Fear of COVID-19 Predicts Depression, Anxiety and Post-Traumatic Stress Disorders in Patients with Implantable Cardioverter Defibrillators and Is Mediated by Positive and Negative Affects—A Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
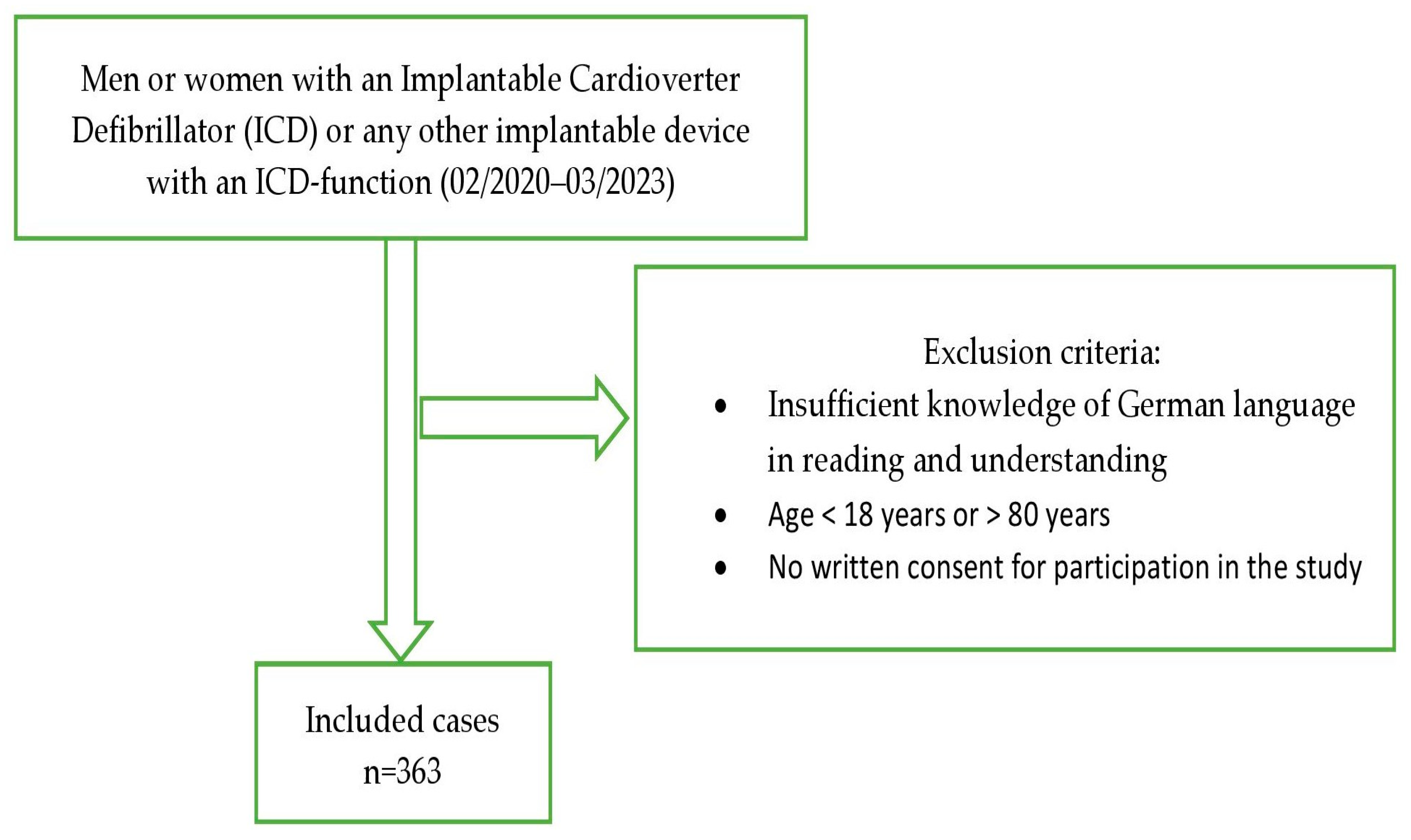
2.1. Design and Sample
2.2. Instruments
2.2.1. Fear of COVID-19 Scale (FCV-19S)
2.2.2. Measurements of Depression, Anxiety and Post-Traumatic Stress Disorder (PTSD)
2.2.3. Measurements of Positive and Negative Affects
2.2.4. ENRICHD Social Support Instrument (ESSI)
2.3. Data Analysis
3. Results
3.1. Description of the Study Sample
3.2. Fear of COVID-19, Anxiety, Depression and PTSD in the Study Sample
3.3. Identification of Predictors for Anxiety, Depression and PTSD
3.4. Mediation Models between Fear of COVID-19 and Anxiety, Depression and PTSD
4. Discussion
4.1. Main Findings of the Study
4.2. Implications of the Study
4.3. Limitations and Future Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Umakanthan, S.; Sahu, P.; Ranade, A.V.; Bukelo, M.M.; Rao, J.S.; Abrahao Machado, L.F.; Dahal, S.; Kumar, H.; Dhananjaya, K. Origin, transmission, diagnosis and management of coronovirus disease 2019 (COVID-19). Postgrad. Med. J. 2020, 96, 753–758. [Google Scholar] [PubMed]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [PubMed]
- Dubey, S.; Biswas, P.; Ghosh, R.; Chatterjee, S.; Dubey, M.J.; Chatterjee, S.; Lahiri, D.; Lavie, C.J. Psychosocial impact of COVID-19. Diabetes Metab. Syndr. 2020, 14, 779–788. [Google Scholar] [CrossRef] [PubMed]
- Adabag, S.; Zimmerman, P.; Black, A.; Madjid, M.; Safavi-Naeini, P.; Cheng, A. Implantable Cardioverter-Defibrillator Shocks during COVID-19 Outbreak. J. Am. Heart Assoc. 2021, 10, e019708. [Google Scholar] [CrossRef] [PubMed]
- Kapa, S.; Rotondi-Trevisan, D.; Mariano, Z.; Aves, T.; Irvine, J.; Dorian, P.; Hayes, D.L. Psychopathology in Patients with ICDs over Time: Results of a Prospective Study. Pace 2010, 33, 198–208. [Google Scholar] [CrossRef] [PubMed]
- Ghezzi, E.S.; Sharman, R.L.S.; Selvanayagam, J.B.; Psaltis, P.J.; Sanders, P.; Astley, J.M.; Knayfati, S.; Batra, V.; Keage, H.A.D. Burden of mood symptoms and disorders in implantable cardioverter defibrillator patients: A systematic review and meta-analysis of 39,954 patients. Europace 2023, 25, euad130. [Google Scholar] [CrossRef] [PubMed]
- Berg, S.K.; Thygesen, L.C.; Svendsen, J.H.; Christensen, A.V.; Zwisler, A.D. Anxiety predicts mortality in ICD patients: Results from the cross-sectional national CopenHeartICD survey with register follow-up. Pacing Clin. Electrophysiol. 2014, 37, 1641–1650. [Google Scholar] [CrossRef]
- Huang, Y.; Zhao, N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Res. 2020, 288, 112954. [Google Scholar] [CrossRef]
- Pasin, L.; Sella, N.; Correale, C.; Bscolo, A.; Mormando, G.; Zordan, M.; Landoni, G.; Navalesi, P. Pandemic COVID-19: The residents’ resilience. Acta Biomed. 2020, 91, e2020120. [Google Scholar]
- Nguyen, H.T.; Do, B.N.; Pham, K.M.; Kim, G.B.; Dam, H.T.B.; Ngyuen, T.T.; Ngyuen, T.T.P.; Ngyuen, Y.H.; Sorensen, K.; Pleasant, A.; et al. Fear of COVID-19 Scale—Associations of Its Scores with Health Literacy and Health-Related Behaviors among Medical Students. Int. J. Environ. Res. Public. Health 2020, 17, 4164. [Google Scholar] [CrossRef]
- Wieteska-Milek, M.; Szmit, S.; Florczyk, M.; Kusmierczyk-Droszcz, B.; Ryczek, R.; Dzienisiewicz, M.; Torbicki, A.; Kurzyna, M. Fear of COVID-19, Anxiety and Depression in Patients with Pulmonary Arterial Hypertension and Chronic Thromboembolic Pulmonary Hypertension during the Pandemic. J. Clin. Med. 2021, 10, 4195. [Google Scholar] [CrossRef] [PubMed]
- Crawford, J.R.; Henry, J.D. The Positive and Negative Affect Schedule (PANAS): Construct validity, measurement properties and normative data in a large non-clinical sample. Br. J. Clin. Psychol. 2004, 43, 245–265. [Google Scholar] [CrossRef] [PubMed]
- Clark, L.A.; Watson, D. Tripartite model of anxiety and depression: Psychometric evidence and taxonomic implications. J. Abnorm. Psychol. 1991, 100, 316–336. [Google Scholar] [CrossRef] [PubMed]
- Ahorsu, D.K.; Lin, C.-Y.; Imani, V.; Saffari, M.; Griffiths, M.D.; Pakpour, A.H. The Fear of COVID-19 Scale: Development and Initial Validation. Int. J. Ment. Health Addict. 2022, 20, 1537–1545. [Google Scholar] [CrossRef] [PubMed]
- Shin, C.; Lee, S.-H.; Han, K.-M.; Yoon, H.-K.; Han, C. Comparison of the Usefulness of the PHQ-8 and PHQ-9 for Screening for Major Depressive Disorder: Analysis of Psychiatric Outpatient Data. Psychiatry Investig. 2019, 16, 300–305. [Google Scholar] [CrossRef] [PubMed]
- Spitzer, R.L.; Korenke, K.; Williams, J.B.W.; Löwe, B. A Brief Measure for Assessing Generalized Anxiety Disorder. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [PubMed]
- Plummer, F.; Manea, L.; Trepel, D.; McMillan, D. Screening for anxiety disorders with the GAD-7 and GAD-2: A systematic review and diagnostic metaanalysis. Gen. Hosp. Psychiatry 2016, 39, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Foa, E.B.; Cashman, L.; Jaycox, L.; Perry, K. The Validation of a Self-Report Measure of Posttraumatic Stress Disorder: The Posttraumatic Diagnostic Scale. Psychol. Assess. 1997, 9, 445–451. [Google Scholar] [CrossRef]
- McCarthy, S. Post-Traumatic Stress Diagnostic Scale (PDS). Occup. Med. 2008, 58, 379. [Google Scholar] [CrossRef]
- Coffey, S.F.; Gudmundsdottir, B.; Beck, J.G.; Palyo, S.A.; Miller, L. Screening for PTSD in Motor Vehicle Accident Survivors Using the PSS-SR and IES*. J. Trauma. Stress 2006, 19, 119–128. [Google Scholar] [CrossRef]
- Sin, G.-L.; Abdin, E.; Lee, J. The PSS-SR as a screening tool for PTSD in first-episode psychosis patients. Early Interv. Psychiatry 2012, 6, 191–194. [Google Scholar] [CrossRef] [PubMed]
- Rottmann, N.; Skov, O.; Andersen, C.M.; Theuns, D.A.M.J.; Pedersen, S.S. Psychological distress in patients with an implantable cardioverter defibrillator and their partners. J. Psychosom. Res. 2018, 113, 16–21. [Google Scholar] [CrossRef] [PubMed]
- Vaglio, J.; Conard, M.; Poston, W.S.; O’Keefe, J.; Haddock, C.K.; House, J.; Spertus, J.A. Testing the performance of the ENRICHD Social Support Instrument in cardiac patients. Health Qual. Life Outcomes 2004, 2, 24. [Google Scholar] [CrossRef] [PubMed]
- Schug, C.; Morawa, E.; Geiser, F.; Hiebel, N.; Beschoner, P.; Jerg-Bretzke, L.; Albus, C.; Weidner, K.; Steudte-Schmiedgen, S.; Borho, A.; et al. Social Suport and Optimism as Protective Factors for Mental Health among 7765 Healthcare Workers in Germany during the COVID-19 Pandemic: Results of the VOICE Study. Int. J. Environ. Res. Public. Health 2021, 18, 3827. [Google Scholar] [CrossRef] [PubMed]
- Kutner, M.H. Applied Linear Statistical Models; McGraw-Hill Irwin: Boston, MA, USA, 2005; p. 410. [Google Scholar]
- Magyar-Russell, G.; Thombs, B.D.; Cai, J.X.; Bavejy, T.; Kuhl, E.A.; Singh, P.P.; Barroso, M.M.B.; Arthurs, E.; Roseman, M.; Amin, N.; et al. The prevalence of anxiety and depression in adults with implantable cardioverter defibrillators: A systematic review. J. Psychosom. Res. 2011, 71, 223–231. [Google Scholar] [CrossRef] [PubMed]
- Baxter, A.J.; Scott, K.M.; Vos, T.; Whiteford, H.A. Global prevalence of anxiety disorders: A systematic review and meta-regression. Psychol. Med. 2013, 43, 897–910. [Google Scholar] [CrossRef] [PubMed]
- Lim, G.Y.; Tam, W.W.; Lu, Y.; Ho, C.S.; Zhang, M.W.; Ho, R.C. Prevalence of Depression in the Community from 30 Countries between 1994–2014. Sci. Rep. 2018, 8, 2861. [Google Scholar] [CrossRef] [PubMed]
- Perkonigg, A.; Kessler, R.C.; Storz, S.; Wittchen, H.U. Traumatic events and post-traumatic stress disorder in the community: Prevalence, risk facotrs and comorbidity. Acta Psychiatr. Scand. 2000, 101, 46–59. [Google Scholar] [CrossRef]
- Morin, C.M.; Bjorvatn, B.; Chung, F.; Holzinger, B.; Partinen, M.; Penzel, T.; Ivers, H.; Wing, Y.K.; Chan, N.Y.; Merikanto, I.; et al. Insomnie, anxiety, and depression during the COVID-19 pandemic: An international collaborative study. Sleep Med. 2021, 87, 38–45. [Google Scholar] [CrossRef]
- Ettman, C.K.; Abdalla, S.M.; Cohen, G.H.; Sampson, L.; Vivier, P.M.; Galea, S. Prevalence of Depression Symptoms in US Adults before and during the COVID-19 Pandemic. JAMA Netw. Open 2020, 3, e2019686. [Google Scholar] [CrossRef]
- Chamaa, F.; Bahmad, H.F.; Darwish, B.; Kobeissi, J.M.; Hoballah, M.; Nassif, S.B.; Ghandour, Y.; Saliba, J.-P.; Lawand, N.; Abou-Kheir, W. PTSD in the COVID-19 era. Curr. Neuropharmacol. 2021, 19, 2164–2179. [Google Scholar] [CrossRef] [PubMed]
- Park, D.H.; Fuge, J.; Meltendorf, T.; Kahl, K.G.; Richter, M.J.; Gall, H.; Ghofrani, H.A.; Kamp, J.C.; Hoeper, M.M.; Olsson, K.M. Impact of SARS-CoV-2-Pandemic on Mental Disorders and Quality of Life in Patients with Pulmonary Arterial Hypertension. Front. Psychiatry 2021, 12, 668647. [Google Scholar] [CrossRef] [PubMed]
- Kayser, M.Z.; Valtin, C.; Greer, M.; Karow, B.; Fuge, J.; Gottlieb, J. Video consultation during the COVID-19 pandemic: A single center’s experience with lung transplant recipients. Telemed. J. E Health 2020, 27, 807–815. [Google Scholar] [CrossRef] [PubMed]
- Evren, C.; Evren, B.; Dalbudak, E.; Topcu, M.; Kutlu, N. Measuring anxiety related to COVID-19: A Turkish validation study of the Coronavirus Anxiety Scale. Death Stud. 2022, 46, 1052–1058. [Google Scholar] [CrossRef] [PubMed]
- Freedenberg, V.; Thomas, S.A.; Friedman, E. Anxiety and depression in implanted cardioverter-defibrillator recipients and heart failure: A review. Heart Fail. Clin. 2011, 7, 59–68. [Google Scholar] [CrossRef] [PubMed]
- Thylen, I.; Dekker, R.L.; Jaarsma, T.; Strömberg, A.; Moser, D.K. Characteristics associated with anxiety, depressive symptoms, and quality-of-life in a large cohort of implantable cardioverter defibrillator recipients. J. Psychosom. Res. 2014, 77, 122–127. [Google Scholar] [CrossRef] [PubMed]
- Mastenbroek, M.H.; Denollet, J.; Versteeg, H.; van den Broek, K.C.; Theuns, D.A.M.J.; Meine, M.; Zijlstra, W.P.; Pedersen, S.S. Trajectories of patient-reported health status in patients with an implantable cardioverter defibrillator. Am. J. Cardiol. 2015, 115, 771–777. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S. Social relationships and health. Am. Psychol. 2004, 59, 676–684. [Google Scholar] [CrossRef] [PubMed]
- Elmer, T.; Boda, Z.; Stadtfeld, C. The co-evolution of emotional well-being with weak and strong friendship ties. Netw. Sci. 2017, 5, 278–307. [Google Scholar] [CrossRef]
- Allemann, H.; Strömberg, A.; Thylen, I. Perceived Sovial Support in Persons with Heart Failure Living with an Implantable Cardioverter Defibrillator: A Cross-sectional Explorative Study. J. Cardiovasc. Nurs. 2018, 33, E1–E8. [Google Scholar] [CrossRef]
- Lang, S.; Becker, R.; Wilke, S.; Hartmann, M.; Herzog, W.; Löwe, B. Anxiety disorders in patients with implantable cardioverter defibrillators: Frequency, course, predictors, and patients’ requests for treatment. Pacing Clin. Electrophysiol. 2014, 37, 35–47. [Google Scholar] [CrossRef] [PubMed]
- Cunha, L.F.; Pellanda, L.C.; Reppold, C.T. Positive Psychology and Gratitude Interventions: A Randomized Clinical Trial. Front. Psychol. 2019, 10, 584. [Google Scholar] [CrossRef] [PubMed]
- Berg, S.K.; Herning, M.; Thygesen, L.C.; Cromhout, P.F.; Wagner, M.K.; Nielsen, K.M.; Christensen, A.V.; Rasmussen, T.B. Do patients with ICD who report anxiety symptoms on Hospital Anxiety Depression Scale suffer from anxiety? J. Psychosom. Res. 2019, 121, 100–104. [Google Scholar] [CrossRef] [PubMed]
- Schulze, J.B.; Günther, M.P.; Riemenschnitter, C.; Wicki, A.; von Känel, R.; Euler, S. Distinct psycho-oncological support inclinations and needs in patients with cancer: A large sample latent class analysis approach. Gen. Hosp. Psychiatry 2022, 75, 17–22. [Google Scholar] [CrossRef]
| Overall (n = 363) | Women (n = 93) | Men (n = 270) | p-Value (p < 0.05) Group Analysis | p-Value Subgroup Analysis | |
|---|---|---|---|---|---|
| Age (y), mean (SD) | 57.96 (13.78) | 52.04 (14.76) | 59.99 (12.83) | <0.001 | |
| Educational status | n = 358 (%) | n = 92 | n = 266 | 0.007 | p < 0.00625 |
| Lower than completed apprenticeship or equivalent | 14 (3.91) | 9 (9.78) | 5 (1.87) | <0.001 | |
| Completed apprenticeship or equivalent | 205 (57.26) | 49 (53.26) | 155 (58.27) | 0.402 | |
| High-school diploma or equivalent | 52 (14.52) | 16 (17.39) | 36 (13.53) | 0.365 | |
| University degree | 88 (24.58) | 18 (19.56) | 70 (26.31) | 0.194 | |
| Civil status | n = 358 (%) | n = 92 | n = 266 | 0.246 | p < 0.00625 |
| Married | 227 (63.40) | 53 (57.60) | 173 (65.03) | 0.203 | |
| Divorced | 54 (15.08) | 19 (20.65) | 35 (13.15) | 0.083 | |
| Widowed | 14 (3.91) | 5 (5.43) | 9 (3.38) | 0.381 | |
| Single | 64 (17.87) | 15 (16.30) | 49 (18.42) | 0.647 | |
| Work status | n = 358 (%) | n = 92 | n = 266 | <0.001 | p < 0.00625 |
| Full time | 99 (27.65) | 12 (13.04) | 87 (32.70) | <0.001 | |
| Part time | 66 (18.43) | 37 (40.21) | 29 (10.90) | <0.001 | |
| Unemployed | 41 (11.45) | 16 (17.39) | 24 (9.02) | 0.028 | |
| Retired | 153 (42.73) | 27 (29.34) | 126 (47.36) | 0.002 |
| Overall (n = 363) | Women (n = 93) | Men (n = 270) | p-Value (p < 0.05) | |
|---|---|---|---|---|
| Smoking | n = 357 (%) 42 (11.76) | n = 92 9 (9.78) | n = 265 33 (12.45) | 0.493 |
| Past myocardial infarction | n = 351 (%) 137 (39.03) | n = 88 14 (15.90) | n = 263 123 (46.76) | <0.001 |
| Number of ICD shocks in the past, mean (SD) | n = 336 1.14 (5.44) | n = 86 1.28 (3.78) | n = 250 1.10 (5.92) | 0.782 |
| History of COVID-19 | n = 228 (%) 67 (29.38) | n = 59 18 (30.50) | n = 169 49 (28.99) | 0.826 |
| Overall; Median (Range) or Mean (SD) | Women | Men | p-Value (p < 0.05) | |
|---|---|---|---|---|
| Level of fear of COVID-19 (FCV-19S) | n = 357 11 (7–35) 11.94 (4.85) | n = 90 12 (7–28) 12.88 (5.21) | n = 267 10 (7–35) 11.64 (4.68) | 0.036 |
| GAD-7 | n = 348 | n = 91 | n = 257 | |
| 2 (0–21) | 3 (0–19) | 1 (0–21) | ||
| 3.29 (4.19) | 4.04 (4.12) | 3.02 (4.20) | 0.048 | |
| GAD-7 score ≥ 10, n (%) | 32 (9.19) | 11 (12.08) | 21 (8.17) | 0.266 |
| PHQ-8 | n = 350 | n = 87 | n = 263 | |
| 4 (0–23) | 5 (0–17) | 3 (0–23) | ||
| 4.53 (4.03) | 5.14 (3.66) | 4.34 (4.14) | 0.115 | |
| PHQ-8 score ≥ 10, n (%) | 38 (10.85) | 9 (10.34) | 29 (11.02) | 0.859 |
| PDS | n = 354 | n = 91 | n = 263 | |
| 2 (0–41) | 5 (0–41) | 2 (0–40) | ||
| 5.60 (8.09) | 7.95 (9.25) | 4.78 (7.50) | 0.004 | |
| PDS score ≥ 14, n (%) | 46 (12.99) | 16 (17.58) | 30 (11.40) | 0.131 |
| FCV-19S Items | Overall (n = 357); Median (Range) or Mean (SD) | Women (n = 90) | Men (n = 267) | p-Value (p < 0.05) |
|---|---|---|---|---|
| 1 I am most afraid of coronavirus-19 | 2 (1–5) 2.34 (1.19) | 2 (1–5) 2.39 (1.20) | 2 (1–5) 2.00 (1.18) | 0.652 |
| score ≥ 4 (agree or strongly agree), n (%) | 71 (19.88) | 18 (20.0) | 53 (19.85) | |
| 2 It makes me uncomfortable to think about coronavirus-19 | 2 (1–5) 2.18 (1.17) | 2 (1–5) 2.41 (1.19) | 2 (1–5) 2.11 (1.15) | 0.032 |
| score ≥ 4, n (%) | 63 (17.64) | 20 (22.22) | 43 (16.10) | |
| 3 My hands become clammy when I think about coronavirus-19 | 1 (1–5) 1.25 (1.09) | 1 (1–4) 1.32 (0.71) | 1 (1–5) 1.23 (0.63) | 0.291 |
| score ≥ 4, n (%) | 5 (1.40) | 2 (2.22) | 3 (1.12) | |
| 4 I am afraid of losing my life because of coronavirus-19 | 2 (1–5) 1.88 (1.09) | 2 (1–5) 2.02 (1.10) | 1 (1–5) 1.83 (1.09) | 0.162 |
| score ≥ 4, n (%) | 32 (8.96) | 8 (8.88) | 24 (8.98) | |
| 5 When watching news and stories about coronavirus-19 on social media, I become nervous or anxious | 1 (1–5) 1.74 (1.01) | 2 (1–5) 1.96 (1.07) | 1 (1–5) 1.67 (0.99) | 0.023 |
| score ≥ 4, n (%) | 31 (8.68) | 11 (12.22) | 20 (7.49) | |
| 6 I cannot sleep because I am worrying about getting coronavirus-19 | 1 (1–5) 1.29 (0.68) | 1 (1–5) 1.41 (0.87) | 1 (1–5) 1.25 (0.61) | 0.102 |
| score ≥ 4, n (%) | 9 (2.52) | 5 (5.55) | 4 (1.49) | |
| 7 My heart races or palpitates when I think about getting coronavirus-19 | 1 (1–5) 1.30 (0.67) | 1 (1–4) 1.39 (0.71) | 1 (1–5) 1.27 (0.66) | 0.156 |
| score ≥ 4, n (%) | 7 (1.96) | 2 (2.22) | 5 (1.87) |
| FCV-19S; Mean (SD) | GAD-7 | PHQ-8 | PDS | |
|---|---|---|---|---|
| Age | p *** | p ** | p *** | |
| Age < 65 years | 12.29 (5.06) | 4.05 (4.64) | 4.96 (4.35) | 6.69 (9.15) |
| ≥65 years | 11.36 (4.37) | 1.87 (2.77) | 3.73 (3.28) | 3.60 (5.24) |
| Educational status | p * | |||
| Lower than completed apprenticeship or equivalent | 12.15 (6.12) | 4.35 (5.95) | 4.92 (4.60) | 7.71 (10.63) |
| Completed apprenticeship or equivalent | 12.17 (5.27) | 3.26 (4.04) | 4.35 (3.73) | 5.39 (8.02) |
| High-school diploma or equivalent | 12.73 (4.49) | 3.78 (5.08) | 6.18 (5.52) | 7.79 (9.50) |
| University degree | 11.02 (3.68) | 2.96 (3.62) | 3.90 (3.32) | 4.55 (6.72) |
| Civil status | ||||
| Married | 11.85 (4.70) | 3.04 (3.81) | 4.29 (3.86) | 4.70 (6.91) |
| Divorced | 13.15 (5.27) | 3.86 (4.88) | 5.37 (4.56) | 7.61 (9.91) |
| Widowed | 12.07 (5.34) | 2.15 (3.13) | 4.50 (3.68) | 5.23 (7.99) |
| Single | 11.27 (4.84) | 3.51 (4.75) | 4.51 (4.19) | 6.53 (9.44) |
| Work status | p *** | p *** | p *** | p *** |
| Full time | 10.74 (3.48) | 2.78 (3.39) | 3.68 (3.39) | 4.04 (5.83) |
| Part time | 12.34 (4.60) | 3.59 (3.61) | 4.79 (3.14) | 5.94 (8.35) |
| Unemployed | 15.03 (6.53) | 6.51 (6.78) | 7.23 (6.31) | 10.58 (13.33) |
| Retired | 11.70 (4.87) | 2.60 (3.57) | 4.27 (3.75) | 5.08 (6.86) |
| FCV-19S; Mean (SD) | GAD-7 | PHQ-8 | PDS | |
|---|---|---|---|---|
| Smoking | ||||
| yes | 12.69 (5.68) | 3.90 (4.77) | 5.29 (4.91) | 6.51 (9.10) |
| no | 11.88 (4.74) | 3.19 (4.00) | 4.38 (3.82) | 5.41 (7.89) |
| Past myocardial infarction | ||||
| yes | 12.12 (5.08) | 3.26 (4.18) | 4.68 (4.13) | 5.33 (8.24) |
| no | 11.80 (4.69) | 3.25 (4.16) | 4.47 (4.01) | 5.79 (8.02) |
| ICD shocks | p * | |||
| yes | 12.30 (5.69) | 3.75 (4.24) | 4.69 (3.91) | 7.21 (9.23) |
| no | 11.81 (4.49) | 3.09 (4.17) | 4.45 (4.10) | 4.89 (7.48) |
| History of COVID-19 | p * | |||
| yes | 10.70 (4.29) | 4.22 (4.97) | 5.60 (4.68) | 6.61 (8.62) |
| no | 12.38 (4.92) | 3.20 (3.77) | 4.61 (3.65) | 5.89 (8.13) |
| GAD | MDD | PTSD | ||||
|---|---|---|---|---|---|---|
| Variables | OR (95% CI) | p-Value | OR (95% CI) | p-Value | OR (95% CI) | p-Value |
| Male sex | 0.74 (0.27 to 1.97) | 0.548 | 0.55 (0.20 to 1.49) | 0.242 | 0.99 (0.42 to 2.34) | 0.990 |
| Age | 0.95 (0.91 to 0.99) | 0.017 | 0.97 (0.93 to 1.01) | 0.277 | 0.92 (0.88 to 0.95) | <0.001 |
| Higher educational status | 0.68 (0.41 to 1.15) | 0.154 | 1.05 (0.67 to 1.64) | 0.831 | 0.78 (0.51 to 1.21) | 0.279 |
| Social support | 0.91 (0.85 to 0.98) | 0.017 | 0.88 (0.83 to 0.94) | <0.001 | 0.91 (0.85 to 0.97) | 0.003 |
| ICD shock number | 1.04 (0.99 to 1.10) | 0.070 | 1.04 (0.99 to 1.09) | 0.077 | 1.05 (0.99 to 1.10) | 0.068 |
| History of COVID-19 | 1.72 (0.51 to 5.75) | 0.374 | 3.58 (1.31 to 9.74) | 0.012 | 1.65 (0.59 to 4.60) | 0.335 |
| Level of fear of COVID-19 | 1.10 (1.03 to 1.19) | 0.005 | 1.12 (1.04 to 1.21) | 0.001 | 1.14 (1.07 to 1.23) | <0.001 |
| Being unemployed | 10.39 (2.37 to 46.25) | 0.002 | 6.54 (1.72 to 24.88) | 0.006 | 3.62 (0.99 to 13.15) | 0.050 |
| Nagelkerke R² | 0.28 | 0.26 | 0.31 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dörner, M.; von Känel, R.; Pazhenkottil, A.P.; Altwegg, R.; Nager, L.; Attanasio, V.; Guth, L.; Zirngast, S.; Menzi, A.; Princip, M.; et al. Fear of COVID-19 Predicts Depression, Anxiety and Post-Traumatic Stress Disorders in Patients with Implantable Cardioverter Defibrillators and Is Mediated by Positive and Negative Affects—A Cross-Sectional Study. J. Clin. Med. 2023, 12, 6884. https://doi.org/10.3390/jcm12216884
Dörner M, von Känel R, Pazhenkottil AP, Altwegg R, Nager L, Attanasio V, Guth L, Zirngast S, Menzi A, Princip M, et al. Fear of COVID-19 Predicts Depression, Anxiety and Post-Traumatic Stress Disorders in Patients with Implantable Cardioverter Defibrillators and Is Mediated by Positive and Negative Affects—A Cross-Sectional Study. Journal of Clinical Medicine. 2023; 12(21):6884. https://doi.org/10.3390/jcm12216884
Chicago/Turabian StyleDörner, Marc, Roland von Känel, Aju P. Pazhenkottil, Rahel Altwegg, Ladina Nager, Veronica Attanasio, Lisa Guth, Sina Zirngast, Anna Menzi, Mary Princip, and et al. 2023. "Fear of COVID-19 Predicts Depression, Anxiety and Post-Traumatic Stress Disorders in Patients with Implantable Cardioverter Defibrillators and Is Mediated by Positive and Negative Affects—A Cross-Sectional Study" Journal of Clinical Medicine 12, no. 21: 6884. https://doi.org/10.3390/jcm12216884
APA StyleDörner, M., von Känel, R., Pazhenkottil, A. P., Altwegg, R., Nager, L., Attanasio, V., Guth, L., Zirngast, S., Menzi, A., Princip, M., & Hackl-Zuccarella, C. (2023). Fear of COVID-19 Predicts Depression, Anxiety and Post-Traumatic Stress Disorders in Patients with Implantable Cardioverter Defibrillators and Is Mediated by Positive and Negative Affects—A Cross-Sectional Study. Journal of Clinical Medicine, 12(21), 6884. https://doi.org/10.3390/jcm12216884







