Application of Virtual Reality-Assisted Exergaming on the Rehabilitation of Children with Cerebral Palsy: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Methods
2.1. Literature Searching and Search Strategy
2.2. Eligibility Criteria
2.3. Selection Process
2.4. Risk of Bias Assessment
2.5. Data Extraction
2.6. Study Outcomes
2.6.1. Gross Motor Function Measurement (GMFM) Score
2.6.2. PBS Score
2.6.3. Pediatric Evaluation of Disability Inventory (PEDI) Score
2.6.4. Canadian Occupational Performance Measure (COPM) Score
2.6.5. WeeFunctional Independence Measure (WeeFIM) Score
2.6.6. Melbourne Assessment of Unilateral Upper Limb Function-2 (MA-2) Score
2.6.7. Quality of Upper Extremity Skills Test (QUEST) Score
2.6.8. ABILHAND-Kids Test Score
2.7. Data Synthesis
3. Results
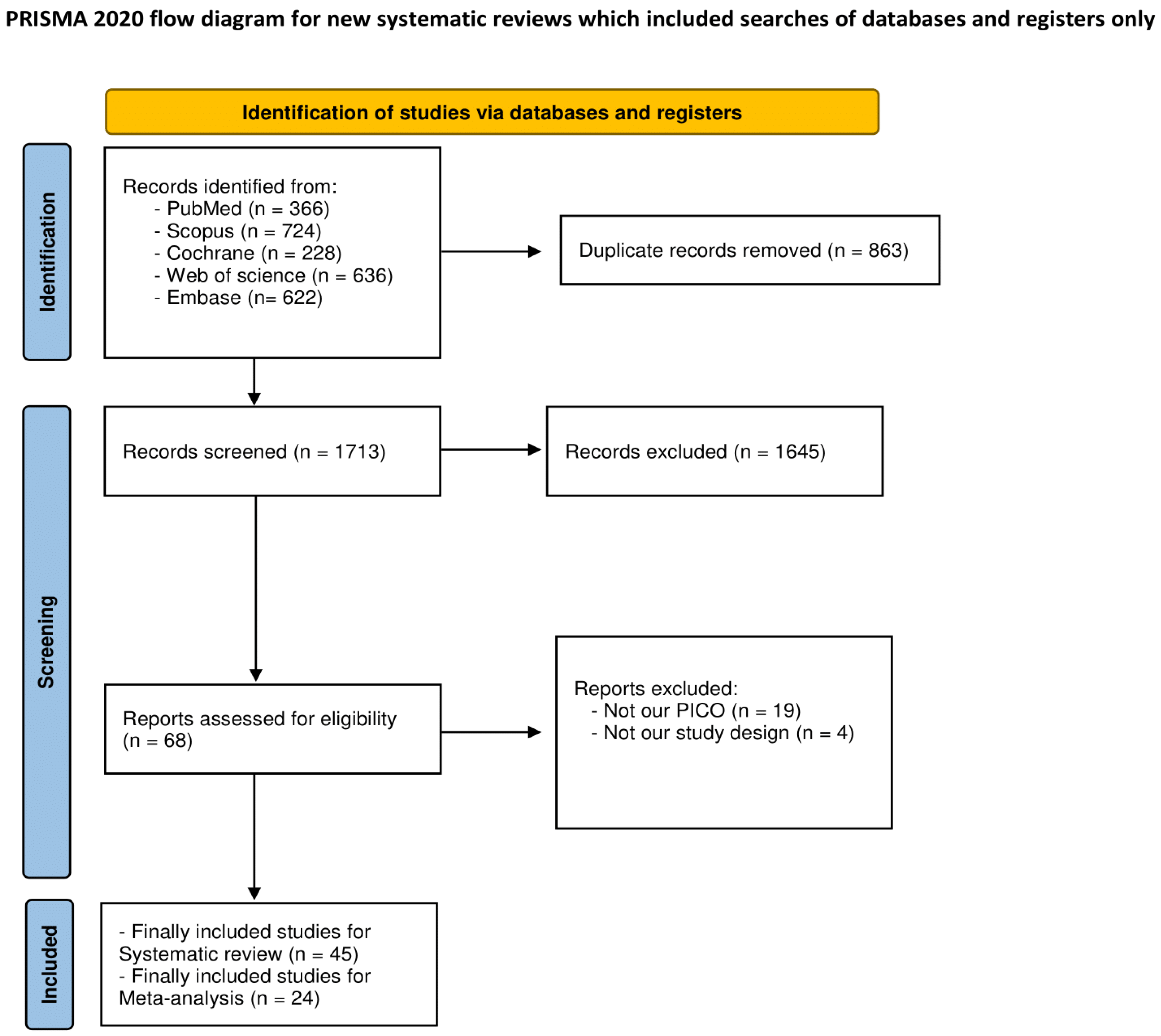
3.1. Literature Search
3.2. Description of the Included Studies
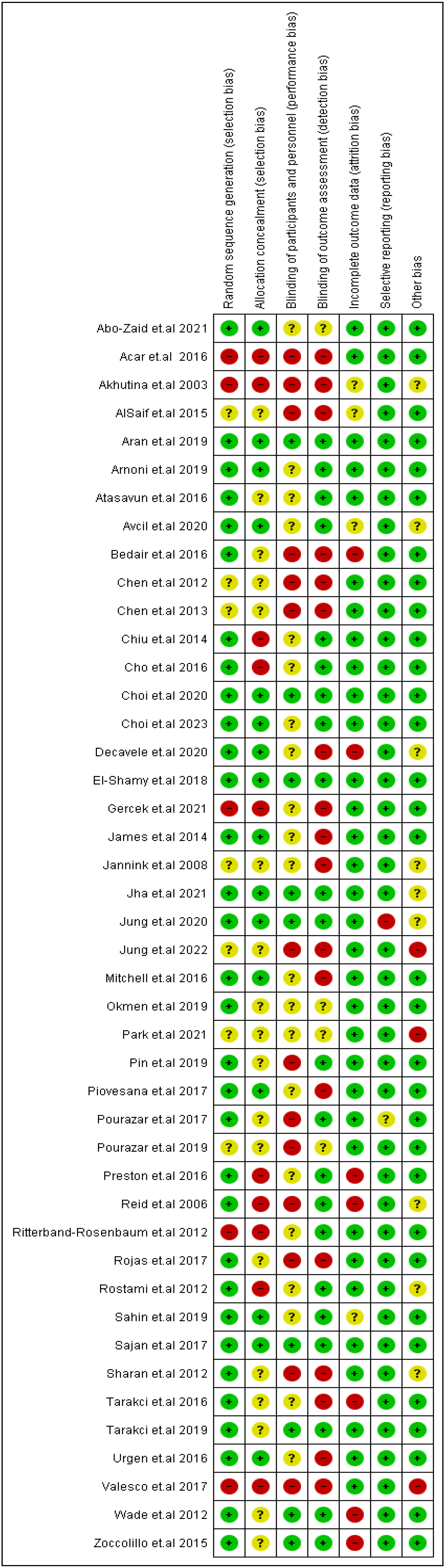
3.3. Quality Assessment Findings
3.4. Results of Quantitative Syntheses
3.4.1. GMFM Score
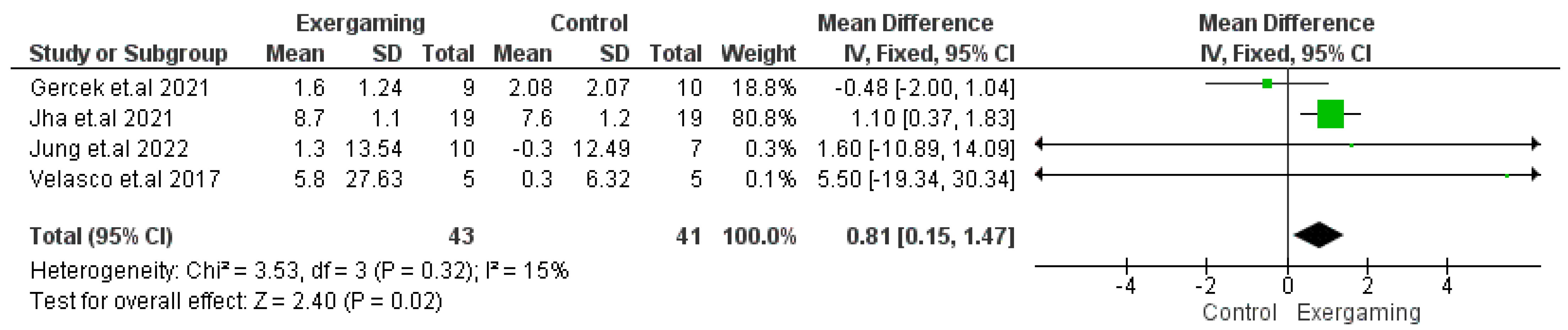
3.4.2. PBS Score
3.4.3. PEDI Score
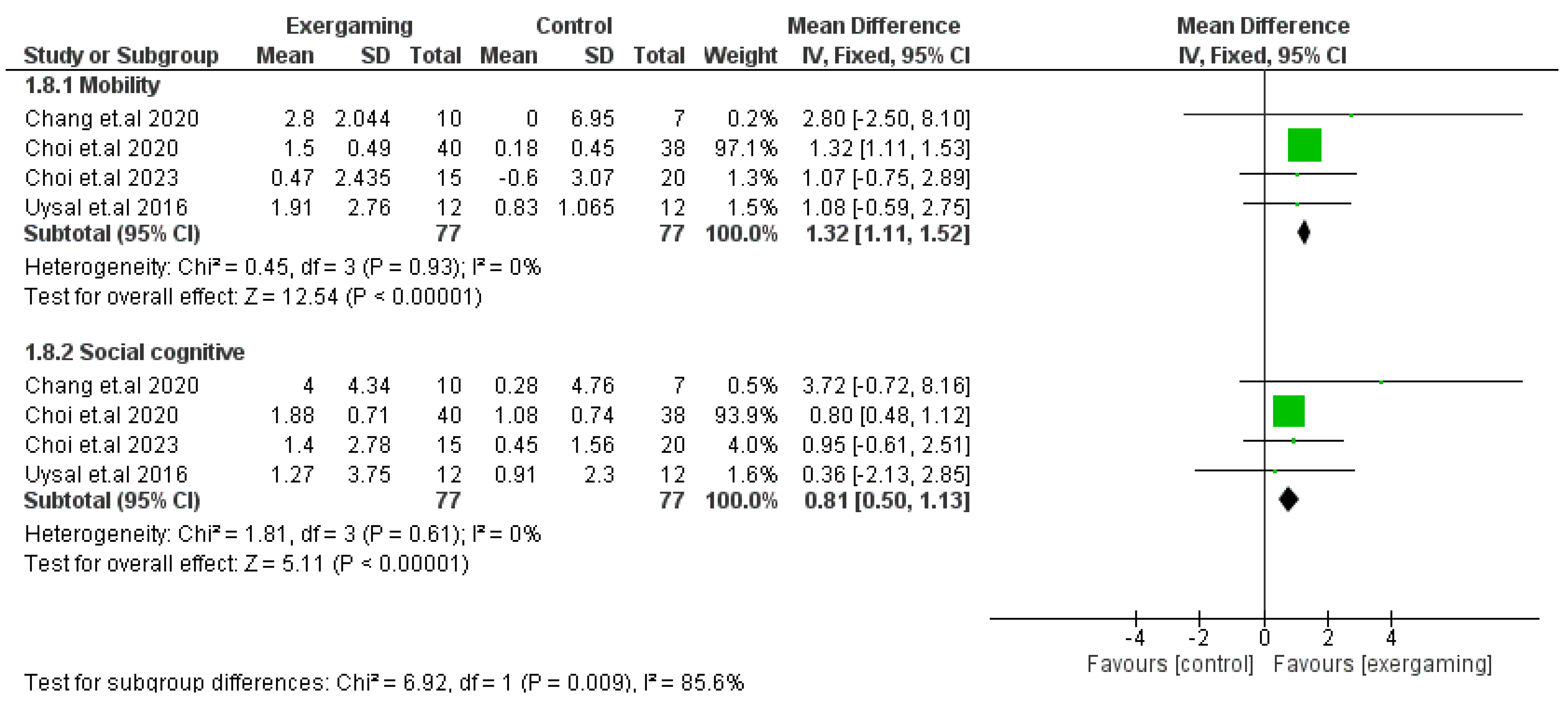
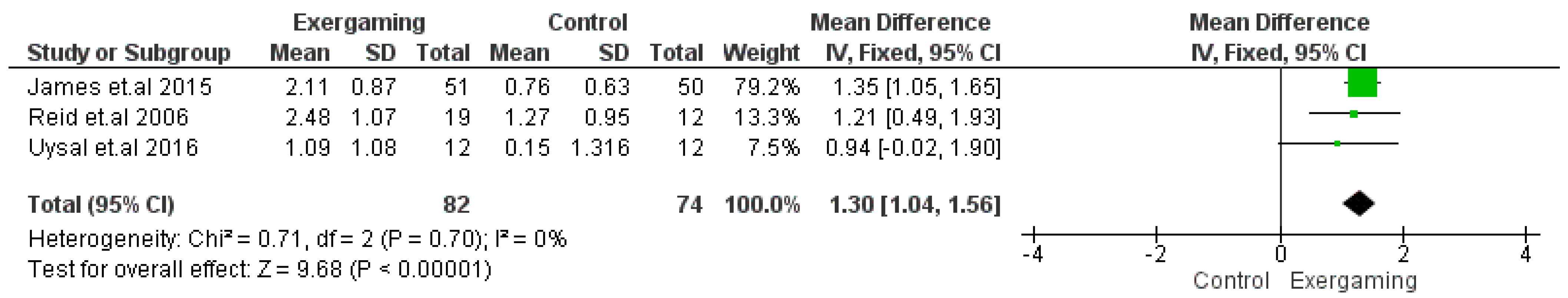
3.4.4. COPM Score
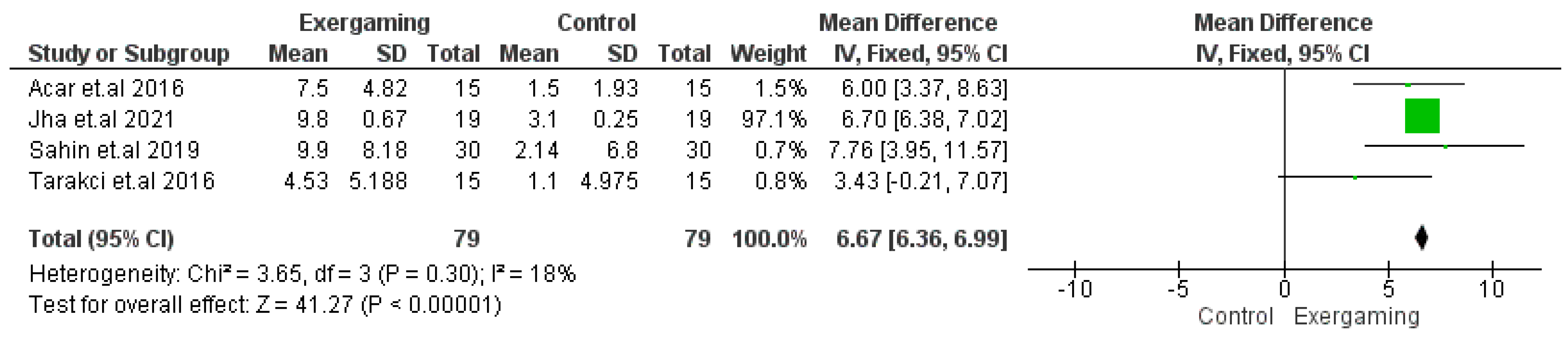
3.4.5. WeeFIM Score
3.4.6. MA-2 Score
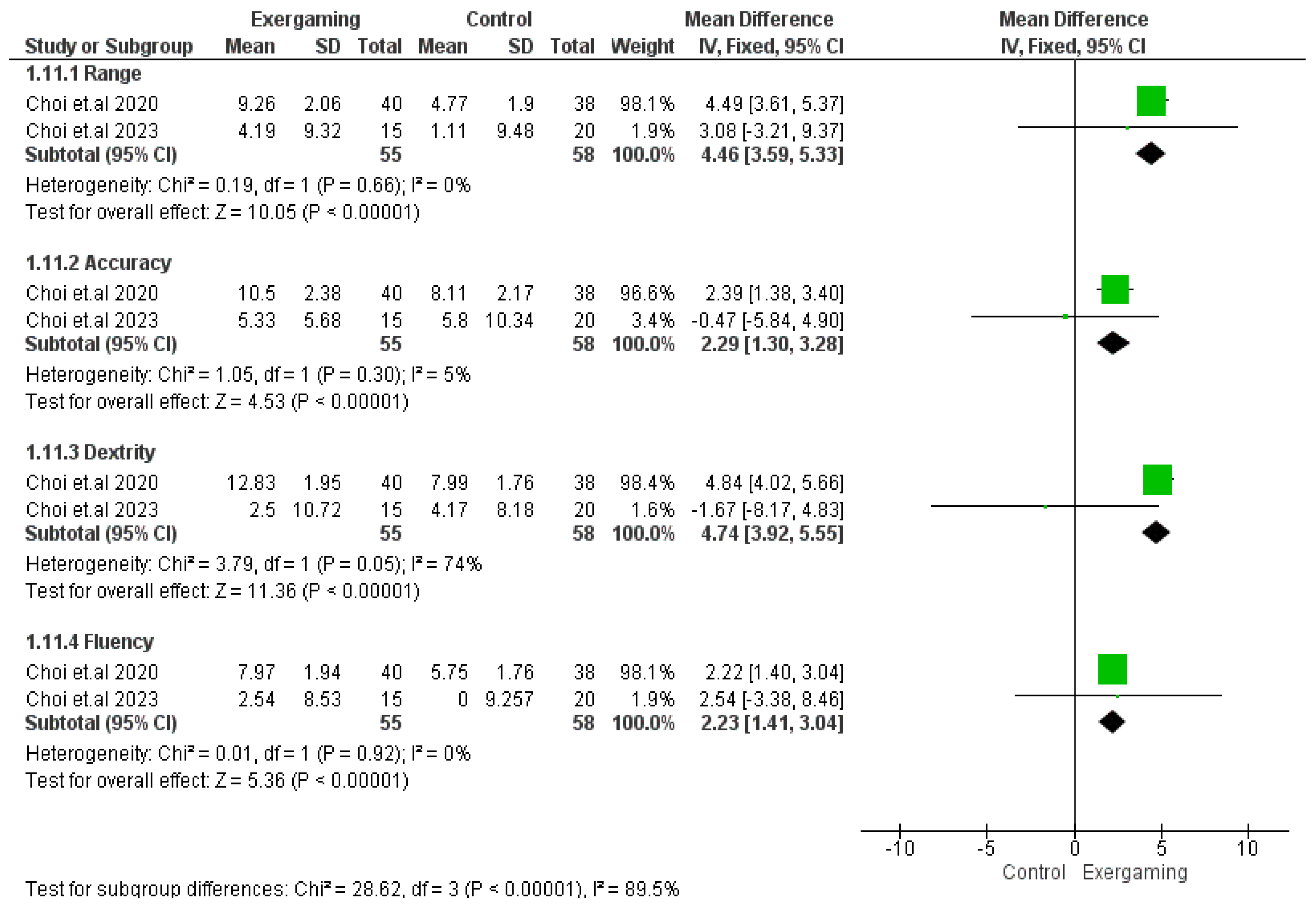
3.4.7. QUEST Score
3.4.8. ABILHAND-Kids Test Score
3.5. Qualitative Synthesis of Other Efficacy Outcomes
3.6. Safety of the Interventions
3.7. GRADE Assessment
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bax, M.; Goldstein, M.; Rosenbaum, P.; Leviton, A.; Paneth, N.; Dan, B.; Jacobsson, B.; Damiano, D. Proposed definition and classification of cerebral palsy, April 2005. Dev. Med. Child Neurol. 2005, 47, 571–576. [Google Scholar] [CrossRef] [PubMed]
- Smithers-Sheedy, H.; Badawi, N.; Blair, E.; Cans, C.; Himmelmann, K.; Krägeloh-Mann, I.; McIntyre, S.; Slee, J.; Uldall, P.; Watson, L.; et al. What constitutes cerebral palsy in the twenty-first century? Dev. Med. Child Neurol. 2014, 56, 323–328. [Google Scholar] [CrossRef] [PubMed]
- Mutch, L.; Alberman, E.; Hagberg, B.; Kodama, K.; Perat, M.V. Cerebral palsy epidemiology: Where are we now and where are we going? Dev. Med. Child Neurol. 1992, 34, 547–551. [Google Scholar] [CrossRef]
- Miller, F.; Bachrach, S. Part one: What is cerebral palsy. In Cerebral Palsy: A Complete Guide for Cargiving, 3rd ed.; John Hopking University Press: Baltimore, MD, USA, 2017; pp. 3–28. [Google Scholar]
- Rosenbaum, P.; Paneth, N.; Leviton, A.; Goldstein, M.; Bax, M.; Damiano, D.; Dan, B.; Jacobsson, B. A report: The definition and classification of cerebral palsy April 2006. Dev. Med. Child Neurol. Suppl. 2007, 109, 8–14. [Google Scholar] [PubMed]
- Gordon, A.M.; Charles, J.; Wolf, S.L. Methods of constraint-induced movement therapy for children with hemiplegic cerebral palsy: Development of a child-friendly intervention for improving upper-extremity function. Arch. Phys. Med. Rehabil. 2005, 86, 837–844. [Google Scholar] [CrossRef]
- Sakzewski, L.; Ziviani, J.; Boyd, R.N. Efficacy of upper limb therapies for unilateral cerebral palsy: A meta-analysis. Pediatrics 2014, 133, e175–e204. [Google Scholar] [CrossRef]
- Odding, E.; Roebroeck, M.E.; Stam, H.J. The epidemiology of cerebral palsy: Incidence, impairments and risk factors. Disabil. Rehabil. 2006, 28, 183–191. [Google Scholar] [CrossRef]
- Noble, J.J.; Chruscikowski, E.; Fry, N.R.D.; Lewis, A.P.; Gough, M.; Shortland, A.P. The relationship between lower limb muscle volume and body mass in ambulant individuals with bilateral cerebral palsy. BMC Neurol. 2017, 17, 223. [Google Scholar] [CrossRef]
- Shumway-Cook, A.; Hutchinson, S.; Kartin, D.; Price, R.; Woollacott, M. Effect of balance training on recovery of stability in children with cerebral palsy. Dev. Med. Child Neurol. 2003, 45, 591–602. [Google Scholar] [CrossRef]
- Deluca, S.C.; Echols, K.; Law, C.R.; Ramey, S.L. Intensive pediatric constraint-induced therapy for children with cerebral palsy: Randomized, controlled, crossover trial. J. Child Neurol. 2006, 21, 931–938. [Google Scholar] [CrossRef]
- Fedrizzi, E.; Pagliano, E.; Andreucci, E.; Oleari, G. Hand function in children with hemiplegic cerebral palsy: Prospective follow-up and functional outcome in adolescence. Dev. Med. Child Neurol. 2003, 45, 85–91. [Google Scholar] [CrossRef] [PubMed]
- Papavasiliou, A.S. Management of motor problems in cerebral palsy: A critical update for the clinician. Eur. J. Paediatr. Neurol. EJPN Off. J. Eur. Paediatr. Neurol. Soc. 2009, 13, 387–396. [Google Scholar] [CrossRef] [PubMed]
- Shepherd, R.B. The changing face of intervention in infants with cerebral palsy. In Cerebral Palsy in Infancy: Targeted Activity to Optimize Early Growth and Development; Shepherd, R.B., Ed.; Elsevier: Amsterdam, The Netherlands, 2014; Churchill Livingstone: Edinburgh, UK, 2014; pp. 3–28. [Google Scholar]
- Rahlin, M.; Duncan, B.; Howe, C.L.; Pottinger, H.L. How does the intensity of physical therapy affect the Gross Motor Function Measure (GMFM-66) total score in children with cerebral palsy? A systematic review protocol. BMJ Open 2020, 10, e036630. [Google Scholar] [CrossRef]
- Chen, Y.; Fanchiang, H.D.; Howard, A. Effectiveness of Virtual Reality in Children With Cerebral Palsy: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Phys. Ther. 2018, 98, 63–77. [Google Scholar] [CrossRef] [PubMed]
- Dewar, R.; Love, S.; Johnston, L.M. Exercise interventions improve postural control in children with cerebral palsy: A systematic review. Dev. Med. Child Neurol. 2015, 57, 504–520. [Google Scholar] [CrossRef] [PubMed]
- Tinderholt Myrhaug, H.; Østensjø, S.; Larun, L.; Odgaard-Jensen, J.; Jahnsen, R. Intensive training of motor function and functional skills among young children with cerebral palsy: A systematic review and meta-analysis. BMC Pediatr. 2014, 14, 292. [Google Scholar] [CrossRef]
- Bryanton, C.; Bossé, J.; Brien, M.; McLean, J.; McCormick, A.; Sveistrup, H. Feasibility, motivation, and selective motor control: Virtual reality compared to conventional home exercise in children with cerebral palsy. Cyberpsychol. Behav. 2006, 9, 123–128. [Google Scholar] [CrossRef] [PubMed]
- Snider, L.; Majnemer, A.; Darsaklis, V. Virtual reality as a therapeutic modality for children with cerebral palsy. Dev. Neurorehabilit. 2010, 13, 120–128. [Google Scholar] [CrossRef]
- Galvin, J.; McDonald, R.; Catroppa, C.; Anderson, V. Does intervention using virtual reality improve upper limb function in children with neurological impairment: A systematic review of the evidence. Brain Inj. 2011, 25, 435–442. [Google Scholar] [CrossRef]
- Holden, M.K. Virtual environments for motor rehabilitation: Review. Cyberpsychol. Behav. 2005, 8, 187–211; discussion 2–9. [Google Scholar] [CrossRef]
- Brütsch, K.; Schuler, T.; Koenig, A.; Zimmerli, L.; Koeneke, S.M.; Lünenburger, L.; Riener, R.; Jäncke, L.; Meyer-Heim, A. Influence of virtual reality soccer game on walking performance in robotic assisted gait training for children. J. Neuroeng. Rehabil. 2010, 7, 15. [Google Scholar] [CrossRef]
- Weiss, P.; Kizony, R.; Feintuch, U.; Katz, N. Virtual reality in neurorehabilitation. In Textbook of Neural Repair and Rehabilitation; Cambridge University Press: Cambridge, UK, 2006; pp. 182–197. [Google Scholar] [CrossRef]
- Pimentel, K.; Teixeira, K. Virtual Reality: Through the New Looking Glass, 2nd ed.; Reed Business Information, Inc.: New York, NY, USA, 1995. [Google Scholar]
- Fehlings, D.; Switzer, L.; Findlay, B.; Knights, S. Interactive computer play as “motor therapy” for individuals with cerebral palsy. Semin. Pediatr. Neurol. 2013, 20, 127–138. [Google Scholar] [CrossRef]
- Weiss, P.L.; Tirosh, E.; Fehlings, D. Role of virtual reality for cerebral palsy management. J. Child Neurol. 2014, 29, 1119–1124. [Google Scholar] [CrossRef] [PubMed]
- Sakzewski, L.; Gordon, A.; Eliasson, A.C. The state of the evidence for intensive upper limb therapy approaches for children with unilateral cerebral palsy. J. Child Neurol. 2014, 29, 1077–1090. [Google Scholar] [CrossRef] [PubMed]
- Ren, Z.; Wu, J. The Effect of Virtual Reality Games on the Gross Motor Skills of Children with Cerebral Palsy: A Meta-Analysis of Randomized Controlled Trials. Int. J. Environ. Res. Public Health 2019, 16, 3885. [Google Scholar] [CrossRef]
- Palaus, M.; Marron, E.M.; Viejo-Sobera, R.; Redolar-Ripoll, D. Neural Basis of Video Gaming: A Systematic Review. Front. Hum. Neurosci. 2017, 11, 248. [Google Scholar] [CrossRef] [PubMed]
- Page, S.J.; Levine, P.; Sisto, S.; Bond, Q.; Johnston, M.V. Stroke patients’ and therapists’ opinions of constraint-induced movement therapy. Clin. Rehabil. 2002, 16, 55–60. [Google Scholar] [CrossRef]
- Levin, M.F. Can virtual reality offer enriched environments for rehabilitation? Expert Rev. Neurother. 2011, 11, 153–155. [Google Scholar] [CrossRef]
- Todorov, E.; Shadmehr, R.; Bizzi, E. Augmented Feedback Presented in a Virtual Environment Accelerates Learning of a Difficult Motor Task. J. Mot. Behav. 1997, 29, 147–158. [Google Scholar] [CrossRef]
- Tatla, S.K.; Sauve, K.; Virji-Babul, N.; Holsti, L.; Butler, C.; Van Der Loos, H.F. Evidence for outcomes of motivational rehabilitation interventions for children and adolescents with cerebral palsy: An American Academy for Cerebral Palsy and Developmental Medicine systematic review. Dev. Med. Child Neurol. 2013, 55, 593–601. [Google Scholar] [CrossRef]
- Bilde, P.E.; Kliim-Due, M.; Rasmussen, B.; Petersen, L.Z.; Petersen, T.H.; Nielsen, J.B. Individualized, home-based interactive training of cerebral palsy children delivered through the Internet. BMC Neurol. 2011, 11, 32. [Google Scholar] [CrossRef]
- Higgins, J.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.; Welch, V. Cochrane Handbook for Systematic Reviews of Interventions, 2nd ed.; John Wiley & Sons: Chichester, UK, 2022. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- NHLBI. Study Quality Assessment Tools; National Institutes of Health: Bethesda, MD, USA, 2018.
- Alotaibi, M.; Long, T.; Kennedy, E.; Bavishi, S. The efficacy of GMFM-88 and GMFM-66 to detect changes in gross motor function in children with cerebral palsy (CP): A literature review. Disabil. Rehabil. 2014, 36, 617–627. [Google Scholar] [CrossRef]
- Russell, D.J.; Rosenbaum, P.L.; Cadman, D.T.; Gowland, C.; Hardy, S.; Jarvis, S. The gross motor function measure: A means to evaluate the effects of physical therapy. Dev. Med. Child Neurol. 1989, 31, 341–352. [Google Scholar] [CrossRef]
- Mayston, M. Gross Motor Function Measure (GMFM-66 & GMFM-88) User’s Manual, 3rd Edition Dianne J Russell, Marilyn Wright, Peter L Rosenbaum, Lisa M AveryLondon: Mac Keith Press, 2021 £80.00 (Paperback), pp. 320 ISBN: 978-1-911612-49-0. Dev. Med. Child Neurol. 2021, 63, 1236. [Google Scholar] [CrossRef]
- Chen, C.L.; Shen, I.H.; Chen, C.Y.; Wu, C.Y.; Liu, W.Y.; Chung, C.Y. Validity, responsiveness, minimal detectable change, and minimal clinically important change of Pediatric Balance Scale in children with cerebral palsy. Res. Dev. Disabil. 2013, 34, 916–922. [Google Scholar] [CrossRef] [PubMed]
- Stephen, M.H.; Coster, W.J.; Ludlow, L.H. Pediatric Functional Outcome Measures. Phys. Med. Rehabil. Clin. N. Am. 1991, 2, 689–723. [Google Scholar] [CrossRef]
- Carswell, A.; McColl, M.A.; Baptiste, S.; Law, M.; Polatajko, H.; Pollock, N. The Canadian Occupational Performance Measure: A research and clinical literature review. Can. J. Occup. Therapy. Rev. Can. d’Ergotherapie 2004, 71, 210–222. [Google Scholar] [CrossRef]
- Tur, B.S.; Küçükdeveci, A.A.; Kutlay, S.; Yavuzer, G.; Elhan, A.H.; Tennant, A. Psychometric properties of the WeeFIM in children with cerebral palsy in Turkey. Dev. Med. Child Neurol. 2009, 51, 732–738. [Google Scholar] [CrossRef]
- Randall, M.; Imms, C.; Carey, L.M.; Pallant, J.F. Rasch analysis of The Melbourne Assessment of Unilateral Upper Limb Function. Dev. Med. Child Neurol. 2014, 56, 665–672. [Google Scholar] [CrossRef]
- Thorley, M.; Lannin, N.; Cusick, A.; Novak, I.; Boyd, R. Reliability of the quality of upper extremity skills test for children with cerebral palsy aged 2 to 12 years. Phys. Occup. Ther. Pediatr. 2012, 32, 4–21. [Google Scholar] [CrossRef]
- Arnould, C.; Penta, M.; Renders, A.; Thonnard, J.L. ABILHAND-Kids: A measure of manual ability in children with cerebral palsy. Neurology 2004, 63, 1045–1052. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef]
- Choi, J.Y.; Yi, S.-H.; Shim, D.; Yoo, B.; Park, E.S.; Rha, D.-W. Home-based virtual reality-enhanced upper limb training system in children with brain injury: A randomized controlled trial. Front. Pediatr. 2023, 11, 1131573. [Google Scholar] [CrossRef]
- Gercek, N.; Tatar, Y.; Uzun, S. Alternative exercise methods for children with cerebral palsy: Effects of virtual vs. traditional golf training. Int. J. Dev. Disabil. 2022, 68, 933–942. [Google Scholar] [CrossRef] [PubMed]
- Jung, Y.G.; Chang, H.J.; Jo, E.S.; Kim, D.H. The Effect of a Horse-Riding Simulator with Virtual Reality on Gross Motor Function and Body Composition of Children with Cerebral Palsy: Preliminary Study. Sensors 2022, 22, 2903. [Google Scholar] [CrossRef] [PubMed]
- Jha, K.K.; Karunanithi, G.B.; Sahana, A.; Karthikbabu, S. Randomised trial of virtual reality gaming and physiotherapy on balance, gross motor performance and daily functions among children with bilateral spastic cerebral palsy. Somatosens. Mot. Res. 2021, 38, 117–126. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.J.; Ku, K.H.; Park, Y.S.; Park, J.G.; Cho, E.S.; Seo, J.S.; Kim, C.W.; O, S.H. Effects of virtual reality-based rehabilitation on upper extremity function among children with cerebral palsy. Healthcare 2020, 10, 391. [Google Scholar] [CrossRef]
- Choi, J.Y.; Yi, S.H.; Ao, L.; Tang, X.; Xu, X.; Shim, D.; Yoo, B.; Park, E.S.; Rha, D.W. Virtual reality rehabilitation in children with brain injury: A randomized controlled trial. Dev. Med. Child Neurol. 2021, 63, 480–487. [Google Scholar] [CrossRef]
- Decavele, S.; Ortibus, E.; Van Campenhout, A.; Molenaers, G.; Jansen, B.; Omelina, L.; Franki, I. The effect of a rehabilitation-specific gaming software platform to achieve individual physiotherapy goals in children with severe spastic cerebral palsy: A randomized crossover trial. Games Health J. 2020, 9, 376–385. [Google Scholar] [CrossRef] [PubMed]
- Jung, S.; Song, S.; Lee, D.; Lee, K.; Lee, G. Effects of Kinect Video Game Training on Lower Extremity Motor Function, Balance, and Gait in Adolescents with Spastic Diplegia Cerebral Palsy: A Pilot Randomized Controlled Trial. Dev. Neurorehabilit. 2021, 24, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Pin, T.W.; Butler, P.B. The effect of interactive computer play on balance and functional abilities in children with moderate cerebral palsy: A pilot randomized study. Clin. Rehabil. 2019, 33, 704–710. [Google Scholar] [CrossRef]
- Şahin, S.; Köse, B.; Aran, O.T.; Bahadır Ağce, Z.; Kayıhan, H. The effects of virtual reality on motor functions and daily life activities in unilateral spastic cerebral palsy: A single-blind randomized controlled trial. Games Health J. 2020, 9, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Velasco, M.A.; Raya, R.; Muzzioli, L.; Morelli, D.; Otero, A.; Iosa, M.; Cincotti, F.; Rocon, E. Evaluation of cervical posture improvement of children with cerebral palsy after physical therapy based on head movements and serious games. BioMedical Eng. OnLine 2017, 16, 74. [Google Scholar] [CrossRef] [PubMed]
- Acar, G.; Altun, G.P.; Yurdalan, S.; Polat, M.G. Efficacy of neurodevelopmental treatment combined with the Nintendo® Wii in patients with cerebral palsy. J. Phys. Ther. Sci. 2016, 28, 774–780. [Google Scholar] [CrossRef]
- Bedair, R.; Al-Talawy, H.; Shoukry, K.; Abdul-Raouf, E. Impact of virtual reality games as an adjunct treatment tool on upper extremity function of spastic hemiplegic children. Int. J. Pharm. Tech. Res. 2016, 9, 1–8. [Google Scholar]
- Cho, C.; Hwang, W.; Hwang, S.; Chung, Y. Treadmill training with virtual reality improves gait, balance, and muscle strength in children with cerebral palsy. Tohoku J. Exp. Med. 2016, 238, 213–218. [Google Scholar] [CrossRef] [PubMed]
- Sajan, J.E.; John, J.A.; Grace, P.; Sabu, S.S.; Tharion, G. Wii-based interactive video games as a supplement to conventional therapy for rehabilitation of children with cerebral palsy: A pilot, randomized controlled trial. Dev. Neurorehabilit. 2017, 20, 361–367. [Google Scholar] [CrossRef]
- Tarakci, D.; Ersoz Huseyinsinoglu, B.; Tarakci, E.; Razak Ozdincler, A. Effects of Nintendo Wii-Fit(®) video games on balance in children with mild cerebral palsy. Pediatr. Int. Off. J. Jpn. Pediatr. Soc. 2016, 58, 1042–1050. [Google Scholar] [CrossRef]
- Urgen, M.S.; Akbayrak, T.; Günel, M.K.; Çankaya, Ö.; Güçhan, Z.; Türkyılmaz, E.S. Investigation of the effects of the Nintendo® Wii-Fit training on balance and advanced motor performance in children with spastic hemiplegic cerebral palsy: A Randomized Controlled Trial. Int. J. Ther. Rehabil. Res. 2016, 5, 146–157. [Google Scholar]
- Atasavun Uysal, S.; Baltaci, G. Effects of Nintendo Wii™ Training on Occupational Performance, Balance, and Daily Living Activities in Children with Spastic Hemiplegic Cerebral Palsy: A Single-Blind and Randomized Trial. Games Health J. 2016, 5, 311–317. [Google Scholar] [CrossRef] [PubMed]
- James, S.; Ziviani, J.; Ware, R.S.; Boyd, R.N. Randomized controlled trial of web-based multimodal therapy for unilateral cerebral palsy to improve occupational performance. Dev. Med. Child Neurol. 2015, 57, 530–538. [Google Scholar] [CrossRef] [PubMed]
- Preston, N.; Weightman, A.; Gallagher, J.; Levesley, M.; Mon-Williams, M.; Clarke, M.; O’Connor, R.J. A pilot single-blind multicentre randomized controlled trial to evaluate the potential benefits of computer-assisted arm rehabilitation gaming technology on the arm function of children with spastic cerebral palsy. Clin. Rehabil. 2016, 30, 1004–1015. [Google Scholar] [CrossRef] [PubMed]
- Zoccolillo, L.; Morelli, D.; Cincotti, F.; Muzzioli, L.; Gobbetti, T.; Paolucci, S.; Iosa, M. Video-game based therapy performed by children with cerebral palsy: A cross-over randomized controlled trial and a cross-sectional quantitative measure of physical activity. Eur. J. Phys. Rehabil. Med. 2015, 51, 669–676. [Google Scholar] [PubMed]
- Salem, Y.; Gropack, S.J.; Coffin, D.; Godwin, E.M. Effectiveness of a low-cost virtual reality system for children with developmental delay: A preliminary randomised single-blind controlled trial. Physiotherapy 2012, 98, 189–195. [Google Scholar] [CrossRef] [PubMed]
- Sharan, D.; Ajeesh, P.S.; Rameshkumar, R.; Mathankumar, M.; Paulina, R.J.; Manjula, M. Virtual reality based therapy for post operative rehabilitation of children with cerebral palsy. Work 2012, 41 (Suppl. S1), 3612–3615. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.L.; Chen, C.Y.; Liaw, M.Y.; Chung, C.Y.; Wang, C.J.; Hong, W.H. Efficacy of home-based virtual cycling training on bone mineral density in ambulatory children with cerebral palsy. Osteoporos. Int. 2013, 24, 1399–1406. [Google Scholar] [CrossRef]
- Reid, D.; Campbell, K. The use of virtual reality with children with cerebral palsy: A pilot randomized trial. Ther. Recreat. J. 2006, 40, 255–268. [Google Scholar]
- Park, S.-H.; Son, S.-M.; Choi, J.-Y. Effect of posture control training using virtual reality program on sitting balance and trunk stability in children with cerebral palsy. NeuroRehabilitation 2021, 48, 247–254. [Google Scholar] [CrossRef]
- Abo-zaid, N.; Helmy, N.; Elsayed, N.; Mohammed, A. Wii Sport. versus task-oriented training on gait in unilateral cerebral palsy: A randomized controlled trial. J. Hum. Sport Exerc. 2021, 16, S522–S531. [Google Scholar] [CrossRef]
- Avcil, E.; Tarakci, D.; Arman, N.; Tarakci, E. Upper extremity rehabilitation using video games in cerebral palsy: A randomized clinical trial. Acta Neurol. Belg. 2021, 121, 1053–1060. [Google Scholar] [CrossRef] [PubMed]
- Aran, O.T.; Şahin, S.; Köse, B.; Ağce, Z.B.; Kayihan, H. Effectiveness of the virtual reality on cognitive function of children with hemiplegic cerebral palsy: A single-blind randomized controlled trial. Int. J. Rehabil. Res. 2020, 43, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Arnoni, J.L.B.; Pavao, S.L.; dos Santos Silva, F.P.; Rocha, N.A.C.F. Effects of virtual reality in body oscillation and motor performance of children with cerebral palsy: A preliminary randomized controlled clinical trial. Complement. Ther. Clin. Pract. 2019, 35, 189–194. [Google Scholar] [CrossRef] [PubMed]
- Ballester, B.R.; Maier, M.; Domingo, D.A.; Aguilar, A.; Mura, A.; Pareja, L.T.; Esteve, M.F.G.; Verschure, P.F.M.J. Adaptive VR-based rehabilitation to prevent deterioration in adults with cerebral palsy. In Proceedings of the 2019 International Conference on Virtual Rehabilitation (ICVR), Tel Aviv, Israel, 21–24 July 2019; pp. 1–7. [Google Scholar]
- Ökmen, B.M.; Aslan, M.D.; Yüzer, G.F.N.; Özgirgin, N. Effect of virtual reality therapy on functional development in children with cerebral palsy: A single-blind, prospective, randomized-controlled study. Turk. J. Phys. Med. Rehabil. 2019, 65, 371. [Google Scholar] [CrossRef]
- Pourazar, M.; Bagherzadeh, F.; Mirakhori, F. Virtual reality training improves dynamic balance in children with cerebral palsy. Int. J. Dev. Disabil. 2021, 67, 422–427. [Google Scholar] [CrossRef]
- Tarakci, E.; Arman, N.; Tarakci, D.; Kasapcopur, O. Leap Motion Controller-based training for upper extremity rehabilitation in children and adolescents with physical disabilities: A randomized controlled trial. J. Hand Ther. Off. J. Am. Soc. Hand Ther. 2020, 33, 220–228.e1. [Google Scholar] [CrossRef]
- El-Shamy, S.M.; El-Banna, M.F. Effect of Wii training on hand function in children with hemiplegic cerebral palsy. Physiother. Theory Pract. 2020, 36, 38–44. [Google Scholar] [CrossRef]
- Gatica-Rojas, V.; Méndez-Rebolledo, G.; Guzman-Muñoz, E.; Soto-Poblete, A.; Cartes-Velásquez, R.; Elgueta-Cancino, E.; Cofré Lizama, E. Does Nintendo Wii Balance Board improve standing balance? A randomized controlled trial in children with cerebral palsy. Eur. J. Phys. Rehabil. Med. 2017, 53, 535–544. [Google Scholar] [CrossRef]
- Pourazar, M.; Mirakhori, F.; Hemayattalab, R.; Bagherzadeh, F. Use of virtual reality intervention to improve reaction time in children with cerebral palsy: A randomized controlled trial. Dev. Neurorehabilit. 2018, 21, 515–520. [Google Scholar] [CrossRef]
- Mitchell, L.E.; Ziviani, J.; Boyd, R.N. A randomized controlled trial of web-based training to increase activity in children with cerebral palsy. Dev. Med. Child Neurol. 2016, 58, 767–773. [Google Scholar] [CrossRef]
- Piovesana, A.M.; Ross, S.; Lloyd, O.; Whittingham, K.; Ziviani, J.; Ware, R.S.; Boyd, R.N. Randomized controlled trial of a web-based multi-modal therapy program for executive functioning in children and adolescents with unilateral cerebral palsy. Disabil. Rehabil. 2017, 39, 2021–2028. [Google Scholar] [CrossRef]
- AlSaif, A.A.; Alsenany, S. Effects of interactive games on motor performance in children with spastic cerebral palsy. J. Phys. Ther. Sci. 2015, 27, 2001–2003. [Google Scholar] [CrossRef] [PubMed]
- Chiu, H.-C.; Ada, L.; Lee, H.-M. Upper limb training using Wii Sports Resort™ for children with hemiplegic cerebral palsy: A randomized, single-blind trial. Clin. Rehabil. 2014, 28, 1015–1024. [Google Scholar] [CrossRef]
- Chen, C.-L.; Hong, W.-H.; Cheng, H.-Y.K.; Liaw, M.-Y.; Chung, C.-Y.; Chen, C.-Y. Muscle strength enhancement following home-based virtual cycling training in ambulatory children with cerebral palsy. Res. Dev. Disabil. 2012, 33, 1087–1094. [Google Scholar] [CrossRef] [PubMed]
- Ritterband-Rosenbaum, A.; Christensen, M.S.; Nielsen, J.B. Twenty weeks of computer-training improves sense of agency in children with spastic cerebral palsy. Res. Dev. Disabil. 2012, 33, 1227–1234. [Google Scholar] [CrossRef]
- Rostami, H.R.; Arastoo, A.A.; Nejad, S.J.; Mahany, M.K.; Malamiri, R.A.; Goharpey, S. Effects of modified constraint-induced movement therapy in virtual environment on upper-limb function in children with spastic hemiparetic cerebral palsy: A randomised controlled trial. NeuroRehabilitation 2012, 31, 357–365. [Google Scholar] [CrossRef]
- Wade, W.; Porter, D. Sitting playfully: Does the use of a centre of gravity computer game controller influence the sitting ability of young people with cerebral palsy? Disabil. Rehabil. Assist. Technol. 2012, 7, 122–129. [Google Scholar] [CrossRef] [PubMed]
- Jannink, M.J.A.; Van Der Wilden, G.J.; Navis, D.W.; Visser, G.; Gussinklo, J.; Ijzerman, M. A low-cost video game applied for training of upper extremity function in children with cerebral palsy: A pilot study. Cyberpsychol. Behav. 2008, 11, 27–32. [Google Scholar] [CrossRef] [PubMed]
- Akhutina, T.y.; Foreman, N.; Krichevets, A.; Matikka, L.; Narhi, V.; Pylaeva, N.; Vahakuopus, J. Improving spatial functioning in children with cerebral palsy using computerized and traditional game tasks. Disabil. Rehabil. 2003, 25, 1361–1371. [Google Scholar] [CrossRef]
- Svraka, E. Cerebral Palsy-Challenges for the Future; InTech: Rijeka, Croatia, 2014; 312p. [Google Scholar]
- Lange, B.; Koenig, S.; Chang, C.Y.; McConnell, E.; Suma, E.; Bolas, M.; Rizzo, A. Designing informed game-based rehabilitation tasks leveraging advances in virtual reality. Disabil. Rehabil. 2012, 34, 1863–1870. [Google Scholar] [CrossRef]
- Mirelman, A.; Maidan, I.; Deutsch, J.E. Virtual reality and motor imagery: Promising tools for assessment and therapy in Parkinson’s disease. Mov. Disord. Off. J. Mov. Disord. Soc. 2013, 28, 1597–1608. [Google Scholar] [CrossRef] [PubMed]
- Damiano, D.L. Activity, activity, activity: Rethinking our physical therapy approach to cerebral palsy. Phys. Ther. 2006, 86, 1534–1540. [Google Scholar] [CrossRef] [PubMed]
- Lang, C.E.; Macdonald, J.R.; Reisman, D.S.; Boyd, L.; Jacobson Kimberley, T.; Schindler-Ivens, S.M.; Hornby, T.G.; Ross, S.A.; Scheets, P.L. Observation of amounts of movement practice provided during stroke rehabilitation. Arch. Phys. Med. Rehabil. 2009, 90, 1692–1698. [Google Scholar] [CrossRef]
- Chen, Y.P.; Lee, S.Y.; Howard, A.M. Effect of virtual reality on upper extremity function in children with cerebral palsy: A meta-analysis. Pediatr. Phys. Ther. Off. Publ. Sect. Pediatr. Am. Phys. Ther. Assoc. 2014, 26, 289–300. [Google Scholar] [CrossRef]
- Meyns, P.; Roman de Mettelinge, T.; van der Spank, J.; Coussens, M.; Van Waelvelde, H. Motivation in pediatric motor rehabilitation: A systematic search of the literature using the self-determination theory as a conceptual framework. Dev. Neurorehabilit. 2018, 21, 371–390. [Google Scholar] [CrossRef]
- You, S.H.; Jang, S.H.; Kim, Y.H.; Kwon, Y.H.; Barrow, I.; Hallett, M. Cortical reorganization induced by virtual reality therapy in a child with hemiparetic cerebral palsy. Dev. Med. Child Neurol. 2005, 47, 628–635. [Google Scholar] [CrossRef]
- Adamovich, S.V.; Fluet, G.G.; Tunik, E.; Merians, A.S. Sensorimotor training in virtual reality: A review. NeuroRehabilitation 2009, 25, 29–44. [Google Scholar] [CrossRef]
- Mulita, F.; Verras, G.I.; Anagnostopoulos, C.N.; Kotis, K. A Smarter Health through the Internet of Surgical Things. Sensors 2022, 22, 4577. [Google Scholar] [CrossRef] [PubMed]
- Fandim, J.V.; Saragiotto, B.T.; Porfírio, G.J.M.; Santana, R.F. Effectiveness of virtual reality in children and young adults with cerebral palsy: A systematic review of randomized controlled trial. Braz. J. Phys. Ther. 2021, 25, 369–386. [Google Scholar] [CrossRef]
| N | Study ID | Study Arms, n (%) | Site | Study Design | Age, (Mean ± SD) y | Boys, n (%) | Duration of Session in Min (Frequency per Week) | Follow-up Duration (Weeks) | Arms Description, n (%) | Types of Cerebral Palsy, n (%) | MACS Level, n (%) | GMFCS Level, n (%) | Drop-Out Rate, n (%) | Inclusion Criteria | Primary Endpoints | Conclusion |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Abo-Zaid et al., 2021 | Exergaming, 20 (33.33%) | Egypt | RCT (NCT04533789) | 10.3 ± 1.17 | 7 (35%) | 60 | 16 | Nintendo Wii | Hemiplegic | - | Between one and Two | 3 (13%) | 1. Unilateral CP children 2. From April 2017 to April 2019 3. Diagnosis based on careful clinical assessment by a physiotherapist | 1. Swing % 2. Support % 3. Stride Length 4. Step Length 5. Cadence | “Wii Sports Training and Task-oriented Training have a significant effect on gait in children with unilateral cerebral palsy in favor of Task-oriented Training group” |
| 9.9 ± 0.91 | 6 (30%) | 30 (Triple) | Neurodevelopmental control | 3 (13%) | ||||||||||||
| Control, 20 (33.33%) | 10.15 ± 1.09 | 4 (20%) | 30 (Triple) | Nintendo Wii and Neurodevelopmental control | 3 (13%) | |||||||||||
| 2 | Akhutina et al., 2003 | Exergaming, 12 (57.14%) | Russia and Finland | RCT | 7 and 14 y | 7 (58%) | 60 (Twice) | Four | Super Scape VRT 3-D construction packages | - | - | - | 0 | 1. Between 7 and 14y 2. Children with Cerebral palsy 3. Given non-specific rehabilitative training | 1. Difference between pre- and post-training scores | “VE-based spatial training is effective for children with complex disabilities, particularly when combined with training that remediates cognitive weaknesses” |
| Control, 9 (42.86%) | 5 (56%) | Two out of the nine children used wheelchairs, the others walked by themselves | 0 | |||||||||||||
| 3 | Aran et al., 2019 | Exergaming, 45 (50%) | Turkey | RCT | 11.18 ± 3.37 | 24 (53.33) | 45 (Twice) | 10 | Exergaming and Traditional occupational therapy | Hemiplegic | a. I, 14 (31.11%) b. II, 26 (57.78%) c. III, 5 (11.11%) | a. I, 28 (62.22%) b. II, 17 (37.78%) | 0 | 1. Children with HCP 2. Between the years 2015 and 2017 3. Aged between 7 and 12 y 4. Level I or II in GMFCS 5. Level I, II, or III of MACS | 1. DOTCA-Ch scores | “Using virtual reality applications in cognitive rehabilitation was recommended to improve spatial perception, praxis, visuomotor construction and thinking operations in children with cerebral palsy” |
| Control, 45 (50%) | 11.06 ± 3.24 | 23 (51.11%) | (Twice) | Traditional occupational therapy | a. I, 12 (26.67%) b. II, 29 (64.44%) c. III, 4 (8.89%) | a. I, 31 (68.89%) b. II, 14 (31.11%) | 0 | |||||||||
| 4 | Arnoni et al., 2019 | Exergaming, 7 (47.67%) | Brazil | Pilot (RCT) | 10 ± 3.36 | 7 (100%) | 45 (Twice) | Eight | Exergaming and Traditional occupational therapy | Mild Spastic Hemiplegic | Between Levels One and Two | a. I, 6 (85.71%) b. II, 1 (14.29%) | 0 | 1. Between October 2013 and October 2014 2. Aged between five and 14 years 3. Levels I and II of the GMFCS 4. Have signed an informed consent | Variables of body sway: 1. Total displacement (cm) 2. Mean Velocity (cm/s) | “Intervention using an active video game is a promising tool that can improve the gross motor function of children with CP, GMFCS I-I” |
| Control, 8 (53.33%) | 9.39 ± 2.79 | 6 (75%) | - | Traditional occupational therapy | a. I, 6 (75%) b. II, 2 (25%) | 0 | ||||||||||
| 5 | Avcil et al., 2020 | Exergaming, 15 (50%) | Turkey | RCT (NCT03078998) | 10.93 ± 4.09 | 8 (53.33%) | (Triple) | Eight | VGBT using Nintendo® Wii and LMC games | 1. Spastic, 12 (80%) 2. Hemiplegia, 8 (53.33%) 3. Diplegia, 4 (26.67%) 4. Dyskinetic, 3 (20%) | a. 1, 2 (13.3%) b. 2, 9 (60%) c. 3, 4 (26.7%) d. 0 | a. 1, 8 (53.3%) b. 2, 4 (26.7%) c. 3, 1 (6.7%) d. 4, 2 (13.3%) | 0 | 1. A diagnosis of Cerebral Palsy 2. The ability to cooperate with exercise or measurement | 1. Minnesota Manual Dexterity Test score 2. Durouz Hand Index score | “VGBT using Nintendo®Wii and LMC games had slightly superior effects on manual dexterity in patients with CP while compared with NDT-based upper extremity rehabilitation. Furthermore, the effects of both treatment programs on grip strengths and functional ability were similar and beneficial” |
| Control, 15 (50%) | 11.07 ± 3.24 | 9 (60%) | - | Neuro-developmental therapy | 1. Spastic, 11 (73.3%) 2. Hemiplegia, 9 (60%) 3. Diplegia, 2 (13.33%) 4. Dyskinetic, 4 (26.7%) | a. 1, 3 (20%) b. 2, 8 (53.3%) c. 3, 2 (13.3%) d. 4, 2 (13.3%) | a. 1, 3 (20%) b. 2, 2 (13.3%) c. 3, 6 (40%) d. 4, 4 (26.7%) | 0 | ||||||||
| 6 | Acar et al., 2016 | Exergaming, 15 (50%) | Turkey | Pilot (RCT) | 9.53 ± 3.04 | - | 45 (Twice) | Six | A neuro-developmental treatment and Nintendo Wii | Spastic | 2 (SD 0.75) | a. I, 6 (40%) b. II, 9 (60%) | 0 | 1. Aged between 6 and 15 y 2. Levels 1–3 of the MACS 3. Levels I and II of the GMFCS 4. Ability to grasp and release an object | 1. QUEST total score 2. JTHFT (s) 3. WeFIM (score) | “Our results showed that neuro-developmental treatment is effective for improving hand functions in hemiplegic cerebral palsy. To provide an enjoyable, motivational, safe, and effective rehabilitation program, the Nin-tendo® Wii may be used in addition to neurodevelopmental treatment” |
| Control, 15 (50%) | 9.73 ± 2.86 | - | A neuro-developmental treatment | 2 (SD 0.75) | a. I, 6 (40%) b. II, 9 (60%) | 0 | ||||||||||
| 7 | Alsaif et al., 2015 | Exergaming, 20 (50%) | Saudi Arabia | RCT | 6 to 10 | - | 20 (Seven) | 12 | Nintendo Wii Fit games | Spastic diplegia | - | Level 3 | 0 | 1. Children diagnosed with CP spastic diplegia 2. Age ranged from 6–10 years old 3. Level 3 on the GMFCS 4. Lower-limb muscle power no less than grade 4 | 1. Balance score 2. BOTMP 5:6 3. 1-min walk test | “Using motion interactive games in-home rehabilitation is feasible for children with cerebral palsy” |
| Control, 20 (50%) | - | - | No training Control | 0 | ||||||||||||
| 8 | Bedair et al., 2016 | Exergaming, 20 (50%) | Egypt | RCT | 7.05 ± 0.99 | 12 (60%) | 30 (Triple) | 16 | VRGTP and selected physical therapy program | Spastic hemiplegic | - | - | 0 | 1. Diagnosed as acquired spastic hemiplegic children 2. Age between 5–10 y 3. They all have the muscle tone of grade 1 or 2 4. Level of disability I–IV in the MACS | 1. Visual-motor skills of PDMS-2 2. Object manipulation 3. Abilhand kids questionnaire | “Significant improvement of object manipulation, visual motor skills and upper limb functions in study group post-treatment are related to the active participation of children in the simulating environment, driven their active motivation and enhance their participation through self-competition activities. VRG can enhance active participation of children with motor deficits in the majority of upper limb activities through consideration of child personality and changing of environmental factors” |
| Control, 20 (50%) | 7.25 ± 0.96 | 11 (55%) | 60 (Triple) | Selected physical therapy program | 0 | |||||||||||
| 9 | Chang et al., 2020 | Exergaming, 10 (58.83%) | South Korea | Retrospective cohort study | 6.08 ±1.77 | 7 (70%) | VR 20 + COT 10 (Twice) | Eight | VR-based rehabilitation with RAPAEL Smart Kids and video games and COT | - | 1.6 (SD 0.7) | 1.1 (SD 0.32) | 0 | 1. Children with CP 2. Age between 5-10y 3. Were selected and received two treatments | 1. QUEST scores 2. PEDI domains | “Our results suggest that VR-based rehabilitation combined with COT may improve the upper extremity functions and decrease caregiver burden among children with CP” |
| Control, 7 (41.17%) | 4.88 ±1.15 | 5 (71.43%) | 30 (Twice) | Conventional occupational therapy | 1.42 (SD 0.78) | 2.28 (SD 1.38) | 0 | |||||||||
| 10 | Chen et al., 2011 | Exergaming, 13 (48.15%) | Taiwan | RCT | 8.7 ± 2.1 | 9 (69.23%) | 40 (Triple) | 12 | Home-based virtual cyclic training with games | 1. Spastic diplegic, 10 (76.92%) 2. Spastic hemiplegic, 3 (23.08%) | - | a. I, 10 (76.92%) b. II, 3 (23.08%) | 2 (12.5%) | 1. Diagnosed CP with GMFS levels I–II 2. Age of 6–12y 3. Ability to walk independently 4. Ability to undergo a motor function and isokinetic muscle test | 1. GMFM-66 scores | “Analytical findings suggest that the muscle strengthening program is more specific in enhancing bone density for children with CP than general physical activity. Thus, the proposed 12-week hVCT protocol is an effective and efficient strategy for improving lower limb aBMD in these children” |
| Control, 14 (51.85%) | 8.6 ± 2.2 | 5 (35.71%) | 30–40 (Triple) | Usual and general physical activity | 1. Spastic diplegic, 9 (64.29%) 2. Spastic hemiplegic, 5 (35.71%) | a. I, 11 (78.57%) b. II, 3 (21.43%) | 1 (6.25%) | |||||||||
| 11 | Chen et al., 2012 | Exergaming, 13 (46.43%) | Taiwan | RCT | 8.7 ± 2.1 | 9 (69.23%) | 40 (Triple) | 12 | Home-based virtual cyclic training with games | 1. Spastic diplegic, 10 (76.92%) 2. Spastic hemiplegic, 3 (23.08%) | - | a. I, 10 (76.92%) b. II, 3 (23.08%) | 0 | 1. Children with spastic CP 2. Diagnosis with CP with GMFCS levels I–II 3. Age 6–12 y 4. Ability to walk independently 5. Ability to undergo a motor function and isokinetic muscle test | 1. BOTMP scores 2. Muscle strength (peak torque, Nm/kg) | “The protocol obtains larger gains in the knee flexor than in the knee extensor at different angular velocities. The study findings will help clinicians to provide more effective and efficient strategies for muscle strength training in children with CP” |
| Control, 15 (53.57%) | 8.5 ± 2.2 | 10 (66.67%) | - | Usual and general physical activity | 1. Spastic diplegic, 10 (66.67%) 2. Spastic hemiplegic, 5 (33.33%) | a. I, 12 (80%) b. II, 3 (20%) | 0 | |||||||||
| 12 | Chiu et al., 2014 | Exergaming, 32 (51.61%) | Taiwan and Australia | RCT | 9.4 ± 1.9 | 15 (47%) | - | 12 | Home-based Wii Sports Resort training | Hemiplegic | a. I–III, 21(66) b. IV–V, 11(34) | a. I–III, 26 (81%) b. IV–V, 6 (19%) | 2 (6.25%) | 1. Children with spastic CP 2. Age above and below 9.5 years | 1. NHPT score 2. JTHFT score | “Wii™ training did not improve coordination, strength, or hand function. Beyond the intervention, carers perceived that the children used their hands more” |
| Control, 30 (48.39%) | 9.5 ± 1.9 | 13 (43%) | - | Usual therapy only | a. I–III, 21(70) b. IV–V, 9(30) | a. I–III, 26 (87%) b. IV–V, 4 (13%) | 3 (10%) | |||||||||
| 13 | Cho et al., 2016 | Exergaming, 9 (50%) | South Korea | RCT | 10.2 ± 3.4 | - | 30 (Triple) | Eight | Virtual reality with games and Tridmail training | Spastic | - | 1. One, 3 (33.33%) 2. Two, 1 (11.11%) 3. Three, 5 (55.56%) | 0 | 1. Diagnosis of spastic cerebral palsy 2. Age 4–16 y 3. Cognitive abilities enabling communication 4. GMFS level I-III | 1. PBS 2. 10-min WT score 3. 2-min walk test score | “In conclusion, VRTT programs are effective for improving gait, balance, muscular strength, and gross motor function in children with CP” |
| Control, 9 (50%) | 9.4 ± 3.8 | 30 (Triple) | Tridmail training | 1. One, 3 (33.33%) 2. Two, 2 (22.22%) 3. Three, 4 (44.44%) | 0 | |||||||||||
| 14 | Choi et al., 2020 | Exergaming, 40 (51.28%) | South Korea | RCT | 4.33 ± 2.3 | 19 (47%) | 30 | Four | Virtual reality with games and Conventional rehabilitation | - | a. I and II, 13 (32.5%) b. III and IV, 27 (67.5%) | - | 0 | 1. Children with CP or other acquired brain injury of at least 12 m 2. Aged 3 to 18 y 3. Children with upper-limb dysfunction 4. MACS levels I to IV and HFCS levels 4 to 7 | 1. MA-2 scale scores 2. ULPRS score 3. PEDI scores | “The virtual reality rehabilitation system used in this study, which consists of wearable inertial sensors and offers intensive, interactive, and repetitive motor training, is effective in children with brain injury” |
| Control, 38 (48.72%) | 5.67 ± 2.37 | 19 (50%) | 60 | Conventional rehabilitation | a. I and II, 16 (42.1%) b. III and IV, 22 (57.9%) | 0 | ||||||||||
| 15 | Choi et al., 2023 | Exergaming, 15 (42.86%) | Italy | RCT (KCT0003172) | 8.1 ± 3.2 | 8 (53%) | 30 | Six | Training at home using the VR-enhanced program and occupational therapy | - | a. II, 8 (53%) b. III, 3 (20%) c. IV, 4 (27%) | - | 2 (11.67%) | 1. Children with CP or other acquired brain injury of at least 12 m 2. Aged 4–17 y 3. Children with upper-limb dysfunction 4. MACS levels I to IV and HFCS levels 4 to 7 | 1. MA-2 scale scores 2. ULPRS score 3. PEDI scores | “Home-based VR training though it had limited impact on improving upper limb function, could help improve social cognitive function, movement pattern, and efficiency in children with brain injury and could be an effective means of extending clinical therapy to the home” |
| Control, 20 (57.14%) | 7.3 ± 2.6 | 10 (50%) | - | Occupational therapy | a. II, 10 (53%) b. III, 5 (25%) c. IV, 5 (25%) | 0 | ||||||||||
| 16 | Decavele et al., 2020 | Exergaming, 27 (50%) | Belgium | RCT | 6 to 15 | - | 45 (Twice) | 12 | Regular Physical therapy and gaming | Spastic | - | - | 4 (14.8%) | 1. Bilateral spastic CP 2. GMFCS level III–IV 3. Age between 6 and 15 y 4. Routinely receiving PT at an intensity of minimally twice a week | 1. PBS score 2. GMFS-88 score 3. DMQ score | “A combined approach of regular PT and rehabilitation specific gaming showed significant effects on individually defined therapy goals, dynamic sitting balance, and standing exercises. However, the lack of persistent effect indicates that continuous individual goal-oriented PT with the addition of gaming is needed” |
| Control, 23 (50%) | - | Regular Physical therapy | 3 (13%) | |||||||||||||
| 17 | El-Shamy et al., 2018 | Exergaming, 20 (50%) | Egypt | RCT | 9.5 ± 1.2 | 12 (60%) | 40 (Triple) | 12 | Wii training and usual care | Spastic Hemiplegic | a. I, 8 (40%) b. II, 9 (45%) | - | 0 | 1. Children with CP 2. Age was 8–12 y 3. Scored I–III on MACS 4. Did not have Musculoskeletal disorders | 1. Modified Ashworth scale scores 2. Spasticity scores 3. PDMS-2 scores | “Wii training plus usual care decreases spasticity and increases grip strength and hand function in children with hemiplegic cerebral palsy” |
| Control, 20 (50%) | 9.8 ± 1.4 | 14 (70%) | 60 (Triple) | Usual care only | a. I, 7 (35%) b. II, 9 (45%) | 0 | ||||||||||
| 18 | Gercek et al., 2021 | Exergaming, 9 (47.37%) | Turkey | RCT | 8.22 ± 1.71 | 7 (77.78%) | 60 (Triple) | 12 | Correct golf swing during the virtual game | Spastic hemiplegic | a. I, 3 (33.33%) b. II, 6 (66.67%) | - | 0 | 1. Children had CP at GMFCS level one or two 2. Age 6–12 y 3. With sufficient hand function to hold the golf club | 1. GMFM-88 score 2. 6 min Walk(m) score | “Both virtual and traditional golf training applied for 12 weeks on children with unilateral cerebral palsy improved lower extremity functions and physical performance. The use of virtual and traditional training as complementary applications to reduce motor problems in children with cerebral palsy could enhance the sustainability of this type of training because of its edutainment features. Virtual golf has an important advantage over traditional golf in that (a) the latter can be expensive and inaccessible for people with disabilities, and (b) making virtual golf a safer activity” |
| Control, 10 (52.63%) | 8.5 ± 2.5 | 7 (70%) | Correct golf swing | a. I, 3 (30%) b. II, 7 (70%) | 0 | |||||||||||
| 19 | Gatica-Rojas et al., 2017 | Exergaming, 16 (50%) | Australia | RCT | 10.2 ± 3.1 | 10 (62.50%) | 30 (Triple) | 10 | Nintendo Wii balance and SPT | Hemiplegia, 4 (44.44%) | - | a. I, 3 (37.50%) b. ii, 5 (62.5%) | 0 | 1. CP type SHE and SDI 2. Level I or II of GMFCS 3. Males and females aged between 7 and 14y | 1. COP for open and closed eyes 2. Mean velocities (cm/s) | “A systematic exercise program like Wii therapy using the Nintendo Wii balance board device can be considered to improve the standing balance in patients with CP, specifically in the SHE type. This program is easy to transfer to physiotherapists and rehabilitation centers” |
| Control, 16 (50%) | 11.2 ± 3.6 | 9 (56.25%) | 40 (Triple) | Standard physiotherapy | Hemiplegia, 5 (55.55%) | a. I, 3 (33.33%) b. II, 6 (66.66%) | 0 | |||||||||
| 20 | Okmin et al., 2019 | Exergaming, 21 (51.22%) | Turkey | RCT | 8.8 ± 2.5 | 14 (66.67%) | 60 (Triple) | Four | VR and (Neurophysiological, conventional, and occupational therapy) | 1. Spastic, 20 (95.5%) 2. Dyskinetic athetoid, 1 (4.8%) | - | - | 0 | 1. Age between 5 and 15 y 2. Being able to cooperate and being motivated 3. Having sitting balance and normal UE passive | 1. Bimanual fine motor function score 2. GMFCS score | “Our study results indicate that VR therapy is a useful treatment method that can be used in the rehabilitation of CP with improved motor function. The addition of this method to conventional rehabilitation techniques may have a significant impact on treatment success” |
| Control, 20 (48.78%) | 8.2 ± 1.8 | 14 (70%) | Neurophysiological, conventional, and occupational therapy | 1. Spastic, 19 (95%) 3. Mixed, 1 (5%) | 0 | |||||||||||
| 21 | James et al., 2015 | Exergaming, 47 (51.09%) | Australia | RCT | 11.67 ± 2.33 | 26 (51%) | 30 (Hexable) | 20 | Mitii (a web camera using green tracking bands worn on the hands, knee, or head)and occupational therapy | Hemiplegia, 28 (55%) | a. I, 11 (21.6%) b. II, 39 (76.5%) c. III, 1 (2%) | 1. I, 20 (39.2%) 2. II, 31 (60.8%) | 4 (7.8%) | 1. Children with spastic type UCP 2. MACS 1 and 3 3. GMFCS 1 and 2 4. Aged 8 to 18y 5. Internet access at home | 1. COPM score 2. MUUL score 3. Test of Visual Perceptual Skills score | “ Mitii delivers individualized, web-based therapy at home and has the potential to increase the therapy dose. Mitii can be considered as an option to enhance occupational performance and visual perception for children with UCP” |
| Control, 45 (48.91%) | 11.83 ± 2.42 | 25 (50%) | Occupational therapy | Hemiplegia, 20 (40%) | a. I, 13 (26%) b. II, 37 (74%) c. III, 0 | 1. I, 25 (50%) 2. II, 25 (50%) | 5 (10%) | |||||||||
| 22 | Jannink et al., 2008 | Exergaming, 5 (50%) | Netherlands | Pilot(RCT) | 12.32 ± 3.18 | 5 (100%) | 30 (Twice) | Six | Low-Cost Video Game and physiotherapy | 1. Spastic tetraplegia, 4 (80%) 2. Spastic diplegia, 1 (20%) | Two, Three, and Four | One and Four | 0 | 1. Age between 7 and 16 y 2. Have a diagnosis of CP 3. Can understand the Dutch language 4. Can stretch and bend the shoulder and elbow of their affected arm | 1. Melbourne score assessment | “In conclusion, it can be said that the Eye Toy is a motivational training tool for the training of children with CP and has the potential to improve upper extremity function” |
| Control, 5 (50%) | 11.88 ± 3.47 | 4 (80%) | Physiotherapy | 1. Spastic tetraplegia, 3 (60%) 2. Spastic Hemiplegia, 1 (20%) 3. Spastic diplegia, 1 (20%) | Two, Three, and Four | One, Three, and Four | 0 | |||||||||
| 23 | Jha et al., 2021 | Exergaming, 19 (50%) | India | RCT | 8.94 ± 1.92 | 14 (74%) | 60 (Pentable) | Six | Combined virtual gaming and physiotherapy session | Spastic | a. 1, 12 (63%) b. 2, 7 (33%) | a. 2, 17 (89%) b. 3, 2 (11%) | 1 (5.3%) | 1. Children with bilateral spastic CP 2. Aged 6–12y 3. With an ability to understand simple verbal instructions 4. GMFCS level II–III 5. MACS level I–II | 1. PBS score 2. GMFM-88 score 3. WeFIM score | “Combined virtual reality gaming and physiotherapy are not superior over physiotherapy alone in improving the gross motor performance and daily functioning among children with bilateral spastic cerebral palsy. Virtual gaming, along with physiotherapy, appears to be beneficial in their balance capacity, warranting further trials to investigate the same in children with GMFCS level III” |
| Control, 19 (50%) | 8.72 ± 1.68 | 9 (47%) | 30 (Pentable) | Physiotherapy session | a. 1, 10 (53%) b. 2, 9 (47%) | a. 2, 16 (84%) b. 3, 3 (16%) | 1 (5.3%) | |||||||||
| 24 | Jung et al., 2020 | Exergaming, 5 (50%) | South Korea | Pilot (RCT) | 12.8 ± 1.6 | 3 (60%) | 80 (Triple) | Six | Kinect Video Game Training and Conventional therapy | Spastic diplegia | a. 1, 2 (40%) b. 2, 3 (60%) | a. 1, 2 (40%) b. 2, 3 (60%) | 0 | 1. Adolescents with CP 2. Aged 11–17 y 3. Levels I and II of the GFMCS 4. Levels I and II of the MACS | 1. Selective control assessment score 2. PBS score | “KVG training might be an effective intervention for the rehabilitation of adolescents with spastic diplegia CP” |
| Control, 5 (50%) | 12 ± 2.53 | 2 (40%) | 40 (Triple) | Conventional therapy | a. 1, 3 (60%) b. 2, 2 (40%) | a. 1, 3 (60%) b. 2, 2 (40%) | 0 | |||||||||
| 25 | Jung et al., 2022 | Exergaming, 10 (58.83%) | South Korea | RCT | 9.34 ± 2.11 | 7 (70%) | 30 (Twice) | Eight | HRS sessions with VR training and conventional physiotherapy | Spastic | - | a. I. 6 (60%) b. II. 1 (10%) c. III. 1 (10%) d. IV. 2 (20%) | 0 | 1. Diagnosed as spastic CP 2. Aged between 5 and 18 y 3. Level I-IV of the GFMCS 4. Able to sit astride on a saddle | 1. GMFM-88 score 2. GMFM-66 score | “HRS with VR may be an effective adjunctive therapeutic approach for the rehabilitation of children with CP” |
| Control, 7 (41.17%) | 9.1 ± 2.41 | 4 (57.14%) | Conventional physiotherapy | a. I. 4 (57.14%) b. II. 1 (14.29%) c. III. 0 d. IV. 2 (28.57%) | 0 | |||||||||||
| 26 | Piovesana et al., 2016 | Exergaming, 51 (50.5%) | Australia | RCT (ACTRN12611001174976) | 11.63 ± 2.30 | 26 (51%) | 30 (Hexable) | 20 | Mitii (a web camera using green tracking bands worn on the hands, knee, or head)and occupational therapy | Hemiplegia, 28 (55%) | a. I, 11 (21.6%) b. II, 39 (76.5%) c. III, 1 (2%) | a. I, 20 (39.2%) b. II, 31 (60.8%) | 4 (7.8%) | 1. Children with UCP 2. GMFCS-E&R I or II 3. MACS level I–II and III 4. Aged 8–18y 5. Received upper-limb or lower-limb surgery | 1. BRIEF scores 2. Executive functioning scores | “In a large RCT, MitiiTM did not lead to significant improvements on measures of EF or parent ratings of EF performance in children with UCP” |
| Control, 50 (49.5%) | 11.86 ± 2.45 | 25 (50%) | Occupational therapy | Hemiplegia, 20 (40%) | a. I, 13 (26%) b. II, 37 (74%) c. III, 0 | a. I, 25(50%) b. II, 25(50%) | 6 (12%) | |||||||||
| 27 | Pourazar et al., 2017 | Exergaming, 15 (50%) | Iran | RCT | 10.9 ± 0.87 | 15 (100%) | 25 (Triple) | Four | Xbox 360 Kinect as a therapeutic device for VR intervention | Spastic hemoplegic | a. I, 9 (60%) b. II, 1 (6.67%) | - | 0 | 1. Between the ages of 7 and 12 y 2. Scores range from 1 to 3 in GFMCS 3. MACS level I–II 4. Able to walk without an assistive device | 1. Simple Reaction Time 2. Discriminative Reaction Time | “This paper proposes VR as a promising tool into the rehabilitation process for improving reaction time in children with cerebral palsy” |
| Control, 15 (50%) | 11.5 ± 0.52 | 15 (100%) | Common therapy programs by the school during the intervention | a. I, 8 (53.33%) b. II, 2 (13.33%) | 0 | |||||||||||
| 28 | Pourazar et al., 2019 | Exergaming, 10 (50%) | Iran | Pilot (RCT) | 9.2 ± 1.4 | - | (Triple) | Six | Xbox 360 Kinect as a therapeutic device for video game-based training | Spastic hemiplegic | a. I, 7 (70%) b. II, 3 (30%) | a. I, 5 (50%) b. II, 2 (20%) c. III, 3 (30%) | 0 | 1. Girls ranging from 7 to 12 y 2. Spastic Hemiplegic Cerebral Palsy 3. MACS level I–II 4. Scores range from 1 to 3 in GMFCS | 1. One-way covariance test scores | “This paper proposes that video game-based training can successfully guide children with cerebral palsy to improve their balance ability. This virtual system is therefore an interesting tool in the therapies related to children with cerebral palsy” |
| Control, 10 (50%) | 9.6 ± 1.5 | Typical physical activity under parental supervision at home | a. I, 9 (90%) b. II, 1 (10%) | a. I, 6 (60%) b. II, 3 (30%) c. III, 1 (10%) | 0 | |||||||||||
| 29 | Rosenbaum et al., 2012 | Exergaming, 20 (50%) | Denmark | RCT | 11.1 ± 2.1 | 14 (70%) | 30 (Triple) | 20 | Internet-based home training system ‘Move It to Improve It’ (MiTii) | Spastic | - | I–II and III | 0 | 1. Diagnosed as spastic CP 2. Level I-IV of the GFMCS 3. Able to sit astride on a saddle | 1. Kinematics of the movements | “These findings suggest that sense of agency may be altered and that training in the sense of agency may help to increase the outcome of training programs in children with CP” |
| Control, 20 (50%) | 12 ± 2.6 | 12 (60%) | Continued their regular daily activities | 0 | ||||||||||||
| 30 | Rostami et al., 2012 | Exergaming, 8 (25%) | Iran | Pilot(RCT) | 7.73 ± 0.795 | 3 (37.5%) | 90 (Triple) | Four | VR with games | Spastic hemiparesis | - | - | 0 | 1. Age range 6 y 2 mo to 11 y 8 mo 2. With spastic hemiparetic CP 3. At least 20◦wrist and 10◦active finger extension from full flexion | 1. Quality of movement score 2. Speed and dexterity score | “Modified constraint-induced movement therapy in a virtual environment could be a promising rehabilitation procedure to enhance the benefits of both virtual reality and constraint-induced therapy techniques” |
| mCIMT, 8 (25%) | 8.29 ± 1.2 | 4 (50%) | Modified Constraint-Induced Movement Therapy | 0 | ||||||||||||
| Exergaming and mCIMT, 8 (25%) | 8.5 ± 1.01 | 4 (50%) | VR and mCIMT | 0 | ||||||||||||
| Control, 8 (25%) | 8.46 ± 1.61 | 3 (37.5%) | Regular routines of treatment programs that had been prescribed before enrolment in the study | 0 | ||||||||||||
| 31 | Mitchell et al., 2016 | Exergaming, 51 (50.5%) | Australia | RCT | 11.25 ± 2.33 | 26 (51%) | 30 (Hexable) | 20 | Physical activity games were interspersed with upper-limb and visual perceptual games | - | a. I, 11 (22%) b. II, 39 (76%) c. III, 1 (2%) | a. I, 21 (41%) b. II, 30 (59%) | 4 (7.8%) | 1. Children and adolescents aged 8 to 17 y 2. With unilateral CP 3. Levels one and two in GFMCS 4. Levels one and three in MACS | 1. Physical activity capacity scores 2. Physical activity performance scores | “Training was effective at increasing functional strength and walking endurance in independently ambulant children with unilateral CP. This did not translate into improvements in activity performance” |
| Control, 50 (49.5%) | 11.33 ± 2.5 | 26 (52%) | Occupational physiotherapy | a. I, 13 (26%) b. II, 37 (74%) c. III, 0 | a. I, 25 (50%) b. II, 25 (50%) | 7 (13.72%) | ||||||||||
| 32 | Park et al., 2021 | Exergaming, 10 (50%) | South Korea | RCT | 14.3 ± 4.2 | 3 (30%) | 60 (Twice) | Four | Balance training in the sitting position using a VR training program | 1. Diplegia, 5 (50%) 2. Quadriplegia, 5 (50%) | - | - | 0 | 1. Children aged 6–18 y 2. Diagnosed with spastic CP 3. Had spastic quadriplegia and 10 had spastic paraplegias 4. Children with no vision and hearing problems 5. With an appropriate cognitive level | 1. Total path length (cm) 2. Velocity (cm/s) | “Posture control training in the sitting position using a VR training program was found to be more effective in improving the sitting balance and trunk stability of children with CP” |
| Control, 10 (50%) | 14.1 ± 4.3 | 4 (40%) | 40 (Twice) | Arm reach training in the sitting position | 1. Diplegia, 5 (50%) 2. Quadriplegia, 5 (50%) | 0 | ||||||||||
| 33 | Pin et al., 2019 | Exergaming, 9 (50%) | UK | Pilot (RCT) (NCT02975804) | 8.92 (2.25) | 5 (56%) | 20 (Pentable) | 12 | Interactive computer play training in sitting four times per a week and (muscle strength physiotherapy program) | Bilateral spastic CP | - | a. III, 8 (88.88%) b. IV, 1 (11.11%) | 0 | 1. Children with moderate cerebral palsy 2. GMFCS level III or IV 3. Were aged between 6 and 14 y 4. Were able to follow instructions | 1. GMFM-66 score | “The intervention protocol of a six-week interactive computer play training was feasible and safe for children with moderate cerebral palsy in special school settings. Future studies with larger sample sizes or using single-subject designs are recommended” |
| Control, 9 (50%) | 9.59 (1.87) | 6 (67%) | - | Muscle strength physiotherapy program | a. III, 8 (88.88%) b. IV, 1 (11.11%) | 0 | ||||||||||
| 34 | Preston et al., 2015 | Exergaming, 8 (53.33%) | UK | RCT (ISRCTN26206379) | 9.41 ± 2.41 | 4 (50%) | 30 | 12 | The computer-assisted arm rehabilitation gaming technology | Spastic | a. II, 2 (25%) b. III, 3 (37.5%) c. IV, 3 (37.5%) | - | 0 | 1. Children aged five to 12 y 2. with a diagnosis of cerebral palsy who were to receive botulinum toxin 3. MACS levels one and two 4. Arm capability sufficient to manipulate the handle of the robotic arm and vision | 1. ABILHAND-kids function scores 2. Canadian Occupational Performance Measure scores | “This study suggests that computer-assisted arm rehabilitation gaming does not benefit arm function, but a Type II error cannot be ruled out” |
| Control, 7 (46.67%) | 8.58 ± 2.58 | 5 (71.43%) | Receive a matching visit for delivery or collection of the device | a. II, 1 (14.29%) b. III, 2 (28.57%) c. IV, 4 (57.14%) | 0 | |||||||||||
| 35 | Reid et al., 2006 | Exergaming, 19 (61.29%) | Canada | Pilot(RCT) | 9.75 ± 1.55 | 12 (63.16%) | 90 (Once) | Eight | Sat on a bench or in a wheelchair viewing a large TV screen in a well-demarcated area | - | - | - | 0 | 1. Children with CP 2. Aged between 8 and 10 y | 1. COPM-P score 2. COPM-S score 3. QUEST scores | “These findings will be discussed to suggest that VR remains a viable rehabilitation tool and future research needs to be done where strategies for control group attention are devised as well as its use in reaction therapy” |
| Control, 12 (28.71%) | 9.23 ± 1.19 | 8 (66.67%) | The standard of care which is occupational therapy or physical therapy | 0 | ||||||||||||
| 36 | Sahin et al., 2019 | Exergaming, 30 (50%) | Turkey | RCT | 10.5 ± 3.62 | 20 (66.67%) | 45 (Twice) | Eight | Box, Wii, Superkick, and Jet Run | Spastic | - | - | 0 | 1. Aged between 7 and 16 y 2. Having a>24 score of MMSE for children 3. MACS levels one and two 4. Having been classified in levels I–II of MACS 5. levels I–III of the GMFCS 6. Able to follow and accept verbal instructions | 1. BOTMP-SF scores 2. WeeFIM scores | “The Kinect-based VR intervention approach is important to improving motor functions and independence in daily activities of children with USCP” |
| Control, 30 (50%) | 10.06 ± 3.24 | 17 (56.67%) | Traditional occupational therapy | 0 | ||||||||||||
| 37 | Sajan et al., 2016 | Exergaming, 10 (50%) | India | RCT (CTRI/2011/11/002137) | 10.6 ± 3.78 | 5 (50%) | 45 (Hexable) | Three | Wii-based interactive video games and conventional therapy | 1. Spastic, 7 (70%) 2. Triplegia, 1 (10%) 3. Quadriplegia, 2 (20%) | - | a. I, 1 (10%) b. II, 2 (20%) c. III, 6 (60%) d. IV, 1 (10%) e. VI, 0 | 1 (10%) | 1. Children with CP 2. Children aged 5–20 y 3. With sufficient balance to play Wii games in the sitting or standing position 4. Children with a history of serious health problems | 1. Sway velocity for eyes (mm/s) 2. QUEST scores 3. TVPS scores | “Wii-based IVG may be offered as an effective supplement to conventional therapy in the rehabilitation of children with CP” |
| Control, 10 (50%) | 12.4 ± 4.93 | 6 (60%) | - | A goal-directed, comprehensive rehabilitation program that involved a team of Various specialties | 1. Spastic,5 (50%) 2. Diplegia, 4 (40%) 3. Quadriplegia, 1 (10%) | a. I, 0 b. II, 1 (10%) c. III, 7 (70%) d. IV, 2 (20%) e. VI, 0 | 1 (10%) | |||||||||
| 38 | Sharan et al., 2012 | Exergaming, 14 (48.28%) | India | Pilot (RCT) | 8.88 ± 3.23 | - | - | Three | (Nintendo Wii Sports and Wii Fit) and CR | - | - | - | 0 | 1. Diagnosed as spastic CP 2. Level I–IV of the GFMCS 3. Able to sit astride on a saddle | 1. PBS score 2. MACS score | “To the author’s best knowledge, this is the first study on using VR-based therapy for the postoperative rehabilitation of children with CP which needs further elaboration with larger sample size” |
| Control, 15 (51.72%) | 10.38 ± 4.41 | Conventional rehabilitation modalities | 0 | |||||||||||||
| 39 | Tarakci et al., 2016 | Exergaming, 15 (50%) | Turkey | Pilot RCT | 10.46 ± 2.69 | 10 (66.67%) | 50 (Twice) | 12 | (Wii-Fit balance-based video game training) and NDT | 1. Hemiplegic, 7 (47%) 2. Diplegic, 5 (33%) 3. Dyskinetic, 3 (20%) | - | 2 (Range 1–2) | 0 | 1. Age 5–18 y 2. GMFCS level 1, level 2, or level 3 3. No history of epilepsy and no botulinum toxin A 4. Between February 2011 and February 2013 | 1. PBS score 2. MACS score | “Wii-fit balance-based video games are better at improving both static and performance-related balance parameters when combined with NDT treatment in children with mild CP” |
| Control, 15 (50%) | 10.53 ± 2.79 | 9 (60%) | Neuro-developmental treatment | 1. Hemiplegic, 7 (47%) 2. Diplegic, 7 (47%) 3. Dyskinetic, 1 (7%) | 2 (Range 1–3) | 0 | ||||||||||
| 40 | Tarakci et al., 2019 | Exergaming, 15 (50%) | Turkey | RCT | 10.93 ± 4.09 | 8 (53.33%) | 60 (Triple) | Eight | Leap Motion Controller-based training | 1. Spastic, 12(80) 2. Dyskinetic, 3(20) | - | - | 4 (21%) | 1. Between April 2016 and July 2017 2. All participants have signed informed consent forms 3. Aged between 5 to 17 y | 1. Durouz Hand Index score 2. JTHFT score 3. CHAQ score 4. NHPT score | “This study has quantitatively shown that LMCBT should be used as an effective alternative treatment option in children and adolescents with physical disabilities” |
| Control, 15 (50%) | 11.06 ± 3.23 | 9 (60%) | Conventional Rehabilitation | 1. Spastic, 11 (73.3%) 2. Dyskinetic, 4 (26.7%) | 4 (21%) | |||||||||||
| 41 | Urgen et al., 2016 | Exergaming, 15 (50%) | Turkey | RCT | 11.07 ± 2.37 | 7 (46.6%) | 45 (Twice) | Nine | Nintendo ®Wii-Fit and conventional rehabilitation | Spastic Hemiplegic | - | I and II | 0 | 1. Children with hemiplegic spastic CP 2. Age from 7 to 14y 3. GMFCS level II 4. To attend the routine rehabilitation program | 1. GMFM scores 2. Soft floor eyes open and closed balance reactions 3. Single Leg Standing and Tandem Standing 4. TUG(s) | “Nintendo®Wii-Fit training may affect advanced motor skills and improve the balance of children with spastic hemiplegic CP with physiotherapy” |
| Control, 15 (50%) | 11.33 ± 2.19 | 7 (46.6%) | - | Routine Physiotherapy and Rehabilitation Program | 0 | |||||||||||
| 42 | Uysal et al., 2016 | Exergaming, 12 (50%) | Turkey | Pilot RCT | 9.13 ± 2.57 | 8 (66.7%) | 30 (Twice) | Four | The NW gaming console with the Wii Sports Games was used for training and PT | Spastic | a. I, 6 (50%) b. II, 2 (16.7%) c. III, 4 (33.3%) | a. I, 9 (75%) b. II, 3 (25%) | 0 | 1. Children diagnosed with CP 2. Between the ages of 6 and 14 y 3. Level I or II on the GMFCS 4. Level I, II, or III on the MACS | 1. PEDI scores 2. PBS score 3. COPM score | “NW contributed to the implementation of occupational performance, daily living activities, and functional balance. We recommend that NW could be used in the rehabilitation program to engage in play-based activities with fun” |
| Control, 12 (50%) | 10.11 ± 2.62 | 2 (16.7%) | - | Regular physiotherapy | a. I, 6 (50%) b. II, 3 (25%) c. III, 3 (25%) | a. I, 10 (83.3%) b. II, 2 (16.7%) | 0 | |||||||||
| 43 | Velasco et al., 2017 | Exergaming, 5 (50%) | Spain | RCT | 4.8 ± 3 | - | 30 (Twice) | 16 | Serious videogames and (Traditional physical and occupational therapy) | - | - | - | 0 | 1. Males and females, aged 4–21 y 2. Diagnosed CP and cervical hypotonia or difficulties with head control 3. Cognitive capacity and behavior appropriate to understand the tasks | 1. GMFM-88 scores 2. VAS score 3. GAS score | “Physical therapy that combines serious games with traditional rehabilitation could allow children with CP to achieve larger function improvements in the trunk and cervical regions. However, given the limited scope of this trial (n = 10) additional studies are needed to corroborate this hypothesis” |
| Control, 5 (50%) | 11.2 ± 3.8 | - | Traditional physical and occupational therapy | 0 | ||||||||||||
| 44 | Wade et al., 2012 | Exergaming, 6 (46.15%) | UK | RCT | Mean 9.1 | - | (Triple) | Six | Computer and equipment with seat and platform(VR) | - | - | IV or V | 0 | 1. Young people aged 5 to 16 y 2. level IV or V on the GMFCS 3. At level three or higher on the Chailey scale of sitting ability | 1. Chailey level of box-sitting ability scores | “The study provides evidence to suggest that a meaningful and engaging therapeutic activity, such as using computer games controlled by leaning the upper body, can help to improve sitting ability in children with neuromotor dysfunction. Further work is required to understand fully what effects such activities have on the various components of sitting ability” |
| Control, 7 (53.85%) | - | No intervention | 0 | |||||||||||||
| 45 | Zoccolillo et al., 2015 | Exergaming, 11 (50%) | Italy | RCT | 6.89 ± 1.91 | - | 90 (Triple) | Eight | Xbox with Kinect device and Conventional therapy | - | - | - | 1 (9%) | 1. Clinical diagnosis of CP 2. Age between 4 and 14 y 3. GMFCS level 1 to 4 | 1. ABILHAND kids function scores | “VGT resulted effective in improving the motor functions of upper limb extremities in children with cerebral palsy, conceivably for the increased quantity of limb movements, but failed in performing the manual abilities for performing activities of daily living which benefited more from CT” |
| Control, 11 (50%) | 60 (Twice) | Conventional therapy | 3 (27.3%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tobaiqi, M.A.; Albadawi, E.A.; Fadlalmola, H.A.; Albadrani, M.S. Application of Virtual Reality-Assisted Exergaming on the Rehabilitation of Children with Cerebral Palsy: A Systematic Review and Meta-Analysis. J. Clin. Med. 2023, 12, 7091. https://doi.org/10.3390/jcm12227091
Tobaiqi MA, Albadawi EA, Fadlalmola HA, Albadrani MS. Application of Virtual Reality-Assisted Exergaming on the Rehabilitation of Children with Cerebral Palsy: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2023; 12(22):7091. https://doi.org/10.3390/jcm12227091
Chicago/Turabian StyleTobaiqi, Muhammad Abubaker, Emad Ali Albadawi, Hammad Ali Fadlalmola, and Muayad Saud Albadrani. 2023. "Application of Virtual Reality-Assisted Exergaming on the Rehabilitation of Children with Cerebral Palsy: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 12, no. 22: 7091. https://doi.org/10.3390/jcm12227091
APA StyleTobaiqi, M. A., Albadawi, E. A., Fadlalmola, H. A., & Albadrani, M. S. (2023). Application of Virtual Reality-Assisted Exergaming on the Rehabilitation of Children with Cerebral Palsy: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 12(22), 7091. https://doi.org/10.3390/jcm12227091






