Patient-Related Factors Associated with Adverse Outcomes Following Weaning from Veno-Arterial Extracorporeal Membrane Oxygenation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Ethical Approval
2.2. Patient Selection
2.3. Clinical and Hemodynamic Parameters
2.4. Echocardiography
2.5. Endpoint Definition
2.6. Statistical Analysis
3. Results
3.1. Baseline Patient Demographics and Clinical Characteristics
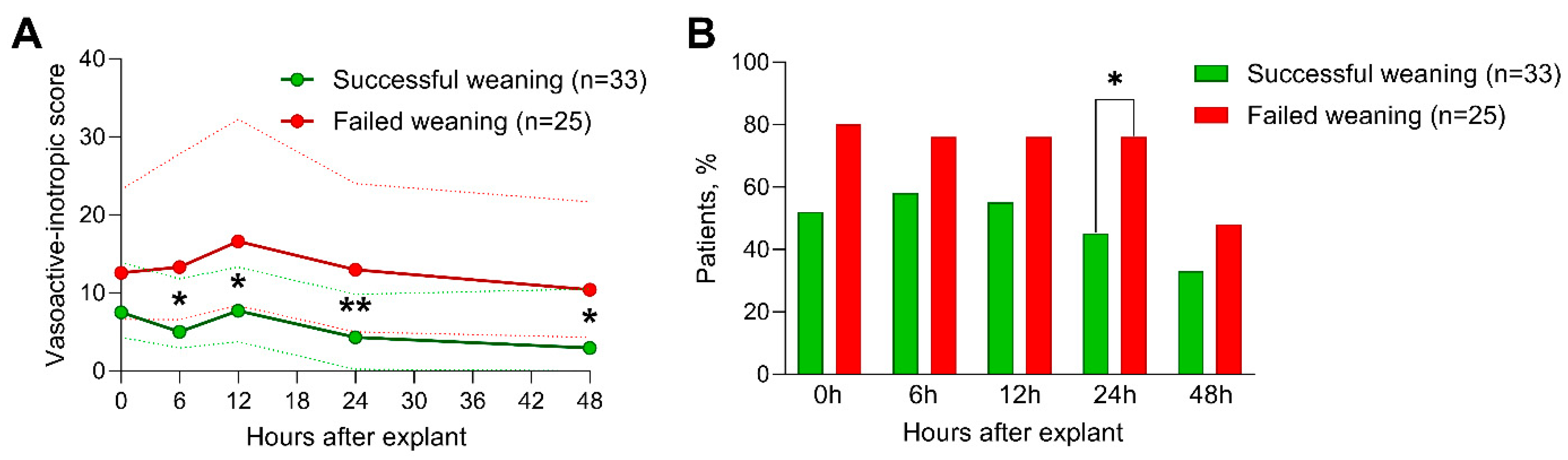
3.2. Vasoactive-Inotropic Agents and Echocardiography
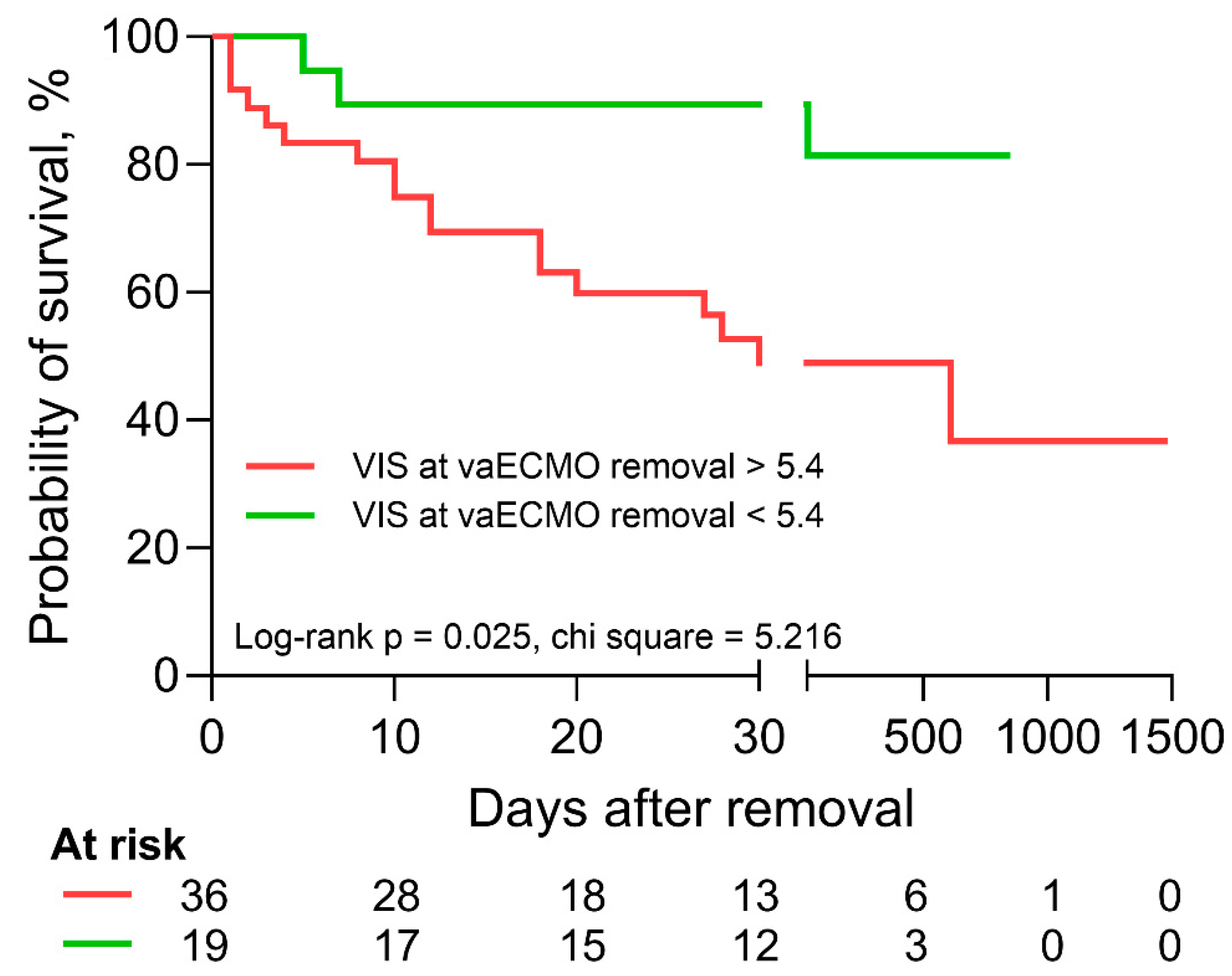
3.3. Association with Outcome
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CI | confidence interval |
| EF | ejection fraction |
| GLS | global longitudinal strain |
| HR | hazard ratio |
| ICU | intensive care unit |
| LV | left ventricle/left ventricular |
| OR | odds ratio |
| RV | right ventricle/right ventricular |
| SAPS | Simplified Acute Physiology Score |
| vaECMO | veno-arterial extracorporeal membrane oxygenation |
| VIS | vasoactive-inotropic score |
References
- Pellegrino, V.; Hockings, L.E.; Davies, A. Veno-arterial extracorporeal membrane oxygenation for adult cardiovascular failure. Curr. Opin. Crit. Care 2014, 20, 484–492. [Google Scholar] [CrossRef]
- Ostadal, P.; Rokyta, R.; Karasek, J.; Kruger, A.; Vondrakova, D.; Janotka, M.; Naar, J.; Smalcova, J.; Hubatova, M.; Hromadka, M.; et al. Extracorporeal Membrane Oxygenation in the Therapy of Cardiogenic Shock: Results of the ECMO-CS Randomized Clinical Trial. Circulation 2023, 147, 454–464. [Google Scholar] [CrossRef]
- Lüsebrink, E.; Stremmel, C.; Stark, K.; Joskowiak, D.; Czermak, T.; Born, F.; Kupka, D.; Scherer, C.; Orban, M.; Petzold, T.; et al. Update on Weaning from Veno-Arterial Extracorporeal Membrane Oxygenation. J. Clin. Med. 2020, 9, 992. [Google Scholar] [CrossRef]
- Schmidt, M.; Burrell, A.; Roberts, L.; Bailey, M.; Sheldrake, J.; Rycus, P.T.; Hodgson, C.; Scheinkestel, C.; Cooper, D.J.; Thiagarajan, R.R.; et al. Predicting survival after ECMO for refractory cardiogenic shock: The survival after veno-arterial-ECMO (SAVE)-score. Eur. Heart J. 2015, 36, 2246–2256. [Google Scholar] [CrossRef]
- Amin, F.; Lombardi, J.; Alhussein, M.; Posada, J.D.; Suszko, A.; Koo, M.; Fan, E.; Ross, H.; Rao, V.; Alba, A.C.; et al. Predicting Survival After VA-ECMO for Refractory Cardiogenic Shock: Validating the SAVE Score. CJC Open 2021, 3, 71–81. [Google Scholar] [CrossRef]
- Ortuno, S.; Delmas, C.; Diehl, J.L.; Bailleul, C.; Lancelot, A.; Naili, M.; Cholley, B.; Pirracchio, R.; Aissaoui, N. Weaning from veno-arterial extra-corporeal membrane oxygenation: Which strategy to use? Ann. Cardiothorac. Surg. 2019, 8, E1–E8. [Google Scholar] [CrossRef]
- Burgos, L.M.; Seoane, L.; Diez, M.; Baro Vila, R.C.; Furmento, J.F.; Vrancic, M.; Aissaoui, N. Multiparameters associated to successful weaning from VA ECMO in adult patients with cardiogenic shock or cardiac arrest: Systematic review and meta-analysis. Ann. Card. Anaesth. 2023, 26, 4–11. [Google Scholar] [CrossRef]
- Charbonneau, F.; Chahinian, K.; Bebawi, E.; Lavigueur, O.; Lévesque, É.; Lamarche, Y.; Serri, K.; Albert, M.; Noly, P.E.; Cournoyer, A.; et al. Parameters associated with successful weaning of veno-arterial extracorporeal membrane oxygenation: A systematic review. Crit. Care 2022, 26, 375. [Google Scholar] [CrossRef]
- Le Gall, J.R.; Lemeshow, S.; Saulnier, F. A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. Jama 1993, 270, 2957–2963. [Google Scholar] [CrossRef]
- Gaies, M.G.; Gurney, J.G.; Yen, A.H.; Napoli, M.L.; Gajarski, R.J.; Ohye, R.G.; Charpie, J.R.; Hirsch, J.C. Vasoactive-inotropic score as a predictor of morbidity and mortality in infants after cardiopulmonary bypass. Pediatr. Crit. Care Med. 2010, 11, 234–238. [Google Scholar] [CrossRef]
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 2015, 28, 1–39.e14. [Google Scholar] [CrossRef] [PubMed]
- Tsangaris, A.; Alexy, T.; Kalra, R.; Kosmopoulos, M.; Elliott, A.; Bartos, J.A.; Yannopoulos, D. Overview of Veno-Arterial Extracorporeal Membrane Oxygenation (VA-ECMO) Support for the Management of Cardiogenic Shock. Front. Cardiovasc. Med. 2021, 8, 686558. [Google Scholar] [CrossRef] [PubMed]
- Thiele, H.; Zeymer, U.; Akin, I.; Behnes, M.; Rassaf, T.; Mahabadi, A.A.; Lehmann, R.; Eitel, I.; Graf, T.; Seidler, T.; et al. Extracorporeal Life Support in Infarct-Related Cardiogenic Shock. N. Engl. J. Med. 2023, 389, 1286–1297. [Google Scholar] [CrossRef] [PubMed]
- Low, C.J.W.; Ramanathan, K.; Ling, R.R.; Ho, M.J.C.; Chen, Y.; Lorusso, R.; MacLaren, G.; Shekar, K.; Brodie, D. Extracorporeal cardiopulmonary resuscitation versus conventional cardiopulmonary resuscitation in adults with cardiac arrest: A comparative meta-analysis and trial sequential analysis. Lancet Respir. Med. 2023, 11, 883–893. [Google Scholar] [CrossRef] [PubMed]
- Sertic, F.; Chavez, L.; Diagne, D.; Richards, T.; Wald, J.; Acker, M.; Birati, E.; Rame, E.; Bermudez, C. Predictors of in-hospital mortality and midterm outcomes of patients successfully weaned from venoarterial extracorporeal membrane oxygenation. J. Thorac. Cardiovasc. Surg. 2021, 161, 666–678.e663. [Google Scholar] [CrossRef] [PubMed]
- Fernando, S.M.; MacLaren, G.; Barbaro, R.P.; Mathew, R.; Munshi, L.; Madahar, P.; Fried, J.A.; Ramanathan, K.; Lorusso, R.; Brodie, D.; et al. Age and associated outcomes among patients receiving venoarterial extracorporeal membrane oxygenation-analysis of the Extracorporeal Life Support Organization registry. Intensive Care Med. 2023. [Google Scholar] [CrossRef]
- Eckman, P.M.; Katz, J.N.; El Banayosy, A.; Bohula, E.A.; Sun, B.; van Diepen, S. Veno-Arterial Extracorporeal Membrane Oxygenation for Cardiogenic Shock: An Introduction for the Busy Clinician. Circulation 2019, 140, 2019–2037. [Google Scholar] [CrossRef]
- Thiagarajan, R.R.; Barbaro, R.P.; Rycus, P.T.; McMullan, D.M.; Conrad, S.A.; Fortenberry, J.D.; Paden, M.L. Extracorporeal Life Support Organization Registry International Report 2016. Asaio J. 2017, 63, 60–67. [Google Scholar] [CrossRef]
- Cusanno, A.; Aissaoui, N.; Minville, V.; Porterie, J.; Biendel, C.; Volle, K.; Crognier, L.; Conil, J.M.; Delmas, C. Predictors of weaning failure in case of VA ECMO implantation. Sci. Rep. 2022, 12, 13842. [Google Scholar] [CrossRef]
- Xie, H.; Yang, F.; Hou, D.; Wang, X.; Wang, L.; Wang, H.; Hou, X. Risk factors of in-hospital mortality in adult postcardiotomy cardiogenic shock patients successfully weaned from venoarterial extracorporeal membrane oxygenation. Perfusion 2020, 35, 417–426. [Google Scholar] [CrossRef]
- Dunton, K.; Weeks, P.A.; Gulbis, B.; Jumean, M.; Kumar, S.; Janowiak, L.; Banjac, I.; Radovancevic, R.; Gregoric, I.; Kar, B. Evaluation of Vasoactive-Inotropic Score and Survival to Decannulation in Adult Patients on Venoarterial Extracorporeal Life Support: An Observational Cohort Study. Asaio J. 2023, 69, 873–878. [Google Scholar] [CrossRef] [PubMed]
- Aissaoui, N.; Luyt, C.E.; Leprince, P.; Trouillet, J.L.; Léger, P.; Pavie, A.; Diebold, B.; Chastre, J.; Combes, A. Predictors of successful extracorporeal membrane oxygenation (ECMO) weaning after assistance for refractory cardiogenic shock. Intensive Care Med. 2011, 37, 1738–1745. [Google Scholar] [CrossRef] [PubMed]
- Platts, D.G.; Sedgwick, J.F.; Burstow, D.J.; Mullany, D.V.; Fraser, J.F. The role of echocardiography in the management of patients supported by extracorporeal membrane oxygenation. J. Am. Soc. Echocardiogr. 2012, 25, 131–141. [Google Scholar] [CrossRef] [PubMed]
- Aissaoui, N.; Guerot, E.; Combes, A.; Delouche, A.; Chastre, J.; Leprince, P.; Leger, P.; Diehl, J.L.; Fagon, J.Y.; Diebold, B. Two-dimensional strain rate and Doppler tissue myocardial velocities: Analysis by echocardiography of hemodynamic and functional changes of the failed left ventricle during different degrees of extracorporeal life support. J. Am. Soc. Echocardiogr. 2012, 25, 632–640. [Google Scholar] [CrossRef] [PubMed]
- Alonso-Fernandez-Gatta, M.; Merchan-Gomez, S.; Gonzalez-Cebrian, M.; Diego-Nieto, A.; Gonzalez-Martin, J.; Toranzo-Nieto, I.; Barrio, A.; Martin-Herrero, F.; Sanchez, P.L. Echocardiographic Prediction of Successful Weaning From Venoarterial Extracorporeal Membrane Oxygenation. Am. J. Crit. Care 2022, 31, 483–493. [Google Scholar] [CrossRef] [PubMed]
- Santise, G.; Panarello, G.; Ruperto, C.; Turrisi, M.; Pilato, G.; Giunta, A.; Sciacca, S.; Pilato, M. Extracorporeal membrane oxygenation for graft failure after heart transplantation: A multidisciplinary approach to maximize weaning rate. Int. J. Artif. Organs 2014, 37, 706–714. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.; Jang, W.J.; Park, T.K.; Cho, Y.H.; Choi, J.O.; Jeon, E.S.; Yang, J.H. Echocardiographic Predictors of Successful Extracorporeal Membrane Oxygenation Weaning After Refractory Cardiogenic Shock. J. Am. Soc. Echocardiogr. 2021, 34, 414–422.e414. [Google Scholar] [CrossRef] [PubMed]
- Huang, K.C.; Lin, L.Y.; Chen, Y.S.; Lai, C.H.; Hwang, J.J.; Lin, L.C. Three-Dimensional Echocardiography-Derived Right Ventricular Ejection Fraction Correlates with Success of Decannulation and Prognosis in Patients Stabilized by Venoarterial Extracorporeal Life Support. J. Am. Soc. Echocardiogr. 2018, 31, 169–179. [Google Scholar] [CrossRef]
- Montero, S.; Huang, F.; Rivas-Lasarte, M.; Chommeloux, J.; Demondion, P.; Bréchot, N.; Hékimian, G.; Franchineau, G.; Persichini, R.; Luyt, C.; et al. Awake venoarterial extracorporeal membrane oxygenation for refractory cardiogenic shock. Eur. Heart J. Acute Cardiovasc. Care 2021, 10, 585–594. [Google Scholar] [CrossRef]
- Luedi, M.; Friess, J.O.; Erdoes, G. Veno-Arterial ECMO Weaning Failure in the Operating Room: Have You Considered Preweaning Bronchoscopy? Artif. Organs 2018, 42, 1234–1235. [Google Scholar] [CrossRef]
| All Patients (n = 58) | Successful Weaning (n = 33) | Failed Weaning (n = 25) | p-Value | |
|---|---|---|---|---|
| Demographics | ||||
| Percentage of total, % | 100 | 57 | 43 | - |
| Age, years | 57 ± 14 | 54 ± 14 | 62 ± 12 | 0.029 |
| Female sex, n | 17 (29%) | 9 (27%) | 8 (32%) | 0.902 |
| Body mass index (kg/m2) | 27.2 (23.9–29.4) | 25.8 (23.8–28.8) | 27.8 (24.8–30.3) | 0.120 |
| Disease severity and comorbidities at ICU admission | ||||
| SAPS II | 47 ± 12 | 49 ± 12 | 45 ± 12 | 0.242 |
| Chronic lung disease, n | 3 (5%) | 2 (6%) | 1 (4%) | 0.796 |
| Coronary artery disease, n | 19 (33%) | 9 (27%) | 10 (40%) | 0.445 |
| Arterial hypertension, n | 30 (52%) | 17 (52%) | 13 (52%) | 0.791 |
| Chronic kidney disease, n | 5 (9%) | 5 (15%) | 0 (0%) | 0.121 |
| History of stroke, n | 4 (7%) | 1 (3%) | 3 (12%) | 0.414 |
| Outcome | ||||
| ICU length of stay, days | 27 ± 16 | 30 ± 19 | 24 ± 11 | 0.151 |
| ICU mortality, n | 22 (38%) | 2 (6%) | 20 (80%) | <0.001 |
| In-hospital mortality, n | 23 (40%) | 2 (6%) | 21 (84%) | <0.001 |
| 14-day mortality, n | 15 (26%) | 0 (0%) | 15 (60%) | <0.001 |
| 28-day mortality, n | 22 (38%) | 0 (0%) | 22 (88%) | <0.001 |
| Survival post-removal, days | 27 (10–262) | 175 (27–558) | 10 (2–19) | <0.001 |
| All Patients (n = 58) | Successful Weaning (n = 33) | Failed Weaning (n = 25) | p-Value | |
|---|---|---|---|---|
| Indications for vaECMO support | ||||
| Acute ischemic or valvular cardiogenic shock, n | 29 (50%) | 17 (52%) | 12 (48%) | 0.875 |
| Decompensated chronic heart failure, n | 1 (2%) | 1 (3%) | 0 (0%) | 0.207 |
| Severe pulmonary artery embolism, n | 1 (2%) | 1 (3%) | 0 (0%) | 0.207 |
| eCPR, n | 27 (46%) | 14 (42%) | 13 (52%) | 0.624 |
| Treatment during vaECMO support | ||||
| Mechanical ventilation prior to vaECMO implantation, n | 32 (55%) | 16 (49%) | 16 (64%) | 0.384 |
| Mechanical ventilation at the time of vaECMO removal, n | 43 (74%) | 23 (70%) | 20 (80%) | 0.576 |
| Total vaECMO run time, days | 9 (5–13) | 7 (5–11) | 10 (8–14) | 0.093 |
| Renal replacement therapy total, n | 26 (45%) | 13 (39%) | 13 (52%) | 0.472 |
| Renal replacement therapy at the time of vaECMO removal, n | 17 (29%) | 9 (27%) | 8 (32%) | 0.0902 |
| Complications of vaECMO support | ||||
| Hemorrhagic complications, n | 21 (36%) | 8 (24%) | 13 (52%) | 0.055 |
| Received blood transfusions, n | 55 (95%) | 30 (91%) | 25 (100%) | 0.348 |
| Limb ischemia, n | 1 (2%) | 1 (3%) | 0 (0%) | 0.881 |
| All Patients (n = 58) | Successful Weaning (n = 33) | Failed Weaning (n = 25) | p-Value | |
|---|---|---|---|---|
| Transesophageal echocardiography, n | 36 (62%) | 17 (52%) | 19 (76%) | 0.111 |
| vaECMO flow at time of echocardiography, L/min | 3.1 ± 1.0 | 3.0 ± 1.0 | 3.2 ± 1.0 | 0.357 |
| LV IDd, mm | 49 ± 9 | 50 ± 11 | 48 ± 8 | 0.555 |
| LV EDV, mL | 139 ± 61 | 135 ± 55 | 145 ± 70 | 0.552 |
| LV EDVi, mL/m2 | 70 ± 31 | 70 ± 29 | 70 ± 35 | 0.988 |
| LV ESV, mL | 92 ± 46 | 89 ± 42 | 97 ± 52 | 0.543 |
| LV ESVi, mL/m2 | 47 ± 24 | 46 ± 22 | 47 ± 26 | 0.933 |
| LV GLS, % | −8.8 ± 5.2 | −8.9 ± 5.5 | −8.8 ± 4.9 | 0.922 |
| LV EF, % | 35 ± 12 | 35 ± 12 | 34 ± 13 | 0.773 |
| RV IDd basal, mm | 35 ± 8 | 34 ± 9 | 37 ± 8 | 0.169 |
| RV IDd, mid, mm | 27 ± 7 | 26 ± 7 | 28 ± 7 | 0.208 |
| RV length, mm | 70 ± 15 | 70 ± 16 | 70 ± 13 | 0.895 |
| RV FAC, % | 33 ± 10 | 32 ± 9 | 35 ± 10 | 0.189 |
| RV GLS, % | −12.1 ± 6.0 | −11.5 ± 5.6 | −12.9 ± 6.6 | 0.382 |
| All Patients (n = 58) | Successful Weaning (n = 33) | Failed Weaning (n = 25) | p-Value | |
|---|---|---|---|---|
| VISat time of echocardiography | 5.0 (1.7–12.7) | 5.0 (0–13.0) | 6.8 (4.0–14.1) | 0.201 |
| Necessity of inotropic agents at time of echocardiography, n | 26 (45%) | 11 (33%) | 15 (60%) | 0.075 |
| VISat time of vaECMO removal | 11.9 (5.0–18.3) | 7.5 (3.1–17.1) | 12.6 (6.7–21.8) | 0.107 |
| Necessity of inotropic agents at time of vaECMO removal, n | 37 (64%) | 17 (52%) | 20 (80%) | 0.054 |
| Norepinephrine dose at the time of vaECMO removal, µg/kg/min | 0.07 (0–0.14) | 0.03 (0–0.13) | 0.08 (0.02–0.14) | 0.254 |
| Dobutamine dose at the time of vaECMO removal, µg/kg/min | 0 (0–2.5) | 0 (0–0) | 0 (0–5.0) | 0.008 |
| Milrinone dose at the time of vaECMO removal, µg/kg/min | 0.26 (0–0.50) | 0.25 (0–0.47) | 0.26 (0–0.50) | 0.811 |
| VIS6 h post-removal | 9.4 (3.1–20.0) | 5.0 (2.3–14.1) | 13.3 (6.9–26.7) | 0.016 |
| Necessity of inotropic agents 6 h post-removal, n | 38 (66%) | 19 (58%) | 19 (76%) | 0.250 |
| VIS12 h post-removal | 10.4 (3.8–23.6) | 7.1 (3.1–16.6) | 16.6 (8.5–31.8) | 0.015 |
| Necessity of inotropic agents 12 h post-removal, n | 37 (64%) | 18 (55%) | 19 (76%) | 0.169 |
| VIS24 h post-removal | 8.0 (1.8–18.0) | 4.3 (0–11.6) | 13.0 (5.0–23.9) | 0.009 |
| Necessity of inotropic agents 24 h post-removal, n | 34 (59%) | 15 (45%) | 19 (76%) | 0.036 |
| VIS48 h post-removal | 5.9 (0–14.5) | 3.0 (0–11.7) | 10.4 (4.5–20.3) | 0.021 |
| Necessity of inotropic agents 48 h post-removal, n | 23 (40%) | 11 (33%) | 12 (48%) | 0.376 |
| OR (95% CI) | p-Value | |
|---|---|---|
| Age, years | 0.952 (0.909–0.997) | 0.038 |
| SAPS II at admission | 1.027 (0.982–1.074) | 0.241 |
| VISat time of echocardiography | 0.974 (0.920–1.031) | 0.358 |
| Inotropic agents at time of echocardiography | 0.333 (0.113–0.981) | 0.046 |
| VISat time of vaECMO removal | 0.975 (0.938–1.013) | 0.193 |
| Inotropic agents at time of vaECMO removal | 0.266 (0.081–0.877) | 0.030 |
| Dobutamine dose at the time of vaECMO removal | 0.649 (0.473–0.890) | 0.007 |
| Univariable HR (95% CI) | Univariable p-Value | Multivariable HR (95% CI) | Multivariable p-Value | |
|---|---|---|---|---|
| Age, years | 1.045 (1.006–1.086) | 0.025 | 1.048 (1.006–1.091) | 0.024 |
| SAPS II at admission | 1.001 (0.969–1.034) | 0.955 | ||
| VIS at time of echocardiography | 1.032 (0.994–1.071) | 0.102 | ||
| Inotropic agents at time of echocardiography | 1.963 (0.873–4.415) | 0.105 | ||
| VIS at time of vaECMO removal | 1.029 (1.003–1.055) | 0.027 | 1.030 (1.004–1.056) | 0.025 |
| Inotropic agents at time of vaECMO removal | 0.503 (0.199–1.270) | 0.148 | ||
| Dobutamine dose at the time of vaECMO removal | 1.232 (1.036–1.466) | 0.029 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Keller, M.; Gloeckner, H.; Sari-Yavuz, S.; Haeberle, H.A.; Schlensak, C.; Rosenberger, P.; Magunia, H.; Koeppen, M. Patient-Related Factors Associated with Adverse Outcomes Following Weaning from Veno-Arterial Extracorporeal Membrane Oxygenation. J. Clin. Med. 2023, 12, 7406. https://doi.org/10.3390/jcm12237406
Keller M, Gloeckner H, Sari-Yavuz S, Haeberle HA, Schlensak C, Rosenberger P, Magunia H, Koeppen M. Patient-Related Factors Associated with Adverse Outcomes Following Weaning from Veno-Arterial Extracorporeal Membrane Oxygenation. Journal of Clinical Medicine. 2023; 12(23):7406. https://doi.org/10.3390/jcm12237406
Chicago/Turabian StyleKeller, Marius, Henning Gloeckner, Sibel Sari-Yavuz, Helene A. Haeberle, Christian Schlensak, Peter Rosenberger, Harry Magunia, and Michael Koeppen. 2023. "Patient-Related Factors Associated with Adverse Outcomes Following Weaning from Veno-Arterial Extracorporeal Membrane Oxygenation" Journal of Clinical Medicine 12, no. 23: 7406. https://doi.org/10.3390/jcm12237406
APA StyleKeller, M., Gloeckner, H., Sari-Yavuz, S., Haeberle, H. A., Schlensak, C., Rosenberger, P., Magunia, H., & Koeppen, M. (2023). Patient-Related Factors Associated with Adverse Outcomes Following Weaning from Veno-Arterial Extracorporeal Membrane Oxygenation. Journal of Clinical Medicine, 12(23), 7406. https://doi.org/10.3390/jcm12237406







