Risk Factors for Recurrent Exacerbations in the General-Practitioner-Based Swiss Chronic Obstructive Pulmonary Disease (COPD) Cohort
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population and Study Design
- Tiffenau (FEV17FVC) < 70 without reversibility (increase in FEV1 after inhalation of a bronchodilator <200 mL and <12%);
- Age: >40 years;
- Both genders;
- Smokers or ex-smokers with at least 20 pack years;
- Informed consent.
- <40 years of age
- Tiffenau (FEV17FVC) > 70.
2.2. Assessment of Severity of COPD
2.3. COPD Assessment Test (CAT)
2.4. Modified Medical Research Council Dyspnea Scale
2.5. Statistical Analysis
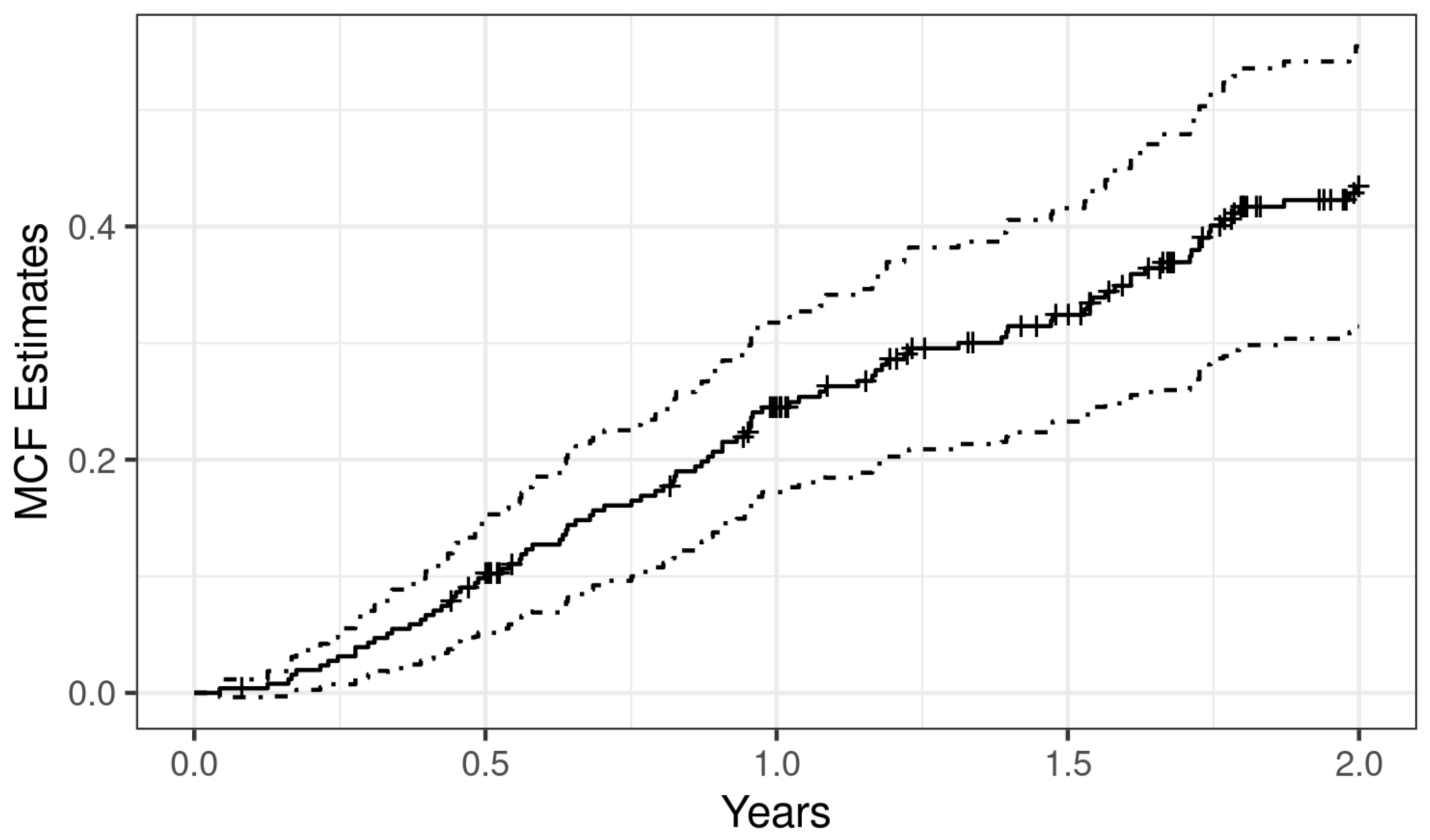
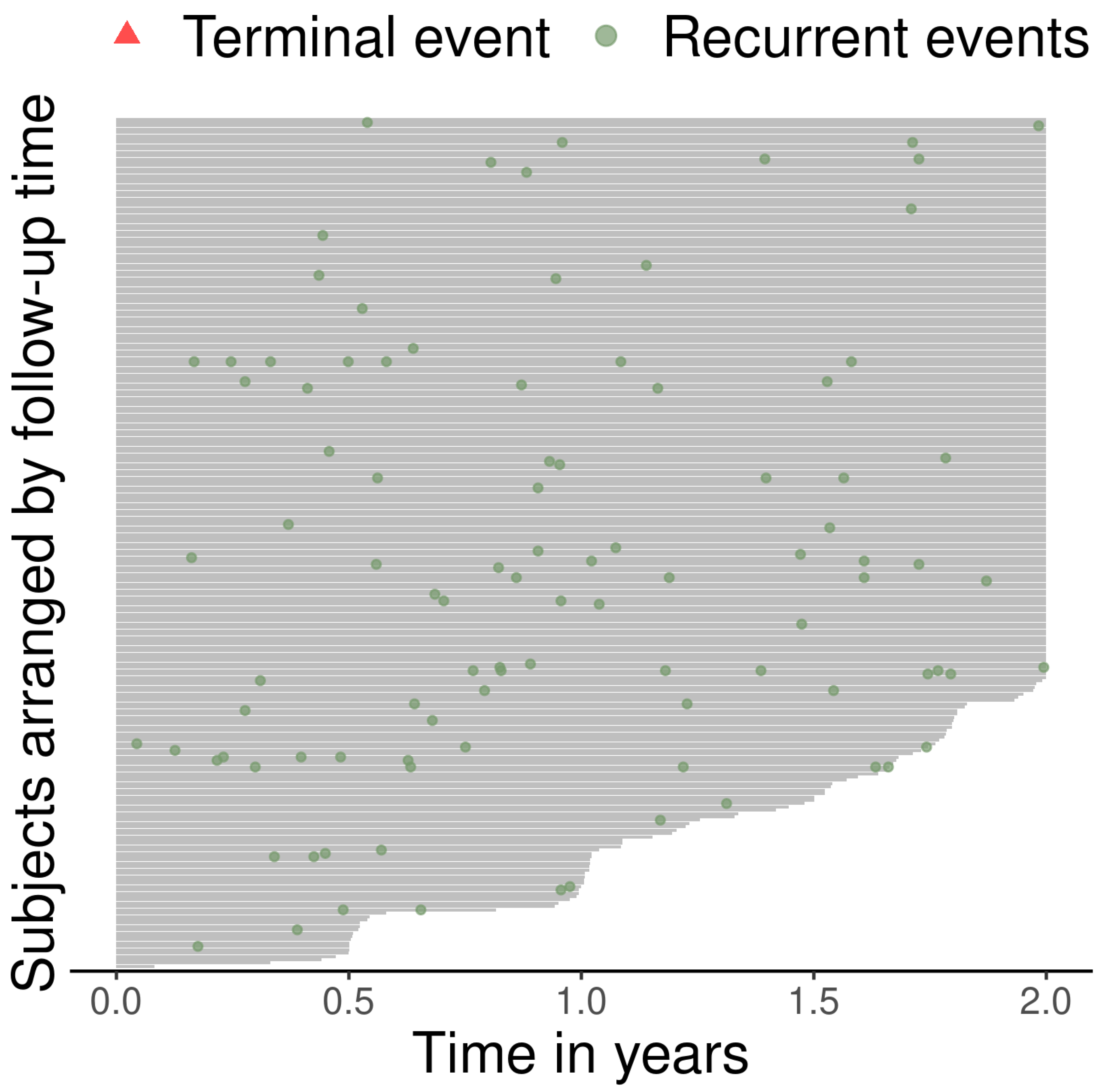
2.6. Description of Recurrent Event Data
2.7. Analysis of Recurrent Event Data Using Negative Binomial Regression
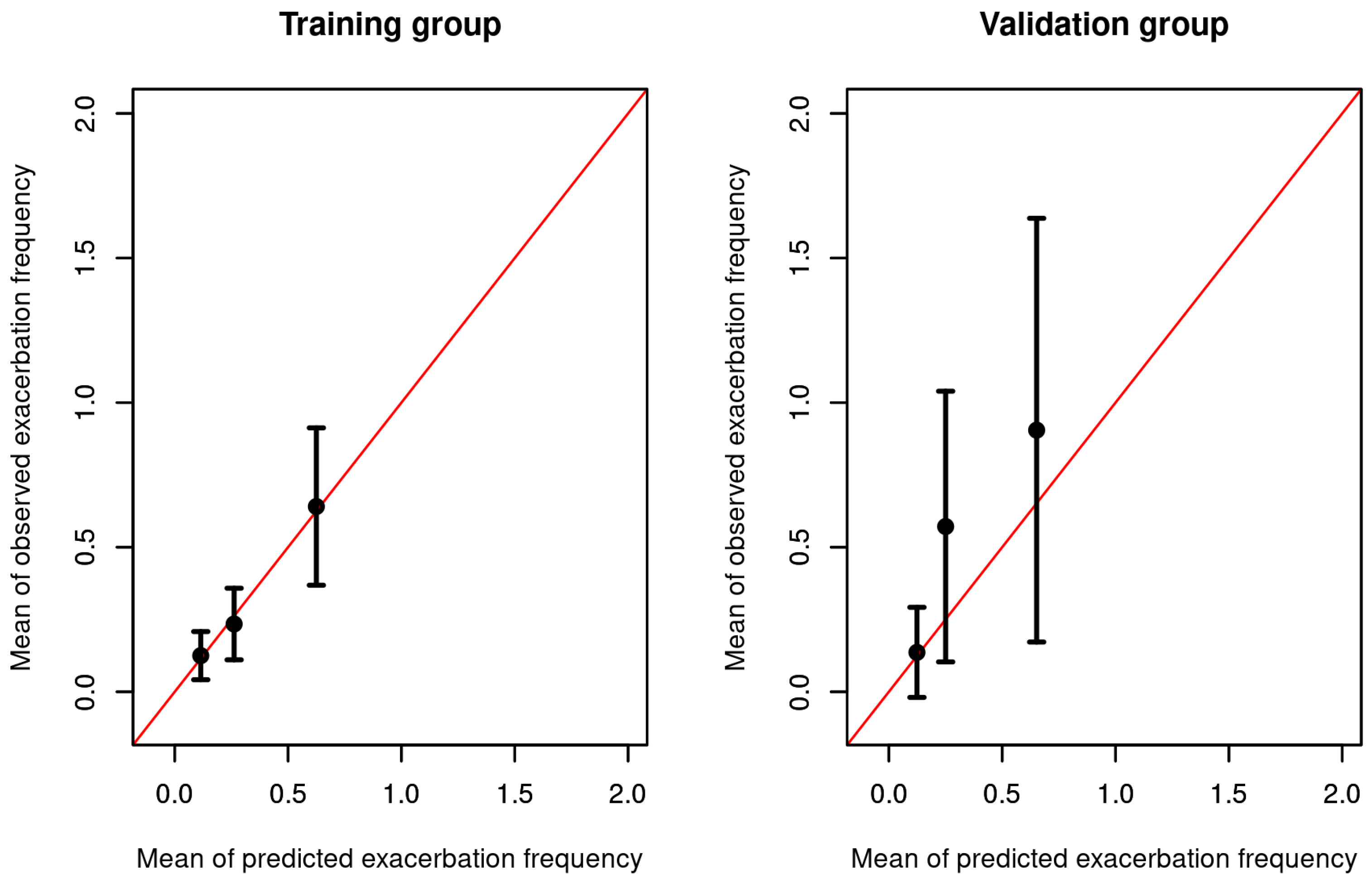
2.8. Assessment of Performance
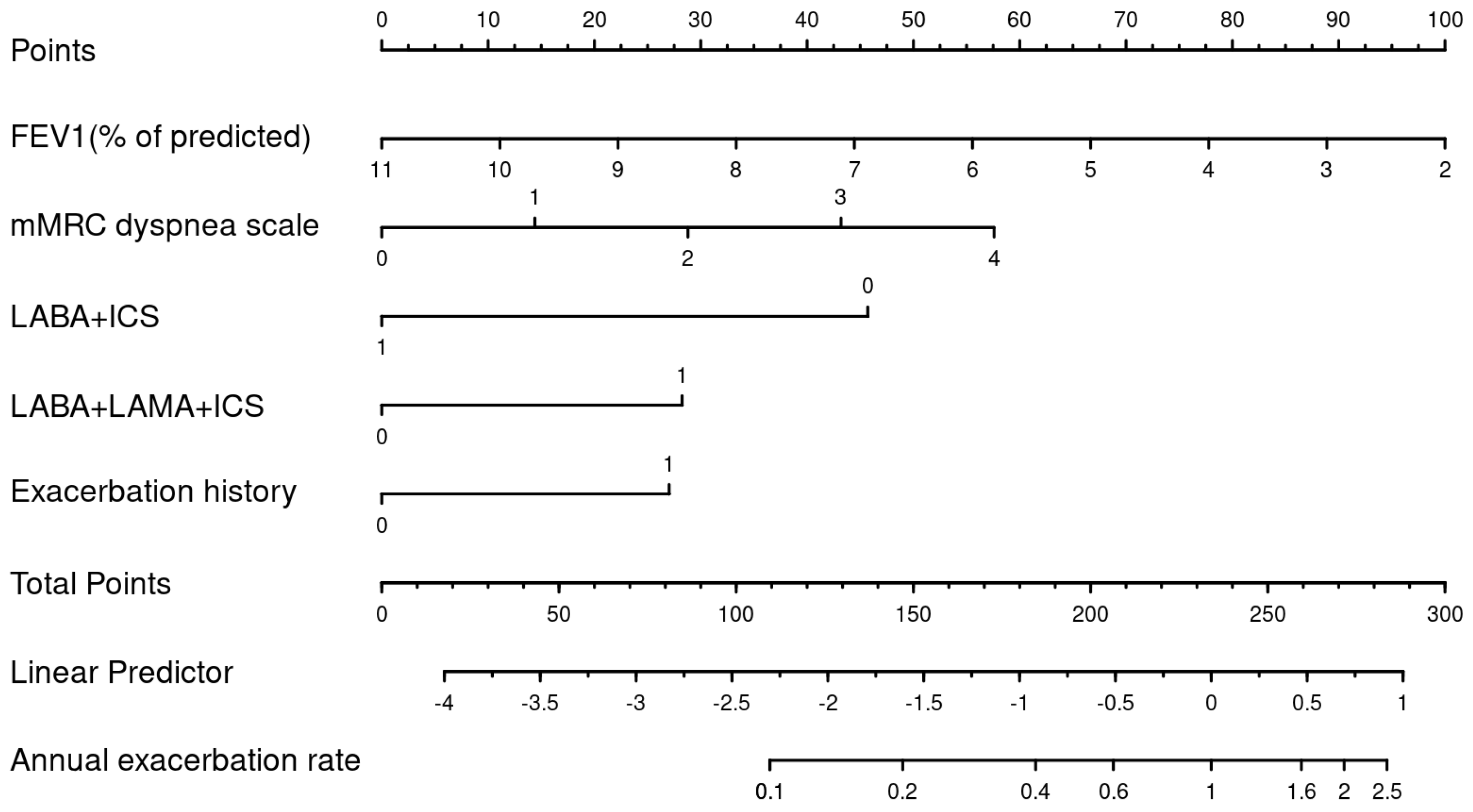
2.9. Nomogram
3. Results
3.1. Demographic and Baseline Data
3.2. Recurrent Event Process
3.3. Factors Associated with Recurrent Exacerbations
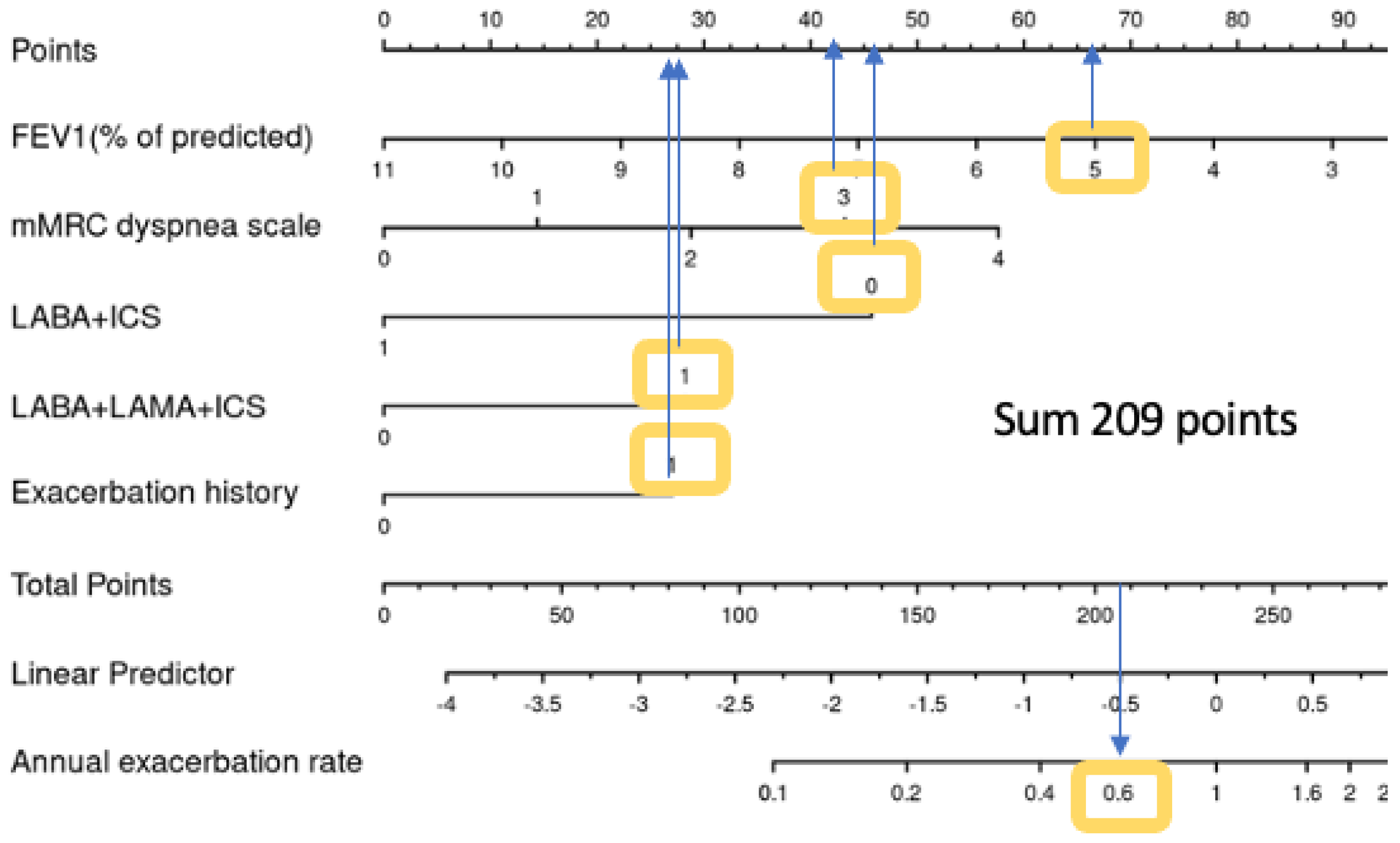
3.4. Nomogram
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| COPD | chronic obstructive pulmonary disease |
| LABA | long-acting beta-agonists |
| LAMA | long-acting muscarinic receptor antagonists |
| ICS | inhaled corticosteroids |
| SABA | short-acting bronchodilators |
| mMRC | Modified Medical Research Council Dyspnea Scale |
References
- World Health Organization. Available online: http://www.who.int (accessed on 11 January 2023).
- Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease; 2021 Report. 2021. Available online: https://staging.goldcopd.org/2021-gold-reports/ (accessed on 7 October 2023).
- Celli, B.R.; MacNee, W.; Force, A.E.T. Standards for the diagnosis and treatment of patients with COPD: A summary of the ATS/ERS position paper. Eur. Respir. J. 2004, 23, 932–946. [Google Scholar] [CrossRef] [PubMed]
- Rabe, K.F.; Hurd, S.; Anzueto, A.; Barnes, P.J.; Buist, S.A.; Calverley, P.; Fukuchi, Y.; Jenkins, C.; Rodriguez-Roisin, R.; van Weel, C.; et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am. J. Respir. Crit. Care Med. 2007, 176, 532–555. [Google Scholar] [CrossRef] [PubMed]
- Jones, R.C.; Donaldson, G.C.; Chavannes, N.H.; Kida, K.; Dickson-Spillmann, M.; Harding, S.; Wedzicha, J.A.; Price, D.; Hyland, M.E. Derivation and validation of a composite index of severity in chronic obstructive pulmonary disease: The DOSE Index. Am. J. Respir. Crit. Care Med. 2009, 180, 1189–1195. [Google Scholar] [CrossRef] [PubMed]
- Siro, C.A.; Bastos, P.G.; Knaus, W.A.; Wagner, D.P. APACHE II scores in the prediction of multiple organ failure syndrome. Arch. Surg. 1991, 126, 528–529. [Google Scholar] [CrossRef]
- Celli, B.R.; Cote, C.G.; Marin, J.M.; Casanova, C.; Montes de Oca, M.; Mendez, R.A.; Plata, V.P.; Cabral, H.J. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N. Engl. J. Med. 2004, 350, 1005–1012. [Google Scholar] [CrossRef]
- Chaudhary, M.F.A.; Hoffman, E.A.; Guo, J.; Comellas, A.P.; Newell, J.D., Jr.; Nagpal, P.; Fortis, S.; Christensen, G.E.; Gerard, S.E.; Pan, Y.; et al. Predicting severe chronic obstructive pulmonary disease exacerbations using quantitative CT: A retrospective model development and external validation study. Lancet Digit. Health 2023, 5, e83–e92. [Google Scholar] [CrossRef]
- Yii, A.C.A.; Loh, C.H.; Tiew, P.Y.; Xu, H.; Taha, A.A.M.; Koh, J.; Tan, J.; Lapperre, T.S.; Anzueto, A.; Tee, A.K. A clinical prediction model for hospitalized COPD exacerbations based on “treatable traits”. Int. J. Chronic Obstr. Pulm. Dis. 2019, 14, 719–728. [Google Scholar] [CrossRef]
- Hoogendoorn, M.; Feenstra, T.L.; Boland, M.; Briggs, A.H.; Borg, S.; Jansson, S.-A.; Risebrough, N.; Slejko, J.F.; Mölken, M.P.R.-V. Prediction models for exacerbations in different COPD patient populations: Comparing results of five large data sources. Int. J. Chronic Obstr. Pulm. Dis. 2017, 12, 3183–3194. [Google Scholar] [CrossRef]
- Safari, A.; Adibi, A.; Sin, D.D.; Lee, T.Y.; Ho, J.K.; Sadatsafavi, M. ACCEPT 2.0: Recalibrating and externally validating the Acute COPD exacerbation prediction tool (ACCEPT). EClinicalMedicine 2022, 51, 101574. [Google Scholar] [CrossRef]
- Jochmann, A.; Neubauer, F.; Miedinger, D.; Schafroth, S.; Tamm, M.; Leuppi, J.D. General practitioner’s adherence to the COPD GOLD guidelines: Baseline data of the Swiss COPD Cohort Study. Swiss Med. Wkly. 2010, 140, w13053. [Google Scholar] [CrossRef]
- Jochmann, A.; Scherr, A.; Jochmann, D.; Miedinger, D.; Schafroth, T.; Chhajed, P.; Tamm, M.; Leuppi, J. Impact of adherence to the GOLD guidelines on symptom prevalence, lung function decline and exacerbation rate in the Swiss COPD cohort. Swiss Med. Wkly. 2012, 142, w13567. [Google Scholar] [CrossRef] [PubMed]
- Stanojevic, S.; Kaminsky, D.A.; Miller, M.R.; Thompson, B.; Aliverti, A.; Barjaktarevic, I.; Cooper, B.G.; Culver, B.; Derom, E.; Hall, G.L.; et al. ERS/ATS technical standard on interpretive strategies for routine lung function tests. Eur. Respir. J. 2022, 60, 2101499. [Google Scholar] [CrossRef] [PubMed]
- Abu Hussein, N.; ter Riet, G.; Schoenenberger, L.; Bridevaux, P.-O.; Chhajed, P.N.; Fitting, J.-W.; Geiser, T.; Jochmann, A.; Zellweger, L.J.; Kohler, M.; et al. The ADO index as a predictor of two-year mortality in general practice-based chronic obstructive pulmonary disease cohorts. Respiration 2014, 88, 208–214. [Google Scholar] [CrossRef] [PubMed]
- Vestbo, J.; Hurd, S.S.; Agustí, A.G.; Jones, P.W.; Vogelmeier, C.; Anzueto, A.; Barnes, P.J.; Fabbri, L.M.; Martinez, F.J.; Nishimura, M.; et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am. J. Respir. Crit. Care Med. 2013, 187, 347–365. [Google Scholar] [CrossRef]
- Jones, P.W.; Harding, G.; Berry, P.; Wiklund, I.; Chen, W.H.; Leidy, N.K. Development and first validation of the COPD Assessment Test. Eur. Respir. J. 2009, 34, 648–654. [Google Scholar] [CrossRef] [PubMed]
- Fletcher, C.M. The clinical diagnosis of pulmonary emphysema; an experimental study. Proc. R. Soc. Med. 1952, 45, 577–584. [Google Scholar]
- Team, R.C.; R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing. 2020. Available online: https://www.r-project.org/ (accessed on 15 September 2021).
- Nelson, W.B. Recurrent Events Data Analysis for Product Repairs, Disease Recurrences, and Other Applications; SIAM: Philadelphia, PA, USA, 2003. [Google Scholar]
- Lawless, J.F.; Nadeau, C. Some simple robust methods for the analysis of recurrent events. Technometrics 1995, 37, 158–168. [Google Scholar] [CrossRef]
- Nelson, W. Confidence limits for recurrence data—Applied to cost or number of product repairs. Technometrics 1995, 37, 147–157. [Google Scholar]
- Chiou, S.H.; Xu, G.; Yan, J.; Huang, C.-Y. Regression Modeling for Recurrent Events Using R Package reReg. arXiv 2021, arXiv:210411708. [Google Scholar]
- Perez, X.; Wisnivesky, J.P.; Lurslurchachai, L.; Kleinman, L.C.; Kronish, I.M. Barriers to adherence to COPD guidelines among primary care providers. Respir. Med. 2012, 106, 374–381. [Google Scholar] [CrossRef]
- Glaab, T.; Vogelmeier, C.; Hellmann, A.; Buhl, R. Guideline-based survey of outpatient COPD management by pulmonary specialists in Germany. Int. J. Chronic Obstr. Pulm. Dis. 2012, 7, 101–108. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Müllerova, H.; Maselli, D.J.; Locantore, N.; Vestbo, J.; Hurst, J.R.; Wedzicha, J.A.; Bakke, P.; Agusti, A.; Anzueto, A. Hospitalized exacerbations of COPD: Risk factors and outcomes in the ECLIPSE cohort. Chest 2015, 147, 999–1007. [Google Scholar] [CrossRef] [PubMed]
- Soler-Cataluna, J.J.; Martinez-Garcia, M.A.; Sanchez, P.R.; Salcedo, E.; Navarro, M.; Ochando, R. Severe acute exacerbations and mortality in patients with chronic obstructive pulmonary disease. Thorax 2005, 60, 925–931. [Google Scholar] [CrossRef] [PubMed]
- Al-ani, S.; Spigt, M.; Hofset, P.; Melbye, H. Predictors of exacerbations of asthma and COPD during one year in primary care. Fam. Pr. 2013, 30, 621–628. [Google Scholar] [CrossRef]
- Sundh, J.; Osterlund Efraimsson, E.; Janson, C.; Montgomery, S.; Stallberg, B.; Lisspers, K. Management of COPD exacerbations in primary care: A clinical cohort study. Prim. Care Respir. J. 2013, 22, 393–399. [Google Scholar] [CrossRef]
- Friedman, M.; Serby, C.W.; Menjoge, S.S.; Wilson, J.D.; Hilleman, D.E.; Witek, T.J., Jr. Pharmacoeconomic evaluation of a combination of ipratropium plus albuterol compared with ipratropium alone and albuterol alone in COPD. Chest 1999, 115, 635–641. [Google Scholar] [CrossRef]
- Kim, V.; Aaron, S.D. What is a COPD exacerbation? Current definitions, pitfalls, challenges and opportunities for improvement. Eur. Respir. J. 2018, 52, 1801261. [Google Scholar] [CrossRef]
- Marshall, D.C.; Al Omari, O.; Goodall, R.; Shalhoub, J.; Adcock, I.M.; Chung, K.F.; Salciccioli, J.D. Trends in prevalence, mortality, and disability-adjusted life-years relating to chronic obstructive pulmonary disease in Europe: An observational study of the global burden of disease database, 2001–2019. BMC Pulm. Med. 2022, 22, 289. [Google Scholar] [CrossRef]
- Rehman, A.U.; Hassali, M.A.A.; Muhammad, S.A.; Harun, S.N.; Shah, S.; Abbas, S. The economic burden of chronic obstructive pulmonary disease (COPD) in Europe: Results from a systematic review of the literature. Eur. J. Health Econ. 2020, 21, 181–194. [Google Scholar] [CrossRef]
- Wilkinson, T.M.; Donaldson, G.C.; Hurst, J.R.; Seemungal, T.A.; Wedzicha, J.A. Early therapy improves outcomes of exacerbations of chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 2004, 169, 1298–1303. [Google Scholar] [CrossRef]
- Muller, D.C.; Johansson, M.; Brennan, P. Lung Cancer Risk Prediction Model Incorporating Lung Function: Development and Validation in the UK Biobank Prospective Cohort Study. J. Clin. Oncol. 2017, 35, 861–869. [Google Scholar] [CrossRef]
- Wells, P.S.; Anderson, D.R.; Rodger, M.; Ginsberg, J.S.; Kearon, C.; Gent, M.; Turpie, A.G.; Bormanis, J.; Weitz, J.; Chamberlain, M.; et al. Derivation of a simple clinical model to categorize patients probability of pulmonary embolism: Increasing the models utility with the SimpliRED D-dimer. Thromb. Haemost. 2000, 83, 416–420. [Google Scholar]
- Celli, B.R. Change in the BODE index reflects disease modification in COPD: Lessons from lung volume reduction surgery. Chest 2006, 129, 835–836. [Google Scholar] [CrossRef]
- Kate, R.J.; Pearce, N.; Mazumdar, D.; Nilakantan, V. A continual prediction model for inpatient acute kidney injury. Comput. Biol. Med. 2020, 116, 103580. [Google Scholar] [CrossRef] [PubMed]
- Adibi, A.; Sin, D.D.; Safari, A.; Johnson, K.M.; Aaron, S.D.; FitzGerald, J.M.; Sadatsafavi, M. The Acute COPD Exacerbation Prediction Tool (ACCEPT): A modelling study. Lancet Respir. Med. 2020, 8, 1013–1021. [Google Scholar] [CrossRef] [PubMed]
- Bertens, L.; Reitsma, J.B.; Moons, K.G.; Mourik, v.; Broekhuizen, B.D.; Hoes, A.W.; Rutten, F.H.; Lammers, J.W.J. Development and validation of a model to predict the risk of exacerbations in chronic obstructive pulmonary disease. Int. J. Chronic Obstr. Pulm. Dis. 2013, 8, 493–499. [Google Scholar] [CrossRef] [PubMed]
- Donaldson, G.C.; Goldring, J.J.; Wedzicha, J.A. Influence of season on exacerbation characteristics in patients with COPD. Chest 2012, 141, 94–100. [Google Scholar] [CrossRef]
- Donaldson, G.C.; Hurst, J.R.; Smith, C.J.; Hubbard, R.B.; Wedzicha, J.A. Increased risk of myocardial infarction and stroke following exacerbation of COPD. Chest 2010, 137, 1091–1097. [Google Scholar] [CrossRef]
- Puhan, M.A.; Garcia-Aymerich, J.; Frey, M.; ter Riet, G.; Anto, J.M.; Agusti, A.G.; Gómez, F.P.; Rodríguez-Roisín, R.; Moons, K.G.; Kessels, A.G.; et al. Expansion of the prognostic assessment of patients with chronic obstructive pulmonary disease: The updated BODE index and the ADO index. Lancet 2009, 374, 704–711. [Google Scholar] [CrossRef]
- Puhan, M.A.; Hansel, N.N.; Sobradillo, P.; Enright, P.; Lange, P.; Hickson, D.; Menezes, A.M.; Riet, G.T.; Held, U.; Domingo-Salvany, A.; et al. Large-scale international validation of the ADO index in subjects with COPD: An individual subject data analysis of 10 cohorts. BMJ Open 2012, 2, e002152. [Google Scholar] [CrossRef]

| General Characteristics | All Patients | Training Dataset | Validation Dataset | p Value |
|---|---|---|---|---|
| N total | 256 | 192 | 64 | |
| Age (years), Mean (SD) | 67.62 (10.17) | 67.86 (10.25) | 66.88 (9.95) | 0.496 |
| BMI (kg/m2), Mean (SD) | 26.93 (6.07) | 26.88 (6.35) | 27.09 (5.21) | 0.786 |
| Male sex | 162 (63.28%) | 120 (62.5%) | 42 (65.62%) | 0.765 |
| Current smoker | 125 (48.83%) | 92 (47.92%) | 33 (51.56%) | 0.718 |
| Lung function | ||||
| FEV1 (% of predicted), Mean (SD) | 59.57 (18.15) | 59.79 (18.6) | 58.91 (16.87) | 0.725 |
| FVC (% of predicted), Mean (SD) | 84.34 (22.51) | 84.83 (23.74) | 82.88 (18.43) | 0.496 |
| FEV1/FVC, Mean (SD) | 56.09 (9.75) | 55.93 (9.65) | 56.57 (10.1) | 0.658 |
| GOLD 1 | 38 (14.84%) | 31 (16.15%) | 7 (10.94%) | 0.708 |
| GOLD 2 | 139 (54.3%) | 101 (52.6%) | 38 (59.38%) | |
| GOLD 3 | 68 (26.56%) | 52 (27.08%) | 16 (25%) | |
| GOLD 4 | 11 (4.3%) | 8 (4.17%) | 3 (4.69%) | |
| Symptoms | ||||
| mMRC dyspnea scale 0 | 22 (8.59%) | 15 (7.81%) | 7 (10.94%) | 0.344 |
| mMRC dyspnea scale 1 | 103 (40.23%) | 73 (38.02%) | 30 (46.88%) | |
| mMRC dyspnea scale 2 | 89 (34.77%) | 73 (38.02%) | 16 (25%) | |
| mMRC dyspnea scale 3 | 35 (13.67%) | 25 (13.02%) | 10 (15.62%) | |
| mMRC dyspnea scale 4 | 7 (2.73%) | 6 (3.12%) | 1 (1.56%) | |
| COPD treatment | ||||
| No LAMA, LABA, or ICS | 28 (10.94%) | 22 (11.46%) | 6 (9.38%) | 0.817 |
| On short-acting bronchodilators (SABA) only | 77 (30.08%) | 60 (31.25%) | 17 (26.56%) | 0.582 |
| On long-acting muscarinic antagonists (LAMA) | 43 (16.8%) | 32 (16.67%) | 11 (17.19%) | 1 |
| On long-acting ß2-agonists (LABA) only | 4 (1.56%) | 3 (1.56%) | 1 (1.56%) | 1 |
| On inhaled corticosteroids (ICS) only | 5 (1.95%) | 3 (1.56%) | 2 (3.12%) | 0.794 |
| Inhaled combination therapy (LABA+ICS) | 36 (14.06%) | 24 (12.5%) | 12 (18.75%) | 0.299 |
| Combination therapy (LABA+LAMA) | 79 (30.86%) | 63 (32.81%) | 16 (25%) | 0.31 |
| LABA + LAMA + ICS | 63 (24.61%) | 46 (23.96%) | 17 (26.56%) | 0.802 |
| On systemic corticosteroids | 7 (2.73%) | 6 (3.12%) | 1 (1.56%) | 0.825 |
| O2 therapy previous year | 17 (6.64%) | 10 (5.21%) | 7 (10.94%) | 0.192 |
| Physical activity | ||||
| Exercise (at least twice a week) | 84 (32.81%) | 60 (31.25%) | 24 (37.5%) | 0.442 |
| Pulmonary rehabilitation | 15 (5.86%) | 13 (6.77%) | 2 (3.12%) | 0.442 |
| Comorbidities | ||||
| Asthma | 31 (12.11%) | 21 (10.94%) | 10 (15.62%) | 0.439 |
| Hypertension | 128 (50%) | 98 (51.04%) | 30 (46.88%) | 0.665 |
| Coronary heart disease | 31 (12.11%) | 24 (12.5%) | 7 (10.94%) | 0.912 |
| Heart failure | 13 (5.08%) | 9 (4.69%) | 4 (6.25%) | 0.869 |
| Peripheral artery disease | 21 (8.2%) | 18 (9.38%) | 3 (4.69%) | 0.357 |
| Cerebrovascular Insult | 8 (3.12%) | 5 (2.6%) | 3 (4.69%) | 0.678 |
| Diabetes | 31 (12.11%) | 23 (11.98%) | 8 (12.5%) | 1 |
| Cancer | 10 (3.91%) | 9 (4.69%) | 1 (1.56%) | 0.456 |
| Exacerbation history over the past year | 66 (25.78%) | 49 (25.52%) | 17 (26.56%) | 1 |
| Outcome | ||||
| Exacerbation count: 0 | 193 (75.39%) | 147 (76.56%) | 46 (71.88%) | 0.123 |
| Exacerbation count: 1 | 42 (16.41%) | 33 (17.19%) | 9 (14.06%) | |
| Exacerbation count: 2 | 15 (5.86%) | 9 (4.69%) | 6 (9.38%) | |
| Exacerbation count: 3 | 3 (1.17%) | 1 (0.52%) | 2 (3.12%) | |
| Exacerbation count: 5 | 2 (0.78%) | 2 (1.04%) | 0 (0%) | |
| Exacerbation count: 7 | 1 (0.39%) | 0 (0%) | 1 (1.56%) | |
| Follow-up time (years), Mean (SD) | 193 (75.39%) | 147 (76.56%) | 46 (71.88%) | 0.123 |
| Factors | IRR | 95% CI Lower | 95% CI Upper | p-Value |
|---|---|---|---|---|
| LABA/LAMA/ICS | 2.5 | 1.34 | 4.67 | 0.004 |
| Exacerbation history over the past year | 2.06 | 1.08 | 3.93 | 0.027 |
| mMRC dyspnea scale (per score) | 1.48 | 1.07 | 2.07 | 0.022 |
| Asthma | 1.36 | 0.53 | 3.37 | 0.517 |
| Age (per 10 years) | 1.22 | 0.88 | 1.71 | 0.208 |
| On SABA only | 1.21 | 0.62 | 2.32 | 0.574 |
| BMI (per 10 kg/m2) | 0.88 | 0.53 | 1.43 | 0.614 |
| Hypertension | 0.88 | 0.48 | 1.63 | 0.688 |
| Diabetes | 0.86 | 0.29 | 2.3 | 0.773 |
| On LAMA only | 0.83 | 0.34 | 1.92 | 0.666 |
| Current smoker at baseline | 0.82 | 0.44 | 1.51 | 0.522 |
| On LABA/LAMA | 0.78 | 0.4 | 1.52 | 0.479 |
| Male vs female sex | 0.76 | 0.41 | 1.42 | 0.381 |
| Coronary heart disease | 0.75 | 0.25 | 2 | 0.582 |
| Baseline FEV1 (per 10% of predicted) | 0.74 | 0.62 | 0.88 | 0.001 |
| On LABA + ICS | 0.36 | 0.08 | 1.15 | 0.116 |
| IRR | 2.50% | 97.50% | p-Value | |
|---|---|---|---|---|
| Baseline FEV1 (per 10% of predicted) | 0.81 | 0.68 | 0.97 | 0.027 |
| mMRC dyspnea scale (per score) | 1.3 | 0.94 | 1.81 | 0.123 |
| LABA/ICS | 0.43 | 0.1 | 1.33 | 0.183 |
| LABA/LAMA/ICS | 1.69 | 0.9 | 3.14 | 0.102 |
| Exacerbation history in the past year | 1.65 | 0.89 | 3.02 | 0.108 |
| Number of Exacerbations | AUC | AUC 95% Lower Limit | AUC 95% Lower Limit | Sensitivity at Best Threshold * | Specificity at Best Threshold * |
|---|---|---|---|---|---|
| Training | |||||
| ≥1 | 0.69 | 0.60 | 0.78 | 0.67 | 0.68 |
| ≥2 | 0.86 | 0.76 | 0.96 | 0.83 | 0.82 |
| ≥3 | 0.88 | 0.77 | 0.99 | 1.00 | 0.79 |
| Validation | |||||
| ≥1 | 0.71 | 0.56 | 0.85 | 0.67 | 0.65 |
| ≥2 | 0.78 | 0.62 | 0.93 | 0.89 | 0.55 |
| ≥3 | 0.67 | 0.32 | 1.00 | 1.00 | 0.38 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abu Hussein, N.S.; Giezendanner, S.; Urwyler, P.; Bridevaux, P.-O.; Chhajed, P.N.; Geiser, T.; Joos Zellweger, L.; Kohler, M.; Miedinger, D.; Pasha, Z.; et al. Risk Factors for Recurrent Exacerbations in the General-Practitioner-Based Swiss Chronic Obstructive Pulmonary Disease (COPD) Cohort. J. Clin. Med. 2023, 12, 6695. https://doi.org/10.3390/jcm12206695
Abu Hussein NS, Giezendanner S, Urwyler P, Bridevaux P-O, Chhajed PN, Geiser T, Joos Zellweger L, Kohler M, Miedinger D, Pasha Z, et al. Risk Factors for Recurrent Exacerbations in the General-Practitioner-Based Swiss Chronic Obstructive Pulmonary Disease (COPD) Cohort. Journal of Clinical Medicine. 2023; 12(20):6695. https://doi.org/10.3390/jcm12206695
Chicago/Turabian StyleAbu Hussein, Nebal S., Stephanie Giezendanner, Pascal Urwyler, Pierre-Olivier Bridevaux, Prashant N. Chhajed, Thomas Geiser, Ladina Joos Zellweger, Malcolm Kohler, David Miedinger, Zahra Pasha, and et al. 2023. "Risk Factors for Recurrent Exacerbations in the General-Practitioner-Based Swiss Chronic Obstructive Pulmonary Disease (COPD) Cohort" Journal of Clinical Medicine 12, no. 20: 6695. https://doi.org/10.3390/jcm12206695
APA StyleAbu Hussein, N. S., Giezendanner, S., Urwyler, P., Bridevaux, P.-O., Chhajed, P. N., Geiser, T., Joos Zellweger, L., Kohler, M., Miedinger, D., Pasha, Z., Thurnheer, R., von Garnier, C., & Leuppi, J. D. (2023). Risk Factors for Recurrent Exacerbations in the General-Practitioner-Based Swiss Chronic Obstructive Pulmonary Disease (COPD) Cohort. Journal of Clinical Medicine, 12(20), 6695. https://doi.org/10.3390/jcm12206695






