Report and Parent Proxy-Reports on the Pediatric Quality of Life InventoryTM 4.0 (PedsQLTM) Generic Core Scales. Health Qual. Life Outcomes 2006, 4, 58. [Google Scholar] [CrossRef]
- Krenz, U.; Timmermann, D.; Gorbunova, A.; Lendt, M.; Schmidt, S.; von Steinbuechel, N. Health-Related Quality of Life after Pediatric Traumatic Brain Injury: A Qualitative Comparison between Children’s and Parents’ Perspectives. PLoS ONE 2021, 16, e0246514. [Google Scholar] [CrossRef]
- Limond, J.; Dorris, L.; McMillan, T.M. Quality of Life in Children with Acquired Brain Injury: Parent Perspectives 1–5 Years after Injury. Brain Inj. 2009, 23, 617–622. [Google Scholar] [CrossRef] [PubMed]
- Souza, L.M.d.N.; Braga, L.W.; Filho, G.N.; Dellatolas, G. Quality-of-Life: Child and Parent Perspectives Following Severe Traumatic Brain Injury. Dev. Neurorehabilit. 2007, 10, 35–47. [Google Scholar] [CrossRef] [PubMed]
- Stancin, T.; Drotar, D.; Taylor, H.G.; Yeates, K.O.; Wade, S.L.; Minich, N.M. Health-Related Quality of Life of Children and Adolescents after Traumatic Brain Injury. Pediatrics 2002, 109, E34. [Google Scholar] [CrossRef] [PubMed]
- Erickson, S.J.; Montague, E.Q.; Gerstle, M.A. Health-Related Quality of Life in Children with Moderate-to-Severe Traumatic Brain Injury. Dev. Neurorehabilit. 2010, 13, 175–181. [Google Scholar] [CrossRef] [PubMed]
- Siegler, R.; Saffran, J.; Gershoff, E.T.; Eisenberg, N.; Pauen, S. Entwicklungspsychologie Im Kindes-Und Jugendalter; Springer: Berlin/Heidelberg, Germany, 2020; ISBN 978-3-662-62771-6. [Google Scholar]
- Eiser, C.; Varni, J.W. Health-Related Quality of Life and Symptom Reporting: Similarities and Differences between Children and Their Parents. Eur. J. Pediatr. 2013, 172, 1299–1304. [Google Scholar] [CrossRef] [PubMed]
- Eiser, C.; Morse, R. Quality-of-Life Measures in Chronic Diseases of Childhood. Health Technol. Assess. 2001, 5, 1–157. [Google Scholar] [CrossRef] [PubMed]
- Upton, P.; Maddocks, A.; Eiser, C.; Barnes, P.M.; Williams, J. Development of a Measure of the Health-Related Quality of Life of Children in Public Care. Child. Care Health Dev. 2005, 31, 409–415. [Google Scholar] [CrossRef]
- Johnson, A.M.; McCarty, C.A.; Marcynyszyn, L.A.; Zatzick, D.F.; Chrisman, S.P.D.; Rivara, F.P. Child- Compared with Parent-Report Ratings on Psychosocial Measures Following a Mild Traumatic Brain Injury among Youth with Persistent Post-Concussion Symptoms. Brain Inj. 2021, 35, 574–586. [Google Scholar] [CrossRef]
- Hemmingsson, H.; Ólafsdóttir, L.B.; Egilson, S.T. Agreements and Disagreements between Children and Their Parents in Health-Related Assessments. Disabil. Rehabil. 2017, 39, 1059–1072. [Google Scholar] [CrossRef]
- Ronen, G.M.; Streiner, D.L.; Rosenbaum, P.; Canadian Pediatric Epilepsy Network. Health-Related Quality of Life in Children with Epilepsy: Development and Validation of Self-Report and Parent Proxy Measures. Epilepsia 2003, 44, 598–612. [Google Scholar] [CrossRef]
- Annett, R.D.; Bender, B.G.; DuHamel, T.R.; Lapidus, J. Factors Influencing Parent Reports on Quality of Life for Children with Asthma. J. Asthma 2003, 40, 577–587. [Google Scholar] [CrossRef] [PubMed]
- Tluczek, A.; Becker, T.; Grieve, A.; Laxova, A.; Rock, M.J.; Gershan, W.M.; Green, C.G.; Farrell, P.M. Health-Related Quality of Life in Children and Adolescents with Cystic Fibrosis: Convergent Validity with Parent-Reports and Objective Measures of Pulmonary Health. Behav. Pediatr. 2013, 34, 10. [Google Scholar] [CrossRef] [PubMed]
- Chang, P.-C.; Yeh, C.-H. Agreement between Child Self-Report and Parent Proxy-Report to Evaluate Quality of Life in Children with Cancer. Psycho-Oncol. 2005, 14, 125–134. [Google Scholar] [CrossRef] [PubMed]
- Dipnall, J.F.; Rivara, F.P.; Lyons, R.A.; Ameratunga, S.; Brussoni, M.; Lecky, F.E.; Bradley, C.; Beck, B.; Lyons, J.; Schneeberg, A.; et al. Predictors of Health-Related Quality of Life Following Injury in Childhood and Adolescence: A Pooled Analysis. Inj. Prev. 2022, 28, 301–310. [Google Scholar] [CrossRef]
- Huang, I.-C.; Shenkman, E.A.; Leite, W.; Knapp, C.A.; Thompson, L.A.; Revicki, D.A. Agreement Was Not Found in Adolescents’ Quality of Life Rated by Parents and Adolescents. J. Clin. Epidemiol. 2009, 62, 337–346. [Google Scholar] [CrossRef]
- Leathem, J.M.; Murphy, L.J.; Flett, R.A. Self- and Informant-Ratings on the Patient Competency Rating Scale in Patients with Traumatic Brain Injury. J. Clin. Exp. Neuropsychol. 1998, 20, 694–705. [Google Scholar] [CrossRef]
- Lloyd, O.; Ownsworth, T.; Fleming, J.; Zimmer-Gembeck, M.J. Awareness Deficits in Children and Adolescents After Traumatic Brain Injury: A Systematic Review. J. Head Trauma Rehabil. 2015, 30, 311–323. [Google Scholar] [CrossRef] [PubMed]
- Beardmore, S. Does Information and Feedback Improve Children’s Knowledge and Awareness of Deficits after Traumatic Brain Injury? Neuropsychol. Rehabil. 1999, 9, 45–62. [Google Scholar] [CrossRef]
- Lloyd, O.; Ownsworth, T.; Fleming, J.; Jackson, M.; Zimmer-Gembeck, M. Impaired Self-Awareness after Pediatric Traumatic Brain Injury: Protective Factor or Liability? J. Neurotrauma 2021, 38, 616–627. [Google Scholar] [CrossRef]
- Rauen, K.; Späni, C.B.; Tartaglia, M.C.; Ferretti, M.T.; Reichelt, L.; Probst, P.; Schäpers, B.; Müller, F.; Jahn, K.; Plesnila, N. Quality of Life after Traumatic Brain Injury: A Cross-Sectional Analysis Uncovers Age- and Sex-Related Differences over the Adult Life Span. GeroScience 2021, 43, 263–278. [Google Scholar] [CrossRef]
- Teasdale, G.M.; Pettigrew, L.E.L.; Wilson, J.T.L.; Murray, G.; Jennett, B. Analyzing Outcome of Treatment of Severe Head Injury: A Review and Update on Advancing the Use of the Glasgow Outcome Scale. J. Neurotrauma 1998, 15, 587–597. [Google Scholar] [CrossRef] [PubMed]
- von Steinbuechel, N.; Wilson, L.; Gibbons, H.; Hawthorne, G.; Höfer, S.; Schmidt, S.; Bullinger, M.; Maas, A.; Neugebauer, E.; Powell, J.; et al. Quality of Life after Brain Injury (QOLIBRI): Scale Validity and Correlates of Quality of Life. J. Neurotrauma 2010, 27, 1157–1165. [Google Scholar] [CrossRef] [PubMed]
- Crouchman, M. A Practical Outcome Scale for Paediatric Head Injury. Arch. Dis. Child. 2001, 84, 120–124. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems, 10th ed.; WHO: Geneva, Switzerland, 2016. Available online: https://icd.who.int/browse10/2016/en (accessed on 15 March 2022).
- SAS. SAS® 9.4 2013; SAS Institute Inc.: Tokyo, Japan, 2023. [Google Scholar]
- Lanza, S.T.; Dziak, J.J.; Huang, L.; Wagner, A.; Collins, L.M. PROC LCA & PROC LTA Users’ Guide Version 1.3.2; The Methodology Center: University Park, PA, USA, 2015. [Google Scholar]
- Hadianfard, H.; Kiani, B.; Azizzadeh Herozi, M.; Mohajelin, F.; Mitchell, J.T. Health-Related Quality of Life in Iranian Adolescents: A Psychometric Evaluation of the Self-Report Form of the PedsQL 4.0 and an Investigation of Gender and Age Differences. Health Qual. Life Outcomes 2021, 19, 108. [Google Scholar] [CrossRef]
- McNeish, D. Thanks Coefficient Alpha, We’ll Take It from Here. Psychol. Methods 2018, 23, 412–433. [Google Scholar] [CrossRef]
- Ravens-Sieberer, U.; Erhart, M.; Wille, N.; Wetzel, R.; Nickel, J.; Bullinger, M. Generic Health-Related Quality-of-Life Assessment in Children and Adolescents. Pharmacoeconomics 2006, 24, 1199–1220. [Google Scholar] [CrossRef]
- Taber, K.S. The Use of Cronbach’s Alpha When Developing and Reporting Research Instruments in Science Education. Res. Sci. Educ. 2018, 48, 1273–1296. [Google Scholar] [CrossRef]
- Shrout, P.E.; Fleiss, J.L. Intraclass Correlations: Uses in Assessing Rater Reliability. Psychol. Bull. 1979, 86, 420–428. [Google Scholar] [CrossRef]
- McGraw, K.O.; Wong, S.P. Forming Inferences about Some Intraclass Correlation Coefficients. Psychol. Methods 1996, 1, 30. [Google Scholar] [CrossRef]
- McHugh, M.L. Interrater Reliability: The Kappa Statistic. Biochem. Med. 2012, 22, 276–282. [Google Scholar] [CrossRef]
- Landis, J.R.; Koch, G.G. The Measurement of Observer Agreement for Categorical Data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef] [PubMed]
- Sim, J.; Wright, C.C. The Kappa Statistic in Reliability Studies: Use, Interpretation, and Sample Size Requirements. Phys. Ther. 2005, 85, 257–268. [Google Scholar] [CrossRef] [PubMed]
- Norman, G.R.; Sloan, J.A.; Wyrwich, K.W. Interpretation of Changes in Health-Related Quality of Life: The Remarkable Universality of Half a Standard Deviation. Med. Care 2003, 41, 12. [Google Scholar] [CrossRef]
- Akaike, H. A New Look at the Statistical Model Identification. IEEE Trans. Autom. Control 1974, 19, 716–723. [Google Scholar] [CrossRef]
- Schwarz, G. Estimating the Dimension of a Model. Ann. Stat. 1978, 6, 461–464. [Google Scholar] [CrossRef]
- Spurk, D.; Hirschi, A.; Wang, M.; Valero, D.; Kauffeld, S. Latent Profile Analysis: A Review and “How to” Guide of Its Application within Vocational Behavior Research. J. Vocat. Behav. 2020, 120, 103445. [Google Scholar] [CrossRef]
- Wang, M.-C.; Deng, Q.; Bi, X.; Ye, H.; Yang, W. Performance of the Entropy as an Index of Classification Accuracy in Latent Profile Analysis: A Monte Carlo Simulation Study. Acta Psychol. Sin. 2017, 49, 1473. [Google Scholar] [CrossRef]
- Weller, B.E.; Bowen, N.K.; Faubert, S.J. Latent Class Analysis: A Guide to Best Practice. J. Black Psychol. 2020, 46, 287–311. [Google Scholar] [CrossRef]
- Slomine, B.S.; McCarthy, M.L.; Ding, R.; MacKenzie, E.J.; Jaffe, K.M.; Aitken, M.E.; Durbin, D.R.; Christensen, J.R.; Dorsch, A.M.; Paidas, C.N.; et al. Health Care Utilization and Needs After Pediatric Traumatic Brain Injury. Pediatrics 2006, 117, e663–e674. [Google Scholar] [CrossRef]
- AWMF. Das Schädel-Hirn-Trauma Im Kindes- und Jugendalter. Available online: https://www.awmf.org/leitlinien/detail/ll/024-018.html (accessed on 11 March 2022).
- Dipnall, J.F.; Rivara, F.P.; Lyons, R.A.; Ameratunga, S.; Brussoni, M.; Lecky, F.E.; Bradley, C.; Beck, B.; Lyons, J.; Schneeberg, A.; et al. Health-Related Quality of Life (HRQoL) Outcomes Following Injury in Childhood and Adolescence Using EuroQol (EQ-5D) Responses with Pooled Longitudinal Data. Int. J. Environ. Res. Public Health 2021, 18, 10156. [Google Scholar] [CrossRef]
- Schneeberg, A.; Ishikawa, T.; Kruse, S.; Zallen, E.; Mitton, C.; Bettinger, J.A.; Brussoni, M. A Longitudinal Study on Quality of Life after Injury in Children. Health Qual. Life Outcomes 2016, 14, 120. [Google Scholar] [CrossRef]
- DeMatteo, C.A.; Hanna, S.E.; Yousefi-Nooraie, R.; Lin, C.-Y.A.; Mahoney, W.J.; Law, M.C.; McCauley, D. Quality-of-Life after Brain Injury in Childhood: Time, Not Severity, Is the Significant Factor. Brain Inj. 2014, 28, 114–121. [Google Scholar] [CrossRef]
- Pinquart, M. Health-Related Quality of Life of Young People With and Without Chronic Conditions. J. Pediatr. Psychol. 2020, 45, 780–792. [Google Scholar] [CrossRef]
- Gornall, A.; Takagi, M.; Morawakage, T.; Liu, X.; Anderson, V. Mental Health after Paediatric Concussion: A Systematic Review and Meta-Analysis. Br. J. Sports Med. 2021, 55, 1048–1058. [Google Scholar] [CrossRef] [PubMed]
- Baumgarten, F.; Cohrdes, C.; Schienkiewitz, A.; Thamm, R.; Meyrose, A.-K.; Ravens-Sieberer, U. Gesundheitsbezogene Lebensqualität und Zusammenhänge mit chronischen Erkrankungen und psychischen Auffälligkeiten bei Kindern und Jugendlichen: Ergebnisse aus KiGGS Welle 2. Bundesgesundheitsbl 2019, 62, 1205–1214. [Google Scholar] [CrossRef] [PubMed]
- Eriksson, M.; Boman, E.; Svedberg, P. Autonomy and Health-Related Quality of Life in Adolescents. BMC Pediatr. 2022, 22, 555. [Google Scholar] [CrossRef] [PubMed]
- Ng, J.Y.Y.; Ntoumanis, N.; Thøgersen-Ntoumani, C.; Deci, E.L.; Ryan, R.M.; Duda, J.L.; Williams, G.C. Self-Determination Theory Applied to Health Contexts: A Meta-Analysis. Perspect. Psychol. Sci. 2012, 7, 325–340. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, L. Long-Term Behavior Problems Following Pediatric Traumatic Brain Injury: Prevalence, Predictors, and Correlates. J. Pediatr. Psychol. 2003, 28, 251–263. [Google Scholar] [CrossRef] [PubMed]
- Hung, R.; Carroll, L.J.; Cancelliere, C.; Côté, P.; Rumney, P.; Keightley, M.; Donovan, J.; Stålnacke, B.-M.; Cassidy, J.D. Systematic Review of the Clinical Course, Natural History, and Prognosis for Pediatric Mild Traumatic Brain Injury: Results of the International Collaboration on Mild Traumatic Brain Injury Prognosis. Arch. Phys. Med. Rehabil. 2014, 95, S174–S191. [Google Scholar] [CrossRef]
- Catroppa, C.; Anderson, V.A.; Morse, S.A.; Haritou, F.; Rosenfeld, J.V. Outcome and Predictors of Functional Recovery 5 Years Following Pediatric Traumatic Brain Injury (TBI). J. Pediatr. Psychol. 2008, 33, 707–718. [Google Scholar] [CrossRef] [PubMed]
- Andruszkow, H.; Deniz, E.; Urner, J.; Probst, C.; Grün, O.; Lohse, R.; Frink, M.; Krettek, C.; Zeckey, C.; Hildebrand, F. Physical and Psychological Long-Term Outcome after Traumatic Brain Injury in Children and Adult Patients. Health Qual. Life Outcomes 2014, 12, 26. [Google Scholar] [CrossRef] [PubMed]
- Ryan, N.P.; Hughes, N.; Godfrey, C.; Rosema, S.; Catroppa, C.; Anderson, V.A. Prevalence and Predictors of Externalizing Behavior in Young Adult Survivors of Pediatric Traumatic Brain Injury. J. Head Trauma Rehabil. 2015, 30, 75–85. [Google Scholar] [CrossRef] [PubMed]
- Horneman, G.; Folkesson, P.; Sintonen, H.; von Wendt, L.; Emanuelson, I. Health-Related Quality of Life of Adolescents and Young Adults 10 Years after Serious Traumatic Brain Injury. Int. J. Rehabil. Res. 2005, 28, 245–249. [Google Scholar] [CrossRef]
- Ledoux, A.-A.; Webster, R.J.; Clarke, A.E.; Fell, D.B.; Knight, B.D.; Gardner, W.; Cloutier, P.; Gray, C.; Tuna, M.; Zemek, R. Risk of Mental Health Problems in Children and Youths Following Concussion. JAMA Netw. Open 2022, 5, e221235. [Google Scholar] [CrossRef]
- Borgers, N.; Sikkel, D.; Hox, J. Response Effects in Surveys on Children and Adolescents: The Effect of Number of Response Options, Negative Wording, and Neutral Mid-Point. Qual. Quant. 2004, 38, 17–33. [Google Scholar] [CrossRef]
- Costa-Santos, C.; Bernardes, J.; Ayres-de-Campos, D.; Costa, A.; Costa, C. The Limits of Agreement and the Intraclass Correlation Coefficient May Be Inconsistent in the Interpretation of Agreement. J. Clin. Epidemiol. 2011, 64, 264–269. [Google Scholar] [CrossRef] [PubMed]
- Papp, Z.K.; Török, S.; Szentes, A.; Hosszú, D.; Kökönyei, G. Parent-Child Agreement on Health-Related Quality of Life: The Role of Perceived Consequences of the Child’s Chronic Illness. Psychol. Health 2022. Online ahead of print. [Google Scholar] [CrossRef]
- Jokovic, A.; Locker, D.; Guyatt, G. How Well Do Parents Know Their Children? Implications for Proxy Reporting of Child Health-Related Quality of Life. Qual Life Res 2004, 13, 1297–1307. [Google Scholar] [CrossRef]
- Prigatano, G.P.; Gray, J.A. Parental Concerns and Distress after Paediatric Traumatic Brain Injury: A Qualitative Study. Brain Inj. 2007, 21, 721–729. [Google Scholar] [CrossRef]
- Klassen, A.F.; Miller, A.; Fine, S. Agreement between Parent and Child Report of Quality of Life in Children with Attention-Deficit/Hyperactivity Disorder. Child Care Health Dev. 2006, 32, 397–406. [Google Scholar] [CrossRef]
- Ganesalingam, K.; Yeates, K.O.; Ginn, M.S.; Taylor, H.G.; Dietrich, A.; Nuss, K.; Wright, M. Family Burden and Parental Distress Following Mild Traumatic Brain Injury in Children and Its Relationship to Post-Concussive Symptoms. J. Pediatr. Psychol. 2008, 33, 621–629. [Google Scholar] [CrossRef] [PubMed]
- Micklewright, J.L.; King, T.Z.; O’Toole, K.; Henrich, C.; Floyd, F.J. Parental Distress, Parenting Practices, and Child Adaptive Outcomes Following Traumatic Brain Injury. J. Int. Neuropsychol. Soc. 2012, 18, 343–350. [Google Scholar] [CrossRef] [PubMed]
- Rashid, M.; Goez, H.R.; Mabood, N.; Damanhoury, S.; Yager, J.Y.; Joyce, A.S.; Newton, A.S. The Impact of Pediatric Traumatic Brain Injury (TBI) on Family Functioning: A Systematic Review. J. Pediatr. Rehabil. Med. 2014, 7, 241–254. [Google Scholar] [CrossRef] [PubMed]
- Bland, J.M.; Altman, D. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986, 327, 307–310. [Google Scholar] [CrossRef]
| Children (n = 152) | Adolescents (n = 148) | (Test Statistic, df) p-Value * | Total (n = 300) | ||
|---|---|---|---|---|---|
| Age (years) | Mean (SD) | 10.6 (1.40) | 15.2 (1.47) | N/A | 12.9 (2.72) |
| Sex | (0.50, 1) 0.479 | ||||
| Female | N (%) | 58 (38.2) | 62 (41.9) | 120 (40.0) | |
| Male | 94 (61.8) | 85 (57.4) | 179 (59.7) | ||
| Missing | 0 (0.0) | 1 (0.7) | 1 (0.3) | ||
| TBI severity | (1.95, 2) 0.377 | ||||
| Mild | N (%) | 106 (69.7) | 109 (73.6) | 215 (71.7) | |
| Moderate | 16 (10.5) | 9 (6.1) | 25 (8.3) | ||
| Severe | 30 (19.7) | 30 (20.3) | 60 (20.0) | ||
| KOSCHI | (8.55, 1) 0.004 | ||||
| 3a/b, 4a/b | N (%) | 8 (5.3) | 23 (15.5) | 31 (10.3) | |
| 5a/b | 144 (94.7) | 125 (84.5) | 269 (89.7) | ||
| Time since injury (years) | (2.16, 3) 0.541 | ||||
| <1 | N (%) | 16 (10.5) | 10 (6.8) | 26 (8.7) | |
| 1 to <2 | 48 (31.6) | 43 (29.1) | 91 (30.3) | ||
| 2 to <4 | 29 (19.1) | 27 (18.2) | 56 (18.7) | ||
| 4 to 10 | 59 (38.8) | 67 (45.3) | 126 (42.0) | ||
| Missing | 0 (0.0) | 1 (0.7) | 1 (0.3) | ||
| Chronic diseases | (0.55, 1) 0.457 | ||||
| No | N (%) | 116 (76.3) | 103 (69.6) | 219 (73.0) | |
| Yes | 36 (23.7) | 39 (26.4) | 75 (25.0) | ||
| Missing | 0 (0.0) | 6 (4.1) | 6 (2.0) | ||
| Treatment for mental disorder before the TBI | (2.64, 1) 0.104 | ||||
| No | N (%) | 137 (90.1) | 130 (87.8) | 267 (89.0) | |
| Yes | 9 (5.9) | 17 (11.5) | 26 (8.7) | ||
| Missing | 6 (3.9) | 1 (0.7) | 7 (2.3) |
| Parent Characteristics | Children (n = 152) | Adolescents (n = 148) | (Test Statistic, df) p-Value | Total (n = 300) | |
|---|---|---|---|---|---|
| Questionnaire completed by | (0.32, 1) 0.572 | ||||
| Mother | N (%) | 118 (77.6) | 121 (81.8) | 239 (79.7) | |
| Father | 30 (19.7) | 26 (17.6) | 56 (18.7) | ||
| Other person | 4 (2.6) | 1 (0.7) | 5 (1.7) | ||
| Parent age (years) | Mean (SD) Missing | 44.6 (5.15) 26 | 48.0 (5.64) 41 | (4.74, 231) <0.001 | 46.2 (5.63) 67 |
| Education of parent completing the questionnaire | (Fisher’s exact test) 0.218 | ||||
| Primary school | N (%) | 1 (0.7) | 0 (0.0) | 1 (0.3) | |
| Secondary/high school | 36 (23.7) | 42 (28.4) | 78 (26.0) | ||
| Post-high school training | 21 (13.8) | 29 (19.6) | 50 (16.7) | ||
| University | 82 (53.9) | 68 (45.9) | 150 (50.0) | ||
| Missing | 12 (7.9) | 9 (6.1) | 21 (7.0) | ||
| Parent living in a partnership | (2.26, 1) 0.133 | ||||
| Single parent | N (%) | 11 (7.2) | 19 (12.8) | 30 (10.0) | |
| In a relationship | 134 (88.2) | 128 (86.5) | 262 (87.3) | ||
| Missing | 7 (4.6) | 1 (0.7) | 8 (2.7) |
| QOLIBRI-KID/ADO Scales and Total Score for Both Age Groups | Directional Differences (Child/Adolescent—Parent) | Mixed Linear Model 2 | Type of Parent (Mother or Father *) | Absolute Differences |Child/Adolescent—Parent| Mean (SD) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Missing | p-Value 1 Paired t-Test | p-Value Repeated Measures Model | Un-adjusted ICC | Mean Estimate (SE) | p-Value | Ad-justed ICC | p-Value 3 Repeated Measures | ICC Adjusted for Type of Parent | ||
| Children (n = 152) | |||||||||||
| Cognition | 3.4 (13.95) | 3 | 0.004 | 0.004 | 0.291 | 3.5 (1.10) | 0.003 | 0.276 | 0.907 | 0.290 | 11.5 (8.49) |
| Self | 10 (14.58) | 3 | <0.001 | <0.001 | 0.308 | 10.2 (1.21) | <0.001 | 0.304 | 0.261 | 0.303 | 13. 8 (11.08) |
| Daily Life and Autonomy | 5.5 (11.27) | 3 | <0.001 | <0.001 | 0.429 | 5.7 (0.93) | <0.001 | 0.393 | 0.571 | 0.426 | 10.0 (7.57) |
| Social Relationships | 8.7 (14.00) | 3 | <0.001 | <0.001 | 0.401 | 8.8 (1.15) | <0.001 | 0.400 | 0.376 | 0.395 | 13.0 (10.11) |
| Emotions | −0.5 (28.74) | 3 | 0.822 | 0.872 | 0.239 | 0.2 (2.34) | 0.937 | 0.255 | 0.342 | 0.233 | 23.9 (15.87) |
| Physical Problems | −8.8 (27.86) | 4 | <0.001 | <0.001 | 0.249 | −8.7 (2.33) | <0.001 | 0.232 | 0.206 | 0.241 | 22.8 (18.20) |
| Total Score | 3.1 (11.18) | 4 | <0.001 | <0.001 | 0.436 | 3.4 (0.93) | <0.001 | 0.409 | 0.881 | 0.435 | 9.3 (6.89) |
| Adolescents (n = 148) | |||||||||||
| Cognition | −1.5 (14.39) | 0 | 0.214 | 0.211 | 0.478 | −1.5 (1.22) | 0.218 | 0.420 | 0.353 | 0.473 | 11.5 (8.72) |
| Self | 1.5 (16.45) | 3 | 0.271 | 0.285 | 0.483 | 1.1 (1.39) | 0.419 | 0.438 | 0.753 | 0.482 | 13.2 (9.85) |
| Daily Life and Autonomy | 3.3 (12.49) | 3 | 0.002 | 0.003 | 0.509 | 2.8 (1.07) | 0.010 | 0.471 | 0.701 | 0.506 | 9.1 (9.17) |
| Social Relationships | 6.0 (15.24) | 0 | <0.001 | <0.001 | 0.412 | 6.0 (1.31) | <0.001 | 0.363 | 0.604 | 0.409 | 12.3 (10.77) |
| Emotions | 2.3 (27.87) | 3 | 0.325 | 0.293 | 0.269 | 2.4 (2.42) | 0.332 | 0.227 | 0.274 | 0.261 | 21.7 (17.53) |
| Physical Problems | 0.3 (24.10) | 6 | 0.897 | 0.926 | 0.368 | 0.3 (2.07) | 0.883 | 0.303 | 0.475 | 0.364 | 19.2 (14.46) |
| Total Score | 2.0 (11.96) | 12 | 0.050 | 0.060 | 0.508 | 1.8 (1.05) | 0.093 | 0.426 | 0.986 | 0.508 | 9.5 (7.46) |
| Variable in the Model | QOLIBRI-KID/ADO Scales | Total Score | |||||
|---|---|---|---|---|---|---|---|
| p-Value Adjusted OR (95% CI) | Cognition | Self | Daily Life and Autonomy | Social Relationships | Emotions | Physical Problems | |
| Number of dyads in the model (%) | 286 (95.3) | 283 (94.3) | 283 (94.3) | 286 (95.3) | 283 (94.3) | 280 (93.3) | 274 (91.3) |
| Age: | 0.001 | 0.002 | 0.176 | 0.136 | |||
| Children vs. Adolescents | 0.41 (0.25, 0.68) | 0.46 (0.29, 0.75) | 0.71 (0.43, 1.17) | 0.68 (0.41, 1.13) | |||
| Sex: | 0.274 | 0.054 | 0.216 | ||||
| Female vs. Male | 0.76 (0.46, 1.24) | 1.66 (0.99, 2.77) | 1.38 (0.83, 2.30) | ||||
| TBI severity: | 0.277 | 0.245 | 0.255 | ||||
| Moderate or Severe vs. Mild | 1.36 (0.78, 2.36) | 0.71 (0.39, 1.27) | 0.71 (0.40, 1.28) | ||||
| KOSCHI: | 0.139 | ||||||
| 3a,b, 4a,b vs. 5a,b | 0.50 (0.20, 1.25) | ||||||
| Chronic disease: | 0.044 | ||||||
| Yes vs. No | 0.52 (0.27, 0.98) | ||||||
| Pre-TBI mental disorder: | 0.192 | 0.140 | |||||
| Yes vs. No | 0.52 (0.19, 1.39) | 0.43 (0.14, 1.31) | |||||
| KID/ADO < Parent (n = 64) | KID/ADO = Parent (n = 102) | KID/ADO > Parent (n = 118) | Total (n = 284) | (χ2, df) p-Value | |
|---|---|---|---|---|---|
| Age category | (2.08, 2) 0.353 | ||||
| Children | 33 (51.6%) | 48 (47.1%) | 67 (56.8%) | 148 (52.1%) | |
| Adolescents | 31 (48.4%) | 54 (52.9%) | 51 (43.2%) | 136 (47.9%) | |
| Child sex | (5.38, 2) 0.068 | ||||
| Female | 34 (53.1%) | 38 (37.3%) | 43 (36.4%) | 115 (40.5%) | |
| Male | 30 (46.9%) | 63 (61.8%) | 75 (63.6%) | 168 (59.2%) | |
| Missing | 0 (0.0%) | 1 (1.0%) | 0 (0.0%) | 1 (0.4%) | |
| TBI severity | (3.05, 2) 0.217 | ||||
| Mild | 47 (73.4%) | 77 (75.5%) | 77 (65.3%) | 201 (70.8%) | |
| Moderate or severe | 17 (26.6%) | 25 (24.5%) | 41 (34.7%) | 83 (29.2%) | |
| KOSCHI | (3.42, 2) 0.181 | ||||
| 3a/b, 4a/b | 6 (9.4%) | 7 (6.9%) | 17 (14.4%) | 30 (10.6%) | |
| 5a/b | 58 (90.6%) | 95 (93.1%) | 101 (85.6%) | 254 (89.4%) | |
| Chronic diseases | (1.48, 2) 0.477 | ||||
| No | 50 (78.1%) | 77 (75.5%) | 81 (68.6%) | 208 (73.2%) | |
| Yes | 14 (21.9%) | 23 (22.5%) | 33 (28.0%) | 70 (24.6%) | |
| Missing | 0 (0.0%) | 2 (2.0%) | 4 (3.4%) | 6 (2.1%) | |
| Before the TBI, the child/adolescent had treatment for mental disorder | (6.11, 2) 0.047 | ||||
| No | 60 (93.8%) | 94 (92.2%) | 102 (86.4%) | 256 (90.1%) | |
| Yes | 2 (3.1%) | 7 (6.9%) | 16 (13.6%) | 25 (8.8%) | |
| Missing | 2 (3.1%) | 1 (1.0%) | 0 (0.0%) | 3 (1.1%) | |
| Education (both parents) | (2.06, 2) 0.356 | ||||
| University | 43 (67.2%) | 68 (66.7%) | 71 (60.2%) | 182 (64.1%) | |
| Other than university | 20 (31.3%) | 28 (27.5%) | 44 (37.3%) | 92 (32.4%) | |
| Missing | 1 (1.6%) | 6 (5.9%) | 3 (2.5%) | 10 (3.5%) | |
| Living in a partnership | (0.34, 2) 0.844 | ||||
| Single parent | 8 (12.5%) | 10 (9.8%) | 12 (10.2%) | 30 (10.6%) | |
| In relationship | 55 (85.9%) | 90 (88.2%) | 105 (89.0%) | 250 (88.0%) | |
| Missing | 1 (1.6%) | 2 (2.0%) | 1 (0.8%) | 4 (1.4%) | |
| Questionnaire completed by | (5.06, 2) 0.080 | ||||
| Mother | 47 (73.4%) | 89 (87.3%) | 95 (80.5%) | 231 (81.3%) | |
| Father | 16 (25.0%) | 12 (11.8%) | 23 (19.5%) | 51 (18.0%) | |
| Missing | 1 (1.6%) | 1 (1.0%) | 0 (0.0%) | 2 (0.7%) | |
| Number of Classes | df | LRT G2 | AIC | BIC | Entropy | % of Seeds Associated with Best Fitted Model |
|---|---|---|---|---|---|---|
| 2 | 492 | 294.0 | 332.0 | 401.3 | 0.70 | 65.0 |
| 3 | 482 | 252.4 | 310.4 | 416.2 | 0.68 | 92.3 |
| 4 | 472 | 226.2 | 304.2 | 446.5 | 0.69 | 18.0 |
| 5 | 462 | 204.7 | 302.7 | 481.5 | 0.74 | 13.3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cunitz, K.; Holloway, I.; Harzendorf, A.; Greving, S.; Zeldovich, M.; Krenz, U.; Timmermann, D.; Koerte, I.K.; Bonfert, M.V.; Berweck, S.; et al. Health-Related Quality of Life after Pediatric Traumatic Brain Injury: A Quantitative Comparison between Children’s and Parents’ Perspectives of the QOLIBRI-KID/ADO Questionnaire. J. Clin. Med. 2023, 12, 7439. https://doi.org/10.3390/jcm12237439
Cunitz K, Holloway I, Harzendorf A, Greving S, Zeldovich M, Krenz U, Timmermann D, Koerte IK, Bonfert MV, Berweck S, et al. Health-Related Quality of Life after Pediatric Traumatic Brain Injury: A Quantitative Comparison between Children’s and Parents’ Perspectives of the QOLIBRI-KID/ADO Questionnaire. Journal of Clinical Medicine. 2023; 12(23):7439. https://doi.org/10.3390/jcm12237439
Chicago/Turabian StyleCunitz, Katrin, Ivana Holloway, Anne Harzendorf, Sven Greving, Marina Zeldovich, Ugne Krenz, Dagmar Timmermann, Inga K. Koerte, Michaela Veronika Bonfert, Steffen Berweck, and et al. 2023. "Health-Related Quality of Life after Pediatric Traumatic Brain Injury: A Quantitative Comparison between Children’s and Parents’ Perspectives of the QOLIBRI-KID/ADO Questionnaire" Journal of Clinical Medicine 12, no. 23: 7439. https://doi.org/10.3390/jcm12237439
APA StyleCunitz, K., Holloway, I., Harzendorf, A., Greving, S., Zeldovich, M., Krenz, U., Timmermann, D., Koerte, I. K., Bonfert, M. V., Berweck, S., Kieslich, M., Brockmann, K., Roediger, M., Buchheim, A., Andelic, N., Lendt, M., Staebler, M., Muehlan, H., & von Steinbuechel, N. (2023). Health-Related Quality of Life after Pediatric Traumatic Brain Injury: A Quantitative Comparison between Children’s and Parents’ Perspectives of the QOLIBRI-KID/ADO Questionnaire. Journal of Clinical Medicine, 12(23), 7439. https://doi.org/10.3390/jcm12237439









