Activity Following Total Hip Arthroplasty: Which Patients Are Active, and Is Being Active Safe?
Abstract
:1. Introduction
2. Materials and Methods
2.1. Outcome Parameters
2.2. Data Collection
2.3. Statistical Analysis
3. Results
3.1. Demographics
3.2. Activity Groups
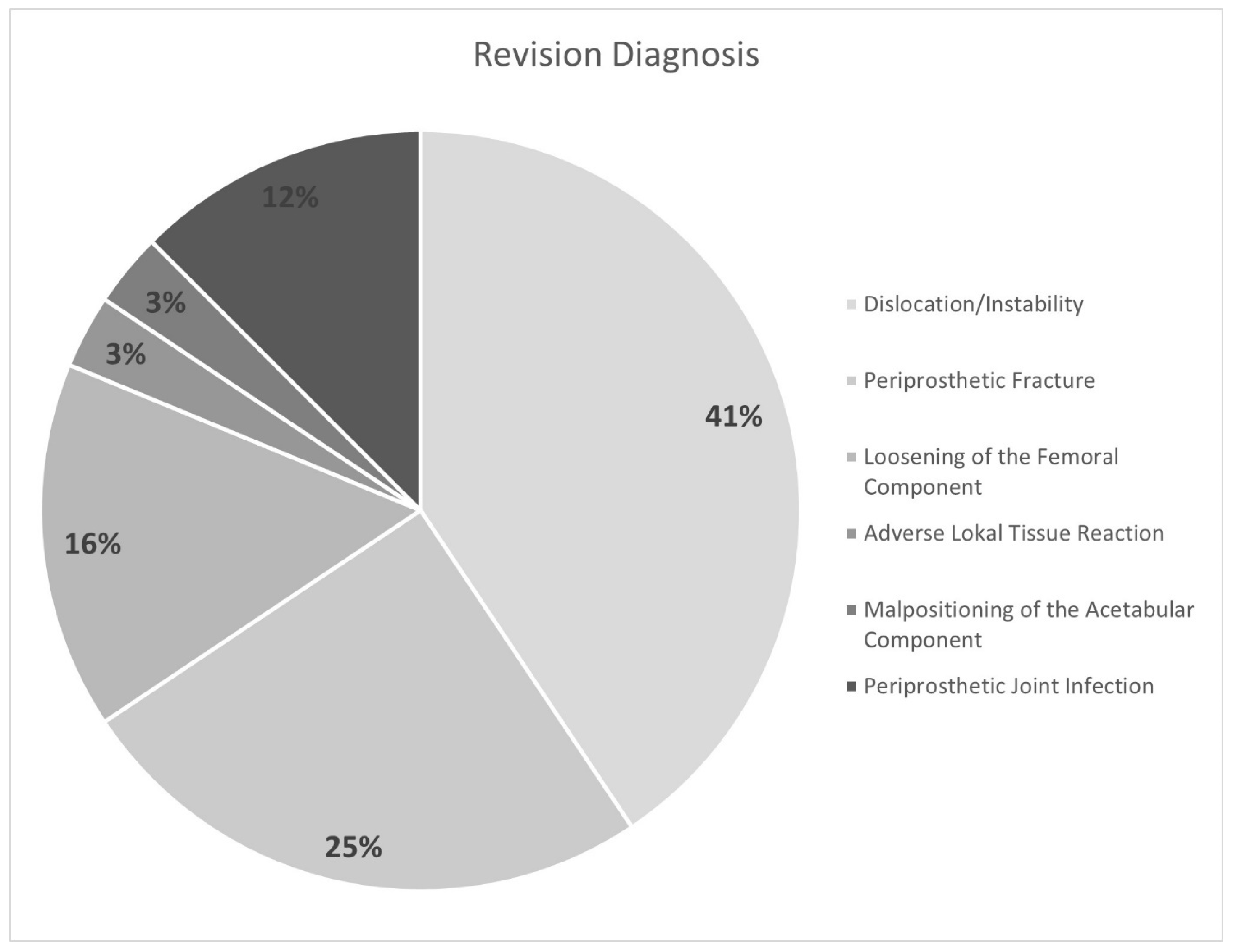
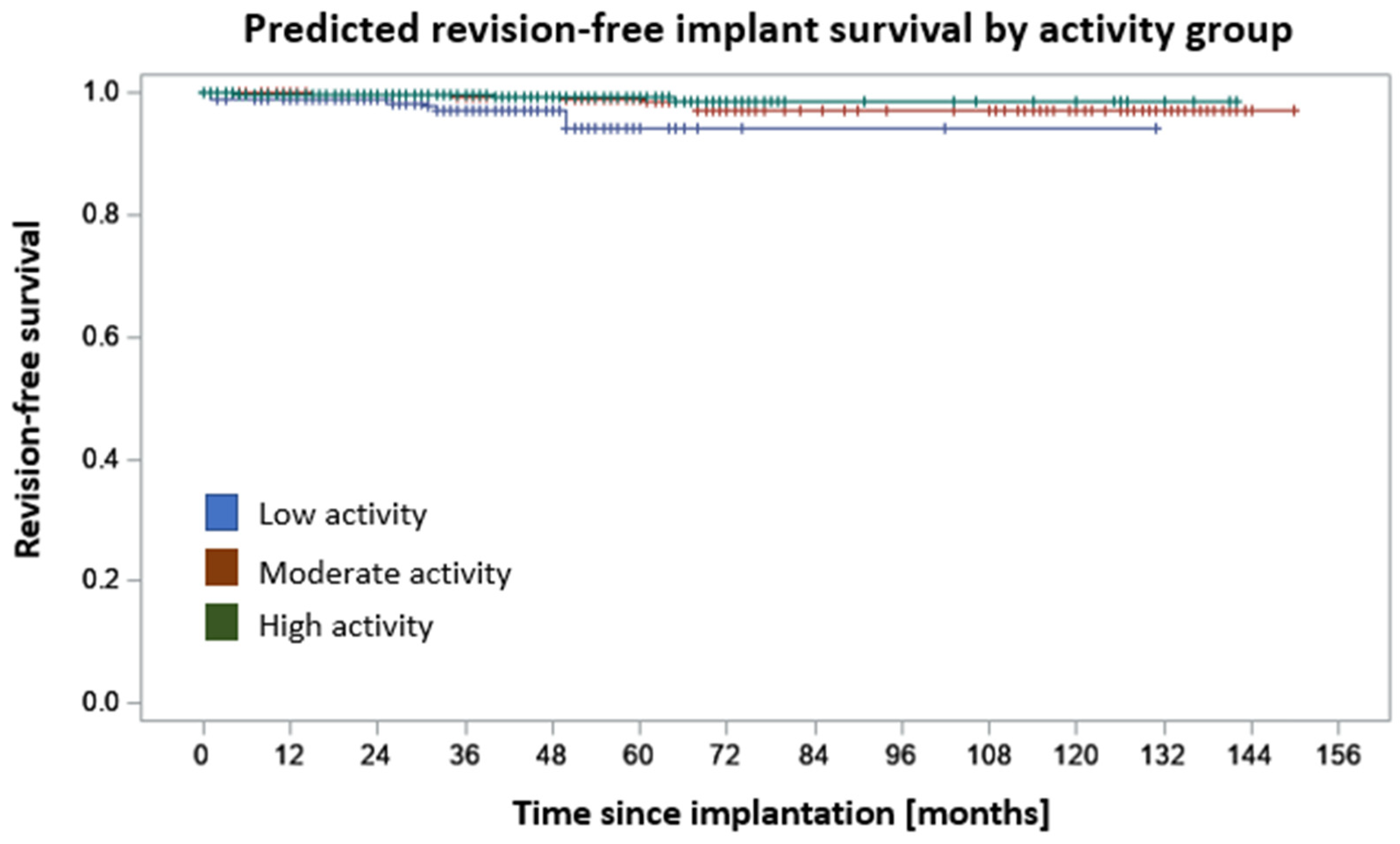
3.3. Revisions
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Stevens, M.; Reininga, I.H.F.; Bulstra, S.K.; Wagenmakers, R.; van den Akker-Scheek, I. Physical activity participation among patients after total hip and knee arthroplasty. Clin. Geriatr. Med. 2012, 28, 509–520. [Google Scholar] [CrossRef]
- Papalia, R.; Campi, S.; Vorini, F.; Zampogna, B.; Vasta, S.; Papalia, G.; Fossati, C.; Torre, G.; Denaro, V. The Role of Physical Activity and Rehabilitation Following Hip and Knee Arthroplasty in the Elderly. J. Clin. Med. 2020, 9, 1401. [Google Scholar] [CrossRef] [PubMed]
- Nocon, M.; Hiemann, T.; Müller-Riemenschneider, F.; Thalau, F.; Roll, S.; Willich, S.N. Association of physical activity with all-cause and cardiovascular mortality: A systematic review and meta-analysis. Eur. J. Cardiovasc. Prev. Rehabil. 2008, 15, 239–246. [Google Scholar] [CrossRef] [PubMed]
- Egan, E.; Reilly, T.; Giacomoni, M.; Redmond, L.; Turner, C. Bone mineral density among female sports participants. Bone 2006, 38, 227–233. [Google Scholar] [CrossRef]
- Ollivier, M.; Frey, S.; Parratte, S.; Flecher, X.; Argenson, J.-N. Does impact sport activity influence total hip arthroplasty durability? Clin. Orthop. Relat. Res. 2012, 470, 3060–3066. [Google Scholar] [CrossRef]
- Schmalzried, T.P.; Shepherd, E.F.; Dorey, F.J.; Jackson, W.O.; dela Rosa, M.; Fa’vae, F.; McKellop, H.A.; McClung, C.D.; Martell, J.; Moreland, J.R.; et al. The John Charnley Award. Wear is a function of use, not time. Clin. Orthop. Relat. Res. 2000, 381, 36–46. [Google Scholar] [CrossRef]
- Healy, W.L.; Sharma, S.; Schwartz, B.; Iorio, R. Athletic activity after total joint arthroplasty. J. Bone Joint Surg. Am. 2008, 90, 2245–2252. [Google Scholar] [CrossRef]
- de Steiger, R.; Lorimer, M.; Graves, S.E. Cross-Linked Polyethylene for Total Hip Arthroplasty Markedly Reduces Revision Surgery at 16 Years. J. Bone Joint Surg. Am. 2018, 100, 1281–1288. [Google Scholar] [CrossRef] [PubMed]
- Guy, S.; Flecher, X.; Sharma, A.; Argenson, J.-N.; Ollivier, M. Highly Crosslinked Polyethylene Can Reduce Wear Rate in THA for High-Demand Patients: A Matched-Paired Controlled Study. J. Arthroplast. 2021, 36, 3226–3232. [Google Scholar] [CrossRef]
- Fisher, J.; Jin, Z.; Tipper, J.; Stone, M.; Ingham, E. Tribology of alternative bearings. Clin. Orthop. Relat. Res. 2006, 453, 25–34. [Google Scholar] [CrossRef]
- Kurtz, S.M.; Lau, E.; Ong, K.; Zhao, K.; Kelly, M.; Bozic, K.J. Future young patient demand for primary and revision joint replacement: National projections from 2010 to 2030. Clin. Orthop. Relat. Res. 2009, 467, 2606–2612. [Google Scholar] [CrossRef] [PubMed]
- Ponzio, D.Y.; Rothermel, S.D.; Chiu, Y.-F.; Stavrakis, A.I.; Lyman, S.; Windsor, R.E. Does Physical Activity Level Influence Total Hip Arthroplasty Expectations, Satisfaction, and Outcomes? J. Arthroplast. 2021, 36, 2850–2857. [Google Scholar] [CrossRef] [PubMed]
- Hafkamp, F.J.; Lodder, P.; de Vries, J.; Gosens, T.; den Oudsten, B.L. Characterizing patients’ expectations in hip and knee osteoarthritis. Qual. Life Res. 2020, 29, 1509–1519. [Google Scholar] [CrossRef]
- Learmonth, I.D.; Young, C.; Rorabeck, C. The operation of the century: Total hip replacement. Lancet 2007, 370, 1508–1519. [Google Scholar] [CrossRef]
- Gschwend, N.; Frei, T.; Morscher, E.; Nigg, B.; Loehr, J. Alpine and cross-country skiing after total hip replacement: 2 cohorts of 50 patients each, one active, the other inactive in skiing, followed for 5–10 years. Acta Orthop. Scand. 2000, 71, 243–249. [Google Scholar] [CrossRef]
- Lancaster, A.; Christie, M.; Blackburn, B.E.; Pelt, C.E.; Peters, C.L.; Dunson, B.; Gililland, J.M.; Anderson, L.A. Can I Ski Doc?: Return to Skiing Following Total Joint Arthroplasty. J. Arthroplast. 2022, 37, 460–467. [Google Scholar] [CrossRef]
- Abe, H.; Sakai, T.; Nishii, T.; Takao, M.; Nakamura, N.; Sugano, N. Jogging after total hip arthroplasty. Am. J. Sports Med. 2014, 42, 131–137. [Google Scholar] [CrossRef] [PubMed]
- Crawford, D.A.; Adams, J.B.; Hobbs, G.R.; Morris, M.J.; Berend, K.R.; Lombardi, A.V., Jr. Does Activity Level After Primary Total Hip Arthroplasty Affect Aseptic Survival? Arthroplast. Today 2021, 11, 68–72. [Google Scholar] [CrossRef]
- Vu-Han, T.; Hardt, S.; Ascherl, R.; Gwinner, C.; Perka, C. Recommendations for return to sports after total hip arthroplasty are becoming less restrictive as implants improve. Arch. Orthop. Trauma Surg. 2021, 141, 497–507. [Google Scholar] [CrossRef]
- Thaler, M.; Khosravi, I.; Putzer, D.; Siebenrock, K.A.; Zagra, L. Return to Sports After Total Hip Arthroplasty: A Survey Among Members of the European Hip Society. J. Arthroplast. 2021, 36, 1645–1654. [Google Scholar] [CrossRef]
- van der Weegen, W.; Kornuijt, A.; Das, D. Do lifestyle restrictions and precautions prevent dislocation after total hip arthroplasty? A systematic review and meta-analysis of the literature. Clin. Rehabil. 2016, 30, 329–339. [Google Scholar] [CrossRef] [PubMed]
- Bose, V.C.; Kalaivanan, K.; Manohar, M.; Kumar, A.; Patil, S.; Suryanarayan, P. Is the Revision Rate Higher After Hip Arthroplasty in Teenage Patients? A Prospective Study with Long-Term Follow-Up of More Than 10 Years. Indian J. Orthop. 2021, 55, 993–1002. [Google Scholar] [CrossRef]
- Saleh, K.J.; Mulhall, K.J.; Bershadsky, B.; Ghomrawi, H.M.; White, L.E.; Buyea, C.M.; Krackow, K.A. Development and validation of a lower-extremity activity scale. Use for patients treated with revision total knee arthroplasty. J. Bone Joint Surg. Am. 2005, 87, 1985–1994. [Google Scholar] [CrossRef]
- Bauman, S.; Williams, D.; Petruccelli, D.; Elliott, W.; de Beer, J. Physical activity after total joint replacement: A cross-sectional survey. Clin. J. Sport Med. 2007, 17, 104–108. [Google Scholar] [CrossRef] [PubMed]
- Arshi, A.; Khan, I.A.; Ciesielka, K.-A.; Cozzarelli, N.F.; Fillingham, Y.A. Participation in sports and physical activities after total joint arthroplasty. J. Arthroplast. 2022, 38, 806–814. [Google Scholar] [CrossRef]
- Jassim, S.S.; Douglas, S.L.; Haddad, F.S. Athletic activity after lower limb arthroplasty: A systematic review of current evidence. Bone Joint J. 2014, 96, 923–927. [Google Scholar] [CrossRef] [PubMed]
- Huch, K.; Müller, K.A.C.; Stürmer, T.; Brenner, H.; Puhl, W.; Günther, K.-P. Sports activities 5 years after total knee or hip arthroplasty: The Ulm Osteoarthritis Study. Ann. Rheum. Dis. 2005, 64, 1715–1720. [Google Scholar] [CrossRef] [PubMed]
- Bonnin, M.P.; Rollier, J.-C.; Chatelet, J.-C.; Ait-Si-Selmi, T.; Chouteau, J.; Jacquot, L.; Hannink, G.; Saffarini, M.; Fessy, M.-H. Can Patients Practice Strenuous Sports After Uncemented Ceramic-on-Ceramic Total Hip Arthroplasty? Orthop. J. Sports Med. 2018, 6, 2325967118763920. [Google Scholar] [CrossRef]
- Hoorntje, A.; Janssen, K.Y.; Bolder, S.B.; Koenraadt, K.L.; Daams, J.G.; Blankevoort, L.; Kerkhoffs, G.M.; Kuijer, P.P.F. The Effect of Total Hip Arthroplasty on Sports and Work Participation: A Systematic Review and Meta-Analysis. Sports Med. 2018, 48, 1695–1726. [Google Scholar] [CrossRef]
- Innmann, M.M.; Weiss, S.; Andreas, F.; Merle, C.; Streit, M.R. Sports and physical activity after cementless total hip arthroplasty with a minimum follow-up of 10 years. Scand. J. Med. Sci. Sports 2016, 26, 550–556. [Google Scholar] [CrossRef] [PubMed]
- Dobson, P.F.; Reed, M.R. Prevention of infection in primary THA and TKA. EFORT Open Rev. 2020, 5, 604–613. [Google Scholar] [CrossRef]
- Haynes, J.; Nam, D.; Barrack, R.L. Obesity in total hip arthroplasty: Does it make a difference? Bone Joint J. 2017, 99, 31–36. [Google Scholar] [CrossRef]
- Ollivier, M.; Frey, S.; Parratte, S.; Flecher, X.; Argenson, J.N. Pre-operative function, motivation and duration of symptoms predict sporting participation after total hip replacement. Bone Joint J. 2014, 96, 1041–1046. [Google Scholar] [CrossRef] [PubMed]
- Delasotta, L.A.; Rangavajjula, A.V.; Porat, M.D.; Frank, M.L.; Orozco, F.R.; Ong, A.C. What are young patients doing after hip reconstruction? J. Arthroplast. 2012, 27, 1518–1525.e2. [Google Scholar] [CrossRef] [PubMed]
- Cleather, D.J.; Goodwin, J.E.; Bull, A.M.J. Hip and knee joint loading during vertical jumping and push jerking. Clin. Biomech. 2013, 28, 98–103. [Google Scholar] [CrossRef] [PubMed]
- van den Bogert, A.J.; Read, L.; Nigg, B.M. An analysis of hip joint loading during walking, running, and skiing. Med. Sci. Sports Exerc. 1999, 31, 131–142. [Google Scholar] [CrossRef] [PubMed]
- Bender, A.; Damm, P.; Hommel, H.; Duda, G.N. Overstretching Expectations May Endanger the Success of the “Millennium Surgery”. Front. Bioeng. Biotechnol. 2022, 10, 789629. [Google Scholar] [CrossRef] [PubMed]
- Thiele, K.; Hube, R. Hip Arthroplasty with Increased Expectancy. Z. Orthop. Unfall. 2021, 159, 91–97. [Google Scholar] [CrossRef] [PubMed]
- Bayliss, L.E.; Culliford, D.; Monk, A.P.; Glyn-Jones, S.; Prieto-Alhambra, D.; Judge, A.; Cooper, C.; Carr, A.J.; Arden, N.K.; Beard, D.J.; et al. The effect of patient age at intervention on risk of implant revision after total replacement of the hip or knee: A population-based cohort study. Lancet 2017, 389, 1424–1430. [Google Scholar] [CrossRef]


| Mean | SD | % | |
|---|---|---|---|
| Age (years) | 64 | 10 | |
| BMI (kg/m2) | 28.4 | 5.9 | |
| ASA | N/A | N/A | |
| 1 | 4.9 | ||
| 2 | 79.3 | ||
| 3+ | 14.9 | ||
| CCI | N/A | N/A | |
| 0 | 71.3 | ||
| 1–2 | 25.8 | ||
| 3+ | 2.7 | ||
| LEAS (points) | 9.5 | 3.2 | |
| Pain (NRS) | 61 | 24 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Streck, L.E.; Chiu, Y.-F.; Braun, S.; Mujaj, A.; Hanreich, C.; Boettner, F. Activity Following Total Hip Arthroplasty: Which Patients Are Active, and Is Being Active Safe? J. Clin. Med. 2023, 12, 6482. https://doi.org/10.3390/jcm12206482
Streck LE, Chiu Y-F, Braun S, Mujaj A, Hanreich C, Boettner F. Activity Following Total Hip Arthroplasty: Which Patients Are Active, and Is Being Active Safe? Journal of Clinical Medicine. 2023; 12(20):6482. https://doi.org/10.3390/jcm12206482
Chicago/Turabian StyleStreck, Laura Elisa, Yu-Fen Chiu, Sebastian Braun, Anisa Mujaj, Carola Hanreich, and Friedrich Boettner. 2023. "Activity Following Total Hip Arthroplasty: Which Patients Are Active, and Is Being Active Safe?" Journal of Clinical Medicine 12, no. 20: 6482. https://doi.org/10.3390/jcm12206482
APA StyleStreck, L. E., Chiu, Y.-F., Braun, S., Mujaj, A., Hanreich, C., & Boettner, F. (2023). Activity Following Total Hip Arthroplasty: Which Patients Are Active, and Is Being Active Safe? Journal of Clinical Medicine, 12(20), 6482. https://doi.org/10.3390/jcm12206482






