Endo Belly: What Is It and Why Does It Happen?—A Narrative Review
Abstract
1. Introduction
2. Endometriosis and Irritable Bowel Syndrome
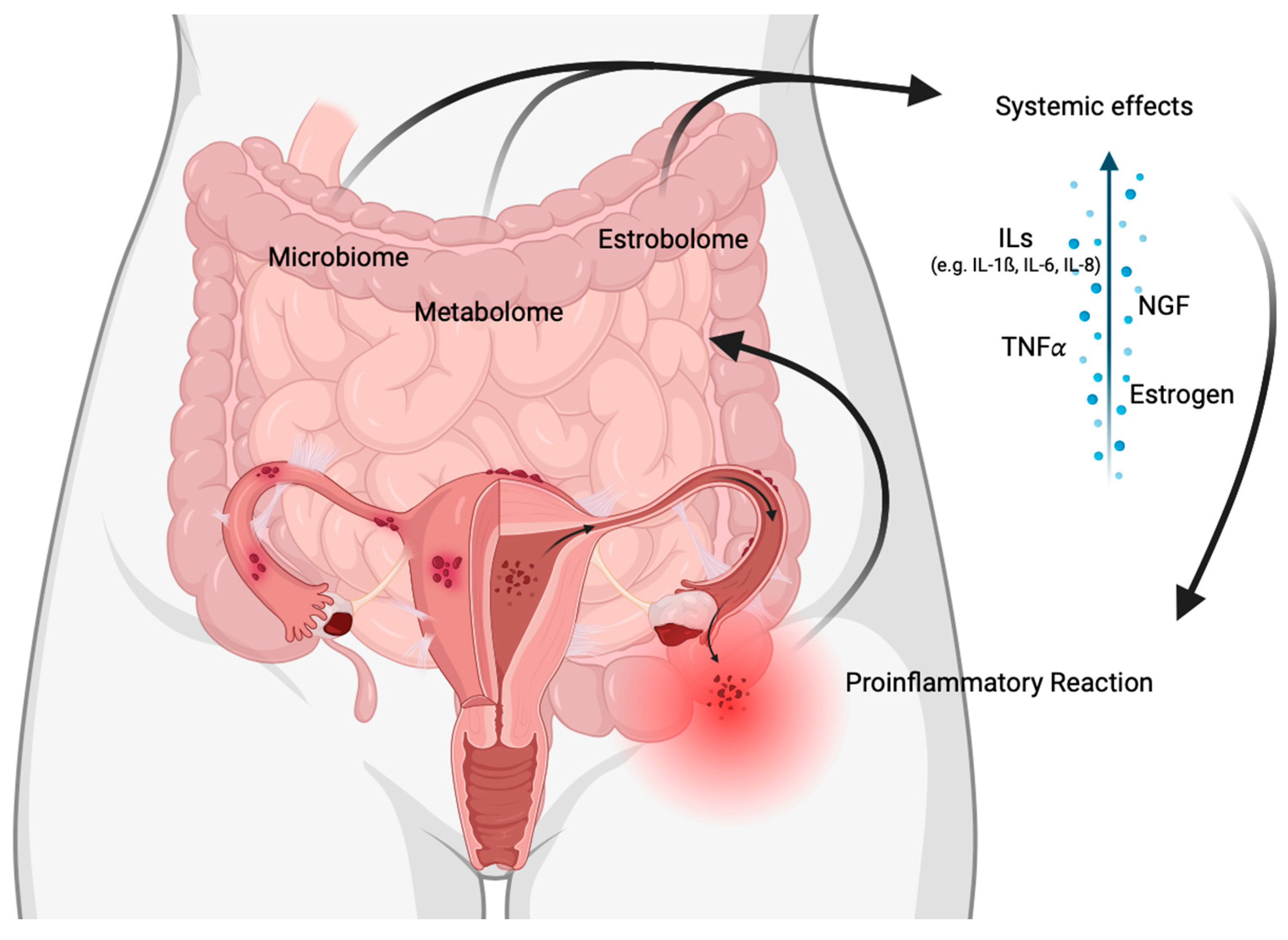
- (a)
- Underlying condition:
- (b)
- Triggers and patterns:
- (c)
- Diagnostic criteria:
3. Pathophysiology of Endometriosis-Associated Pain
4. Microbiome
5. Intestinal Activity Hormonal Regulated
6. Enteric Nervous System
7. Nutrition
8. Strengths
9. Limitations
10. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Velho, R.V.; Taube, E.; Sehouli, J.; Mechsner, S. Neurogenic Inflammation in the Context of Endometriosis—What Do We Know? Int. J. Mol. Sci. 2021, 22, 13102. [Google Scholar] [CrossRef] [PubMed]
- Duckelmann, A.M.; Taube, E.; Abesadze, E.; Chiantera, V.; Sehouli, J.; Mechsner, S. When and how should peritoneal endometriosis be operated on in order to improve fertility rates and symptoms? The experience and outcomes of nearly 100 cases. Arch. Gynecol. Obstet. 2021, 304, 143–155. [Google Scholar] [CrossRef] [PubMed]
- Velho, R.V.; Halben, N.; Chekerov, R.; Keye, J.; Plendl, J.; Sehouli, J.; Mechsner, S. Functional changes of immune cells: Signal of immune tolerance of the ectopic lesions in endometriosis? Reprod. BioMed. Online 2021, 43, 319–328. [Google Scholar] [CrossRef] [PubMed]
- Laganà, A.S.; Naem, A. The pathogenesis of endometriosis: Are endometrial stem/progenitor cells involved. In Stem Cells in Reproductive Tissues and Organs: From Fertility to Cancer; Springer Nature: Cham, Switzerland, 2022; pp. 193–216. [Google Scholar]
- Greene, R.; Stratton, P.; Cleary, S.D.; Ballweg, M.L.; Sinaii, N. Diagnostic experience among 4,334 women reporting surgically diagnosed endometriosis. Fertil. Steril. 2009, 91, 32–39. [Google Scholar] [CrossRef]
- Naem, A.; Andrikos, D.; Schimmack, S.; Krentel, H. The incidental diagnosis of a rectal neuroendocrine tumor after a segmental rectal resection for bowel endometriosis. Asian J. Surg. 2023. ahead of print. [Google Scholar] [CrossRef]
- Mechsner, S. Endometriosis, an Ongoing Pain-Step-by-Step Treatment. J. Clin. Med. 2022, 11, 467. [Google Scholar] [CrossRef]
- Wojcik, M.; Gozdziewicz, T.; Hudakova, Z.; Siatkowski, I. Endometriosis and the Temporomandibular Joint-Preliminary Observations. J. Clin. Med. 2023, 12, 2862. [Google Scholar] [CrossRef]
- Taylor, H.S. Reimagining Endometriosis. Med 2021, 2, 481–485. [Google Scholar] [CrossRef]
- Salmeri, N.; Sinagra, E.; Dolci, C.; Buzzaccarini, G.; Sozzi, G.; Sutera, M.; Candiani, M.; Ungaro, F.; Massimino, L.; Danese, S.; et al. Microbiota in Irritable Bowel Syndrome and Endometriosis: Birds of a Feather Flock Together—A Review. Microorganisms 2023, 11, 2089. [Google Scholar] [CrossRef]
- Shigesi, N.; Kvaskoff, M.; Kirtley, S.; Feng, Q.; Fang, H.; Knight, J.C.; Missmer, S.A.; Rahmioglu, N.; Zondervan, K.T.; Becker, C.M. The association between endometriosis and autoimmune diseases: A systematic review and meta-analysis. Hum. Reprod. Update 2019, 25, 486–503. [Google Scholar] [CrossRef]
- Matalliotakis, I.; Cakmak, H.; Matalliotakis, M.; Kappou, D.; Arici, A. High rate of allergies among women with endometriosis. J. Obstet. Gynaecol. 2012, 32, 291–293. [Google Scholar] [CrossRef] [PubMed]
- Fuentes, A.; Escalona, J.; Cespedes, P.; Espinoza, A.; Johnson, M.C. Prevalence of endometriosis in 287 women undergoing surgical sterilization in Santiago Chile. Rev. Med. Chil. 2014, 142, 16–19. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Shafrir, A.L.; Farland, L.V.; Shah, D.K.; Harris, H.R.; Kvaskoff, M.; Zondervan, K.; Missmer, S.A. Risk for and consequences of endometriosis: A critical epidemiologic review. Best Pract. Res. Clin. Obstet. Gynaecol. 2018, 51, 1–15. [Google Scholar] [CrossRef]
- Issa, B.; Onon, T.S.; Agrawal, A.; Shekhar, C.; Morris, J.; Hamdy, S.; Whorwell, P.J. Visceral hypersensitivity in endometriosis: A new target for treatment? Gut 2012, 61, 367–372. [Google Scholar] [CrossRef] [PubMed]
- Ek, M.; Roth, B.; Ekstrom, P.; Valentin, L.; Bengtsson, M.; Ohlsson, B. Gastrointestinal symptoms among endometriosis patients—A case-cohort study. BMC Womens Health 2015, 15, 59. [Google Scholar] [CrossRef]
- Chiaffarino, F.; Cipriani, S.; Ricci, E.; Roncella, E.; Mauri, P.A.; Parazzini, F.; Vercellini, P. Endometriosis and inflammatory bowel disease: A systematic review of the literature. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 252, 246–251. [Google Scholar] [CrossRef]
- Nabi, M.Y.; Nauhria, S.; Reel, M.; Londono, S.; Vasireddi, A.; Elmiry, M.; Ramdass, P.V. Endometriosis and irritable bowel syndrome: A systematic review and meta-analyses. Front. Med. 2022, 9, 914356. [Google Scholar] [CrossRef]
- Willer, D.; Peters, G.; Tesch, K.; Maass, N.; Alkatout, I. Endometriose–mehr als „nur “Dysmenorrhö! Die Gynäkologie 2023, 56, 445–453. [Google Scholar] [CrossRef]
- Mills, J.; Shu, C.; Misajon, R.; Rush-Privitera, G. ‘My body is out to wreck everything I have’: A qualitative study of how women with endometriosis feel about their bodies. Psychol. Health 2023, 1–19. [Google Scholar] [CrossRef]
- Bouaziz, J.; Bar On, A.; Seidman, D.S.; Soriano, D. The Clinical Significance of Endocannabinoids in Endometriosis Pain Management. Cannabis Cannabinoid Res. 2017, 2, 72–80. [Google Scholar] [CrossRef]
- Hudelist, G.; Fritzer, N.; Thomas, A.; Niehues, C.; Oppelt, P.; Haas, D.; Tammaa, A.; Salzer, H. Diagnostic delay for endometriosis in Austria and Germany: Causes and possible consequences. Hum. Reprod. 2012, 27, 3412–3416. [Google Scholar] [CrossRef] [PubMed]
- Gruber, T.M.; Mechsner, S. Pathogenesis of Endometriosis: The Origin of Pain and Subfertility. Cells 2021, 10, 1381. [Google Scholar] [CrossRef] [PubMed]
- Muallem, J.; Velho, R.V.; Netzl, J.; Sehouli, J.; Mechsner, S. Pelvic floor hypertension: Possible factors for pelvic floor tenderness in endometriosis patients—A pilot study. Arch. Gynecol. Obstet. 2023, 308, 1803–1809. [Google Scholar] [CrossRef] [PubMed]
- Arnold, J.; Vercellino, G.F.; Chiantera, V.; Schneider, A.; Mechsner, S.; Barcena de Arellano, M.L. Neuroimmunomodulatory alterations in non-lesional peritoneum close to peritoneal endometriosis. Neuroimmunomodulation 2013, 20, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Ballweg, M.L. Impact of endometriosis on women’s health: Comparative historical data show that the earlier the onset, the more severe the disease. Best Pract. Res. Clin. Obstet. Gynaecol. 2004, 18, 201–218. [Google Scholar] [CrossRef]
- Hoffman, D. Central and peripheral pain generators in women with chronic pelvic pain: Patient centered assessment and treatment. Curr. Rheumatol. Rev. 2015, 11, 146–166. [Google Scholar] [CrossRef]
- Hauser, W. Endometriosis and chronic overlapping pain conditions. Schmerz 2021, 35, 179–182. [Google Scholar]
- Ghosh, N.; Kesh, K.; Ramakrishnan, S.; Roy, S. Opioid Use in Murine Model Results in Severe Gastric Pathology that May Be Attenuated by Proton Pump Inhibition. Am. J. Pathol. 2022, 192, 1136–1150. [Google Scholar] [CrossRef]
- Kalfas, M.; Chisari, C.; Windgassen, S. Psychosocial factors associated with pain and health-related quality of life in Endometriosis: A systematic review. Eur. J. Pain 2022, 26, 1827–1848. [Google Scholar] [CrossRef]
- Cani, P.D. Human gut microbiome: Hopes, threats and promises. Gut 2018, 67, 1716–1725. [Google Scholar] [CrossRef]
- Blaser, M.J. The microbiome revolution. J. Clin. Investig. 2014, 124, 4162–4165. [Google Scholar] [CrossRef] [PubMed]
- Leonardi, M.; Hicks, C.; El-Assaad, F.; El-Omar, E.; Condous, G. Endometriosis and the microbiome: A systematic review. BJOG 2020, 127, 239–249. [Google Scholar] [CrossRef] [PubMed]
- Afzaal, M.; Saeed, F.; Shah, Y.A.; Hussain, M.; Rabail, R.; Socol, C.T.; Hassoun, A.; Pateiro, M.; Lorenzo, J.M.; Rusu, A.V.; et al. Human gut microbiota in health and disease: Unveiling the relationship. Front. Microbiol. 2022, 13, 999001. [Google Scholar] [CrossRef] [PubMed]
- Elkafas, H.; Walls, M.; Al-Hendy, A.; Ismail, N. Gut and genital tract microbiomes: Dysbiosis and link to gynecological disorders. Front. Cell. Infect. Microbiol. 2022, 12, 1059825. [Google Scholar] [CrossRef]
- Bailey, M.T.; Coe, C.L. Endometriosis is associated with an altered profile of intestinal microflora in female rhesus monkeys. Hum. Reprod. 2002, 17, 1704–1708. [Google Scholar] [CrossRef] [PubMed]
- Ata, B.; Yildiz, S.; Turkgeldi, E.; Brocal, V.P.; Dinleyici, E.C.; Moya, A.; Urman, B. The Endobiota Study: Comparison of Vaginal, Cervical and Gut Microbiota Between Women with Stage 3/4 Endometriosis and Healthy Controls. Sci. Rep. 2019, 9, 2204. [Google Scholar] [CrossRef]
- Shan, J.; Ni, Z.; Cheng, W.; Zhou, L.; Zhai, D.; Sun, S.; Yu, C. Gut microbiota imbalance and its correlations with hormone and inflammatory factors in patients with stage 3/4 endometriosis. Arch. Gynecol. Obstet. 2021, 304, 1363–1373. [Google Scholar] [CrossRef]
- Svensson, A.; Brunkwall, L.; Roth, B.; Orho-Melander, M.; Ohlsson, B. Associations Between Endometriosis and Gut Microbiota. Reprod. Sci. 2021, 28, 2367–2377. [Google Scholar] [CrossRef]
- Jiang, I.; Yong, P.J.; Allaire, C.; Bedaiwy, M.A. Intricate Connections between the Microbiota and Endometriosis. Int. J. Mol. Sci. 2021, 22, 5644. [Google Scholar] [CrossRef]
- Sourial, S.; Tempest, N.; Hapangama, D.K. Theories on the pathogenesis of endometriosis. Int. J. Reprod. Med. 2014, 2014, 179515. [Google Scholar] [CrossRef]
- Laschke, M.W.; Menger, M.D. The gut microbiota: A puppet master in the pathogenesis of endometriosis? Am. J. Obstet. Gynecol. 2016, 215, 68.e61–64. [Google Scholar] [CrossRef] [PubMed]
- Zizolfi, B.; Foreste, V.; Gallo, A.; Martone, S.; Giampaolino, P.; Di Spiezio Sardo, A. Endometriosis and dysbiosis: State of art. Front. Endocrinol. 2023, 14, 1140774. [Google Scholar] [CrossRef] [PubMed]
- Salliss, M.E.; Farland, L.V.; Mahnert, N.D.; Herbst-Kralovetz, M.M. The role of gut and genital microbiota and the estrobolome in endometriosis, infertility and chronic pelvic pain. Hum. Reprod. Update 2021, 28, 92–131. [Google Scholar] [CrossRef] [PubMed]
- Uchida, M.; Kobayashi, O. Effects of Lactobacillus gasseri OLL2809 on the induced endometriosis in rats. Biosci. Biotechnol. Biochem. 2013, 77, 1879–1881. [Google Scholar] [CrossRef]
- Itoh, H.; Sashihara, T.; Hosono, A.; Kaminogawa, S.; Uchida, M. Lactobacillus gasseri OLL2809 inhibits development of ectopic endometrial cell in peritoneal cavity via activation of NK cells in a murine endometriosis model. Cytotechnology 2011, 63, 205–210. [Google Scholar] [CrossRef]
- Khan, K.N.; Kitajima, M.; Hiraki, K.; Fujishita, A.; Sekine, I.; Ishimaru, T.; Masuzaki, H. Toll-like receptors in innate immunity: Role of bacterial endotoxin and toll-like receptor 4 in endometrium and endometriosis. Gynecol. Obstet. Investig. 2009, 68, 40–52. [Google Scholar] [CrossRef]
- Oka, P.; Parr, H.; Barberio, B.; Black, C.J.; Savarino, E.V.; Ford, A.C. Global prevalence of irritable bowel syndrome according to Rome III or IV criteria: A systematic review and meta-analysis. Lancet Gastroenterol. Hepatol. 2020, 5, 908–917. [Google Scholar] [CrossRef]
- Chang, L.; Toner, B.B.; Fukudo, S.; Guthrie, E.; Locke, G.R.; Norton, N.J.; Sperber, A.D. Gender, age, society, culture, and the patient’s perspective in the functional gastrointestinal disorders. Gastroenterology 2006, 130, 1435–1446. [Google Scholar] [CrossRef]
- Prochazkova, N.; Falony, G.; Dragsted, L.O.; Licht, T.R.; Raes, J.; Roager, H.M. Advancing human gut microbiota research by considering gut transit time. Gut 2023, 72, 180–191. [Google Scholar] [CrossRef]
- Nandhra, G.K.; Mark, E.B.; Di Tanna, G.L.; Haase, A.M.; Poulsen, J.; Christodoulides, S.; Kung, V.; Klinge, M.W.; Knudsen, K.; Borghammer, P.; et al. Normative values for region-specific colonic and gastrointestinal transit times in 111 healthy volunteers using the 3D-Transit electromagnet tracking system: Influence of age, gender, and body mass index. Neurogastroenterol. Motil. 2020, 32, e13734. [Google Scholar] [CrossRef]
- Mulak, A.; Tache, Y.; Larauche, M. Sex hormones in the modulation of irritable bowel syndrome. World J. Gastroenterol. 2014, 20, 2433–2448. [Google Scholar] [CrossRef] [PubMed]
- Altman, G.; Cain, K.C.; Motzer, S.; Jarrett, M.; Burr, R.; Heitkemper, M. Increased symptoms in female IBS patients with dysmenorrhea and PMS. Gastroenterol. Nurs. 2006, 29, 4–11. [Google Scholar] [CrossRef] [PubMed]
- Kane, S.V.; Sable, K.; Hanauer, S.B. The menstrual cycle and its effect on inflammatory bowel disease and irritable bowel syndrome: A prevalence study. Am. J. Gastroenterol. 1998, 93, 1867–1872. [Google Scholar] [CrossRef] [PubMed]
- Olafsdottir, L.B.; Gudjonsson, H.; Jonsdottir, H.H.; Bjornsson, E.; Thjodleifsson, B. Natural history of irritable bowel syndrome in women and dysmenorrhea: A 10-year follow-up study. Gastroenterol. Res. Pract. 2012, 2012, 534204. [Google Scholar] [CrossRef] [PubMed]
- Pati, G.K.; Kar, C.; Narayan, J.; Uthansingh, K.; Behera, M.; Sahu, M.K.; Mishra, D.; Singh, A. Irritable Bowel Syndrome and the Menstrual Cycle. Cureus 2021, 13, e12692. [Google Scholar] [CrossRef]
- Sharkey, K.A.; Mawe, G.M. The enteric nervous system. Physiol. Rev. 2023, 103, 1487–1564. [Google Scholar] [CrossRef] [PubMed]
- Al-Nasiry, S.; Ambrosino, E.; Schlaepfer, M.; Morre, S.A.; Wieten, L.; Voncken, J.W.; Spinelli, M.; Mueller, M.; Kramer, B.W. The Interplay Between Reproductive Tract Microbiota and Immunological System in Human Reproduction. Front. Immunol. 2020, 11, 378. [Google Scholar] [CrossRef] [PubMed]
- Spencer, N.J.; Hu, H. Enteric nervous system: Sensory transduction, neural circuits and gastrointestinal motility. Nat. Rev. Gastroenterol. Hepatol. 2020, 17, 338–351. [Google Scholar] [CrossRef]
- Million, M.; Larauche, M. Stress, sex, and the enteric nervous system. Neurogastroenterol. Motil. 2016, 28, 1283–1289. [Google Scholar] [CrossRef]
- Ho, J.S.; Nagle, G.T.; Mathias, J.R.; Clench, M.H.; Fan, X.; Kalmaz, G.D.; Sallustio, J.E.; Eaker, E.Y. Presence of gonadotropin-releasing hormone (GnRH) receptor mRNA in rat myenteric plexus cells. Comp. Biochem. Physiol. B Biochem. Mol. Biol. 1996, 113, 817–821. [Google Scholar] [CrossRef]
- Mathias, J.R.; Clench, M.H.; Reeves-Darby, V.G.; Fox, L.M.; Hsu, P.H.; Roberts, P.H.; Smith, L.L.; Stiglich, N.J. Effect of leuprolide acetate in patients with moderate to severe functional bowel disease. Double-blind, placebo-controlled study. Dig. Dis. Sci. 1994, 39, 1155–1162. [Google Scholar] [CrossRef]
- Ferrero, S.; Haas, S.; Remorgida, V.; Camerini, G.; Fulcheri, E.; Ragni, N.; Straub, R.H.; Capellino, S. Loss of sympathetic nerve fibers in intestinal endometriosis. Fertil. Steril. 2010, 94, 2817–2819. [Google Scholar] [CrossRef] [PubMed]
- Mathias, J.R.; Franklin, R.; Quast, D.C.; Fraga, N.; Loftin, C.A.; Yates, L.; Harrison, V. Relation of endometriosis and neuromuscular disease of the gastrointestinal tract: New insights. Fertil. Steril. 1998, 70, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Cryan, J.F.; O’Riordan, K.J.; Cowan, C.S.M.; Sandhu, K.V.; Bastiaanssen, T.F.S.; Boehme, M.; Codagnone, M.G.; Cussotto, S.; Fulling, C.; Golubeva, A.V.; et al. The Microbiota-Gut-Brain Axis. Physiol. Rev. 2019, 99, 1877–2013. [Google Scholar] [CrossRef] [PubMed]
- Barnard, N.D.; Holtz, D.N.; Schmidt, N.; Kolipaka, S.; Hata, E.; Sutton, M.; Znayenko-Miller, T.; Hazen, N.; Cobb, C.; Kahleova, H. Nutrition in the prevention and treatment of endometriosis: A review. Front. Nutr. 2023, 10, 1089891. [Google Scholar] [CrossRef] [PubMed]
- Osmanlioglu, S.; Sanlier, N. The relationship between endometriosis and diet. Hum. Fertil. 2023, 26, 649–664. [Google Scholar] [CrossRef] [PubMed]
- Nap, A.; de Roos, N. Endometriosis and the effects of dietary interventions: What are we looking for? Reprod. Fertil. 2022, 3, C14–C22. [Google Scholar] [CrossRef]
- Armour, M.; Sinclair, J.; Chalmers, K.J.; Smith, C.A. Self-management strategies amongst Australian women with endometriosis: A national online survey. BMC Complement. Altern. Med. 2019, 19, 17. [Google Scholar] [CrossRef]
- Barnard, N.D.; Scialli, A.R.; Hurlock, D.; Bertron, P. Diet and sex-hormone binding globulin, dysmenorrhea, and premenstrual symptoms. Obstet. Gynecol. 2000, 95, 245–250. [Google Scholar]
- Schwartz, N.R.M.; Afeiche, M.C.; Terry, K.L.; Farland, L.V.; Chavarro, J.E.; Missmer, S.A.; Harris, H.R. Glycemic Index, Glycemic Load, Fiber, and Gluten Intake and Risk of Laparoscopically Confirmed Endometriosis in Premenopausal Women. J. Nutr. 2022, 152, 2088–2096. [Google Scholar] [CrossRef]
- Harris, H.R.; Eke, A.C.; Chavarro, J.E.; Missmer, S.A. Fruit and vegetable consumption and risk of endometriosis. Hum. Reprod. 2018, 33, 715–727. [Google Scholar] [CrossRef] [PubMed]
- Parazzini, F.; Chiaffarino, F.; Surace, M.; Chatenoud, L.; Cipriani, S.; Chiantera, V.; Benzi, G.; Fedele, L. Selected food intake and risk of endometriosis. Hum. Reprod. 2004, 19, 1755–1759. [Google Scholar] [CrossRef] [PubMed]
- Missmer, S.A.; Chavarro, J.E.; Malspeis, S.; Bertone-Johnson, E.R.; Hornstein, M.D.; Spiegelman, D.; Barbieri, R.L.; Willett, W.C.; Hankinson, S.E. A prospective study of dietary fat consumption and endometriosis risk. Hum. Reprod. 2010, 25, 1528–1535. [Google Scholar] [CrossRef]
- Nodler, J.L.; DiVasta, A.D.; Vitonis, A.F.; Karevicius, S.; Malsch, M.; Sarda, V.; Fadayomi, A.; Harris, H.R.; Missmer, S.A. Supplementation with vitamin D or omega-3 fatty acids in adolescent girls and young women with endometriosis (SAGE): A double-blind, randomized, placebo-controlled trial. Am. J. Clin. Nutr. 2020, 112, 229–236. [Google Scholar] [CrossRef] [PubMed]
- Signorile, P.G.; Viceconte, R.; Baldi, A. Novel dietary supplement association reduces symptoms in endometriosis patients. J. Cell. Physiol. 2018, 233, 5920–5925. [Google Scholar] [CrossRef] [PubMed]
- Hopeman, M.M.; Riley, J.K.; Frolova, A.I.; Jiang, H.; Jungheim, E.S. Serum Polyunsaturated Fatty Acids and Endometriosis. Reprod. Sci. 2015, 22, 1083–1087. [Google Scholar] [CrossRef]
- Schink, M.; Konturek, P.C.; Herbert, S.L.; Renner, S.P.; Burghaus, S.; Blum, S.; Fasching, P.A.; Neurath, M.F.; Zopf, Y. Different nutrient intake and prevalence of gastrointestinal comorbidities in women with endometriosis. J. Physiol. Pharmacol. 2019, 70, 10–26402. [Google Scholar]
- Mier-Cabrera, J.; Genera-Garcia, M.; De la Jara-Diaz, J.; Perichart-Perera, O.; Vadillo-Ortega, F.; Hernandez-Guerrero, C. Effect of vitamins C and E supplementation on peripheral oxidative stress markers and pregnancy rate in women with endometriosis. Int. J. Gynaecol. Obstet. 2008, 100, 252–256. [Google Scholar] [CrossRef]
- Anastasi, E.; Fuggetta, E.; De Vito, C.; Migliara, G.; Viggiani, V.; Manganaro, L.; Granato, T.; Panici, P.B.; Angeloni, A.; Porpora, M.G. Low levels of 25-OH vitamin D in women with endometriosis and associated pelvic pain. Clin. Chem. Lab. Med. 2017, 55, e282–e284. [Google Scholar] [CrossRef]
- Harris, H.R.; Chavarro, J.E.; Malspeis, S.; Willett, W.C.; Missmer, S.A. Dairy-food, calcium, magnesium, and vitamin D intake and endometriosis: A prospective cohort study. Am. J. Epidemiol. 2013, 177, 420–430. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Velho, R.V.; Werner, F.; Mechsner, S. Endo Belly: What Is It and Why Does It Happen?—A Narrative Review. J. Clin. Med. 2023, 12, 7176. https://doi.org/10.3390/jcm12227176
Velho RV, Werner F, Mechsner S. Endo Belly: What Is It and Why Does It Happen?—A Narrative Review. Journal of Clinical Medicine. 2023; 12(22):7176. https://doi.org/10.3390/jcm12227176
Chicago/Turabian StyleVelho, Renata Voltolini, Franziska Werner, and Sylvia Mechsner. 2023. "Endo Belly: What Is It and Why Does It Happen?—A Narrative Review" Journal of Clinical Medicine 12, no. 22: 7176. https://doi.org/10.3390/jcm12227176
APA StyleVelho, R. V., Werner, F., & Mechsner, S. (2023). Endo Belly: What Is It and Why Does It Happen?—A Narrative Review. Journal of Clinical Medicine, 12(22), 7176. https://doi.org/10.3390/jcm12227176







