The Utility and Appropriateness of Single-Position Circumferential Lumbar Interbody Fusion Using O-Arm-Based Navigation in the Novel Oblique Position
Abstract
:1. Introduction
2. Methods
2.1. Patient Group
2.2. Surgical Technique for the Dual-Position (DP) Group
2.3. Surgical Technique for the Lateral Decubitus Position (LD) Group
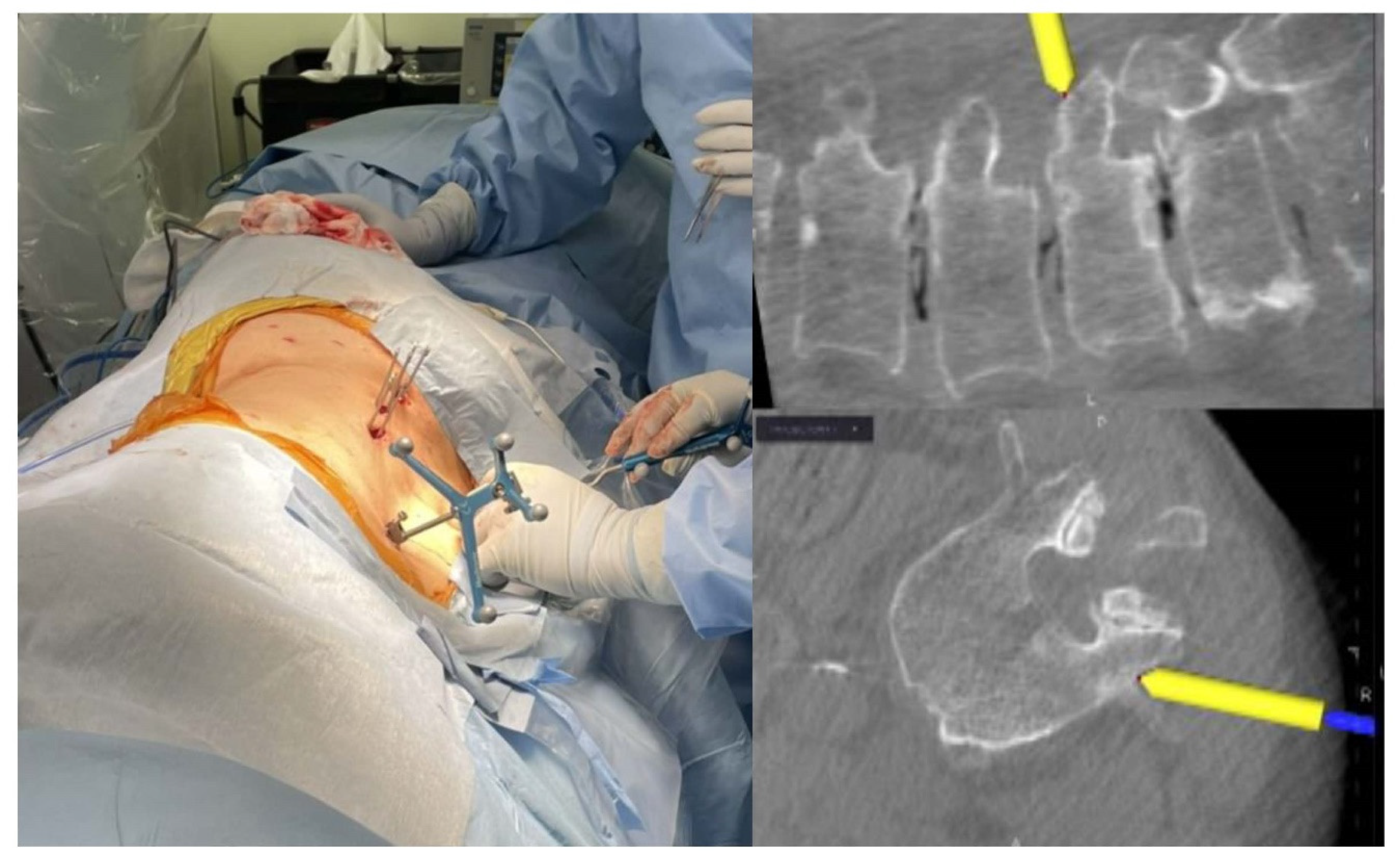
2.4. Surgical Technique for the Oblique (O)-Position Group
2.5. Radiological Evaluation
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sasso, R.C.; Kitchel, S.H.; Dawson, E.G. A prospective, randomized controlled clinical trial of anterior lumbar interbody fusion using a titanium cylindrical threaded fusion device. Spine 2004, 29, 113–122; discussion 121–112. [Google Scholar] [CrossRef]
- O’Toole, J.E.; Eichholz, K.M.; Fessler, R.G. Surgical site infection rates after minimally invasive spinal surgery. J. Neurosurg. Spine 2009, 11, 471–476. [Google Scholar] [CrossRef]
- Kameyama, K.; Ohba, T.; Endo, T.; Katsu, M.; Koji, F.; Kensuke, K.; Oda, K.; Tanaka, N.; Haro, H. Radiological Assessment of Postoperative Paraspinal Muscle Changes After Lumbar Interbody Fusion with or Without Minimally Invasive Techniques. Glob. Spine J. 2023, 13, 295–303. [Google Scholar] [CrossRef]
- Khajavi, K.; Shen, A.; Lagina, M.; Hutchison, A. Comparison of clinical outcomes following minimally invasive lateral interbody fusion stratified by preoperative diagnosis. Eur. Spine J. 2015, 24 (Suppl. S3), 322–330. [Google Scholar] [CrossRef] [PubMed]
- Elowitz, E.H. Central and foraminal indirect decompression in MIS lateral interbody fusion (XLIF): Video lecture. Eur. Spine J. 2015, 24 (Suppl. S3), 449–450. [Google Scholar] [CrossRef] [PubMed]
- Ohba, T.; Ebata, S.; Haro, H. Comparison of serum markers for muscle damage, surgical blood loss, postoperative recovery, and surgical site pain after extreme lateral interbody fusion with percutaneous pedicle screws or traditional open posterior lumbar interbody fusion. BMC Musculoskelet. Disord. 2017, 18, 415. [Google Scholar] [CrossRef] [PubMed]
- Yson, S.C.; Sembrano, J.N.; Santos, E.R.G.; Luna, J.T.P.; Polly, D.W. Does Prone Repositioning Before Posterior Fixation Produce Greater Lordosis in Lateral Lumbar Interbody Fusion (LLIF)? J. Spinal Disord. Tech. 2014, 27, 364–369. [Google Scholar] [CrossRef]
- Blizzard, D.J.; Thomas, J.A. MIS Single-position Lateral and Oblique Lateral Lumbar Interbody Fusion and Bilateral Pedicle Screw Fixation. Spine 2018, 43, 440–446. [Google Scholar] [CrossRef]
- Ouchida, J.; Kanemura, T.; Satake, K.; Nakashima, H.; Ishikawa, Y.; Imagama, S. Simultaneous single-position lateral interbody fusion and percutaneous pedicle screw fixation using O-arm-based navigation reduces the occupancy time of the operating room. Eur. Spine J. 2020, 29, 1277–1286. [Google Scholar] [CrossRef]
- Buckland, A.J.; Ashayeri, K.; Leon, C.; Manning, J.; Eisen, L.; Medley, M.; Protopsaltis, T.S.; Thomas, J.A. Single position circumferential fusion improves operative efficiency, reduces complications and length of stay compared with traditional circumferential fusion. Spine J. 2020, 21, 810–820. [Google Scholar] [CrossRef]
- Romero, S.H.; Berbeo, M.; Diaz, R.; Torres, D.V. Minimally invasive lateral single-position surgery for multilevel degenerative lumbar spine disease: Feasibility and perioperative results in a single Latin-American spine center. Eur. Spine J. 2023, 32, 1688–1694. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, J.L.; McGrath, L.B.; Kirnaz, S.; Sommer, F.; Carnevale, J.A.; Medary, B.; Härtl, R. Single-Position Fluoroscopy-Guided Lateral Lumbar Interbody Fusion with Intraoperative Computed Tomography–Navigated Posterior Pedicle Screw Fixation: Technical Report and Literature Review. Int. J. Spine Surg. 2022, 16, S9–S16. [Google Scholar] [CrossRef] [PubMed]
- Guiroy, A.; Carazzo, C.; Camino-Willhuber, G.; Gagliardi, M.; Fernandes-Joaquim, A.; Cabrera, J.P.; Menezes, C.; Asghar, J. Single-Position Surgery versus Lateral-Then-Prone-Position Circumferential Lumbar Interbody Fusion: A Systematic Literature Review. World Neurosurg. 2021, 151, e379–e386. [Google Scholar] [CrossRef] [PubMed]
- Hiyama, A.; Katoh, H.; Sakai, D.; Tanaka, M.; Sato, M.; Watanabe, M. Facet joint violation after single-position versus dual-position lateral interbody fusion and percutaneous pedicle screw fixation: A comparison of two techniques. J. Clin. Neurosci. 2020, 78, 47–52. [Google Scholar] [CrossRef]
- Ohba, T.; Ebata, S.; Fujita, K.; Sato, H.; Haro, H. Percutaneous pedicle screw placements: Accuracy and rates of cranial facet joint violation using conventional fluoroscopy compared with intraoperative three-dimensional computed tomography computer navigation. Eur. Spine J. 2016, 25, 1775–1780. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.-C.; Chung, H.-T.; Cho, J.-L.; Kim, D.-J.; Chung, N.-S. Factors affecting the accurate placement of percutaneous pedicle screws during minimally invasive transforaminal lumbar interbody fusion. Eur. Spine J. 2011, 20, 1635–1643. [Google Scholar] [CrossRef]
- Neo, M.; Sakamoto, T.; Fujibayashi, S.; Nakamura, T. The clinical risk of vertebral artery injury from cervical pedicle screws inserted in degenerative vertebrae. Spine 2005, 30, 2800–2805. [Google Scholar] [CrossRef]
- Pojskić, M.; Bopp, M.; Saß, B.; Kirschbaum, A.; Nimsky, C.; Carl, B. Intraoperative Computed Tomography-Based Navigation with Augmented Reality for Lateral Approaches to the Spine. Brain Sci. 2021, 11, 646. [Google Scholar] [CrossRef]
- Tan, Y.; Tanaka, M.; Sonawane, S.; Uotani, K.; Oda, Y.; Fujiwara, Y.; Arataki, S.; Yamauchi, T.; Takigawa, T.; Ito, Y. Comparison of Simultaneous Single-Position Oblique Lumbar Interbody Fusion and Percutaneous Pedicle Screw Fixation with Posterior Lumbar Interbody Fusion Using O-arm Navigated Technique for Lumbar Degenerative Diseases. J. Clin. Med. 2021, 10, 4938. [Google Scholar] [CrossRef]
- Chang, C.-C.; Chang, H.-K.; Wu, J.-C.; Tu, T.-H.; Cheng, H.; Huang, W.-C. Comparison of Radiation Exposure Between O-Arm Navigated and C-Arm Guided Screw Placement in Minimally Invasive Transforaminal Lumbar Interbody Fusion. World Neurosurg. 2020, 139, e489–e495. [Google Scholar] [CrossRef]
- DePasse, J.M.; Palumbo, M.A.; Haque, M.; Eberson, C.P.; Daniels, A.H. Complications associated with prone positioning in elective spinal surgery. World J. Orthop. 2015, 6, 351–359. [Google Scholar] [CrossRef] [PubMed]
- Kwee, M.M.; Ho, Y.-H.; Rozen, W.M. The Prone Position During Surgery and its Complications: A Systematic Review and Evidence-Based Guidelines. Int. Surg. 2015, 100, 292–303. [Google Scholar] [CrossRef] [PubMed]
- Warren, S.I.; Wadhwa, H.; Koltsov, J.C.B.; Michaud, J.B.; Cheng, I. One surgeon’s learning curve with single position lateral lumbar interbody fusion: Perioperative outcomes and complications. J. Spine Surg. 2021, 7, 162–169. [Google Scholar] [CrossRef] [PubMed]
- Hiyama, A.; Katoh, H.; Sakai, D.; Sato, M.; Tanaka, M.; Watanabe, M. Accuracy of Percutaneous Pedicle Screw Placement after Single-Position versus Dual-Position Insertion for Lateral Interbody Fusion and Pedicle Screw Fixation Using Fluoroscopy. Asian Spine J. 2022, 16, 20–27. [Google Scholar] [CrossRef]
- Sellin, J.N.; Mayer, R.R.; Hoffman, M.; Ropper, A.E. Simultaneous lateral interbody fusion and pedicle screws (SLIPS) with CT-guided navigation. Clin. Neurol. Neurosurg. 2018, 175, 91–97. [Google Scholar] [CrossRef]
- Thomas, J.A.; Menezes, C.; Buckland, A.J.; Khajavi, K.; Ashayeri, K.; Braly, B.A.; Kwon, B.; Cheng, I.; Berjano, P. Single-position circumferential lumbar spinal fusion: An overview of terminology, concepts, rationale and the current evidence base. Eur. Spine J. 2022, 31, 2167–2174. [Google Scholar] [CrossRef] [PubMed]
- Oba, H.; Ebata, S.; Takahashi, J.; Koyama, K.; Uehara, M.; Kato, H.; Haro, H.; Ohba, T. Pedicle Perforation While Inserting Screws Using O-arm Navigation During Surgery for Adolescent Idiopathic Scoliosis. Spine 2018, 43, E1463–E1468. [Google Scholar] [CrossRef]

| Single Position | p | |||
|---|---|---|---|---|
| Dual Position (n = 35) | Lateral (n = 24) | Oblique (n = 33) | ||
| Age * (years) | 70.2 ± 9.3 | 72.7 ± 12.0 | 73.0 ± 11.8 | 0.26 |
| Sex (female/male) | 24/11 | 19/5 | 26/7 | 0.53 |
| BMI (kg/m2) | 23.1 ± 3.4 | 23.3 ± 4.7 | 22.8 ± 4.1 | 0.21 |
| Fusion length * | 2.06 ± 0.69 | 1.75 ± 0.85 | 1.83 ± 0.89 | 0.19 |
| Fused level of vertebra | ||||
| L2–3 | 8 | 4 | 7 | |
| L3–4 | 9 | 6 | 8 | |
| L4–5 | 34 | 23 | 31 | |
| Single Position | p | |||
|---|---|---|---|---|
| DP (n = 35) | LD (n = 24) | O (n = 33) | ||
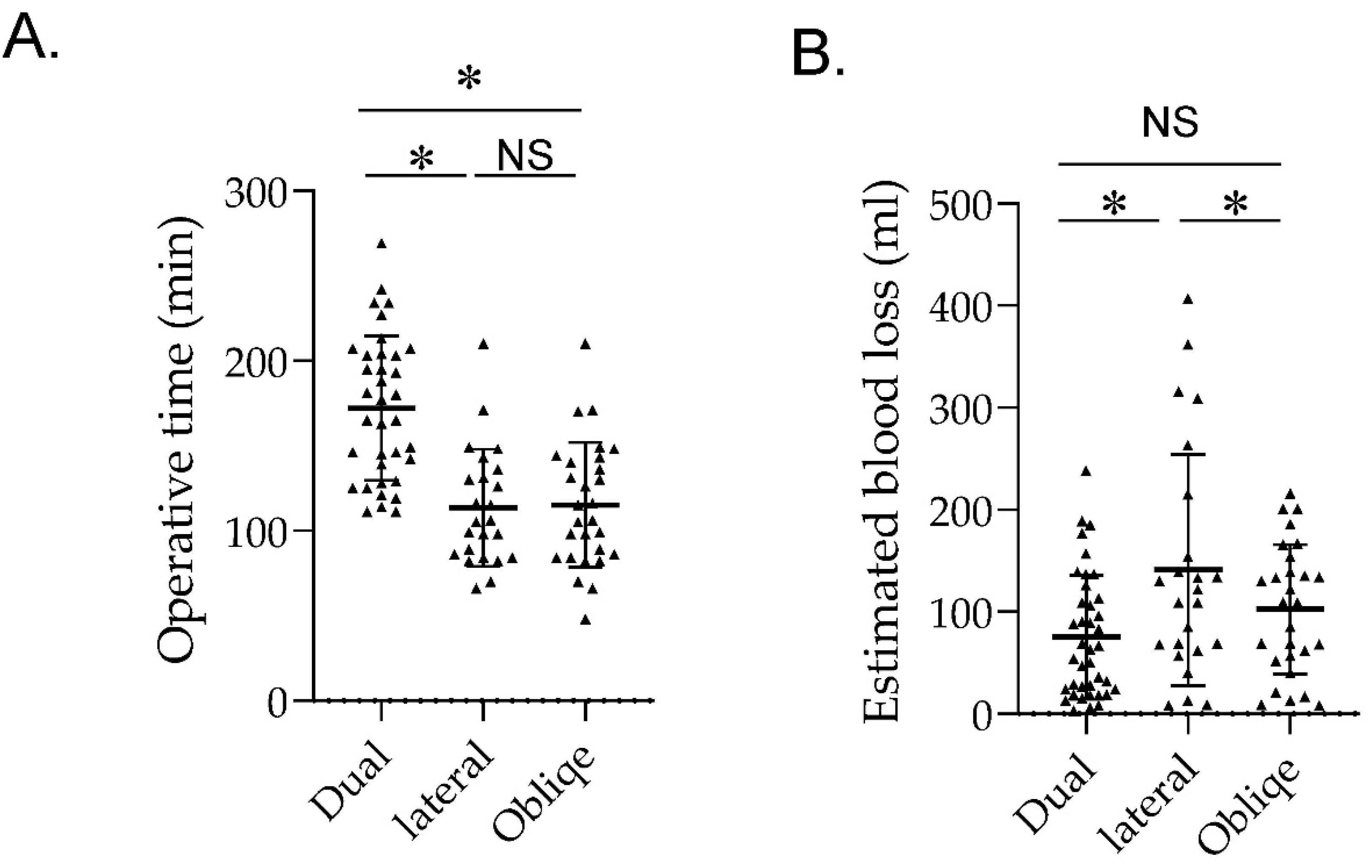
| Operative time (min) | 172.1 ± 42.5 * | 113.5 ± 34.4 | 115.2 ± 36.7 | <0.001 |
| Estimated blood loss (mL) | 75 ± 60.6 | 140.9 ± 113 | 102.6 ± 63.6 | <0.05 |
| Screw parameters | n = 198 | n = 148 | n = 188 | |
| Screw trajectory angle (°) | ||||
| Upside | 34.8 ± 7.1 | 34.2 ± 7.6 | 34.1 ± 5.6 | 0.9 |
| Downside | 33.9 ± 6.6 | 30.1 ± 6.1 * | 33.6 ± 6.2 | <0.05 |
| Accuracy of PPS placement (Grade) † | ||||
| Grade 0 (Upside) | 91 (91.9) | 67 (90.5) | 86 (95.5) | 0.95 |
| Grade 1 | 6 (6.1) | 4 (5.4) | 4 (4.3) | 0.85 |
| Grade 2 | 2 (2.0) | 3 (4.1) | 4 (4.3) | 0.66 |
| Grade 3 | 0 | 0 | 0 | NS |
| Grade 0 (Downside) | 90 (91.0) | 58 (78.4) * | 87 (92.6) | <0.05 |
| Grade 1 | 7 (7.2) | 6 (9.7) | 4 (4.3) | 0.58 |
| Grade 2 | 2 (2.0) | 6 (9.7) | 3 (3.2) | 0.16 |
| Grade 3 | 0 | 4 * | 0 | <0.05 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ohba, T.; Oda, K.; Tanaka, N.; Haro, H. The Utility and Appropriateness of Single-Position Circumferential Lumbar Interbody Fusion Using O-Arm-Based Navigation in the Novel Oblique Position. J. Clin. Med. 2023, 12, 7114. https://doi.org/10.3390/jcm12227114
Ohba T, Oda K, Tanaka N, Haro H. The Utility and Appropriateness of Single-Position Circumferential Lumbar Interbody Fusion Using O-Arm-Based Navigation in the Novel Oblique Position. Journal of Clinical Medicine. 2023; 12(22):7114. https://doi.org/10.3390/jcm12227114
Chicago/Turabian StyleOhba, Tetsuro, Kotaro Oda, Nobuki Tanaka, and Hirotaka Haro. 2023. "The Utility and Appropriateness of Single-Position Circumferential Lumbar Interbody Fusion Using O-Arm-Based Navigation in the Novel Oblique Position" Journal of Clinical Medicine 12, no. 22: 7114. https://doi.org/10.3390/jcm12227114
APA StyleOhba, T., Oda, K., Tanaka, N., & Haro, H. (2023). The Utility and Appropriateness of Single-Position Circumferential Lumbar Interbody Fusion Using O-Arm-Based Navigation in the Novel Oblique Position. Journal of Clinical Medicine, 12(22), 7114. https://doi.org/10.3390/jcm12227114






