Prognostic Performance of Sequential Organ Failure Assessment, Acute Physiology and Chronic Health Evaluation III, and Simplified Acute Physiology Score II Scores in Patients with Suspected Infection According to Intensive Care Unit Type
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Setting and Data Source
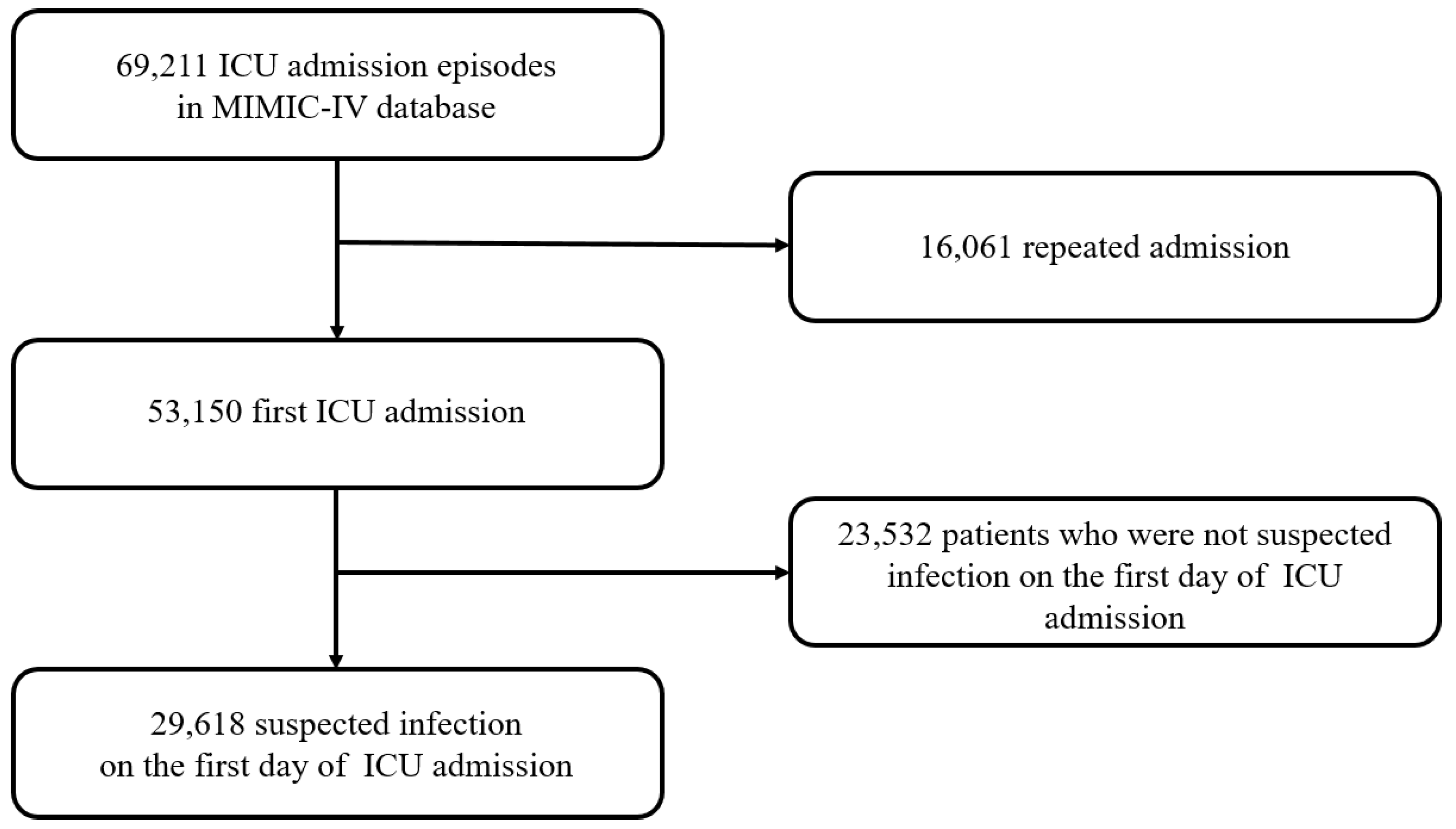
2.2. Study Population
2.3. Data Extraction
2.4. Calculation of SOFA, APACHE III, and SAPS II Scores
2.5. Outcome
2.6. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. In-Hospital Mortality and ICU Scores According to ICU Type
3.3. SOFA Score According to ICU Type
3.4. APACHE III Score According to ICU Type
3.5. SAPS II Score According to ICU Type
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Vincent, J.L.; Moreno, R. Clinical review: Scoring systems in the critically ill. Crit. Care 2010, 14, 207. [Google Scholar] [CrossRef] [PubMed]
- Vincent, J.L.; Moreno, R.; Takala, J.; Willatts, S.; De Mendonca, A.; Bruining, H.; Reinhart, C.K.; Suter, P.M.; Thijs, L.G. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996, 22, 707–710. [Google Scholar] [CrossRef]
- Zhu, Y.; Zhang, R.; Ye, X.; Liu, H.; Wei, J. SAPS III is superior to SOFA for predicting 28-day mortality in sepsis patients based on Sepsis 3.0 criteria. Int. J. Infect Dis. 2022, 114, 135–141. [Google Scholar] [CrossRef] [PubMed]
- Moreno, R.P.; Metnitz, P.G.; Almeida, E.; Jordan, B.; Bauer, P.; Campos, R.A.; Iapichino, G.; Edbrooke, D.; Capuzzo, M.; Le Gall, J.R. SAPS 3—From evaluation of the patient to evaluation of the intensive care unit. Part 2: Development of a prognostic model for hospital mortality at ICU admission. Intensive Care Med. 2005, 31, 1345–1355. [Google Scholar] [CrossRef] [PubMed]
- Raith, E.P.; Udy, A.A.; Bailey, M.; McGloughlin, S.; MacIsaac, C.; Bellomo, R.; Pilcher, D.V.; Australian and New Zealand Intensive Care Society (ANZICS) Centre for Outcomes and Resource Evaluation (CORE). Prognostic Accuracy of the SOFA Score, SIRS Criteria, and qSOFA Score for In-Hospital Mortality Among Adults With Suspected Infection Admitted to the Intensive Care Unit. JAMA 2017, 317, 290–300. [Google Scholar] [CrossRef] [PubMed]
- Le Gall, J.R.; Lemeshow, S.; Saulnier, F. A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA 1993, 270, 2957–2963. [Google Scholar] [CrossRef] [PubMed]
- Schoe, A.; Bakhshi-Raiez, F.; de Keizer, N.; van Dissel, J.T.; de Jonge, E. Mortality prediction by SOFA score in ICU-patients after cardiac surgery; comparison with traditional prognostic-models. BMC Anesth. 2020, 20, 65. [Google Scholar] [CrossRef]
- Higgins, T.L.; Teres, D.; Copes, W.S.; Nathanson, B.H.; Stark, M.; Kramer, A.A. Assessing contemporary intensive care unit outcome: An updated Mortality Probability Admission Model (MPM0-III). Crit. Care Med. 2007, 35, 827–835. [Google Scholar] [CrossRef]
- Knaus, W.A.; Wagner, D.P.; Draper, E.A.; Zimmerman, J.E.; Bergner, M.; Bastos, P.G.; Sirio, C.A.; Murphy, D.J.; Lotring, T.; Damiano, A.; et al. The APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults. Chest 1991, 100, 1619–1636. [Google Scholar] [CrossRef]
- Zhang, Z.; Chen, K.; Chen, L. APACHE III Outcome Prediction in Patients Admitted to the Intensive Care Unit with Sepsis Associated Acute Lung Injury. PLoS ONE 2015, 10, e0139374. [Google Scholar] [CrossRef]
- Knaus, W.A.; Draper, E.A.; Wagner, D.P.; Zimmerman, J.E. APACHE II: A severity of disease classification system. Crit. Care Med. 1985, 13, 818–829. [Google Scholar] [CrossRef] [PubMed]
- Sekulic, A.D.; Trpkovic, S.V.; Pavlovic, A.P.; Marinkovic, O.M.; Ilic, A.N. Scoring Systems in Assessing Survival of Critically Ill ICU Patients. Med. Sci. Monit. 2015, 21, 2621–2629. [Google Scholar] [CrossRef] [PubMed]
- Ogero, M.; Sarguta, R.J.; Malla, L.; Aluvaala, J.; Agweyu, A.; English, M.; Onyango, N.O.; Akech, S. Prognostic models for predicting in-hospital paediatric mortality in resource-limited countries: A systematic review. BMJ Open 2020, 10, e035045. [Google Scholar] [CrossRef] [PubMed]
- Castella, X.; Artigas, A.; Bion, J.; Kari, A. A comparison of severity of illness scoring systems for intensive care unit patients: Results of a multicenter, multinational study. The European/North American Severity Study Group. Crit. Care Med. 1995, 23, 1327–1335. [Google Scholar] [CrossRef]
- Keegan, M.T.; Gajic, O.; Afessa, B. Comparison of APACHE III, APACHE IV, SAPS 3, and MPM0III and influence of resuscitation status on model performance. Chest 2012, 142, 851–858. [Google Scholar] [CrossRef]
- Quintairos, A.; Pilcher, D.; Salluh, J.I.F. ICU scoring systems. Intensive Care Med. 2023, 49, 223–225. [Google Scholar] [CrossRef] [PubMed]
- Higgins, T.L.; Kramer, A.A.; Nathanson, B.H.; Copes, W.; Stark, M.; Teres, D. Prospective validation of the intensive care unit admission Mortality Probability Model (MPM0-III). Crit. Care Med. 2009, 37, 1619–1623. [Google Scholar] [CrossRef]
- Thodphetch, M.; Chenthanakij, B.; Wittayachamnankul, B.; Sruamsiri, K.; Tangsuwanaruk, T. A comparison of scoring systems for predicting mortality and sepsis in the emergency department patients with a suspected infection. Clin. Exp. Emerg. Med. 2021, 8, 289–295. [Google Scholar] [CrossRef]
- Nishimoto, Y.; Ohbe, H.; Matsui, H.; Nakajima, M.; Sasabuchi, Y.; Goto, T.; Morita, K.; Fushimi, K.; Sato, Y.; Yasunaga, H. Predictive ability of the sequential organ failure assessment score for in-hospital mortality in patients with cardiac critical illnesses: A nationwide observational study. Eur. Heart J. Acute Cardiovasc. Care 2022, 11, 312–321. [Google Scholar] [CrossRef]
- Cour, M.; Bresson, D.; Hernu, R.; Argaud, L. SOFA score to assess the severity of the post-cardiac arrest syndrome. Resuscitation 2016, 102, 110–115. [Google Scholar] [CrossRef]
- Lambden, S.; Laterre, P.F.; Levy, M.M.; Francois, B. The SOFA score-development, utility and challenges of accurate assessment in clinical trials. Crit. Care 2019, 23, 374. [Google Scholar] [CrossRef] [PubMed]
- Moreno, R.; Vincent, J.L.; Matos, R.; Mendonca, A.; Cantraine, F.; Thijs, L.; Takala, J.; Sprung, C.; Antonelli, M.; Bruining, H.; et al. The use of maximum SOFA score to quantify organ dysfunction/failure in intensive care. Results of a prospective, multicentre study. Working Group on Sepsis related Problems of the ESICM. Intensive Care Med. 1999, 25, 686–696. [Google Scholar] [CrossRef]
- Salluh, J.I.; Soares, M. ICU severity of illness scores: APACHE, SAPS and MPM. Curr. Opin. Crit. Care 2014, 20, 557–565. [Google Scholar] [CrossRef] [PubMed]
- Haniffa, R.; Isaam, I.; De Silva, A.P.; Dondorp, A.M.; De Keizer, N.F. Performance of critical care prognostic scoring systems in low and middle-income countries: A systematic review. Crit. Care 2018, 22, 18. [Google Scholar] [CrossRef] [PubMed]
- Paul, E.; Bailey, M.; Pilcher, D. Risk prediction of hospital mortality for adult patients admitted to Australian and New Zealand intensive care units: Development and validation of the Australian and New Zealand Risk of Death model. J. Crit. Care 2013, 28, 935–941. [Google Scholar] [CrossRef] [PubMed]
- McCoy, I.E.; Chertow, G.M.; Chang, T.I. Patterns of diuretic use in the intensive care unit. PLoS ONE 2019, 14, e0217911. [Google Scholar] [CrossRef]
- Quan, H.; Sundararajan, V.; Halfon, P.; Fong, A.; Burnand, B.; Luthi, J.C.; Saunders, L.D.; Beck, C.A.; Feasby, T.E.; Ghali, W.A. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med. Care 2005, 43, 1130–1139. [Google Scholar] [CrossRef]
- Charlson, M.; Szatrowski, T.P.; Peterson, J.; Gold, J. Validation of a combined comorbidity index. J. Clin. Epidemiol. 1994, 47, 1245–1251. [Google Scholar] [CrossRef] [PubMed]
- Johnson, A.E.; Stone, D.J.; Celi, L.A.; Pollard, T.J. The MIMIC Code Repository: Enabling reproducibility in critical care research. J. Am. Med. Inf. Assoc. 2018, 25, 32–39. [Google Scholar] [CrossRef]
- Seymour, C.W.; Liu, V.X.; Iwashyna, T.J.; Brunkhorst, F.M.; Rea, T.D.; Scherag, A.; Rubenfeld, G.; Kahn, J.M.; Shankar-Hari, M.; Singer, M.; et al. Assessment of Clinical Criteria for Sepsis: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 762–774. [Google Scholar] [CrossRef]
- Moreno, R.; Rhodes, A.; Piquilloud, L.; Hernandez, G.; Takala, J.; Gershengorn, H.B.; Tavares, M.; Coopersmith, C.M.; Myatra, S.N.; Singer, M.; et al. The Sequential Organ Failure Assessment (SOFA) Score: Has the time come for an update? Crit. Care 2023, 27, 15. [Google Scholar] [CrossRef] [PubMed]
- Pellathy, T.P.; Pinsky, M.R.; Hravnak, M. Intensive Care Unit Scoring Systems. Crit. Care Nurse 2021, 41, 54–64. [Google Scholar] [CrossRef] [PubMed]
- Jeong, S. Scoring Systems for the Patients of Intensive Care Unit. Acute. Crit. Care 2018, 33, 102–104. [Google Scholar] [CrossRef] [PubMed]
- Kim, K. Future of sepsis: Perspective on diagnosis. Clin. Exp. Emerg. Med. 2022, 9, 269–270. [Google Scholar] [CrossRef] [PubMed]
- Evans, L.; Rhodes, A.; Alhazzani, W.; Antonelli, M.; Coopersmith, C.M.; French, C.; Machado, F.R.; McIntyre, L.; Ostermann, M.; Prescott, H.C.; et al. Surviving sepsis campaign: International guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 2021, 47, 1181–1247. [Google Scholar] [CrossRef]
- Chang, H.; Cha, W.C. Artificial intelligence decision points in an emergency department. Clin. Exp. Emerg. Med. 2022, 9, 165–168. [Google Scholar] [CrossRef]
- Kang, C.Y.; Yoon, J.H. Current challenges in adopting machine learning to critical care and emergency medicine. Clin. Exp. Emerg. Med. 2023, 10, 132–137. [Google Scholar] [CrossRef]
| Variables | All Patients (n = 29,618) | Survivors (n = 25,943) | In-Hospital Death (n = 3675) | p |
|---|---|---|---|---|
| Age (mean ± SD), years | 65.4 ± 16.7 | 64.7 ± 16.7 | 69.8 ± 15.6 | <0.001 |
| Male sex, No. (%) | 16,806 (56.7) | 14,833 (57.2) | 1973 (53.7) | <0.001 |
| Charlson comorbidity score (mean ± SD) | 5.5 ± 2.9 | 5.3 ± 2.9 | 7.0 ± 3.0 | <0.001 |
| Intensive care unit | <0.001 | |||
| MICU | 6532 (22.1) | 5393 (20.8) | 1139 (31.0) | |
| MICU/SICU (mixed) | 5787 (19.5) | 4836 (18.6) | 951 (25.9) | |
| CCU | 2590 (8.7) | 2138 (8.2) | 452 (12.3) | |
| CVICU | 6747 (22.8) | 6562 (25.3) | 185 (5.0) | |
| NSICU | 411 (1.4) | 338 (1.3) | 73 (2.0) | |
| Neuro-ICU | 310 (1.1) | 294 (1.1) | 16 (0.4) | |
| SICU | 3967 (13.4) | 3473(13.4) | 494 (13.4) | |
| Trauma SICU | 3274 (11.1) | 2909 (11.2) | 365 (9.9) | |
| Vital signs a | ||||
| Lowest MAP (mean ± SD), mmHg | 61.5 ± 11.5 | 62.3 ± 11.0 | 55.8 ± 13.6 | <0.001 |
| Highest HR (mean ± SD), beat per min | 105.0 ± 20.6 | 103.9 ± 19.9 | 113.2 ± 23.4 | <0.001 |
| Highest RR (mean ± SD), breath per min | 28.4 ± 6.6 | 28.1 ± 6.5 | 31.0 ± 7.2 | <0.001 |
| Highest temperature, °C | 37.4 ± 0.8 | 37.5 ± 0.8 | 37.3 ± 1.1 | <0.001 |
| Laboratory findings a (mean ± SD) | ||||
| Highest WBCs, 109/L | 15.3 ± 11.9 | 14.9 ± 10.8 | 18.1 ± 17.4 | <0.001 |
| Lowest Hb, g/dL | 9.6 ± 2.4 | 9.6 ± 2.3 | 9.9 ± 2.7 | <0.001 |
| Lowest platelets, 109/L | 171.8 ± 81.3 | 174.0 ± 79.2 | 155.8 ± 93.0 | <0.001 |
| Highest bilirubin, mg/dL | 2.1 ± 4.7 | 1.8 ± 3.8 | 3.7 ± 7.4 | <0.001 |
| Highest creatinine, mg/dL | 1.5 ± 1.5 | 1.4 ± 1.5 | 2.1 ± 1.7 | <0.001 |
| Highest lactate, mmol/L | 2.9 ± 2.5 | 2.6 ± 1.8 | 4.9 ±4.4 | <0.001 |
| GCS score a (mean ± SD) | 13.5 ± 2.9 | 13.6 ± 2.8 | 12.8 ± 3.6 | <0.001 |
| Vasopressor use a, No. (%) | 10,156 (34.3) | 8151 (31.4) | 2005 (54.6) | <0.001 |
| Norepinephrine, No. (%) | 5392 (18.2) | 3779 (14.6) | 1613 (43.9) | <0.001 |
| Epinephrine, No. (%) | 1489 (5.0) | 1186 (4.6) | 303 (8.2) | <0.001 |
| Dopamine, No. (%) | 601 (2.0) | 368 (1.4) | 233 (6.3) | <0.001 |
| Vasopressin, No. (%) | 1611 (5.4) | 845 (3.3) | 766 (20.8) | <0.001 |
| Phenylephrine, No. (%) | 5294 (17.9) | 4505 (17.4) | 789 (21.5) | <0.001 |
| Dobutamine use, No. (%) | 276 (0.9) | 165 (0.6) | 111 (3.0) | <0.001 |
| Norepinephrine-equivalent dose b (mean ± SD), µg/kg/min | 0.20 ± 0.25 | 0.15 ± 0.19 | 0.40 ± 0.37 | <0.001 |
| Mechanical ventilation a, No. (%) | 14,812 (50.0) | 12,590 (48.5) | 2222 (60.5) | <0.001 |
| Renal replacement therapy a, No. (%) | 629 (2.2) | 420 (1.6) | 209 (5.7) | <0.001 |
| SOFA score a (mean ± SD) | 5.5 ± 3.8 | 5.0 ± 3.4 | 9.0 ± 4.5 | <0.001 |
| APACHE III score | 61.1 ± 24.6 | 57.3 ± 21.5 | 87.7 ± 28.4 | <0.001 |
| SAPS II score | 37.0 ± 14.5 | 34.9 ± 12.9 | 51.8 ± 16.5 | <0.001 |
| ICU Type | In-Hospital Mortality, % | Total SOFA | APACHE III Score | SAPS II Score |
|---|---|---|---|---|
| MICU | 17.4 | 6.3 ± 4.4 | 67.4 ± 25.8 | 37.9 ± 15.2 |
| MICU/SICU | 16.4 | 5.5 ± 3.9 a | 65.7 ± 25.7 a | 38.7 ± 15.8 a |
| CCU | 17.5 | 5.5 ± 4.0 a | 65.2 ± 23.7 a | 38.7 ± 14.7 a |
| CVICU | 2.7 a | 5.6 ± 3.0 a | 54.6 ± 20.1 a | 36.9 ± 12.5 a |
| NSICU | 17.8 | 4.8 ± 3.0 a | 54.0 ± 20.2 a | 35.7 ± 11.9 a |
| Neuro-ICU | 5.2 a | 2.8 ± 2.1 a | 48.3 ± 18.5 a | 31.6 ± 10.9 a |
| SICU | 12.5 a | 5.0 ± 3.8 a | 58.3 ± 24.3 a | 35.3 ± 14.3 a |
| Trauma SICU | 11.2 a | 4.8 ± 3.6 a | 54.2 ± 23.7 a | 33.6 ± 14.2 a |
| ICU Type | SOFA Score (95% CI) | APACHE III Score (95% CI) | SAPS II Score (95% CI) |
|---|---|---|---|
| Overall | 0.785 (0.773–0.797) a,c | 0.807 (0.799–0.814) b,c | 0.795 (0.787–0.811) a,b |
| MICU | 0.793 (0.779–0.808) | 0.796 (0.782–0.810) | 0.795 (0.780–0.809) |
| MICU/SICU | 0.793 (0.778–0.808) | 0.801 (0.786–0.816) | 0.806 (0.791–0.821) |
| CCU | 0.826 (0.806–0.846) d | 0.808 (0.785–0.830) | 0.810 (0.788–0.832) |
| CVICU | 0.805 (0.768–0.841) | 0.837 (0.812–0.863) c,d | 0.799 (0.769–0.830) a |
| NSICU | 0.723 (0.657–0.790) d | 0.728 (0.668–0.787) d | 0.760 (0.706–0.813) |
| Neuro-ICU | 0.821 (0.732–0.91) | 0.860 (0.790–0.930) c | 0.803 (0.705–0.902) a |
| SICU | 0.748 (0.725–0.771) d | 0.766 (0.742–0.789) d | 0.759 (0.737–0.782) d |
| Trauma SICU | 0.786 (0.760–0.812) c | 0.795 (0.769–0.819) c | 0.819 (0.796–0.841) a,b |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hwang, S.-Y.; Kim, I.-K.; Jeong, D.; Park, J.-E.; Lee, G.-T.; Yoo, J.; Choi, K.; Shin, T.-G.; Kim, K., on behalf of the Korean Shock Society (KoSS) Investigators. Prognostic Performance of Sequential Organ Failure Assessment, Acute Physiology and Chronic Health Evaluation III, and Simplified Acute Physiology Score II Scores in Patients with Suspected Infection According to Intensive Care Unit Type. J. Clin. Med. 2023, 12, 6402. https://doi.org/10.3390/jcm12196402
Hwang S-Y, Kim I-K, Jeong D, Park J-E, Lee G-T, Yoo J, Choi K, Shin T-G, Kim K on behalf of the Korean Shock Society (KoSS) Investigators. Prognostic Performance of Sequential Organ Failure Assessment, Acute Physiology and Chronic Health Evaluation III, and Simplified Acute Physiology Score II Scores in Patients with Suspected Infection According to Intensive Care Unit Type. Journal of Clinical Medicine. 2023; 12(19):6402. https://doi.org/10.3390/jcm12196402
Chicago/Turabian StyleHwang, Sung-Yeon, In-Kyu Kim, Daun Jeong, Jong-Eun Park, Gun-Tak Lee, Junsang Yoo, Kihwan Choi, Tae-Gun Shin, and Kyuseok Kim on behalf of the Korean Shock Society (KoSS) Investigators. 2023. "Prognostic Performance of Sequential Organ Failure Assessment, Acute Physiology and Chronic Health Evaluation III, and Simplified Acute Physiology Score II Scores in Patients with Suspected Infection According to Intensive Care Unit Type" Journal of Clinical Medicine 12, no. 19: 6402. https://doi.org/10.3390/jcm12196402
APA StyleHwang, S.-Y., Kim, I.-K., Jeong, D., Park, J.-E., Lee, G.-T., Yoo, J., Choi, K., Shin, T.-G., & Kim, K., on behalf of the Korean Shock Society (KoSS) Investigators. (2023). Prognostic Performance of Sequential Organ Failure Assessment, Acute Physiology and Chronic Health Evaluation III, and Simplified Acute Physiology Score II Scores in Patients with Suspected Infection According to Intensive Care Unit Type. Journal of Clinical Medicine, 12(19), 6402. https://doi.org/10.3390/jcm12196402






