Changes in the End-of-Life Process in Patients with Life-Limiting Diseases through the Intervention of the Pediatric Palliative Care Team
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Survey
2.2. Definitions
2.3. Statistical Analysis
3. Results
3.1. Patients’ General Characteristics
3.2. Support in the Decision-Making Process
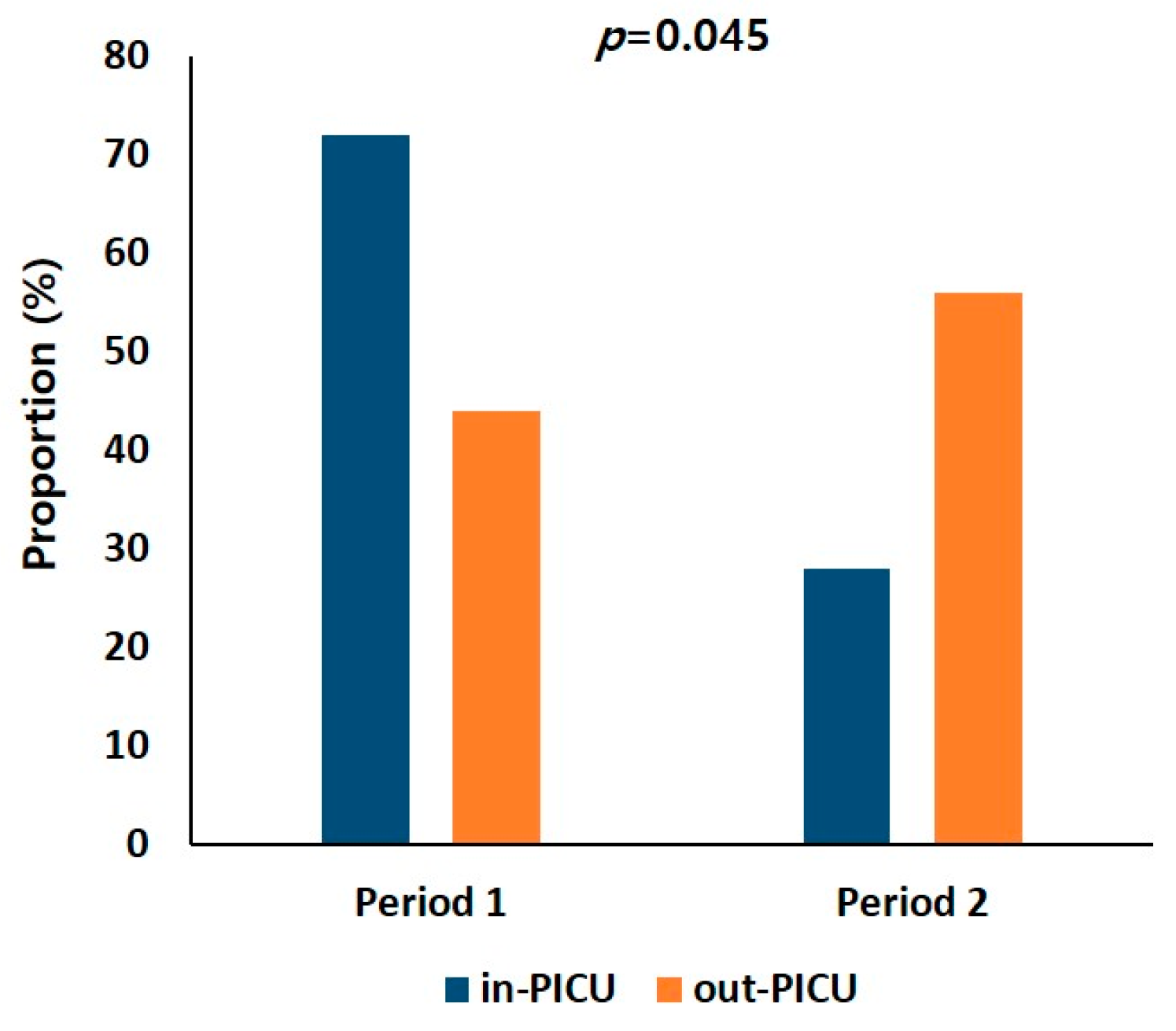
3.3. Change in Place of Death
3.4. Service Satisfaction Survey of Bereaved Families
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chambers, L. A Guide to Children’s Palliative Care; Supporting Babies, Children and Young People with Life-Limiting and Life-Threatening Conditions and Their Families, 4th ed.; Together for Short Lives: Bristol, UK, 2018. [Google Scholar]
- Fraser, L.K.; Parslow, R. Children with life-limiting conditions in paediatric intensive care units: A national cohort, data linkage study. Arch. Dis. Child. 2018, 103, 540–547. [Google Scholar] [CrossRef] [PubMed]
- Spicer, S.; Macdonald, M.E.; Davies, D.; Vadeboncoeur, C.; Siden, H. Introducing a lexicon of terms for paediatric palliative care. Paediatr. Child. Health 2015, 20, 155–156. [Google Scholar] [CrossRef] [PubMed]
- Shin, H.Y.; Kim, M.S.; Kang, S.H.; Kim, C.H.; Moon, Y.J.; Song, I.G. A Practical Guide for Pediatric Advance Care Planning; Seoul National University Children’s Hospital: Seoul, Republic of Korea, 2019. [Google Scholar]
- Aoun, S.; Bird, S.; Kristjanson, L.J.; Currow, D. Reliability testing of the FAMCARE-2 scale: Measuring family carer satisfaction with palliative care. Palliat. Med. 2010, 24, 674–681. [Google Scholar] [CrossRef] [PubMed]
- Ko, S.B.; Kim, Y.J.; Kim, J.H.; Ra, S.H.; Moon, J.Y.; Park, S.Y. Korean Professional Consensus for Comfort Care and Withdrawing/Withholding in the Intensive Care Unit; by the Task Force of Korean Society of Critical Care Medicine; Korea Society of Critical Care Medicine: Seoul, Republic of Korea, 2018. [Google Scholar]
- Act on Decisions on Life-Sustaining Treatment for Patients in Hospice and Palliative Care or at the End of Life. Available online: https://law.go.kr (accessed on 15 August 2022).
- Durall, A.; Zurakowski, D.; Wolfe, J. Barriers to conducting advance care discussions for children with life-threatening conditions. Pediatrics 2012, 129, e975–e982. [Google Scholar] [CrossRef] [PubMed]
- Van der Geest, I.M.; Darlington, A.S.E.; Streng, I.C.; Michiels, E.M.; Pieters, R.; van den Heuvel-Eibrink, M.M. Parents’ experiences of pediatric palliative care and the impact on long-term parental grief. J. Pain Symptom Manag. 2014, 47, 1043–1053. [Google Scholar] [CrossRef] [PubMed]
- The Guideline for Korea Pediatric Palliative Care Project. Available online: https://hospice.go.kr (accessed on 15 August 2022).
- Burns, J.P.; Mitchell, C.; Outwater, K.M.; Geller, M.; Griffith, J.L.; Todres, I.D.; Truog, R.D. End-of-life care in the pediatric intensive care unit after the forgoing of life-sustaining treatment. Crit. Care Med. 2000, 28, 3060–3066. [Google Scholar] [CrossRef] [PubMed]
- Garros, D.; Rosychuk, R.J.; Cox, P.N. Circumstances surrounding end of life in a pediatric intensive care unit. Pediatrics 2003, 112, e371. [Google Scholar] [CrossRef] [PubMed]
- Althabe, M.; Cardigni, G.; Vassallo, J.C.; Allende, D.; Berrueta, M.; Codermatz, M.; Córdoba, J.; Castellano, S.; Jabornisky, R.; Marrone, Y.; et al. Dying in the intensive care unit: Collaborative multicenter study about forgoing life-sustaining treatment in Argentine pediatric intensive care units. Pediatr. Crit. Care Med. 2003, 4, 164–169. [Google Scholar] [CrossRef] [PubMed]
- Devictor, D.J.; Nguyen, D.T. Forgoing life-sustaining treatments in children: A comparison between Northern and Southern European pediatric intensive care units. Pediatr. Crit. Care Med. 2004, 5, 211–215. [Google Scholar] [CrossRef] [PubMed]
- Kreicbergs, U.C.; Lannen, P.; Onelov, E.; Wolfe, J. Parental grief after losing a child to cancer: Impact of professional and social support on long-term outcomes. J. Clin. Oncol. 2007, 25, 3307–3312. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.S.; Lim, N.G.; Kim, H.J.; Kim, C.; Lee, J.Y. Pediatric deaths attributed to complex chronic conditions over 10 years in Korea: Evidence for the need to provide pediatric palliative care. J. Korean Med. Sci. 2018, 33, e1. [Google Scholar] [CrossRef] [PubMed]
- Johnston, E.E.; Martinez, I.; Currie, E.; Brock, K.E.; Wolfe, J. Hospital or home? Where should children die and how do we make that a reality? J. Pain Symptom Manag. 2020, 60, 106–115. [Google Scholar] [CrossRef]
- Dussel, V.; Kreicbergs, U.; Hilden, J.M.; Watterson, J.; Moore, C.; Turner, B.G.; Weeks, J.C.; Wolfe, J. Looking beyond where children die: Determinants and effects of planning a child’s location of death. J. Pain Symptom Manag. 2009, 37, 33–43. [Google Scholar] [CrossRef] [PubMed]
- Shields, L.; Pratt, J.; Davis, L.; Hunter, J. Family-centred care for children in hospital. Cochrane Database Syst. Rev. 2007, 1, CD004811. [Google Scholar]
| Characteristics | Total | Period 1 (n = 25) | Period 2 (n = 23) |
|---|---|---|---|
| Sex | |||
| Male | 27 (56.2) | 16 (64.0) | 11 (47.8) |
| Female | 21 (43.8) | 9 (36.0) | 12 (52.2) |
| Age (years) | |||
| <1 | 5 (10.4) | 3 (12.0) | 2 (8.7) |
| 1–9 | 24 (50) | 12 (48.0) | 12 (52.2) |
| 10–19 | 19 (39.6) | 10 (40.0) | 9 (39.1) |
| Main problem | |||
| Neurology | 23 (47.9) | 16 (64.0) | 7 (30.4) |
| Haemato-oncology | 15 (31.2) | 6 (24.0) | 9 (39.1) |
| Cardiology | 6 (12.5) | 0 (0.0) | 6 (26.1) |
| Pulmonology | 2 (4.2) | 2 (8.0) | 0 (0.0) |
| Gastroenterology | 2 (4.2) | 1 (4.0) | 1 (4.3) |
| Valuables | Period 1 (n = 25) | Period 2 (n = 23) | p | ||
|---|---|---|---|---|---|
| Yes | No | Yes | No | ||
| Advanced care planning | 7 (28.0) | 18 (72.0) | 15 (65.2) | 8 (34.8) | 0.01 |
| Life-sustaining treatment | 9 (36.0) | 16 (64.0) | 2 (8.7) | 21 (91.3) | 0.025 |
| End-of-life process | |||||
| Intubation | 19 (76.0) | 6 (24.0) | 2 (8.7) | 21 (91.3) | 0.000 |
| CPR | 11 (44.0) | 14 (56.0) | 3 (13.0) | 20 (87.0) | 0.018 |
| Item Description | Response (%) | ||
|---|---|---|---|
| Very Satisfied/ Satisfied | Neither | Dissatisfied/Very Dissatisfied | |
| 1. The patient’s comfort | 91.7 | 8.3 | 0.0 |
| 2. The way in which the patient’s condition and likely progress were explained by the palliative care team | 83.3 | 8.3 | 8.3 |
| 3. Information given about the side effects of treatment | 75.0 | 25.0 | 0.0 |
| 4. The way in which the palliative care team respects the patient’s dignity | 91.7 | 8.3 | 0.0 |
| 5. Meetings with the palliative care team to discuss the patient’s condition and plan of care | 83.3 | 16.7 | 0.0 |
| 6. Speed with which symptoms are treated | 75.0 | 25.0 | 0.0 |
| 7. Palliative care team’s attention to the patient’s description of symptoms | 83.4 | 16.7 | 0.0 |
| 8. The way in which the patient’s physical needs for comfort are met | 83.3 | 16.7 | 0.0 |
| 9. Availability of the palliative care team to the family | 100 | 0.0 | 0.0 |
| 10. Emotional support provided to family members by the palliative care team | 91.6 | 8.3 | 0.0 |
| 11. The practical assistance provided by the palliative care team (e.g., bathing, home care, respite) | 91.6 | 8.3 | 0.0 |
| 12. The doctor’s attention to the patient’s symptoms | 83.3 | 16.7 | 0.0 |
| 13. The way in which the family is included in treatment and care decisions | 83.4 | 16.7 | 0.0 |
| 14. Information given about how to manage the patient’s symptoms (e.g., pain, constipation) | 83.4 | 8.3 | 8.3 |
| 15. How effectively the palliative care team manages the patient’s symptoms | 83.3 | 16.7 | 0.0 |
| 16. The palliative care team’s response to changes in the patient’s care needs | 91.7 | 8.3 | 0.0 |
| 17. Emotional support provided to the patient by the palliative care team | 91.7 | 8.3 | 0.0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kwon, J.E.; Kim, Y.H. Changes in the End-of-Life Process in Patients with Life-Limiting Diseases through the Intervention of the Pediatric Palliative Care Team. J. Clin. Med. 2023, 12, 6588. https://doi.org/10.3390/jcm12206588
Kwon JE, Kim YH. Changes in the End-of-Life Process in Patients with Life-Limiting Diseases through the Intervention of the Pediatric Palliative Care Team. Journal of Clinical Medicine. 2023; 12(20):6588. https://doi.org/10.3390/jcm12206588
Chicago/Turabian StyleKwon, Jung Eun, and Yeo Hyang Kim. 2023. "Changes in the End-of-Life Process in Patients with Life-Limiting Diseases through the Intervention of the Pediatric Palliative Care Team" Journal of Clinical Medicine 12, no. 20: 6588. https://doi.org/10.3390/jcm12206588
APA StyleKwon, J. E., & Kim, Y. H. (2023). Changes in the End-of-Life Process in Patients with Life-Limiting Diseases through the Intervention of the Pediatric Palliative Care Team. Journal of Clinical Medicine, 12(20), 6588. https://doi.org/10.3390/jcm12206588






