Articular Cartilage Reconstruction with Hyaluronate-Based Scaffold Significantly Decreases Pain and Improves Patient’s Functioning
Abstract
:1. Introduction
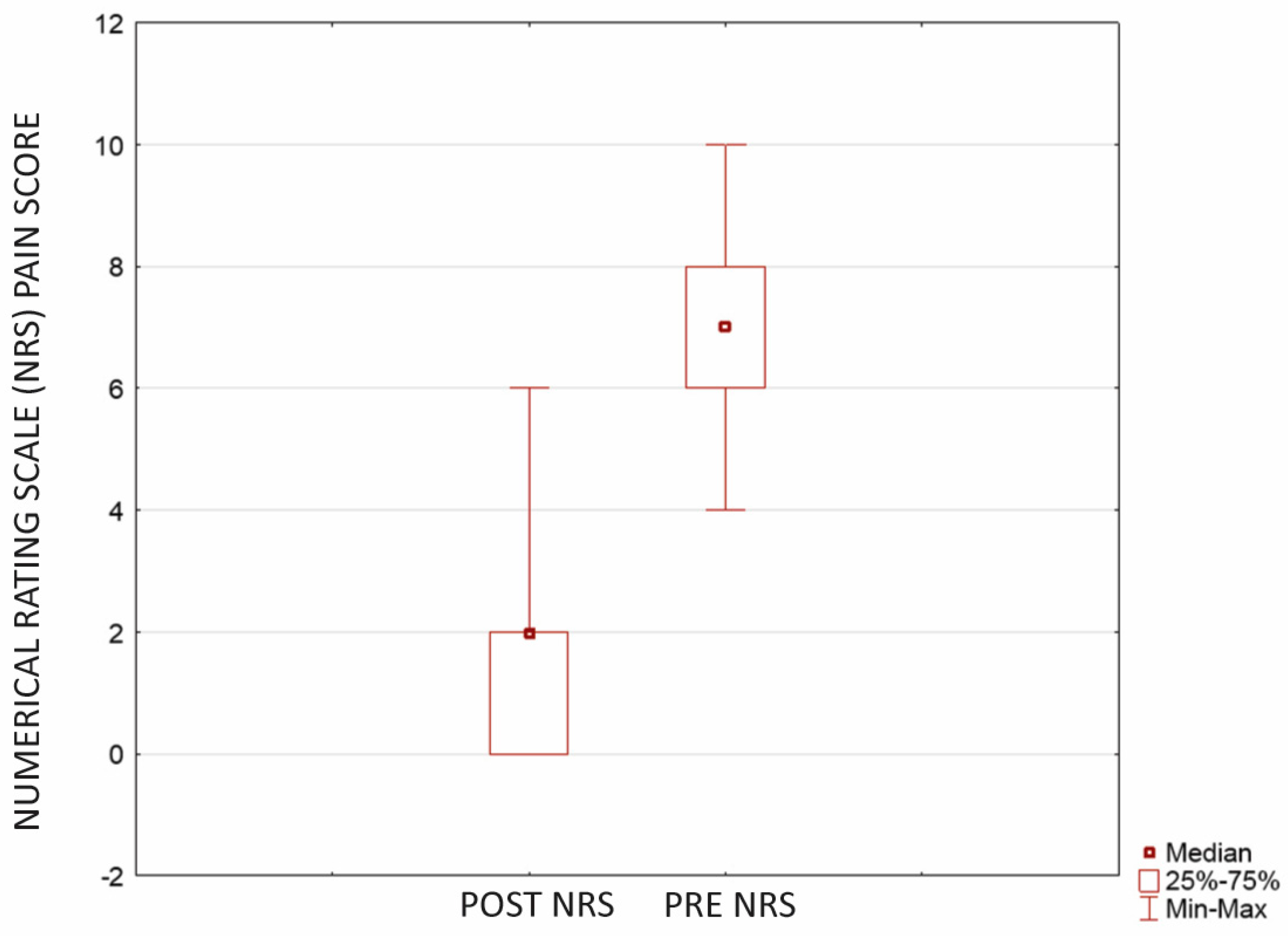
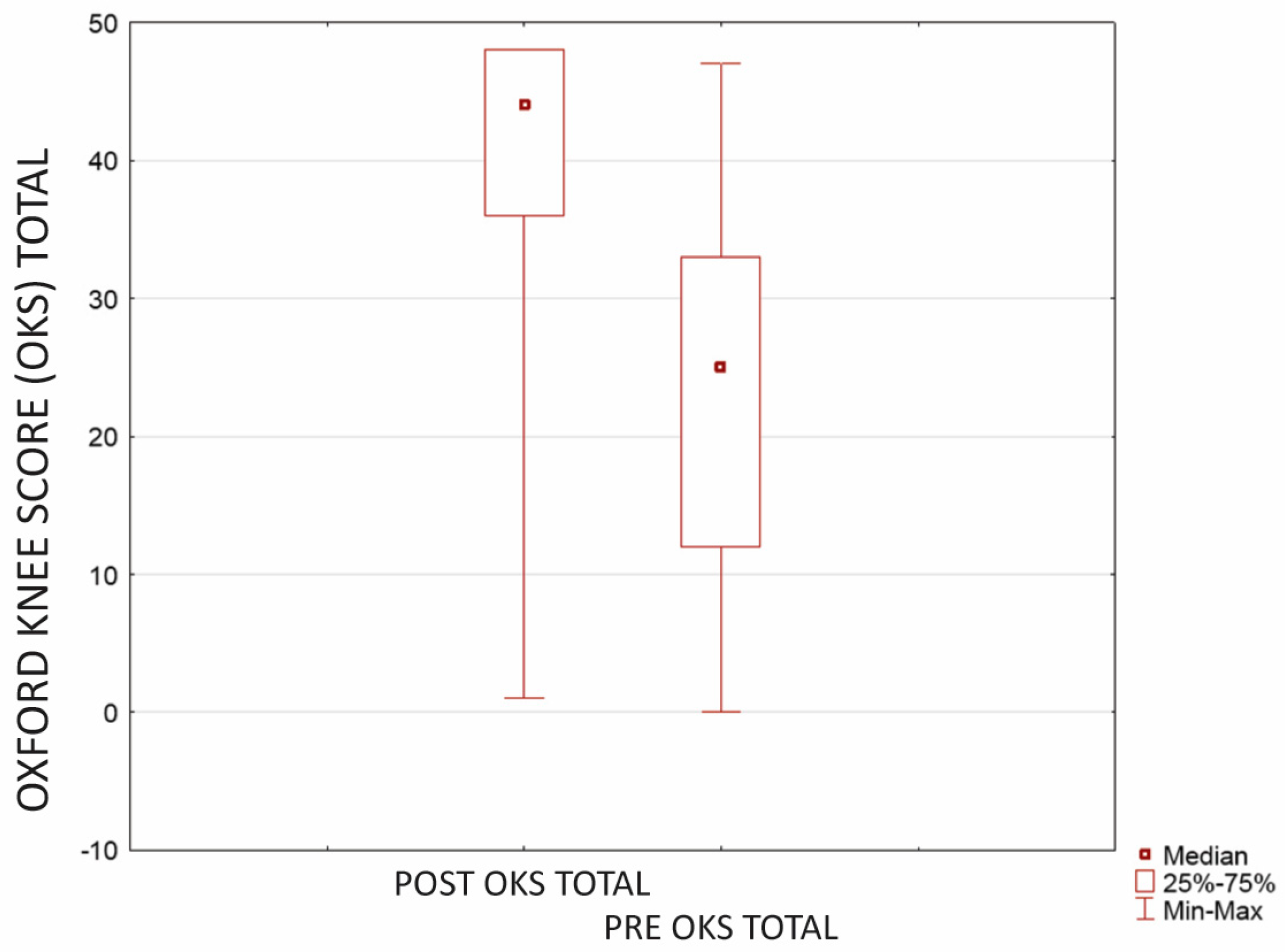
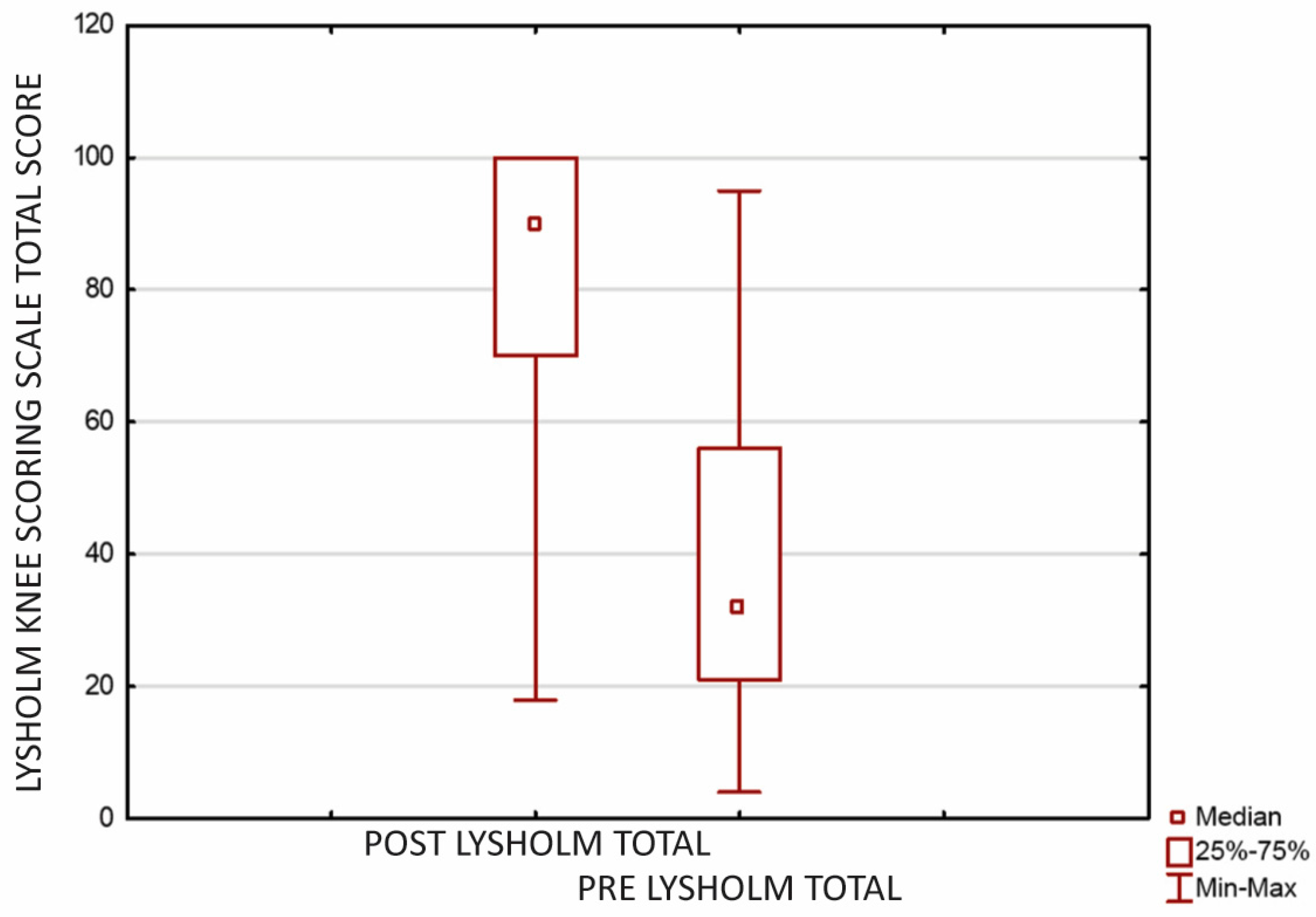
2. Results
3. Discussion
4. Materials and Methods
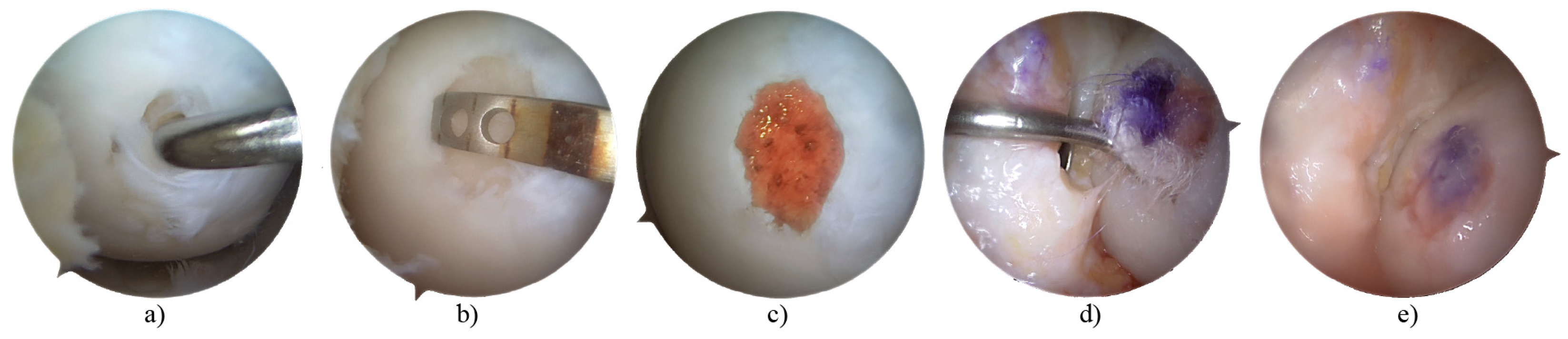
4.1. Procedure
4.2. Assessments
4.3. Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zikria, B.; Rinaldi, J.; Guermazi, A.; Haj-Mirzaian, A.; Pishgar, F.; Roemer, F.W.; Hakky, M.; Sereni, C.; Demehri, S. Lateral patellar tilt and its longitudinal association with patellofemoral osteoarthritis-related structural damage: Analysis of the osteoarthritis initiative data. Knee 2020, 27, 1971–1979. [Google Scholar] [CrossRef] [PubMed]
- Ayariga, J.A.; Huang, H.; Dean, D. Decellularized Avian Cartilage, a Promising Alternative for Human Cartilage Tissue Regeneration. Materials 2022, 15, 1974. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Wang, R.; Xiang, S.; Gu, Y.; Xu, T.; Jin, H.; Gu, X.; Tong, P.; Zhan, H.; Lv, S. Assessment of the effectiveness and satisfaction of platelet-rich plasma compared with hyaluronic acid in knee osteoarthritis at minimum 7-year follow-up: A post hoc analysis of a randomized controlled trial. Front. Bioeng. Biotechnol. 2022, 10, 1062371. [Google Scholar] [CrossRef] [PubMed]
- Kraeutler, M.J.; Aliberti, G.M.; Scillia, A.J.; McCarty, E.C.; Mulcahey, M.K. Microfracture Versus Drilling of Articular Cartilage Defects: A Systematic Review of the Basic Science Evidence. Orthop. J. Sport. Med. 2020, 8, 2325967120945313. [Google Scholar] [CrossRef]
- Gryglewicz, J.B.; Łukasz Dragan, S.A. Ortopedii Traumatologii Narządu Ruchu dla Dorosłych Dzieci, K. Review of Surgical Management Techniques for Osteochondral Lesions. Ortop. Traumatol. Rehabil. 2023, 25, 157–163. [Google Scholar] [CrossRef]
- Kuyucu, E.; Çabuk, H.; Güler, Y.; Çabuk, F.; Kiliç, E.; Bülbül, M. Can Intra-articular 1α, 25-Dihydroxyvitamin D3 Administration Be Therapeutical in Joint Cartilage Damage? Může intraartikulárně aplikovaný 1α, 25-dihydroxyvitamin D3 působit terapeuticky u poškození kloubní chrupavky? Acta Chir. Orthop. Traumatol. Cech. 2020, 87, 90–94. [Google Scholar] [CrossRef]
- Muthuri, S.G.; McWilliams, D.F.; Doherty, M.; Zhang, W. History of knee injuries and knee osteoarthritis: A meta-analysis of observational studies. Osteoarthr. Cartil. 2011, 19, 1286–1293. [Google Scholar] [CrossRef]
- Horga, L.M.; Hirschmann, A.C.; Henckel, J.; Fotiadou, A.; Di Laura, A.; Torlasco, C.; D’Silva, A.; Sharma, S.; Moon, J.C.; Hart, A.J. Prevalence of abnormal findings in 230 knees of asymptomatic adults using 3.0 T MRI. Skelet. Radiol. 2020, 49, 1099–1107. [Google Scholar] [CrossRef]
- Laprade, R.F.; Burnett, Q.M.; Veenstra, M.A.; Hodgman, C.G. The Prevalence of Abnormal Magnetic Resonance Imaging Findings in Asymptomatic Knees. Am. J. Sports Med. 1994, 22, 739–745. [Google Scholar] [CrossRef]
- Peers, S.C.; Maerz, T.; Baker, E.A.; Shetty, A.; Xia, Y.; Puwal, S.; Marcantonio, D.; Keyes, D.; Guettler, J. T1ρ magnetic resonance imaging for detection of early cartilage changes in knees of asymptomatic collegiate female impact and nonimpact athletes. Clin. J. Sport Med. 2014, 24, 218–225. [Google Scholar] [CrossRef]
- Stahl, R.; Luke, A.; Ma, C.B.; Krug, R.; Steinbach, L.; Majumdar, S.; Link, T.M. Prevalence of pathologic findings in asymptomatic knees of marathon runners before and after a competition in comparison with physically active subjects—A 3.0 T magnetic resonance imaging study. Skelet. Radiol. 2008, 37, 627–638. [Google Scholar] [CrossRef]
- Culvenor, A.G.; Øiestad, B.E.; Hart, H.F.; Stefanik, J.J.; Guermazi, A.; Crossley, K.M. Prevalence of knee osteoarthritis features on magnetic resonance imaging in asymptomatic uninjured adults: A systematic review and meta-analysis. Br. J. Sports Med. 2019, 53, 1268–1278. [Google Scholar] [CrossRef] [PubMed]
- Widuchowski, W.; Widuchowski, J.; Trzaska, T. Articular cartilage defects: Study of 25,124 knee arthroscopies. Knee 2007, 14, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Flanigan, D.C.; Harris, J.D.; Trinh, T.Q.; Siston, R.A.; Brophy, R.H.; Flanigan, D.C.; Harris, J.D.; Trinh, T.Q.; Siston, R.A.; Brophy, R.H. Prevalence of Chondral Defects in Athletes’ Knees: A Systematic Review. Med. Sci. Sport. Exerc. 2010, 42, 1795–1801. [Google Scholar] [CrossRef]
- Davies-Tuck, M.L.; Wluka, A.E.; Wang, Y.; Teichtahl, A.J.; Jones, G.; Ding, C.; Cicuttini, F.M. The natural history of cartilage defects in people with knee osteoarthritis. Osteoarthr. Cartil. 2008, 16, 337–342. [Google Scholar] [CrossRef]
- Wluka, A.E.; Ding, C.; Jones, G.; Cicuttini, F.M. The clinical correlates of articular cartilage defects in symptomatic knee osteoarthritis: A prospective study. Rheumatology 2005, 44, 1311–1316. [Google Scholar] [CrossRef] [PubMed]
- Houck, D.A.; Kraeutler, M.J.; Belk, J.W.; Frank, R.M.; Mccarty, E.C.; Bravman, J.T. Do Focal Chondral Defects of the Knee Increase the Risk for Progression to Osteoarthritis? A Review of the Literature. Orthop. J. Sports Med. 2018, 6, 2325967118801931. [Google Scholar] [CrossRef]
- Serlin, R.C.; Mendoza, T.R.; Nakamura, Y.; Edwards, K.R.; Cleeland, C.S. When is cancer pain mild, moderate or severe? Grading pain severity by its interference with function. Pain 1995, 61, 277–284. [Google Scholar] [CrossRef]
- Boonstra, A.M.; Preuper, H.R.S.; Balk, G.A.; Stewart, R.E. Cut-off points for mild, moderate, and severe pain on the visual analogue scale for pain in patients with chronic musculoskeletal pain. Pain 2014, 155, 2545–2550. [Google Scholar] [CrossRef]
- Mithoefer, K.; Hambly, K.; Logerstedt, D.; Ricci, M.; Silvers, H.; Villa, S. Della Current concepts for rehabilitation and return to sport after knee articular cartilage repair in the athlete. J. Orthop. Sports Phys. Ther. 2012, 42, 254–273. [Google Scholar] [CrossRef]
- Szychlinska, M.A.; Imbesi, R.; Castrogiovanni, P.; Guglielmino, C.; Ravalli, S.; Rosa, M.D.; Musumeci, G. Assessment of Vitamin D Supplementation on Articular Cartilage Morphology in a Young Healthy Sedentary Rat Model. Nutrients 2019, 11, 1260. [Google Scholar] [CrossRef]
- Pascual-Garrido, C.; Angeline, M.E.; Ma, R.; Chahla, J.; Voigt, C.; Deng, X.H.; Nguyen, J.; Warren, R.F.; Rodeo, S.A. Low Levels of Vitamin D have a Deleterious Effect on the Articular Cartilage in a Rat Model. HSS J. 2016, 12, 150–157. [Google Scholar] [CrossRef]
- Li, S.; Niu, G.; Dong, X.N.; Liu, Z.; Song, C.; Leng, H. Vitamin D inhibits activities of metalloproteinase-9/-13 in articular cartilage in vivo and in vitro. J. Nutr. Sci. Vitaminol. 2019, 65, 107–112. [Google Scholar] [CrossRef]
- van der Wielen, R.P.J.; de Groot, L.C.P.G.M.; van Staveren, W.A.; Löwik, M.R.H.; van den Berg, H.; Haller, J.; Moreiras, O. Serum vitamin D concentrations among elderly people in Europe. Lancet 1995, 346, 207–210. [Google Scholar] [CrossRef] [PubMed]
- Holick, M.F. Vitamin D deficiency. N. Engl. J. Med. 2007, 357, 266–281. [Google Scholar] [CrossRef] [PubMed]
- Malas, F.Ü.; Kara, M.; Aktekin, L.; Ersöz, M.; Özçakar, L. Does vitamin D affect femoral cartilage thickness? An ultrasonographic study. Clin. Rheumatol. 2014, 33, 1331–1334. [Google Scholar] [CrossRef] [PubMed]
- Joseph, G.B.; McCulloch, C.E.; Nevitt, M.C.; Neumann, J.; Lynch, J.A.; Lane, N.E.; Link, T.M. Associations Between Vitamins C and D Intake and Cartilage Composition and Knee Joint Morphology Over 4 Years: Data From the Osteoarthritis Initiative. Arthritis Care Res. 2020, 72, 1239–1247. [Google Scholar] [CrossRef]
| Variable 1 | Value 1 | No. (%) | Value 2 | No. (%) | Value 3 | No. (%) | Value 4 | No. (%) | Value 5 | No. (%) |
|---|---|---|---|---|---|---|---|---|---|---|
| Vitamin D supplementation | Yes | 19 (65.52%) | No | 10 (34.48%) | ||||||
| Supplemented dose | 0–1000 u/d | 1 (3.45%) | 1001–2000 u/d | 6 (20.69%) | 2001–4000 u/d | 8 (27.59%) | 4001–10,000 u/d | 3 (10.34%) | >10,000 u/d | 1 (3.45%) |
| Supplementation period after surgery | 1 (3.45%) | 2 (6.90%) | 1–3 months | 5 (17.24%) | 3–6 months | 5 (17.24%) | 6–12 months | 0 (0.00%) | >12 months | 7 (24.14%) |
| Relation with a meal | on an empty stomach | 4 (13.79%) | before a meal but not on an empty stomach | 0 (0.00%) | during a meal | 2 (6.90%) | up to 30 min after a meal | 7 (24.14%) | independent from a meal | 6 (20.69%) |
| Elimination diet | vegetarian | 4 (13.79%) | vegan | 0 (0.00%) | gluten-free | 2 (6.90%) | lactose-free | 0 (0.00%) | other | 0 (0.00%) |
| Variable 1 | Value 1 | No. (%) | Value 2 | No. (%) | Value 3 | No. (%) | Value 4 | No. (%) | Value 5 | No. (%) |
|---|---|---|---|---|---|---|---|---|---|---|
| Rehabilitation up to 12 months after surgery | Yes | 29 (100%) | No | 0 (00.00%) | ||||||
| Gap between surgery and first rehabilitation | <2 weeks | 7 (24.14%) | 2–4 weeks | 10 (34.48%) | 4–12 weeks | 10 (34.48%) | 12–24 weeks | 1 (3.45%) | >24 weeks | 1 (3.45%) |
| Duration of rehabilitation | <1 month | 5 (17.24%) | 1–3 months | 9 (31.03%) | 3–6 months | 8 (27.59%) | 6–12 months | 3 (10.34%) | >12 months | 4 (13.79%) |
| Frequency of sessions (per week) | less that once | 0 (00.00%) | once | 7 (24.14%) | 2 times | 8 (27.59%) | 3 times | 11 (37.93%) | >3 times | 3 (10.34%) |
| Types of applied treatments | physical therapy | 17 (58.62%) | kinesiotherapy | 12 (41.38%) | CPM | 3 (10.34%) | manual therapy | 17 (58.62%) | other | 2 (6.90%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gryglewicz, J.; Chaszczewska-Markowska, M.; Dorochowicz, M.; Drożdż, J.; Dragan, S.Ł. Articular Cartilage Reconstruction with Hyaluronate-Based Scaffold Significantly Decreases Pain and Improves Patient’s Functioning. J. Clin. Med. 2023, 12, 7342. https://doi.org/10.3390/jcm12237342
Gryglewicz J, Chaszczewska-Markowska M, Dorochowicz M, Drożdż J, Dragan SŁ. Articular Cartilage Reconstruction with Hyaluronate-Based Scaffold Significantly Decreases Pain and Improves Patient’s Functioning. Journal of Clinical Medicine. 2023; 12(23):7342. https://doi.org/10.3390/jcm12237342
Chicago/Turabian StyleGryglewicz, Jarosław, Monika Chaszczewska-Markowska, Mateusz Dorochowicz, Jerzy Drożdż, and Szymon Łukasz Dragan. 2023. "Articular Cartilage Reconstruction with Hyaluronate-Based Scaffold Significantly Decreases Pain and Improves Patient’s Functioning" Journal of Clinical Medicine 12, no. 23: 7342. https://doi.org/10.3390/jcm12237342
APA StyleGryglewicz, J., Chaszczewska-Markowska, M., Dorochowicz, M., Drożdż, J., & Dragan, S. Ł. (2023). Articular Cartilage Reconstruction with Hyaluronate-Based Scaffold Significantly Decreases Pain and Improves Patient’s Functioning. Journal of Clinical Medicine, 12(23), 7342. https://doi.org/10.3390/jcm12237342






