Consultation-Based Deprescribing Service to Optimize Palliative Care for Terminal Cancer Patients
Abstract
:1. Introduction
2. Materials and Methods
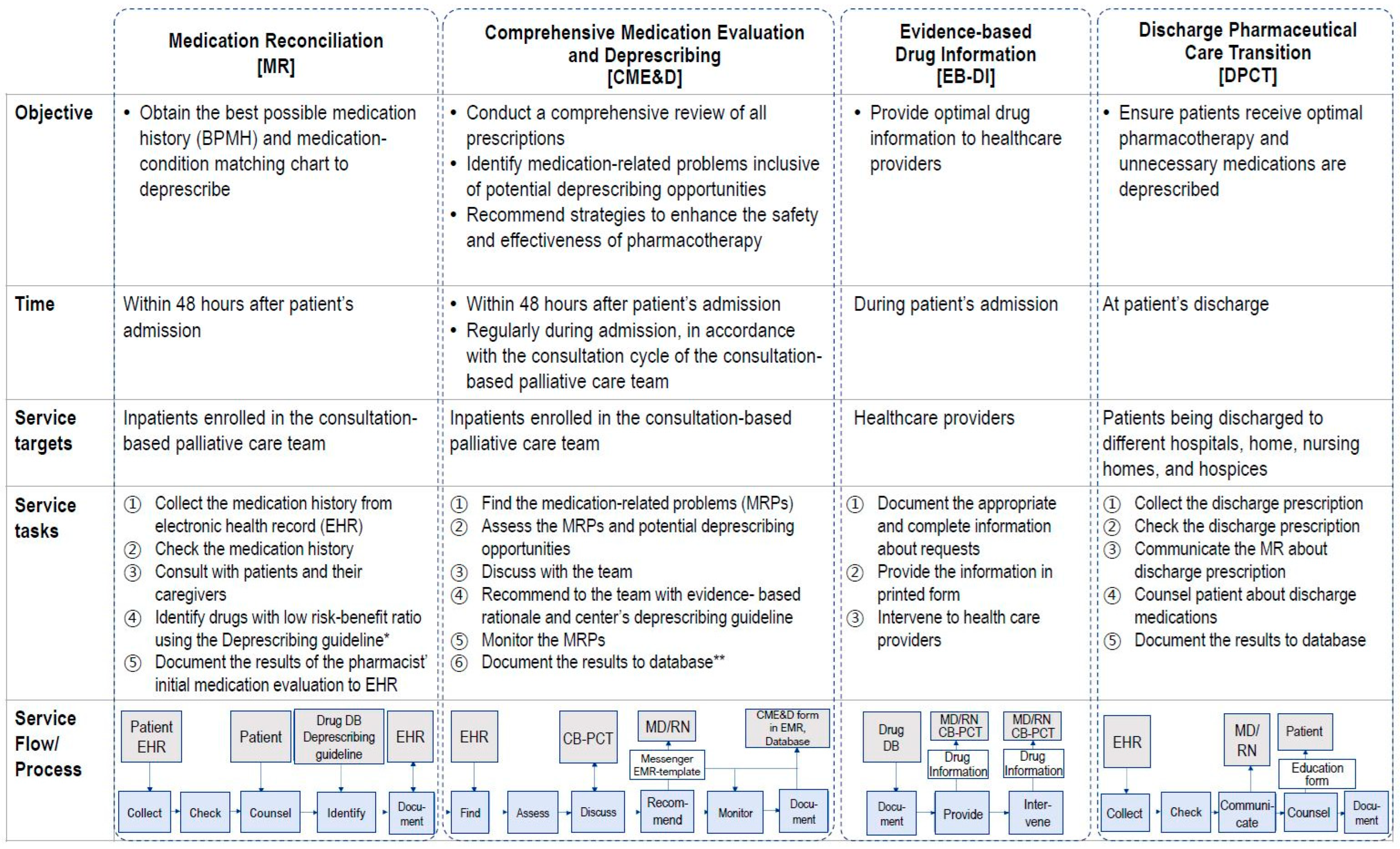
2.1. Pharmacist-Led Deprescribing Service of CB-PCT
- Medication Reconciliation (MR) service: This sub-service aimed to curtail medication discrepancies and obtain the best possible medication history (BPMH) within 48 h of patients’ admission or enrollment in CB-PCT.
- Comprehensive Medication Evaluation and Deprescribing (CME&D): Initiated within 48 h post CB-PCT enrollment, this core sub-service continued throughout the patients’ stay. CME&D offered deprescribing interventions and an in-depth medication assessment to identify MRPs, which include both evident problems and potentially inappropriate prescriptions. CME&D involved stages of finding, assessing, discussing, recommending, monitoring, and documenting. During the finding stage, patients’ medications were evaluated and pharmacy consultations were provided to patients as needed, with pharmacists typically spending about 15 min with each patient. In the assessing stage, opportunities for deprescribing were identified primarily based on the previously developed deprescribing guidelines (SNUH deprescribing guidelines, Supplementary Methods S2) and a variety of established guidelines, including Beers’ criteria [32] and STOPPFrail [21]. Detected MRPs were shared within the team and actively discussed, not only during CB-PCT weekly meetings, but also via the team’s instant messaging apps, ensuring timely interventions. Pharmacists intervened via short message service to physicians or through verbal communication. Following evaluation, the findings were documented in the electronic health records (EHR) using department-specific forms. Pharmacists evaluated patients’ prescriptions within 24 h of notification by the team’s nurse of the patient’s enrollment. Aligned with the patient’s consultation cycle of the team, MRPs were tracked and monitored for resolution. Finally, the results of the interventions were recorded in the electronic health record and pharmacist’s database.
- Evidence-based Drug Information (EB-DI): A service proffering optimal drug information to healthcare providers.
- Discharge Pharmaceutical Care Transition (DPCT): Implemented at discharge, the primary objective of DPCT was to facilitate the transition by addressing the pharmaceutical care needs tailored for these patients. Pharmacists reviewed the appropriateness of prescribed medications, focusing on optimizing symptom management for the patient. The continued necessity of previously used medications was reassessed, and recommendations for medication adjustments and deprescribing were given for the prescribed discharge medications.
2.2. Study Design
2.2.1. Clinical Outcomes
2.2.2. Implementability
2.3. Statistical Analysis and Network Analysis
3. Results
3.1. Patient Characteristics
3.2. Clinical Outcomes
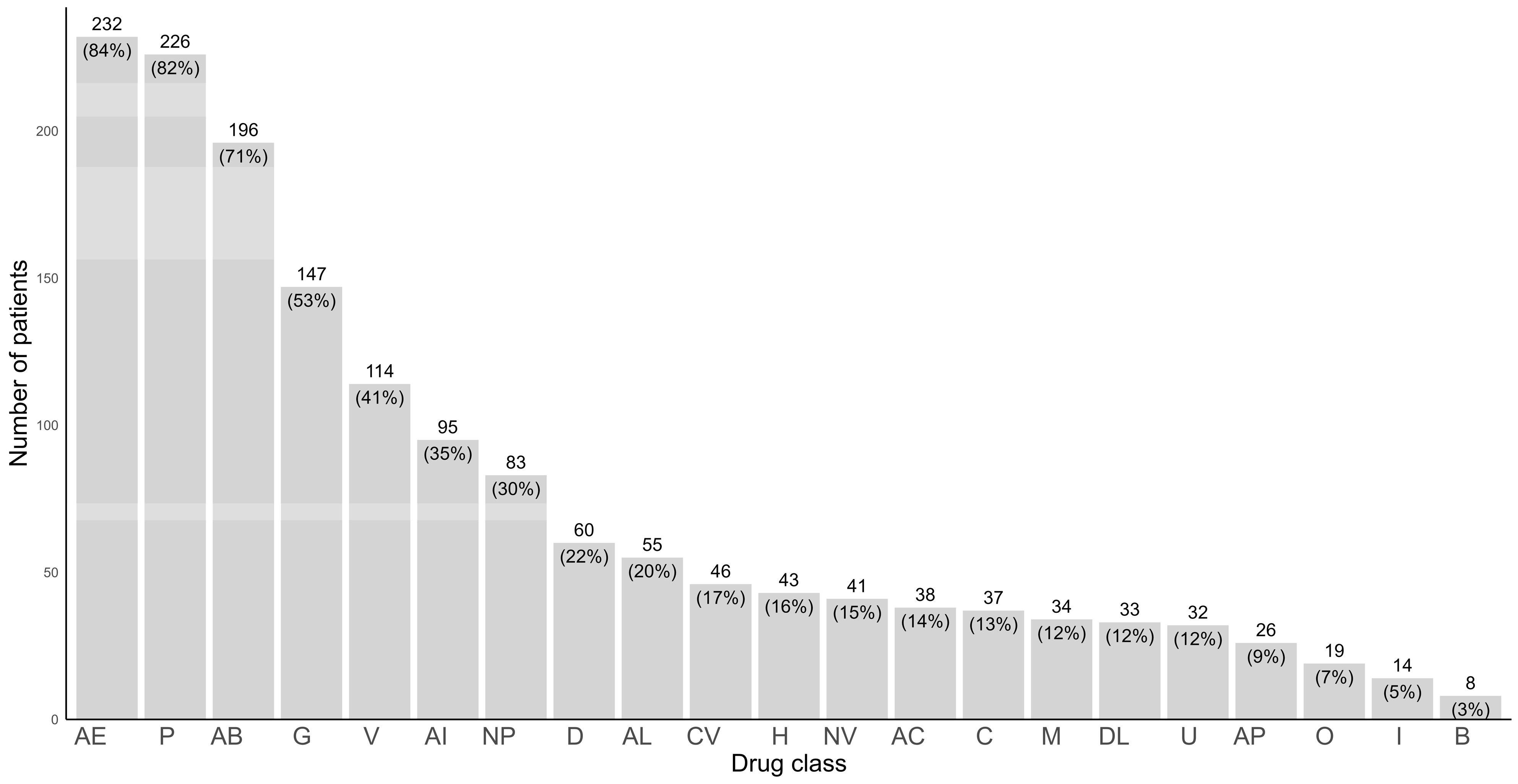
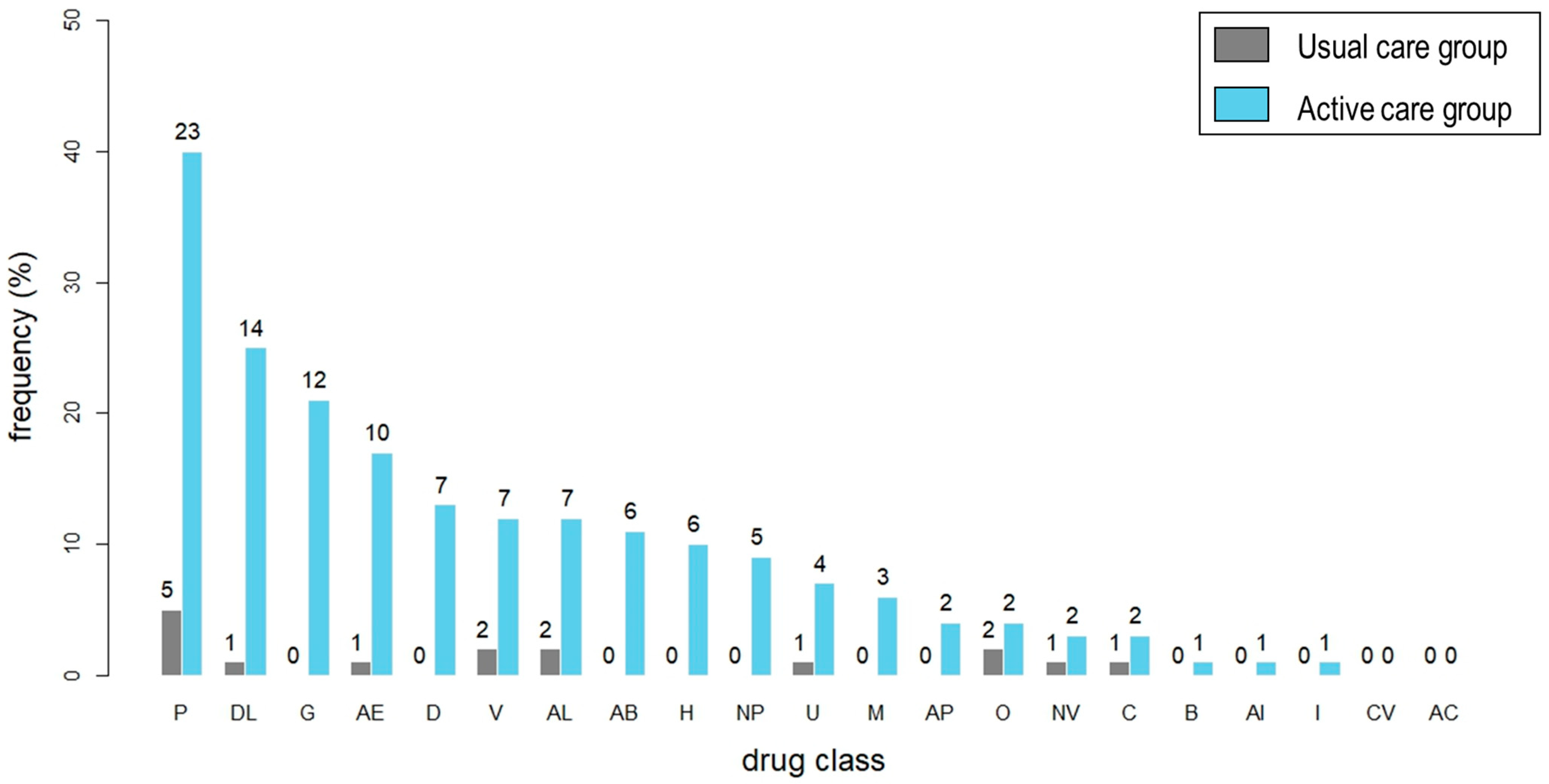
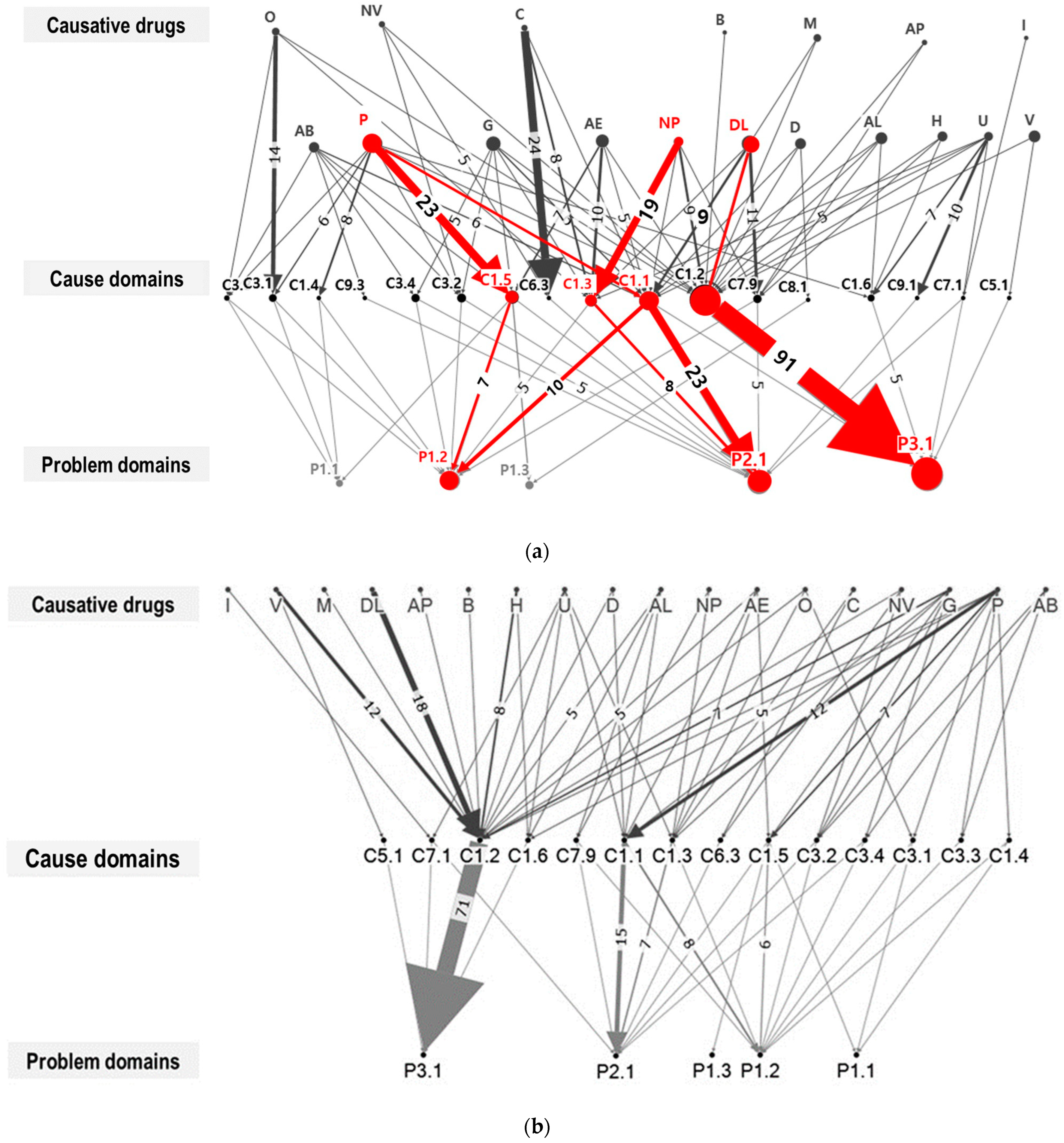
3.3. Implementability
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kim, C.G. Hospice & Palliative Care Policy in Korea. J. Hosp. Palliat. Care 2017, 20, 8–17. [Google Scholar]
- National Hospice Center & Ministry of Health and Welfare. Hospice & Palliative care in Korea: Facts & Figures 2017. Available online: https://hospice.go.kr:8444/index.html?menuno=22 (accessed on 29 October 2023).
- Hutchison, L. Biomedical Principles of Aging. In American Society of Health-System Pharmacists, Fundamentals of Geriatric Pharmacotherapy: An Evidence-Based Approach; Hutchison, L., Sleeper, R., Eds.; American Society of Health-System Pharmacists: Bethesda, MD, USA, 2015; pp. 57–76. [Google Scholar]
- Peralta, T.; Castel-Branco, M.M.; Reis-Pina, P.; Figueiredo, I.V.; Dourado, M. Prescription trends at the end of life in a palliative care unit: Observational study. BMC Palliat. Care 2022, 21, 65. [Google Scholar] [CrossRef] [PubMed]
- Fede, A.; Miranda, M.; Antonangelo, D.; Trevizan, L.; Schaffhausser, H.; Hamermesz, B.; Zimmermann, C.; Del Giglio, A.; Riechelmann, R.P. Use of unnecessary medications by patients with advanced cancer: Cross-sectional survey. Support. Care Cancer 2011, 19, 1313–1318. [Google Scholar] [CrossRef]
- Todd, A.; Husband, A.; Andrew, I.; Pearson, S.-A.; Lindsey, L.; Holmes, H. Inappropriate prescribing of preventative medication in patients with life-limiting illness: A systematic review. BMJ Support. Palliat. Care 2017, 7, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Park, S.; Yoo, S.H.; Choi, K.H.; Lee, J.-Y. Potentially inappropriate medication use based on two deprescribing criteria and related factors in patients with terminal cancer: A cross-sectional study. J. Geriatr. Oncol. 2023, 14, 101472. [Google Scholar] [CrossRef]
- Alkan, A.; Yaşar, A.; Karcı, E.; Köksoy, E.B.; Ürün, M.; Şenler, F.; Ürün, Y.; Tuncay, G.; Ergün, H.; Akbulut, H. Severe drug interactions and potentially inappropriate medication usage in elderly cancer patients. Support. Care Cancer 2017, 25, 229–236. [Google Scholar] [CrossRef] [PubMed]
- Hong, S.; Lee, J.H.; Chun, E.K.; Kim, K.-I.; Kim, S.H.; Lee, Y.-G.; Hwang, I.G.; Kim, J.Y.; Koh, S.-J.; Ko, Y.H.; et al. Polypharmacy, Inappropriate Medication Use, and Drug Interactions in Older Korean Patients with Cancer Receiving First-Line Palliative Chemotherapy. Oncolologist 2020, 25, e502–e511. [Google Scholar] [CrossRef]
- Ruiter, R.; Visser, L.E.; Rodenburg, E.M.; Trifiró, G.; Ziere, G.; Stricker, B.H. Adverse drug reaction-related hospitalizations in persons aged 55 years and over: A population-based study in the Netherlands. Drugs Aging 2012, 29, 225–232. [Google Scholar] [CrossRef]
- Chae, H.-W.; Kim, Y.; Suh, Y.; Lee, J.; Lee, E.; Lee, E.; Choi, J.-Y.; Kim, K.-I.; Lee, J.-Y. Prevalence of potentially inappropriate medications based on the STOPPFrail criteria in frail older patients with limited life expectancy: A cross-sectional study. BMC Geriatr. 2022, 22, 367. [Google Scholar] [CrossRef]
- Barlow, A.; Prusak, E.S.; Barlow, B.; Nightingale, G. Interventions to reduce polypharmacy and optimize medication use in older adults with cancer. J. Geriatr. Oncol. 2021, 12, 863–871. [Google Scholar] [CrossRef]
- Schenker, Y.; Park, S.Y.; Jeong, K.; Pruskowski, J.; Kavalieratos, D.; Resick, J.; Abernethy, A.; Kutner, J.S. Associations Between Polypharmacy, Symptom Burden, and Quality of Life in Patients with Advanced, Life-Limiting Illness. J. Gen. Intern. Med. 2019, 34, 559–566. [Google Scholar] [CrossRef] [PubMed]
- Woodward, M.C. Deprescribing: Achieving better health outcomes for older people through reducing medications. J. Pharm. Pract. Res. 2003, 33, 323–328. [Google Scholar] [CrossRef]
- Reeve, E.; Gnjidic, D.; Long, J.; Hilmer, S. A systematic review of the emerging definition of ‘deprescribing’ with network analysis: Implications for future research and clinical practice. Br. J. Clin. Pharmacol. 2015, 80, 1254–1268. [Google Scholar] [CrossRef] [PubMed]
- Coe, A.; Kaylor-Hughes, C.; Fletcher, S.; Murray, E.; Gunn, J. Deprescribing intervention activities mapped to guiding principles for use in general practice: A scoping review. BMJ Open 2021, 11, e052547. [Google Scholar] [CrossRef] [PubMed]
- Bemben, N.M. Deprescribing: An Application to Medication Management in Older Adults. Pharmacother. J. Hum. Pharmacol. Drug Ther. 2016, 36, 774–780. [Google Scholar] [CrossRef] [PubMed]
- Etherton-Beer, C.; Page, A.; Naganathan, V.; Potter, K.; Comans, T.; Hilmer, S.N.; McLachlan, A.J.; I Lindley, R.; Mangin, D. Deprescribing to optimise health outcomes for frail older people: A double-blind placebo-controlled randomised controlled trial—Outcomes of the Opti-med study. Age Ageing 2023, 52, afad081. [Google Scholar] [CrossRef]
- Lee, H.-G.; Kwon, S.; Jang, B.-H.; Jeon, J.P.; Lee, Y.-S.; Jung, W.-S.; Moon, S.-K.; Cho, K.-H. A Study on the Perceptions of Korean Older Adult Patients and Caregivers about Polypharmacy and Deprescribing. Int. J. Environ. Res. Public Health 2022, 19, 11446. [Google Scholar] [CrossRef] [PubMed]
- Lindsay, J.; Dooley, M.; Martin, J.; Fay, M.; Kearney, A.; Khatun, M.; Barras, M. The development and evaluation of an oncological palliative care deprescribing guideline: The ‘OncPal deprescribing guideline’. Support. Care Cancer 2015, 23, 71–78. [Google Scholar] [CrossRef]
- Curtin, D.; Gallagher, P.; O’mahony, D. Deprescribing in older people approaching end-of-life: Development and validation of STOPPFrail version 2. Age Ageing 2021, 50, 465–471. [Google Scholar] [CrossRef]
- McNeill, R.; Hanger, H.C.; Chieng, J.; Chin, P. Polypharmacy in Palliative Care: Two Deprescribing Tools Compared with a Clinical Review. J. Palliat. Med. 2021, 24, 661–667. [Google Scholar] [CrossRef]
- Whitman, A.; DeGregory, K.; Morris, A.; Mohile, S.; Ramsdale, E. Pharmacist-led medication assessment and deprescribing intervention for older adults with cancer and polypharmacy: A pilot study. Support. Care Cancer 2018, 26, 4105–4113. [Google Scholar] [CrossRef] [PubMed]
- Syversen, M.O.; Shah, S.F.; Mathiesen, L.; Mowé, M.; Lea, M. Effect of integrated medicines management on the quality of drug treatment in hospitalised multimorbid patients—A secondary endpoint analysis of a randomised controlled trial. Int. J. Pharm. Pract. 2023, 31, 314–320. [Google Scholar] [CrossRef] [PubMed]
- Geum, M.J.; Ahn, J.H.; Kim, J.S.; Kim, S.H.; Son, E.S.; Hu, Y.J.; Choi, H.J.; Rhie, S.J. Interprofessional Collaboration Between a Multidisciplinary Palliative Care Team and the Team Pharmacist on Pain Management. Am. J. Hosp. Palliat. Med. 2019, 36, 616–622. [Google Scholar] [CrossRef] [PubMed]
- Thillainadesan, J.; Gnjidic, D.; Green, S.; Hilmer, S.N. Impact of Deprescribing Interventions in Older Hospitalised Patients on Prescribing and Clinical Outcomes: A Systematic Review of Randomised Trials. Drugs Aging 2018, 35, 303–319. [Google Scholar] [CrossRef] [PubMed]
- Moody, J.J.; Poon, I.O.; Braun, U.K. The Role of an Inpatient Hospice and Palliative Clinical Pharmacist in the Interdisciplinary Team. Am. J. Hosp. Palliat. Palliat. Care 2022, 39, 856–864. [Google Scholar] [CrossRef]
- Herledan, C.; Cerfon, M.-A.; Baudouin, A.; Larbre, V.; Lattard, C.; Poletto, N.; Ranchon, F.; Rioufol, C. Impact of pharmaceutical care interventions on multidisciplinary care of older patients with cancer: A systematic review. J. Geriatr. Oncol. 2023, 14, 101450. [Google Scholar] [CrossRef]
- Basger, B.J.; Moles, R.J.; Chen, T.F. Uptake of pharmacist recommendations by patients after discharge: Implementation study of a patient-centered medicines review service. BMC Geriatr. 2023, 23, 183. [Google Scholar] [CrossRef]
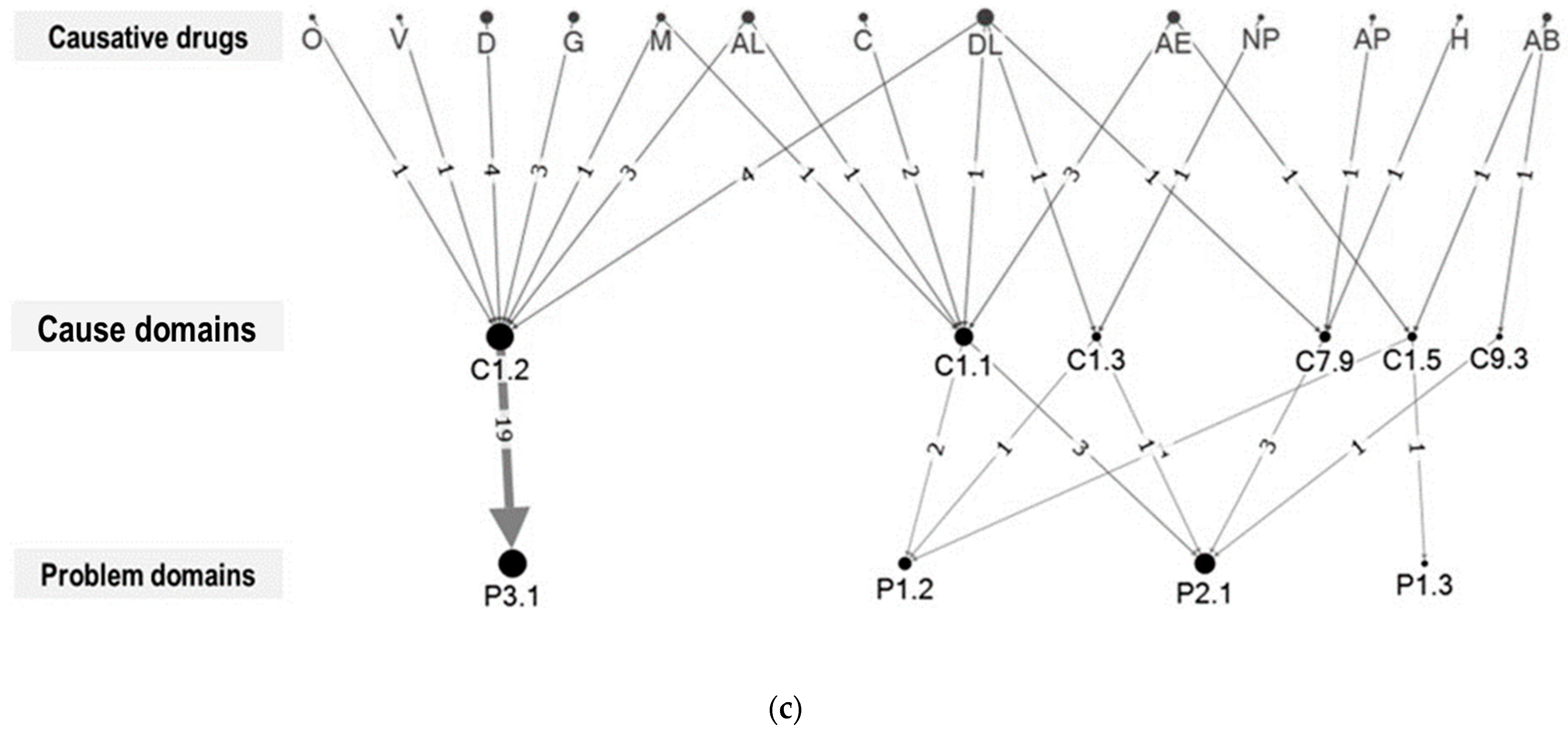
- Kim, M.G.; Jeong, C.R.; Kim, H.J.; Kim, J.H.; Song, Y.-K.; Kim, K.I.; Ji, E.; Yoon, S.-S.; Koh, Y.; Cho, Y.-S.; et al. Network analysis of drug-related problems in hospitalized patients with hematologic malignancies. Support. Care Cancer 2018, 26, 2737–2742. [Google Scholar] [CrossRef]
- Han, N.; Han, S.H.; Chu, H.; Kim, J.; Rhew, K.Y.; Yoon, J.-H.; Je, N.K.; Rhie, S.J.; Ji, E.; Lee, E.; et al. Service design oriented multidisciplinary collaborative team care service model development for resolving drug related problems. PLoS ONE 2018, 13, e0201705. [Google Scholar] [CrossRef]
- American Geriatrics Society 2019 Updated AGS Beers Criteria® for Potentially Inappropriate Medication Use in Older Adults. J. Am. Geriatr. Soc. 2019, 67, 674–694. [CrossRef]
- Pharmaceutical Care Network Europe (PCNE). Classification for Drug Related Problems V 9.1. 2020. Available online: https://www.pcne.org/working-groups/2/drug-related-problems (accessed on 29 October 2023).
- Lee, H.R.; Yi, S.Y.; Kim, D.Y. Evaluation of Prescribing Medications for Terminal Cancer Patients near Death: Essential or Futile. Cancer Res. Treat. 2013, 45, 220–225. [Google Scholar] [CrossRef] [PubMed]
- Overhage, J.M.; Lukes, A. Practical, reliable, comprehensive method for characterizing pharmacists’ clinical activities. Am. J. Health Syst. Pharm. 1999, 56, 2444–2450. [Google Scholar] [CrossRef] [PubMed]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Lee, S.; Lee, Y.J.; Kim, S.; Jo, Y.H.; Cho, Y.-S.; An, H.Y.; Hong, K.T.; Choi, J.Y.; Kang, H.J.; et al. Clinical and Economic Impact of Pharmacists’ Intervention on Care of Pediatric Hematology and Oncology Patients. J. Oncol. Pharm. Pract. 2021, 29, 319–325. [Google Scholar] [CrossRef] [PubMed]
- Hilgarth, H.; Wichmann, D.; Baehr, M.; Kluge, S.; Langebrake, C. Clinical pharmacy services in critical care: Results of an observational study comparing ward-based with remote pharmacy services. Int. J. Clin. Pharm. 2023, 45, 847–856. [Google Scholar] [CrossRef] [PubMed]
- Le, V.; Patel, N.; Nguyen, Q.; Woldu, H.; Nguyen, L.; Lee, A.; Deguzman, L.; Krishnaswami, A. Retrospective analysis of a pilot pharmacist-led hospice deprescribing program initiative. J. Am. Geriatr. Soc. 2021, 69, 1370–1376. [Google Scholar] [CrossRef]
- Scott, I.A.; Hilmer, S.N.; Reeve, E.; Potter, K.; Le Couteur, D.; Rigby, D.; Gnjidic, D.; Del Mar, C.B.; Roughead, E.E.; Page, A.; et al. Reducing inappropriate polypharmacy: The process of deprescribing. JAMA Intern. Med. 2015, 175, 827–834. [Google Scholar] [CrossRef]
- Tjia, J.; Ellington, L.; Clayton, M.F.; Lemay, C.; Reblin, M. Managing Medications During Home Hospice Cancer Care: The Needs of Family Caregivers. J. Pain Symptom. Manag. 2015, 50, 630–641. [Google Scholar] [CrossRef]
- Seol, E.-M.; Suh, Y.-S.; Ju, D.L.; Bae, H.J.; Kim, E.K.; Lee, H.-J. Nutrition Support Team Reconsultation During Nutrition Therapy in Korea. JPEN J. Parenter. Enter. Nutr. 2021, 45, 357–365. [Google Scholar] [CrossRef]
- Nguyen, K.; Subramanya, V.; Kulshreshtha, A. Risk Factors Associated With Polypharmacy and Potentially Inappropriate Medication Use in Ambulatory Care Among the Elderly in the United States: A Cross-Sectional Study. Drugs Real World Outcomes 2023, 10, 357–362. [Google Scholar] [CrossRef]
| Value of Service | Score | Criteria |
|---|---|---|
| Extremely significant | 4 | Recommendation qualified by extremely serious consequences or potential life-and-death situation |
| Very significant | 3 | Recommendation qualified by a potential or existing dysfunction in a major organ or avoidance of serious adverse drug interaction or contraindication to use |
| Significant | 2 | Recommendation would bring patient care to a more acceptable, appropriate level (i.e., standard of practice), including quality-of-life issues with evidence from the patient or documentation elsewhere, as well as issues of cost and convenience. |
| Somewhat significant | 1 | Patient’s benefit from the recommendation could be neutral depending on professional interpretation or more information or a clarification must be obtained by the pharmacist from the physician, nurse, or other appropriate health care professional before an order can be processed |
| No significance | 0 | Information only or recommendation not patient specific |
| Adverse significance | −1 | Recommendation inappropriate; its implementation may lead to adverse outcomes |
| Characteristics | UC Group (n = 100) | AC Group (n = 170) | p-Value |
|---|---|---|---|
| Age (yr) a | 66.5 [57–74.5] | 63 [56–72] | 0.22 |
| Sex (Female) | 47 (47.0%) | 75 (44.1%) | 0.74 |
| Cancer diagnosis | 0.12 | ||
| Non-small cell lung cancer | 13 (13.0%) | 37 (21.8%) | |
| Pancreatic cancer | 17 (17.0%) | 19 (11.2%) | |
| Others * | 70 (70.0%) | 114 (67.1%) | |
| Co-morbid diseases | |||
| Hypertension | 28 (28.0%) | 43 (25.3%) | 0.73 |
| Diabetes | 19 (19.0%) | 44 (25.9%) | 0.25 |
| Dyslipidemia | 10 (10.0%) | 13 (7.6%) | 0.66 |
| Ischemic heart disease | 30 (30.0%) | 51 (30.0%) | 1.00 |
| Chronic obstructive pulmonary disease | 4 (4.0%) | 8 (4.7%) | 1.00 |
| Performance status (ECOG score) | |||
| ≥3 | 97 (97.0%) | 159 (93.5%) | 0.61 |
| Diet | |||
| NPO | 15 (15.0%) | 21 (12.4%) | 0.28 |
| On total parenteral nutrition | 65 (65.0%) | 97 (57.1%) | 0.18 |
| History of chemotherapy | 91 (91.0%) | 160 (94.1%) | 0.45 |
| Continuation of cancer treatment | 0.06 | ||
| Chemotherapy | 16 (16.0%) | 46 (27.1%) | |
| Radiotherapy | 4 (4.0%) | 3 (1.8%) | |
| Follow-up duration a※ | 7.0 [4.0–14.0] | 9.0 [4.0–14.0] | 0.41 |
| Type of discharge | 0.02 | ||
| Expiration | 42 (42.0%) | 71 (41.8%) | |
| Places other than home † | 42 (42.0%) | 49 (28.8%) | |
| Home | 16 (16.0%) | 50 (29.4%) | |
| Department requesting consultation | 0.30 | ||
| Hemato-oncology | 75 (75.0%) | 116 (68.2%) | |
| Non hemato-oncology | 25 (25.0%) | 54 (31.8%) |
| Characteristics | UC Group (n = 100) | AC Group (n = 170) | p-Value |
|---|---|---|---|
| Number of medications | |||
| Number of total medications in use at the time of enrollment a | 9 [6–11] | 9.5 [7–13] | 0.04 |
| Number of oral medications in use at the time of enrollment a | 4 [1–7] | 5 [2–8] | 0.05 |
| Proportion (%) of polypharmacy | |||
| Proportion (%) of patients administering 5 or more drugs | 90 (90.0%) | 154 (90.6%) | 1.00 |
| Proportion (%) of patients administering 10 or more drugs | 39 (39.0%) | 85 (50.0%) | 0.10 |
| Causative Drug | Cause * | Problem * |
|---|---|---|
| Lipid lowering agents | C1.2. No indication for drug | P3.1. Unnecessary drug-treatment |
| Pain managing agents | C1.1. Inappropriate drug according to guidelines/formulary | P2.1. Adverse drug event (possibly) occurring |
| Pain managing agents | C1.1. Inappropriate drug according to guidelines/formulary | P1.2. Effect of drug treatment not optimal |
| Neuropsychiatric drugs | C1.3. Inappropriate combination of drugs, or drugs and herbal medications, or drugs and dietary supplements | P2.1. Adverse drug event (possibly) occurring |
| Pain managing agents | C1.5. No or incomplete drug treatment in spite of existing indication | P1.2. Effect of drug treatment not optimal |
| Total Number of Prescriptions of Preventive Medications in the UC Group (N) (N = 100) | Deprescribing Rate of Preventive Medications in the UC Group (N, (%)) (N = 100) | Total Number of Prescriptions of Preventive Medications in the AC Group (N) (N = 170) | Deprescribing Rate of Preventive Medications in the AC Group (N, (%)) (N = 170) | p-Value |
|---|---|---|---|---|
| 125 | 12 (10.4) | 270 | 80 (29.6) | <0.001 |
| Outcomes | UC Group (N = 100) | AC Group (N = 170) | Title 4 |
|---|---|---|---|
| Proportion of patients deprescribed one or more MRPs at discharge (frequency, %) | 3.00% (3/100) | 40.0% (68/170) | <0.001 * |
| Changes of pill burden a | 0 [−9–10] | 0 [−11, 7] | 0.13 |
| Change in proportion of patients with PP * at discharge (%) | −14% | −8.1% | 0.87 |
| Intervention Domain in PCNE Classification | Usual Care (UC) | Active Care (AC) | p-Value * | ||
|---|---|---|---|---|---|
| N (%) | Acceptance Rate (%) | N (%) | Acceptance Rate (%) | ||
| At prescriber level | 16 (100) | 68.8 | 199 (100) | 78.9 | 0.021 |
| I1.1 Prescriber informed only | 1 (6.2) | 0 | 36 (18.0) | 66.7 | |
| I1.2 Prescriber asked for information | 6 (37.5) | 100 | 10 (5.0) | 100 | |
| I1.3 Intervention proposed to prescriber | 9 (56.2) | 55.6 | 143 (71.5) | 81.8 | |
| I1.4 Intervention discussed with prescriber | 0 (0.0) | - | 10 (5.0) | 60 | |
| At patient level | - | - | 23 (100) | 100 | - |
| I2.1 Patient (drug) counseling | - | - | 5 (2.5) | 100 | |
| I2.2 Written information provided (only) | - | - | - | - | |
| I2.3 Patient referred to prescriber | - | - | - | - | |
| I2.4 Spoken to family member/caregiver | - | - | 18 (9) | 100 | |
| At drug level | 10 (100) | 30.0 | 186 (100) | 78.0 | 0.003 |
| I3.1 Drug changed to… | 1 (6.2) | 100 | 31 (15.5) | 74.2 | |
| I3.2 Dosage changed to… | 2 (12.5) | 0 | 21 (10.5) | 85.7 | |
| I3.3 Formulation changed to… | 0 (0.0) | - | 2 (1.0) | 100 | |
| I3.4 Instructions for use changed to… | 0 (0.0) | - | 5 (2.5) | 100 | |
| I3.5 Drug paused or stopped | 6 (37.5) | 66.7 | 116 (58.0) | 75 | |
| I3.6 Drug started | 1 (6.2) | 0 | 11 (5.5) | 90.9 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ko, M.; Kim, S.; Suh, S.Y.; Cho, Y.S.; Kim, I.-W.; Yoo, S.H.; Lee, J.-Y.; Oh, J.M. Consultation-Based Deprescribing Service to Optimize Palliative Care for Terminal Cancer Patients. J. Clin. Med. 2023, 12, 7431. https://doi.org/10.3390/jcm12237431
Ko M, Kim S, Suh SY, Cho YS, Kim I-W, Yoo SH, Lee J-Y, Oh JM. Consultation-Based Deprescribing Service to Optimize Palliative Care for Terminal Cancer Patients. Journal of Clinical Medicine. 2023; 12(23):7431. https://doi.org/10.3390/jcm12237431
Chicago/Turabian StyleKo, Minoh, Sunghwan Kim, Sung Yun Suh, Yoon Sook Cho, In-Wha Kim, Shin Hye Yoo, Ju-Yeun Lee, and Jung Mi Oh. 2023. "Consultation-Based Deprescribing Service to Optimize Palliative Care for Terminal Cancer Patients" Journal of Clinical Medicine 12, no. 23: 7431. https://doi.org/10.3390/jcm12237431
APA StyleKo, M., Kim, S., Suh, S. Y., Cho, Y. S., Kim, I.-W., Yoo, S. H., Lee, J.-Y., & Oh, J. M. (2023). Consultation-Based Deprescribing Service to Optimize Palliative Care for Terminal Cancer Patients. Journal of Clinical Medicine, 12(23), 7431. https://doi.org/10.3390/jcm12237431






