Time to Change Our Viewpoints to Assess Renal Risks in Patients with Solitary Kidneys beyond Traditional Approaches?
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Inclusion and Exclusion Criteria
2.3. Urinary Biomarkers and Proteinuria/Albuminuria
2.4. Sociodemographic Data Survey
2.5. Ambulatory Blood Pressure Monitoring and Carotis Intima Media Thickness (CIMT)
2.6. Statistical Analysis
2.7. Ethical Procedure
3. Results
4. Discussion
4.1. General Perspective
4.2. SFK and Renal Dysfunction Findings
4.3. Congenital and Acquired SFK, Not the “Same Script, Different Cast”?
4.4. Our Findings about ABPM
4.5. Directions for Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Queißer-Luft, A.; Stolz, G.; Wiesel, A.; Schlaefer, K.; Spranger, J. Malformations in newborn: Results based on 30,940 infants and fetuses from the Mainz congenital birth defect monitoring system (1990–1998). Arch. Gynecol. Obstet. 2002, 266, 163–167. [Google Scholar] [CrossRef] [PubMed]
- Caiulo, V.A.; Caiulo, S.; Gargasole, C.; Chiriacò, G.; Latini, G.; Cataldi, L.; Mele, G. Ultrasound mass screening for congenital anomalies of the kidney and urinary tract. Pediatr. Nephrol. 2012, 27, 949–953. [Google Scholar] [CrossRef] [PubMed]
- Forouzanfar, M.H.; Liu, P.; Roth, G.A.; Ng, M.; Biryukov, S.; Marczak, L.; Alexander, L.; Estep, K.; Abate, K.H.; Akinyemiju, T.F.; et al. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mm Hg, 1990–2015. JAMA 2017, 317, 165–182. [Google Scholar] [CrossRef]
- Mancia Chairperson, G.; Kreutz Co-Chair, R.; Brunström, M.; Burnier, M.; Grassi, G.; Januszewicz, A.; Muiesan, M.L.; Tsioufis, K.; Agabiti-Rosei, E.; Algharably, E.A.E.; et al. 2023 ESH Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension Endorsed by the European Renal Association (ERA) and the International Society of Hypertension (ISH). J. Hypertens. 2023; ahead of print. [Google Scholar] [CrossRef]
- Yang, W.Y.; Melgarejo, J.D.; Thijs, L.; Zhang, Z.Y.; Boggia, J.; Wei, F.F.; Hansen, T.W.; Asayama, K.; Ohkubo, T.; Jeppesen, J.; et al. Association of office and ambulatory blood pressure with mortality and cardiovascular outcomes. JAMA 2019, 322, 409–420. [Google Scholar] [CrossRef]
- Kim, S.; Chang, Y.; Lee, Y.R.; Jung, H.-S.; Hyun, Y.Y.; Lee, K.-B.; Joo, K.J.; Yun, K.E.; Shin, H.; Ryu, S. Solitary kidney and risk of chronic kidney disease. Eur. J. Epidemiol. 2019, 34, 879–888. [Google Scholar] [CrossRef] [PubMed]
- Teppo, A.-M.; Törnroth, T.; Honkanen, E.; Grönhagen-Riska, C. Urinary amino-terminal propeptide of type III procollagen (PIIINP) as a marker of interstitial fibrosis in renal transplant recipients. Transplantation 2003, 75, 2113–2119. [Google Scholar] [CrossRef]
- Jhee, J.H.; Nam, B.Y.; Lee, C.J.; Park, J.T.; Han, S.H.; Kang, S.; Park, S.; Yoo, T. Soluble Urokinase-Type Plasminogen Activator Receptor, Changes of 24-Hour Blood Pressure, and Progression of Chronic Kidney Disease. J. Am. Hear. Assoc. 2021, 10, e017225. [Google Scholar] [CrossRef]
- Esse, R.; Barroso, M.; De Almeida, I.T.; Castro, R. The contribution of homocysteine metabolism disruption to endothelial dysfunction: State-of-the-art. Int. J. Mol. Sci. 2019, 20, 867. [Google Scholar] [CrossRef]
- Franssen, P.M.; Imholz, B.P. Evaluation of the Mobil-O-Graph new generation ABPM device using the ESH criteria. Blood Press. Monit. 2010, 15, 229–231. [Google Scholar] [CrossRef]
- American Medical Association önerisiyle Valide cihaz US Blood Pressure Validated Device Listing. Available online: https://www.validatebp.org (accessed on 7 July 2022).
- Parati, G.; Stergiou, G.; O’brien, E.; Asmar, R.; Beilin, L.; Bilo, G.; Clement, D.; de la Sierra, A.; de Leeuw, P.; Dolan, E.; et al. European Society of hypertension practice guidelines for ambulatory blood pressure monitoring. J. Hypertens. 2014, 32, 1359–1366. [Google Scholar] [CrossRef] [PubMed]
- Murugapoopathy, V.; Gupta, I.R. A Primer on Congenital Anomalies of the Kidneys and Urinary Tracts (CAKUT). Clin. J. Am. Soc. Nephrol. 2020, 15, 723–731. [Google Scholar] [CrossRef] [PubMed]
- Schreuder, M.F.; Westland, R.; van Wijk, J.A.E. Unilateral multicystic dysplastic kidney: A meta-analysis of observational studies on the incidence, associated urinary tract malformations and the contralateral kidney. Nephrol. Dial. Transplant. 2009, 24, 1810–1818. [Google Scholar] [CrossRef] [PubMed]
- Westland, R.; Schreuder, M.F.; Ket, J.C.; van Wijk, J.A. Unilateral renal agenesis: A systematic review on associated anomalies and renal injury. Nephrol. Dial. Transplant. 2013, 28, 1844–1855. [Google Scholar] [CrossRef]
- Srivastava, T.; Celsi, G.E.; Sharma, M.; Dai, H.; McCarthy, E.T.; Ruiz, M.; Cudmore, P.A.; Alon, U.S.; Sharma, R.; Savin, V.A. Fluid flow shear stress over podocytes is increased in the solitary kidney. Nephrol. Dial. Transplant. 2014, 29, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Sanna-Cherchi, S.; Ravani, P.; Corbani, V.; Parodi, S.; Haupt, R.; Piaggio, G.; Innocenti, M.L.; Somenzi, D.; Trivelli, A.; Caridi, G.; et al. Renal outcome in patients with congenital anomalies of the kidney and urinary tract. Kidney Int. 2009, 76, 528–533. [Google Scholar] [CrossRef]
- Oldrizzi, L.; Rugiu, C.; De Biase, V.; Maschio, G. The solitary kidney: A risky situation for progressive renal damage? Am. J. Kidney Dis. 1991, 17, S57–S61. [Google Scholar]
- Wang, Y.; Wang, Z.; Wang, W.; Ren, H.; Zhang, W.; Chen, N. Analysis of factors associated with renal function in Chinese adults with congenital solitary kidney. Intern. Med. 2010, 49, 2203–2209. [Google Scholar] [CrossRef]
- Argueso, L.R.; Ritchey, M.L.; Boyle, E.T.; Milliner, D.S.; Bergstralh, E.J.; Kramer, S.A. Prognosis of patients with unilateral renal agenesis. Pediatr. Nephrol. 1992, 6, 412–416. [Google Scholar] [CrossRef]
- Cochat, P.; Febvey, O.; Bacchetta, J.; Bérard, E.; Cabrera, N.; Dubourg, L. Towards adulthood with a solitary kidney. Pediatr. Nephrol. 2019, 34, 2311–2323. [Google Scholar] [CrossRef]
- Grams, M.E.; Sang, Y.; Levey, A.S.; Matsushita, K.; Ballew, S.; Chang, A.R.; Chow, E.K.; Kasiske, B.L.; Kovesdy, C.P.; Nadkarni, G.N.; et al. Kidney-failure risk projection for the living kidney-donor candidate. N. Engl. J. Med. 2016, 374, 411–421. [Google Scholar] [CrossRef]
- Park, J.Y.; Yang, W.J.; Doo, S.W.; Park, J.J.; Gwon, Y.N.; Kim, K.M.; Kim, J.H.; Kim, D.K. Long-term end-stage renal disease risks after living kidney donation: A systematic review and meta-analysis. BMC Nephrol. 2023, 24, 152. [Google Scholar] [CrossRef] [PubMed]
- Haberal, G.; Yildirim, T.; Yilmaz, S.R.; Altun, B.; Aki, F.T.; Erdem, Y.; Arici, M. Chronic Kidney Disease Risk in Living Kidney Transplant Donors: A Long-Term Follow-Up Study. Nephron, 2023; ahead of print. [Google Scholar] [CrossRef]
- Munch, P.; Christiansen, C.F.; Birn, H.; Erikstrup, C.; Nørgaard, M. Is the risk of cardiovascular disease increased in living kidney donors? A Danish population-based cohort study. Am. J. Transplant. 2021, 21, 1857–1865. [Google Scholar] [CrossRef] [PubMed]
- Cachat, F.; Combescure, C.; Chehade, H.; Zeier, G.; Mosig, D.; Meyrat, B.; Frey, P.; Girardin, E. Microalbuminuria and hyperfiltration in subjects with nephro-urological disorders. Nephrol. Dial. Transplant. 2013, 28, 386–391. [Google Scholar] [CrossRef]
- Srivastava, T.; Ju, W.; Milne, G.L.; Rezaiekhaligh, M.H.; Staggs, V.S.; Alon, U.S.; Sharma, R.; Zhou, J.; El-Meanawy, A.; McCarthy, E.T.; et al. Urinary prostaglandin E2 is a biomarker of early adaptive hyperfiltration in solitary functioning kidney. Prostaglandins Other Lipid Mediat. 2020, 146, 106403. [Google Scholar] [CrossRef]
- Naik, A.S.; Wang, S.Q.; Chowdhury, M.; Aqeel, J.; O’connor, C.L.; Wiggins, J.E.; Bitzer, M.; Wiggins, R.C. Critical timing of ACEi initiation prevents compensatory glomerular hypertrophy in the remaining single kidney. Sci. Rep. 2021, 11, 19605. [Google Scholar] [CrossRef]
- Westland, R.; Schreuder, M.F.; Van Goudoever, J.B.; Sanna-Cherchi, S.; Van Wijk, J.A.E. Clinical Implications of the Solitary Functioning Kidney. Clin. J. Am. Soc. Nephrol. 2014, 9, 978–986. [Google Scholar] [CrossRef] [PubMed]
- Simeoni, M.; Armeni, A.; Summaria, C.; Cerantonio, A.; Fuiano, G. Current evidence on the use of anti-RAAS agents in congenital or acquired solitary kidney. Ren. Fail. 2017, 39, 660–670. [Google Scholar] [CrossRef] [PubMed]
- Spira, E.M.; Jacobi, C.; Frankenschmidt, A.; Pohl, M.; von Schnakenburg, C. Sonographic long-term study: Paediatric growth charts for single kidneys. Arch. Dis. Child. 2009, 94, 693–698. [Google Scholar] [CrossRef]
- Lenihan, C.R.; Busque, S.; Derby, G.; Blouch, K.; Myers, B.D.; Tan, J.C. Longitudinal study of living kidney donor glomerular dynamics after nephrectomy. J. Clin. Investig. 2015, 125, 1311–1318. [Google Scholar] [CrossRef] [PubMed]
- Chevalier, R.L. Reduced renal mass in early postnatal development. Glomerular dynamics in the guinea pig. Neonatology 1983, 44, 158–165. [Google Scholar] [CrossRef] [PubMed]
- Larsson, L.; Aperia, A.; Wilton, P. Effect of normal development on compensatory renal growth. Kidney Int. 1980, 18, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Maluf, N. On the enlargement of the normal congenitally solitary kidney. Br. J. Urol. 1997, 79, 836–841. [Google Scholar] [CrossRef] [PubMed]
- Jaoudé, P.A.; Dubourg, L.; Bacchetta, J.; Berthiller, J.; Ranchin, B.; Cochat, P. Congenital versus acquired solitary kidney: Is the difference relevant? Nephrol. Dial. Transplant. 2011, 26, 2188–2194. [Google Scholar] [CrossRef]
- Yazıcı, R.; Altıntepe, L.; Guney, I.; Yazıcı, M. Effect of congenital or acquired renal mass reduction on arterial stiffness. Clin. Physiol. Funct. Imaging 2022, 42, 436–442. [Google Scholar] [CrossRef]
- Kasap-Demir, B.; Soyaltın, E.; Arslansoyu-Çamlar, S.; Alparslan, C.; Alaygut, D.; Yavaşcan, Ö.; Demircan, T.; Mutlubaş, F.; Karadeniz, C. Cardiovascular risk assessment in children and adolescents with congenital solitary kidneys. J. Clin. Hypertens. 2021, 23, 245–252. [Google Scholar] [CrossRef]
- Gadalean, F.N.; Gluhovschi, G.; Trandafirescu, V.; Petrica, L.; Velciov, S.; Bozdog, G.; Gluhovschi, C.; Bob, F.; Vernic, C. Estimated glomerular filtration rate in patients with surgically acquired single kidney compared with patients with congenital single kidney: Implications for kidney transplant from live donors. Exp. Clin. Transplant. 2010, 8, 228–236. [Google Scholar]
- Bohle, A.; Mackensen-Haen, S.; Gise, H. Significance of tubule-interstitial changes in the renal cortex for the excretory func-tion and concentration ability of the kidney. A morphometric contribution. Am. J. Nephrol. 1987, 7, 421–433. [Google Scholar] [CrossRef]
- Fu, L.; Li, Y.; Luo, D.; Deng, S.; Wu, B.; Hu, Y. Evidence on the causal link between homocysteine and hypertension from a meta-analysis of 40173 individuals implementing Mendelian randomization. J. Clin. Hypertens. 2019, 21, 1879–1894. [Google Scholar] [CrossRef]
- Lim, U.; Cassano, P.A. Homocysteine and Blood Pressure in the Third National Health and Nutrition Examination Survey, 1988–1994. Am. J. Epidemiol. 2002, 156, 1105–1113. [Google Scholar] [CrossRef] [PubMed]
- Haloul, M.; Vinjamuri, S.J.; Naquiallah, D.; Mirza, M.I.; Qureshi, M.; Hassan, C.; Masrur, M.; Bianco, F.M.; Frederick, P.; Cristoforo, G.P. Hyperhomocysteinemia and low folate and vitamin B12 are associated with vascular dysfunction and impaired nitric oxide sensitivity in morbidly obese patients. Nutrients 2020, 12, 2014. [Google Scholar] [CrossRef]
- Deng, Y.; Li, Z.; An, X.; Fan, R.; Wang, Y.; Li, J.; Yang, X.; Liao, J.; Xia, Y. Hyperhomocysteinemia Promotes Cardiac Hypertrophy in Hypertension. Oxidative Med. Cell. Longev. 2022, 2022, 1486157. [Google Scholar] [CrossRef] [PubMed]
- Stiefel, P.; Vallejo-Vaz, A.J.; García Morillo, S.; Villar, J. Role of the Renin-Angiotensin system and aldosterone on cardiometabolic syndrome. Int. J. Hypertens. 2011, 2011, 685238. [Google Scholar] [CrossRef]
- Huang, A.; Pinto, J.T.; Froogh, G.; Kandhi, S.; Qin, J.; Wolin, M.S.; Hintze, T.H.; Sun, D. Role of homocysteinylation of ACE in endothelial dysfunction of arteries. Am. J. Physiol. Circ. Physiol. 2015, 308, H92–H100. [Google Scholar] [CrossRef] [PubMed]
- Xie, D.; Yuan, Y.; Guo, J.; Yang, S.; Xu, X.; Wang, Q.; Li, Y.; Qin, X.; Tang, G.; Huo, Y.; et al. Hyperhomocysteinemia predicts renal function decline: A prospective study in hypertensive adults. Sci. Rep. 2015, 5, 16268. [Google Scholar] [CrossRef]
- Carnagarin, R.; Nolde, J.M.; Ward, N.C.; Lugo-Gavidia, L.M.; Chan, J.; Robinson, S.; Jose, A.; Joyson, A.; Azzam, O.; Kiuchi, M.G.; et al. Homocysteine predicts vascular target organ damage in hypertension and may serve as guidance for first-line antihypertensive therapy. J. Clin. Hypertens. 2021, 23, 1380–1389. [Google Scholar] [CrossRef]
- Kasiske, B.L.; Anderson-Haag, T.; Israni, A.K.; Kalil, R.S.; Kimmel, P.L.; Kraus, E.S.; Kumar, R.; Posselt, A.A.; Pesavento, T.E.; Rabb, H.; et al. A prospective controlled study of living kidney donors: Three-year follow-up. Am. J. Kidney Dis. 2015, 66, 114–124. [Google Scholar] [CrossRef]
- Conen, D.; Bamberg, F. Noninvasive 24-h ambulatory blood pressure and cardiovascular disease: A systematic review and meta-analysis. J. Hypertens. 2008, 26, 1290–1299. [Google Scholar] [CrossRef]
- US Preventive Services Task Force. Screening for Hypertension in Adults: US Preventive Services Task Force Reaffirmation Recommendation Statement. JAMA 2021, 325, 1650–1656. [Google Scholar] [CrossRef]
- Li, Y.; Staessen, J.A.; Lu, L.; Li, L.-H.; Wang, G.-L.; Wang, J.-G. Is isolated nocturnal hypertension a novel clinical entity? Findings from a Chinese population study. Hypertension 2007, 50, 333–339. [Google Scholar] [CrossRef] [PubMed]
- Wijkman, M.; Länne, T.; Engvall, J.; Lindström, T.; Östgren, C.J.; Nystrom, F.H. Masked nocturnal hypertension—A novel marker of risk in type 2 diabetes. Diabetologia 2009, 52, 1258–1264. [Google Scholar] [CrossRef] [PubMed]
- Vinyoles, E.; Puig, C.; Roso-Llorach, A.; Soldevila, N.; de la Sierra, A.; Gorostidi, M.; Segura, J.; Divison-Garrote, J.A.; Muñoz, M.; Ruilope, L.M. Role of ambulatory blood pressure on prediction of cardiovascular disease. A cohort study. J. Hum. Hypertens. 2023, 37, 279–285. [Google Scholar] [CrossRef] [PubMed]
- Fan, H.-Q.; Li, Y.; Thijs, L.; Hansen, T.W.; Boggia, J.; Kikuya, M.; Björklund-Bodegård, K.; Richart, T.; Ohkubo, T.; Jeppesen, J.; et al. Prognostic value of isolated nocturnal hypertension on ambulatory measurement in 8711 individuals from 10 populations. J. Hypertens. 2010, 28, 2036–2045. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Su, X.; Nie, Y.; Zeng, Z.; Chen, H.; NARRAS investigators. Nocturnal blood pressure rather than night-to-day blood pressure ratio is related to arterial stiffening in untreated young and middle-aged adults with non-dipper hypertension. J. Clin. Hypertens. 2022, 24, 1044–1050. [Google Scholar] [CrossRef]
- Gu, Y.-M.; Thijs, L.; Li, Y.; Asayama, K.; Boggia, J.; Hansen, T.W.; Liu, Y.-P.; Ohkubo, T.; Björklund-Bodegård, K.; Jeppesen, J.; et al. Outcome-driven thresholds for ambulatory pulse pressure in 9938 participants recruited from 11 populations. Hypertension 2014, 63, 229–237. [Google Scholar] [CrossRef]
- Ciobanu, D.M.; Bala, C.; Rusu, A.; Cismaru, G.; Roman, G. E-Selectin Is Associated with Daytime and 24-Hour Diastolic Blood Pressure Variability in Type 2 Diabetes. Biomedicines 2022, 10, 279. [Google Scholar] [CrossRef]
- Kayikçioğlu, H.; Akbuğa, K. Relationship between C-reactive protein/albumin ratio and dipper/nondipper pattern in normotensive individuals. Blood Press. Monit. 2022, 27, 310–313. [Google Scholar] [CrossRef]
- Szumińska, A.R.; Wasilewska, A.; Kamianowska, M. Protein Biomarkers in Chronic Kidney Disease in Children—What Do We Know So Far? J. Clin. Med. 2023, 12, 3934. [Google Scholar] [CrossRef]
- Koh, A.S.; Velmurugan, B.; Gao, F.; Tan, R.S.; Wong, J.-I.; Teo, L.L.Y.; Keng, B.M.H.; Chua, S.J.M.; Yuan, J.-M.; Koh, W.-P.; et al. Value of soluble Urokinase plasminogen activator receptor over age as a biomarker of impaired myocardial relaxation. BMC Geriatr. 2017, 17, 275. [Google Scholar] [CrossRef]
- Greenberg, J.H.; Abraham, A.G.; Xu, Y.; Schelling, J.R.; Feldman, H.I.; Sabbisetti, V.S.; Gonzalez, M.C.; Coca, S.; Schrauben, S.J.; Waikar, S.S.; et al. Plasma Biomarkers of Tubular Injury and Inflammation Are Associated with CKD Progression in Children. J. Am. Soc. Nephrol. 2020, 31, 1067–1077. [Google Scholar] [CrossRef] [PubMed]
- Weidemann, D.K.; Abraham, A.G.; Roem, J.L.; Furth, S.L.; Warady, B.A. Plasma Soluble Urokinase Plasminogen Activator Receptor (suPAR) and CKD Progression in Children. Am. J. Kidney Dis. 2020, 76, 194–202. [Google Scholar] [CrossRef] [PubMed]
- Hayek, S.S.; Sever, S.; Ko, Y.-A.; Trachtman, H.; Awad, M.; Wadhwani, S.; Altintas, M.M.; Wei, C.; Hotton, A.L.; French, A.L.; et al. Soluble Urokinase Receptor and Chronic Kidney Disease. N. Engl. J. Med. 2015, 373, 1916–1925. [Google Scholar] [CrossRef]
- Rowaiye, O.O.; Kusztal, M.; Zabinska, M.; Bartoszek, D.; Myszka, M.; Kościelska-Kasprzak, K.; Banasik, M.; Mazanowska, O.; Klinger, M.; Krajewska, M. Anti-ETAR and suPAR as markers of disease activity in renal ANCA-associated vasculitis. Adv. Med. Sci. 2022, 67, 23–28. [Google Scholar] [CrossRef] [PubMed]
- Fujimoto, K.; Imura, J.; Atsumi, H.; Matsui, Y.; Adachi, H.; Okuyama, H.; Yamaya, H.; Yokoyama, H. Clinical significance of serum and urinary soluble urokinase receptor (suPAR) in primary nephrotic syndrome and MPO-ANCA-associated glomerulonephritis in Japanese. Clin. Exp. Nephrol. 2015, 19, 804–814. [Google Scholar] [CrossRef]
- El Ghoul, B.; Squalli, T.; Servais, A.; Elie, C.; Meas-Yedid, V.; Trivint, C.; Vanmassenhove, J.; Grünfeld, J.-P.; Olivo-Marin, J.-C.; Thervet, E.; et al. Urinary procollagen III aminoterminal propeptide (PIIINP): A fibrotest for the nephrologist. Clin. J. Am. Soc. Nephrol. 2010, 5, 205–210. [Google Scholar] [CrossRef]
- Weidemann, F.; Beer, M.; Kralewski, M.; Siwy, J.; Kampmann, C. Early detection of organ involvement in Fabry disease by biomarker assessment in conjunction with LGE cardiac MRI: Results from the SOPHIA study. Mol. Genet. Metab. 2019, 126, 169–182. [Google Scholar] [CrossRef]
- Soylemezoglu, O.; Wild, G.; Dalley, A.J.; MacNeil, S.; Milford-Ward, A.; Brown, C.B.; el Nahas, A.M. Urinary and serum type III collagen: Markers of renal fibrosis. Nephrol. Dial. Transplant. 1997, 12, 1883–1889. [Google Scholar] [CrossRef]
- Dhingra, R.; Pencina, M.J.; Schrader, P.; Wang, T.J.; Levy, D.; Pencina, K.; Siwik, D.A.; Colucci, W.S.; Benjamin, E.J.; Vasan, R.S.; et al. Relations of matrix remodeling biomarkers to blood pressure progression and incidence of hypertension in the community. Circulation 2009, 119, 1101–1107. [Google Scholar] [CrossRef]
- Timms, P.M.; Wright, A.; Maxwell, P.; Campbell, S.; Dawnay, A.B.; Srikanthan, V. Plasma tissue inhibitor of metalloproteinase-1 levels are elevated in essential hypertension and related to left ventricular hypertrophy. Am. J. Hypertens. 2002, 15, 269–272. [Google Scholar] [CrossRef]
- Gonzalez, E.; Gutierrez, E.; Morales, E.; Hernandez, E.; Andres, A.; Bello, I.; Diaz-Gonzalez, R.; Leiva, O.; Praga, M. Factors influencing the progression of renal damage in patients with unilateral renal agenesis and remnant kidney. Kidney Int. 2005, 68, 263–270. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Alfandary, H.; Haskin, O.; Goldberg, O.; Dagan, A.; Borovitz, Y.; Levi, S.; Davidovits, M.; Erlich, T.; Landau, D.; Pleniceanu, O. Is the prognosis of congenital single functioning kidney benign? A population-based study. Pediatr. Nephrol. 2021, 36, 2837–2845. [Google Scholar] [CrossRef] [PubMed]
- Zappitelli, M.; Parvex, P.; Joseph, L.; Paradis, G.; Grey, V.; Lau, S.; Bell, L. Derivation and validation of cystatin C-based prediction equations for GFR in children. Am. J. Kidney Dis. 2006, 48, 221–230. [Google Scholar] [CrossRef] [PubMed]
- Tan, J.C.; Ho, B.; Busque, S.; Blouch, K.; Derby, G.; Efron, B.; Myers, B.D. Imprecision of creatinine-based GFR estimates in uninephric kidney donors. Clin. J. Am. Soc. Nephrol. 2010, 5, 497–502. [Google Scholar] [CrossRef] [PubMed][Green Version]
- La Scola, C.; Ammenti, A.; Bertulli, C.; Bodria, M.; Brugnara, M.; Camilla, R.; Capone, V.; Casadio, L.; Chimenz, R.; Conte, M.L.; et al. Management of the congenital solitary kidney: Consensus recommendations of the Italian Society of Pediatric Nephrology. Pediatr. Nephrol. 2022, 37, 2185–2207. [Google Scholar] [CrossRef] [PubMed]
- Khokhar, M.; Roy, D.; Modi, A.; Agarwal, R.; Yadav, D.; Purohit, P.; Sharma, P. Perspectives on the role of PTEN in diabetic nephropathy: An update. Crit. Rev. Clin. Lab. Sci. 2020, 57, 470–483. [Google Scholar] [CrossRef]
- An, C.; Jiao, B.; Du, H.; Tran, M.; Zhou, D.; Wang, Y. Myeloid PTEN deficiency aggravates renal inflammation and fibrosis in angiotensin II-induced hypertension. J. Cell. Physiol. 2022, 237, 983–991. [Google Scholar] [CrossRef]
| Nx(+) (n = 35) | Nx(−) (n = 50) | p | |
|---|---|---|---|
| Age | 56.88 ± 13.91 | 45.86 ± 13.47 | <0.001 |
| f/m (n, %) | 19 (54.3%)/16 (45.7%) | 25 (50.0%)/25 (50.0%) | 0.697 |
| BMI (kg/m2) | 29.42 ± 4.63 | 27.54 ± 4.62 | 0.347 |
| Parenchyma thickness, SFK (mm) | 14.48 ± 2.88 | 15.41 ± 3.27 | 0.895 |
| SFK, (right%) | 24 (68.6%) | 25 (50.0%) | 0.088 |
| Presence/history of nephrolithiasis (n, %) | 11 (31.4%) | 9 (18.0%) | 0.151 |
| Hypertension (n, %) | 24 (68.6%) | 34 (68.0%) | 0.956 |
| Diabetes Mellitus (n, %) | 13 (37.1%) | 12 (24.0%) | 0.191 |
| Smoking (n, %) | 11 (31.4%) | 20 (40.0%) | 0.419 |
| LDL < 130 mg/dL (n, %) | 28 (80.0%) | 35 (70.0%) | 0.300 |
| Mean antihypertensives, (n) | 1 (0–4) | 1 (0–4) | 0.978 |
| Antihypertensive treatments | |||
| RAAS inhibitors (n, %) | 16 (45.7%) | 28 (56.0%) | 0.350 |
| Thiazides (n, %) | 7 (20.0%) | 12 (24.0%) | 0.663 |
| Calcium channel blockers (n, %) | 11 (31.4%) | 16 (32.0%) | 0.956 |
| Beta blockers (n, %) | 10 (28.6%) | 10 (20.0%) | 0.359 |
| Alpha-blockers (n, %) | 2 (5.7%) | 0 (0.0%) | 0.167 |
| Nx etiology | |||
| Renal cancer | 9 (25.7%) | ||
| Nephrol./pyelonephr. | 10 (26.6%) | ||
| Unknown | 6 (17.1%) | ||
| Donor | 7 (20.0%) | ||
| Atrophic/dysfunction | 2 (5.7%) | ||
| Hydronephrosis | 1 (2.9%) |
| Nx(+) | Nx(−) | p | |
|---|---|---|---|
| Creatinine (mg/dL) | 1.15 (0.48–4.00) | 1.08 (0.54–4.23) | 0.780 |
| GFR (mL/min/1.73 m2) | 64.64 ± 26.41 | 72.28 ± 31.91 | 0.481 |
| UA (mg/dL) | 5.91 ± 1.08 | 6.16 ± 1.76 | 0.358 |
| CRP (mg/dL) | 1.63 (0.60–23.15) | 2.92 (0.60–63.30) | 0.188 |
| Albumin (g/dL) | 4.53 ± 0.37 | 4.56 ± 0.31 | 0.906 |
| 25OH Vitamin D (ng/mL) | 21.12 ± 11.21 | 18.45 ± 9.56 | 0.736 |
| Hemoglobin (g/L) | 13.38 ± 2.11 | 13.60 ± 1.80 | 0.607 |
| Homocysteine(µmol/L) | 16.60 (7.90–41.20) | 18.05 (9.30–46.20) | 0.151 |
| Proteinuria (24 h, mg/d) | 210 (44–4808) | 250 (38–6829) | 0.448 |
| Albuminuria(24 h, mg/d) | 23 (2–2649) | 48.5 (4–5615) | 0.262 |
| Natriuria (24 h, mmol/d) | 138.11 ± 68.74 | 173.68 ± 87.68 | 0.156 |
| Kaliuria (24 h, mmol/d) | 45.04 ± 20.58 | 51.19 ± 21.74 | 0.460 |
| suPAR (24 h urine, ng/L) | 250.70 (86.40–316.30) | 239.85 (113.70–331.90) | 0.422 |
| PIIINP (24 h urine, ng/L) | 1988.00 (661.30–8254.00) | 1869.50 (652.10–8165.00) | 0.80 |
| Natriuria/kaliuria | 3.13 (0.95–7.70) | 3.23 (1.23–7.27) | 0.526 |
| CRP/albumin | 0.36 (0.12–5.35) | 0.66 (0.12–13.33) | 0.203 |
| Parameter | r | p |
|---|---|---|
| Age (years) with: | ||
| BMI (kg/m2) | 0.296 | 0.006 |
| eGFR (mL/min/1.73 m2) | −0.507 | <0.001 |
| meanSyst | 0.272 | 0.012 |
| 24 hMAP | 0.280 | 0.012 |
| dSyst | 0.238 | 0.028 |
| dMean | 0.229 | 0.041 |
| nSyst | 0.294 | 0.006 |
| nMean | 0.280 | 0.012 |
| CIMTr (mm) | 0.501 | <0.001 |
| CIMTl (mm) | 0.602 | <0.001 |
| Antihypertensives | 0.354 | 0.001 |
| Nx(+) | Nx(−) | p | |
|---|---|---|---|
| 24 h-Mean Syst. | 118.22 ± 15.20 | 118.24 ± 12.96 | 0.379 |
| 24 h-Mean Diast. | 74.77 ± 9.53 | 75.94 ± 9.25 | 0.262 |
| 24 h-MAP | 94.72 ± 11.74 | 75.94 ± 9.25 | 0.254 |
| 24 h-Pulse | 72.97 ± 9.05 | 76.92 ± 9.69 | 0.318 |
| 24 h-Pulse Pressure | 43.59 ± 10.00 | 42.30 ± 8.00 | 0.922 |
| Mean SD | 9.22 ± 2.51 | 10.15 ± 3.24 | 0.037 |
| DaytimeSyst. | 119.91 ± 15.79 | 119.62 ± 13.57 | 0.496 |
| DaytimeDiast. | 76.17 ± 9.78 | 77.40 ± 9.89 | 0.306 |
| DaytimeMAP | 96.24 ± 12.22 | 96.74 ± 11.15 | 0.359 |
| NighttimeSyst. | 113.25 ± 15.04 | 114.36 ± 14.72 | 0.175 |
| NighttimeDiast. | 70.34 ± 10.23 | 72.10 ± 10.76 | 0.186 |
| NighttimeMAP | 89.90 ± 11.84 | 91.72 ± 12.03 | 0.110 |
| CIMTr (mm) | 0.73 ± 0.29 | 0.65 ± 0.23 | 0.852 |
| CIMTl (mm) | 0.76 ± 0.27 | 0.66 ± 0.17 | 0.853 |
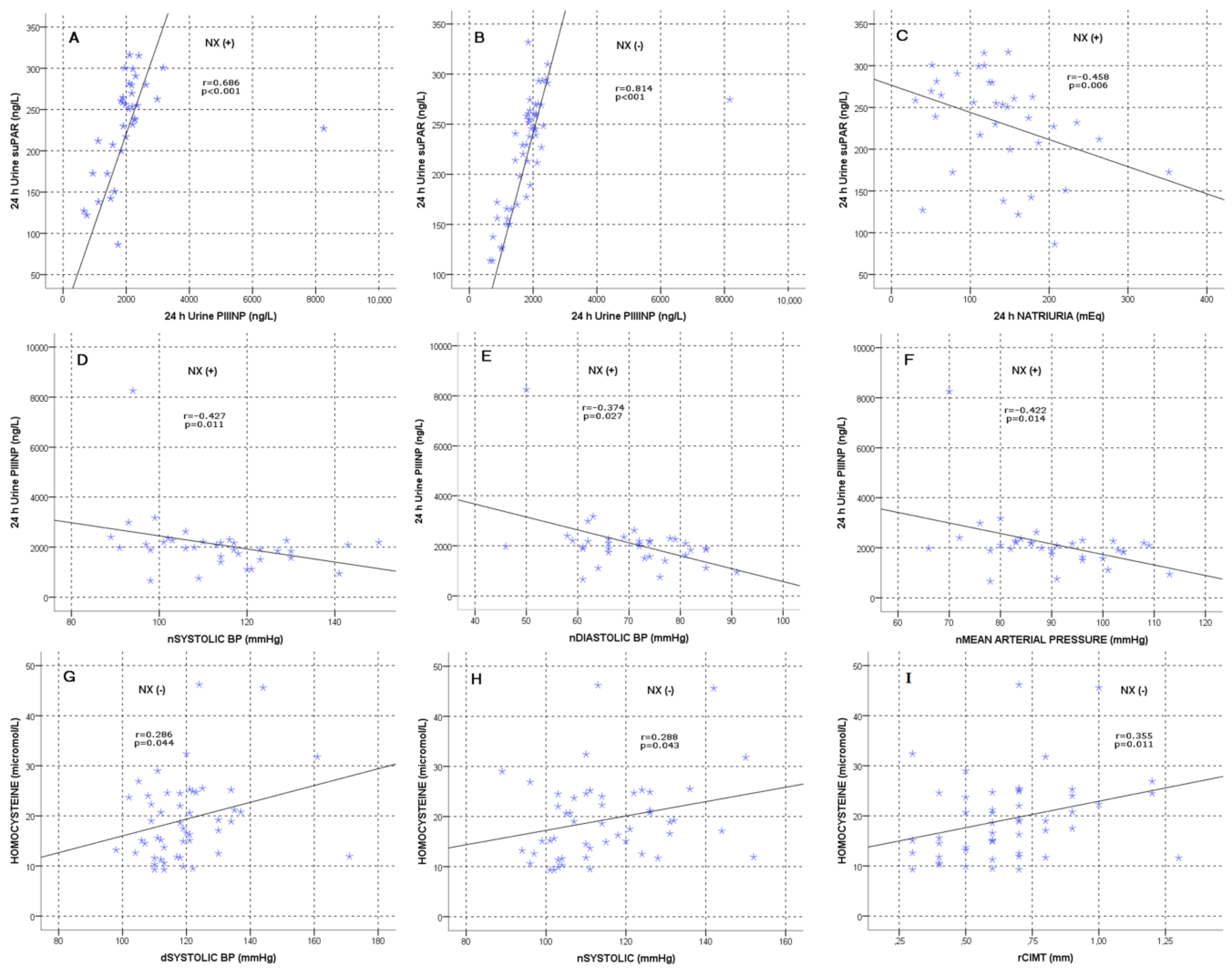
| Nx(+) | Nx(−) | |||
|---|---|---|---|---|
| r | p | r | p | |
| PIIINP with: | ||||
| suPAR | 0.686 | <0.001 | 0.814 | <0.001 |
| meanSyst | −0.357 | 0.035 | 0.017 | 0.905 |
| nSyst | −0.427 | 0.011 | −0.040 | 0.781 |
| nDiast | −0.374 | 0.027 | −0.038 | 0.794 |
| nMAP | −0.422 | 0.014 | −0.021 | 0.886 |
| suPAR with: | ||||
| Natriuria | −0.458 | 0.006 | −0.066 | 0.651 |
| nDiast | −0.378 | 0.025 | −0.072 | 0.620 |
| Homocysteine with: | ||||
| BMI | −0.039 | 0.826 | 0.365 | 0.009 |
| eGFR | −0.580 | <0.001 | −0.658 | <0.001 |
| UA | 0.318 | 0.062 | 0.469 | 0.001 |
| Albumin | −0.206 | 0.235 | −0.291 | 0.041 |
| Alb/Glob | −0.488 | 0.007 | −0.417 | 0.003 |
| Proteinuria | 0.159 | 0.362 | 0.396 | 0.004 |
| Albuminuria | 0.227 | 0.189 | 0.440 | 0.001 |
| meanSyst | 0.209 | 0.229 | 0.310 | 0.028 |
| Pulse pressure | 0.256 | 0.138 | 0.414 | 0.003 |
| dSyst | 0.225 | 0.194 | 0.286 | 0.044 |
| nSyst | 0.198 | 0.254 | 0.288 | 0.043 |
| CIMTr | 0.101 | 0.564 | 0.355 | 0.011 |
| Antihypertensives | 0.275 | 0.110 | 0.325 | 0.021 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alp, A.; Saruhan, E.; Doğan, E.; Genek, D.G.; Huddam, B. Time to Change Our Viewpoints to Assess Renal Risks in Patients with Solitary Kidneys beyond Traditional Approaches? J. Clin. Med. 2023, 12, 6885. https://doi.org/10.3390/jcm12216885
Alp A, Saruhan E, Doğan E, Genek DG, Huddam B. Time to Change Our Viewpoints to Assess Renal Risks in Patients with Solitary Kidneys beyond Traditional Approaches? Journal of Clinical Medicine. 2023; 12(21):6885. https://doi.org/10.3390/jcm12216885
Chicago/Turabian StyleAlp, Alper, Ercan Saruhan, Emrah Doğan, Dilek Gibyeli Genek, and Bülent Huddam. 2023. "Time to Change Our Viewpoints to Assess Renal Risks in Patients with Solitary Kidneys beyond Traditional Approaches?" Journal of Clinical Medicine 12, no. 21: 6885. https://doi.org/10.3390/jcm12216885
APA StyleAlp, A., Saruhan, E., Doğan, E., Genek, D. G., & Huddam, B. (2023). Time to Change Our Viewpoints to Assess Renal Risks in Patients with Solitary Kidneys beyond Traditional Approaches? Journal of Clinical Medicine, 12(21), 6885. https://doi.org/10.3390/jcm12216885






