External Stenting for Saphenous Vein Grafts in Coronary Surgery: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Protocol Registration
2.2. Device Description
2.3. Search Strategy
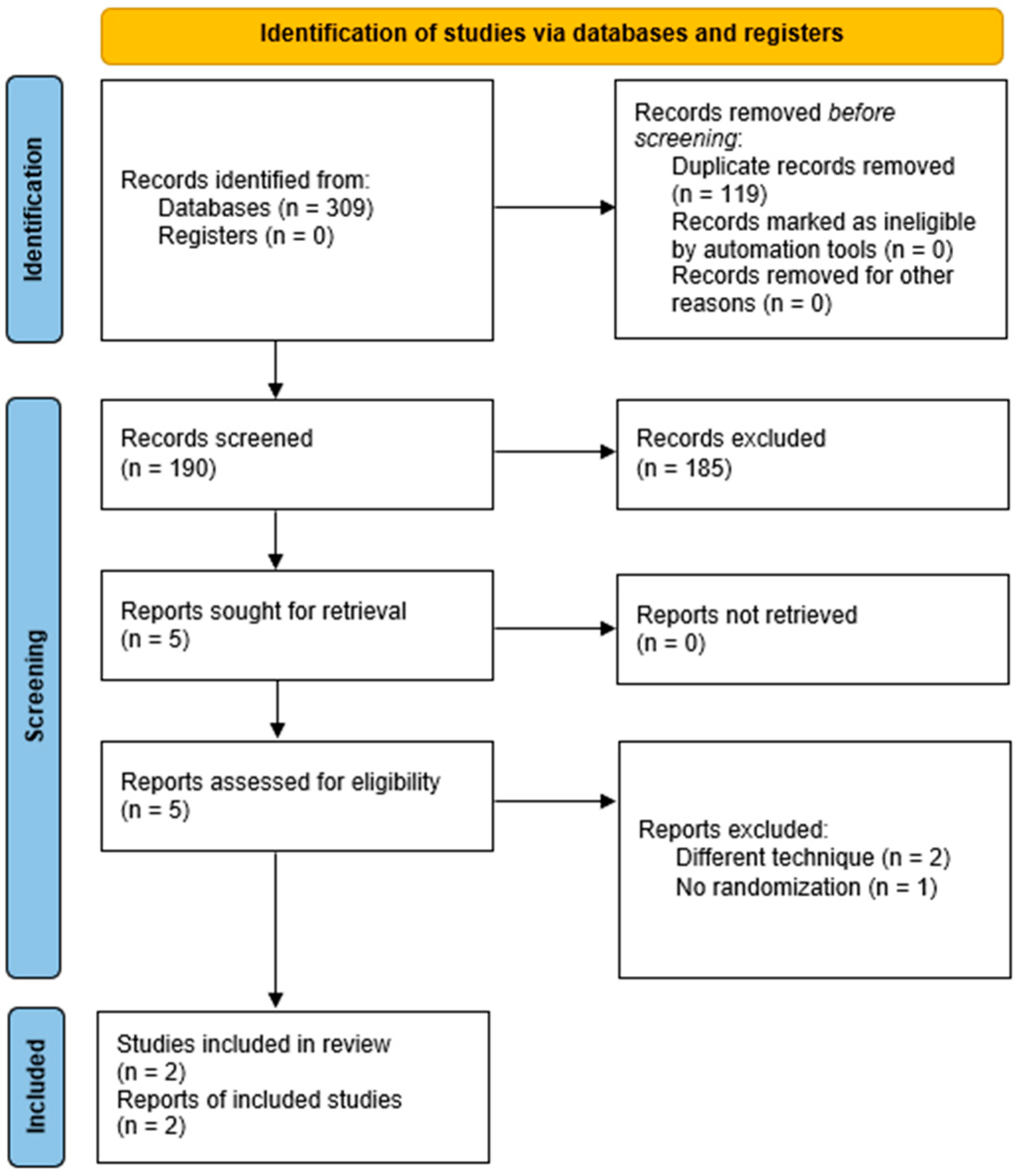
2.4. Study Selection
2.5. Data Abstraction and Risk of Bias Assessment
2.6. Outcomes and Definitions
2.7. Statistical Analysis
3. Results
3.1. Primary Outcome
3.2. Secondary Outcomes
4. Discussion
5. Conclusions
Limitations
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kim, K.M.; Arghami, A.; Habib, R.; Daneshmand, M.A.; Parsons, N.; Elhalabi, Z.; Krohn, C.; Thourani, V.; Bowdish, M.E. The Society of Thoracic Surgeons Adult Cardiac Surgery Database: 2022 Update on Outcomes and Research. Ann. Thorac. Surg. 2023, 115, 566–574. [Google Scholar] [CrossRef] [PubMed]
- Fitzgibbon, G.M.; Kafka, H.P.; Leach, A.J.; Keon, W.J.; Hooper, G.D.; Burton, J.R. Coronary bypass graft fate and patient outcome: Angiographic follow-up of 5,065 grafts related to survival and reoperation in 1,388 patients during 25 years. J. Am. Coll. Cardiol. 1996, 28, 616–626. [Google Scholar] [CrossRef] [PubMed]
- Caliskan, E.; de Souza, D.R.; Böning, A.; Liakopoulos, O.J.; Choi, Y.-H.; Pepper, J.; Gibson, C.M.; Perrault, L.P.; Wolf, R.K.; Kim, K.-B.; et al. Saphenous vein grafts in contemporary coronary artery bypass graft surgery. Nat. Rev. Cardiol. 2020, 17, 155–169. [Google Scholar] [CrossRef]
- Alexander, J.H.; Hafley, G.; Harrington, R.A.; Peterson, E.D.; Ferguson, T.B.; Lorenz, T.J.; Goyal, A.; Gibson, M.; Mack, M.J.; Gennevois, D.; et al. Efficacy and safety of edifoligide, an E2F transcription factor decoy, for prevention of vein graft failure following coronary artery bypass graft surgery: PREVENT IV: A randomized controlled trial. JAMA 2005, 294, 2446–2454. [Google Scholar]
- Ben-Gal, Y.; Taggart, D.P.; Williams, M.R.; Orion, E.; Uretzky, G.; Shofti, R.; Banai, S.; Yosef, L.; Bolotin, G. Expandable external support device to improve Saphenous Vein Graft Patency after CABG. J. Cardiothorac. Surg. 2013, 8, 122. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- McGuinness, L.A.; Higgins, J.P.T. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res. Synth. Methods 2021, 12, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Taggart, D.P.; Gavrilov, Y.; Krasopoulos, G.; Rajakaruna, C.; Zacharias, J.; De Silva, R.; Channon, K.M.; Gehrig, T.; Donovan, T.J.; Friedrich, I.; et al. External stenting and disease progression in saphenous vein grafts two years after coronary artery bypass grafting: A multicenter randomized trial. J. Thorac. Cardiovasc. Surg. 2022, 164, 1532–1541.e2. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, D.J.; Puskas, J.D.; Alexander, J.H.; Chang, H.L.; Gammie, J.S.; Marks, M.E.; Iribarne, A.; Vengrenyuk, Y.; Raymond, S.; Taylor, B.S.; et al. External Support for Saphenous Vein Grafts in Coronary Artery Bypass Surgery: A Randomized Clinical Trial. JAMA Cardiol. 2022, 7, 808–816. [Google Scholar] [CrossRef] [PubMed]
- Taggart, D.P.; Ben Gal, Y.; Lees, B.; Patel, N.; Webb, C.; Rehman, S.M.; Desouza, A.; Yadav, R.; De Robertis, F.; Dalby, M.; et al. A Randomized Trial of External Stenting for Saphenous Vein Grafts in Coronary Artery Bypass Grafting. Ann. Thorac. Surg. 2015, 99, 2039–2045. [Google Scholar] [CrossRef]
- Taggart, D.P.; Webb, C.M.; Desouza, A.; Yadav, R.; Channon, K.M.; De Robertis, F.; Di Mario, C. Long-term performance of an external stent for saphenous vein grafts: The VEST IV trial. J. Cardiothorac. Surg. 2018, 13, 117. [Google Scholar] [CrossRef] [PubMed]
- Taggart, D.P.; Amin, S.; Djordjevic, J.; Oikonomou, E.K.; Thomas, S.; Kampoli, A.-M.; Sabharwal, N.; Antoniades, C.; Krasopoulos, G. A prospective study of external stenting of saphenous vein grafts to the right coronary artery: The VEST II study. Eur. J. Cardio-Thorac. Surg. Off. J. Eur. Assoc. Cardio-Thorac. Surg. 2017, 51, 952–958. [Google Scholar] [CrossRef] [PubMed]
- Raza, S.; Chang, C.; Deo, S.V.; Sabik, J.F. Current role of saphenous vein graft in coronary artery bypass grafting. Indian J. Thorac. Cardiovasc. Surg. 2018, 34 (Suppl. S3), 245–250. [Google Scholar] [CrossRef] [PubMed]
- Gemelli, M.; Gallo, M.; Addonizio, M.; Pahwa, S.; Van den Eynde, J.; Trivedi, J.; Slaughter, M.S.; Gerosa, G. Venous External Support in Coronary Artery Bypass Surgery: A Systematic Review and Meta-Analysis. Curr. Probl. Cardiol. 2023, 48, 101687. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, D.J.; Chang, H.L.; Mack, M.J.; Voisine, P.; Gammie, J.S.; Marks, M.E.; Iribarne, A.; Vengrenyuk, Y.; Raymond, S.; Taylor, B.S.; et al. Intimal hyperplasia, saphenous vein graft disease, and clinical outcomes: Insights from the CTSN VEST randomized trial. J. Thorac. Cardiovasc. Surg. 2022. [Google Scholar] [CrossRef] [PubMed]
- Lee, G.S.; Fremes, S.E.; Tam, D.Y. Commentary: Can the Venous Graft External SupporT (VEST) trials bypass surrogate outcomes? J. Thorac. Cardiovasc. Surg. 2022. [Google Scholar] [CrossRef] [PubMed]
- Tian, M.; Wang, X.; Sun, H.; Feng, W.; Song, Y.; Lu, F.; Wang, L.; Wang, Y.; Xu, B.; Wang, H.; et al. No-Touch Versus Conventional Vein Harvesting Techniques at 12 Months After Coronary Artery Bypass Grafting Surgery: Multicenter Randomized, Controlled Trial. Circulation 2021, 144, 1120–1129. [Google Scholar] [CrossRef] [PubMed]
- Cancelli, G.; Audisio, K.; Chadow, D.; Soletti, G.J.; Gaudino, M. The evidence for radial artery grafting: When and when not? JTCVS Tech. 2021, 10, 114–119. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Soletti, G.J.; Dimagli, A.; Harik, L.; Cancelli, G.; Perezgrovas-Olaria, R.; Alzghari, T.; Dell’Aquila, M.; Leith, J.; Castagnini, S.; Lau, C.; et al. External Stenting for Saphenous Vein Grafts in Coronary Surgery: A Systematic Review and Meta-Analysis. J. Clin. Med. 2023, 12, 7395. https://doi.org/10.3390/jcm12237395
Soletti GJ, Dimagli A, Harik L, Cancelli G, Perezgrovas-Olaria R, Alzghari T, Dell’Aquila M, Leith J, Castagnini S, Lau C, et al. External Stenting for Saphenous Vein Grafts in Coronary Surgery: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2023; 12(23):7395. https://doi.org/10.3390/jcm12237395
Chicago/Turabian StyleSoletti, Giovanni Jr, Arnaldo Dimagli, Lamia Harik, Gianmarco Cancelli, Roberto Perezgrovas-Olaria, Talal Alzghari, Michele Dell’Aquila, Jordan Leith, Sabrina Castagnini, Christopher Lau, and et al. 2023. "External Stenting for Saphenous Vein Grafts in Coronary Surgery: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 12, no. 23: 7395. https://doi.org/10.3390/jcm12237395
APA StyleSoletti, G. J., Dimagli, A., Harik, L., Cancelli, G., Perezgrovas-Olaria, R., Alzghari, T., Dell’Aquila, M., Leith, J., Castagnini, S., Lau, C., Girardi, L. N., & Gaudino, M. (2023). External Stenting for Saphenous Vein Grafts in Coronary Surgery: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 12(23), 7395. https://doi.org/10.3390/jcm12237395







