Blood Purification in Patients with Sepsis Associated with Acute Kidney Injury: A Narrative Review
Abstract
1. Introduction
2. Indications for Acute BPT in Sepsis
2.1. Renal Indications
2.2. Non-Renal Indications
3. Definition and Staging Criteria of AKI
4. Biomarkers for AKI
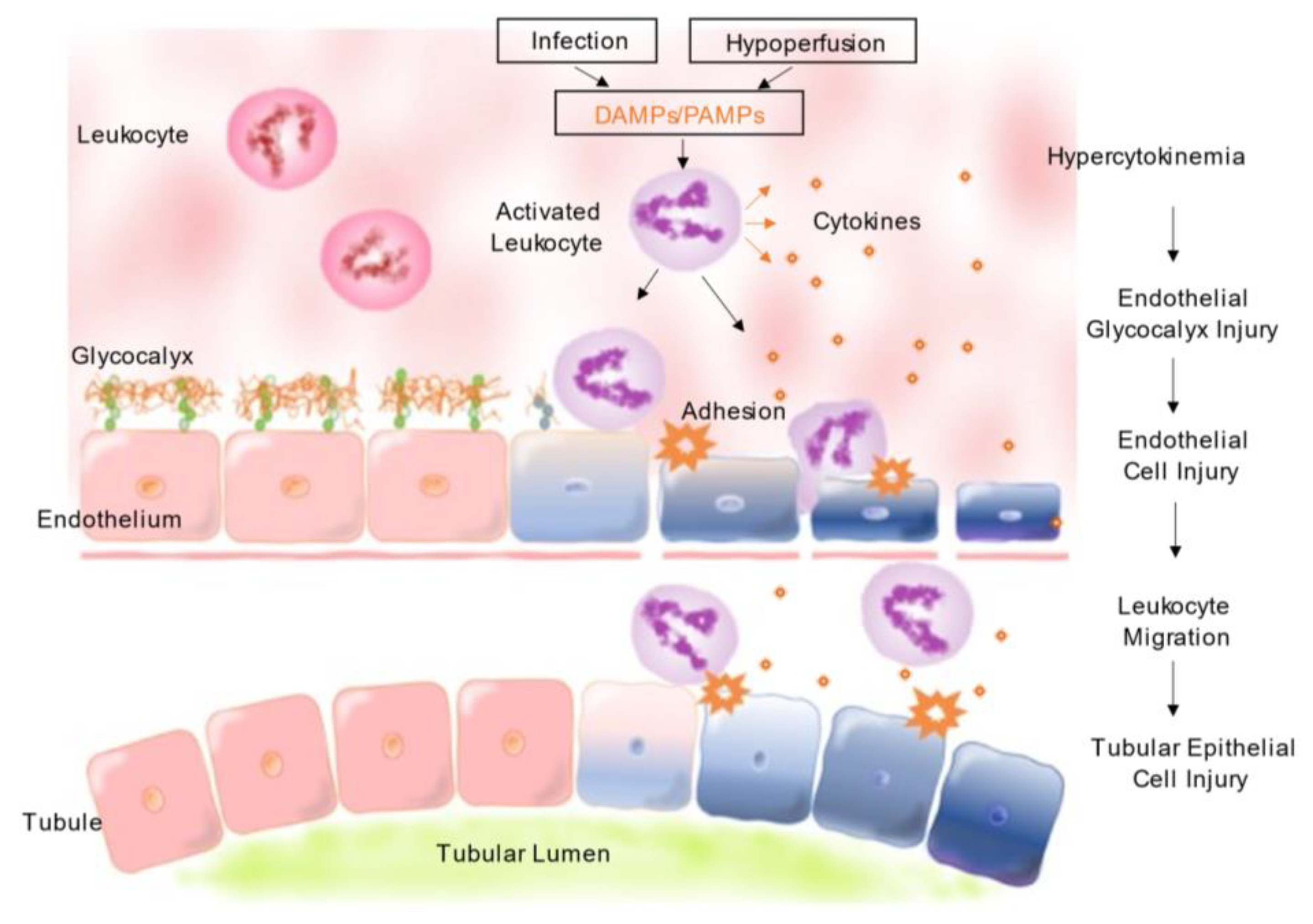
5. Epidemiology and Pathophysiology of Septic AKI
6. KRT Initiation Timing for AKI
7. Intensity of KRT
8. AN69/AN69ST/oXiris
9. Polymethyl Methacrylate
10. CytoSorb®
11. Polimyxin B-Immobilized Fiber Column Direct Hemoperfusion
12. Future Directions
13. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Singer, M.; Deutschman, C.S.; Seymour, C.W.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.D.; Coopersmith, C.M.; et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 801–810. [Google Scholar] [CrossRef]
- Bagshaw, S.M.; Uchino, S.; Bellomo, R.; Morimatsu, H.; Morgera, S.; Schetz, M.; Tan, I.; Bouman, C.; Macedo, E.; Gibney, N.; et al. Septic Acute Kidney Injury in Critically Ill Patients: Clinical Characteristics and Outcomes. Clin. J. Am. Soc. Nephrol. 2007, 2, 431–439. [Google Scholar] [CrossRef]
- Pan, H.C.; Chen, Y.Y.; Tsai, I.J.; Shiao, C.C.; Huang, T.M.; Chan, C.K.; Liao, H.W.; Lai, T.S.; Chueh, Y.; Wu, V.C.; et al. Accelerated Versus Standard Initiation of Renal Replacement Therapy for Critically Ill Patients with Acute Kidney Injury: A Systematic Review and Meta-Analysis of RCT Studies. Crit. Care 2021, 25, 5. [Google Scholar] [CrossRef]
- Snow, T.A.C.; Littlewood, S.; Corredor, C.; Singer, M.; Arulkumaran, N. Effect of Extracorporeal Blood Purification on Mortality in Sepsis: A Meta-analysis and Trial Sequential Analysis. Blood Purif. 2021, 50, 462–472. [Google Scholar] [CrossRef]
- Monard, C.; Abraham, P.; Schneider, A.; Rimmelé, T. New Targets for Extracorporeal Blood Purification Therapies in Sepsis. Blood Purif. 2023, 52, 1–7. [Google Scholar] [CrossRef]
- Forni, L.G.; Ricci, Z.; Ronco, C. Extracorporeal Renal Replacement Therapies in the Treatment of Sepsis: Where Are We? Semin. Nephrol. 2015, 35, 55–63. [Google Scholar] [CrossRef]
- Uchino, S.; Kellum, J.A.; Bellomo, R.; Doig, G.S.; Morimatsu, H.; Morgera, S.; Schetz, M.; Tan, I.; Bouman, C.; Macedo, E.; et al. Beginning and Ending Supportive Therapy for the Kidney (BEST Kidney) Investigators. Acute Renal Failure in Critically Ill Patients: A Multinational, Multicenter Study. JAMA 2005, 294, 813–818. [Google Scholar] [CrossRef]
- Hoste, E.A.; Bagshaw, S.M.; Bellomo, R.; Cely, C.M.; Colman, R.; Cruz, D.N.; Edipidis, K.; Forni, L.G.; Gomersall, C.D.; Govil, D.; et al. Epidemiology of Acute Kidney Injury in Critically Ill Patients: The Multinational AKI-EPI Study. Intensive Care Med. 2015, 41, 1411–1423. [Google Scholar] [CrossRef]
- Bagshaw, S.M.; George, C.; Bellomo, R. ANZICS Database Management Committee. Early Acute Kidney Injury and Sepsis: A Multicentre Evaluation. Crit. Care 2008, 12, R47. [Google Scholar] [CrossRef]
- Kellum, J.A.; Kong, L.; Fink, M.P.; Weissfeld, L.A.; Yealy, D.M.; Pinsky, M.R.; Fine, J.; Krichevsky, A.; Delude, R.L.; Angus, D.C.; et al. Understanding the Inflammatory Cytokine Response in Pneumonia and Sepsis: Results of the Genetic and Inflammatory Markers of Sepsis (GenIMS) Study. Arch. Intern. Med. 2007, 167, 1655–1663. [Google Scholar] [CrossRef]
- Honore, P.M.; Joannes-Boyau, O.; Boer, W.; Collin, V. High-Volume Hemofiltration in Sepsis and SIRS: Current Concepts and Future Prospects. Blood Purif. 2009, 28, 1–11. [Google Scholar] [CrossRef]
- Ronco, C.; Tetta, C.; Mariano, F.; Wratten, M.L.; Bonello, M.; Bordoni, V.; Cardona, X.; Inguaggiato, P.; Pilotto, L.; d’Intini, V.; et al. Interpreting the Mechanisms of Continuous Renal Replacement Therapy in Sepsis: The Peak Concentration Hypothesis. Artif. Organs 2003, 27, 792–801. [Google Scholar] [CrossRef]
- Honoré, P.M.; Matson, J.R. Extracorporeal Removal for Sepsis: Acting at the Tissue Level—The Beginning of a New Era for This Treatment Modality in Septic Shock. Crit. Care Med. 2004, 32, 896–897. [Google Scholar] [CrossRef]
- Di Carlo, J.V.; Alexander, S.R. Hemofiltration for Cytokine-Driven Illnesses: The Mediator Delivery Hypothesis. Int. J. Artif. Organs 2005, 28, 777–786. [Google Scholar] [CrossRef]
- Bellomo, R.; Ronco, C.; Kellum, J.A.; Mehta, R.L.; Palevsky, P.; Acute Dialysis Quality Initiative Workgroup. Acute Renal Failure—Definition, Outcome Measures, Animal Models, Fluid Therapy and Information Technology Needs: The Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit. Care 2004, 8, R204–R212. [Google Scholar] [CrossRef]
- Mehta, R.L.; Kellum, J.A.; Shah, S.V.; Molitoris, B.A.; Ronco, C.; Warnock, D.G.; Levin, A.; Acute Kidney Injury Network. Acute Kidney Injury Network: Report of an Initiative to Improve Outcomes in Acute Kidney Injury. Crit. Care 2007, 11, R31. [Google Scholar] [CrossRef]
- Khwaja, A. KDIGO Clinical Practice Guidelines for Acute Kidney Injury. Nephron Clin. Pract. 2012, 120, c179–c184. [Google Scholar] [CrossRef]
- Luo, X.; Jiang, L.; Du, B.; Wen, Y.; Wang, M.; Xi, X.; Beijing Acute Kidney Injury Trial (BAKIT) Workgroup. A Comparison of Different Diagnostic Criteria of Acute Kidney Injury in Critically Ill Patients. Crit. Care 2014, 18, R144. [Google Scholar] [CrossRef]
- Li, Z.; Cai, L.; Liang, X.; Du, Z.; Chen, Y.; An, S.; Tan, N.; Xu, L.; Li, R.; Li, L.; et al. Identification and Predicting Short-Term Prognosis of Early Cardiorenal Syndrome Type 1: KDIGO Is Superior to RIFLE or AKIN. PLoS ONE 2014, 9, e114369. [Google Scholar] [CrossRef]
- Rodrigues, F.B.; Bruetto, R.G.; Torres, U.S.; Otaviano, A.P.; Zanetta, D.M.; Burdmann, E.A. Incidence and Mortality of Acute Kidney Injury After Myocardial Infarction: A Comparison Between KDIGO and RIFLE Criteria. PLoS ONE 2013, 8, e69998. [Google Scholar] [CrossRef]
- Mishra, J.; Dent, C.; Tarabishi, R.; Mitsnefes, M.M.; Ma, Q.; Kelly, C.; Ruff, S.M.; Zahedi, K.; Shao, M.; Bean, J.; et al. Neutrophil Gelatinase-Associated Lipocalin (NGAL) as a Biomarker for Acute Renal Injury After Cardiac Surgery. Lancet 2005, 365, 1231–1238. [Google Scholar] [CrossRef]
- Haase, M.; Haase-Fielitz, A.; Bellomo, R.; Mertens, P.R. Neutrophil Gelatinase-Associated Lipocalin as a Marker of Acute Renal Disease. Curr. Opin. Hematol. 2011, 18, 11–18. [Google Scholar] [CrossRef] [PubMed]
- Kamijo, A.; Sugaya, T.; Hikawa, A.; Okada, M.; Okumura, F.; Yamanouchi, M.; Honda, A.; Okabe, M.; Fujino, T.; Hirata, Y.; et al. Urinary Excretion of Fatty Acid-Binding Protein Reflects Stress Overload on the Proximal Tubules. Am. J. Pathol. 2004, 165, 1243–1255. [Google Scholar] [CrossRef] [PubMed]
- Susantitaphong, P.; Siribamrungwong, M.; Doi, K.; Noiri, E.; Terrin, N.; Jaber, B.L. Performance of Urinary Liver-Type Fatty Acid-Binding Protein in Acute Kidney Injury: A Meta-Analysis. Am. J. Kidney Dis. 2013, 61, 430–439. [Google Scholar] [CrossRef] [PubMed]
- Kashani, K.; Al-Khafaji, A.; Ardiles, T.; Artigas, A.; Bagshaw, S.M.; Bell, M.; Bihorac, A.; Birkhahn, R.; Cely, C.M.; Chawla, L.S.; et al. Discovery and Validation of Cell Cycle Arrest Biomarkers in Human Acute Kidney Injury. Crit. Care 2013, 17, R25. [Google Scholar] [CrossRef]
- American College of Chest Physicians/Society of Critical Care Medicine. American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference: Definitions for Sepsis and Organ Failure and Guidelines for the Use of Innovative Therapies in Sepsis. Crit. Care Med. 1992, 20, 864–874. [Google Scholar] [CrossRef]
- de Miranda, A.C.; de Menezes, I.A.C.; Junior, H.C.; Luy, A.M.; do Nascimento, M.M. Monitoring Peripheral Perfusion in Sepsis Associated Acute Kidney Injury: Analysis of Mortality. PLoS ONE 2020, 15, e0239770. [Google Scholar] [CrossRef] [PubMed]
- Wald, R.; McArthur, E.; Adhikari, N.K.; Bagshaw, S.M.; Burns, K.E.; Garg, A.X.; Harel, Z.; Kitchlu, A.; Mazer, C.D.; Nash, D.M.; et al. Changing Incidence and Outcomes Following Dialysis-Requiring Acute Kidney Injury Among Critically Ill Adults: A Population-Based Cohort Study. Am. J. Kidney Dis. 2015, 65, 870–877. [Google Scholar] [CrossRef]
- Kellum, J.A.; Chawla, L.S.; Keener, C.; Singbartl, K.; Palevsky, P.M.; Pike, F.L.; Yealy, D.M.; Huang, D.T.; Angus, D.C.; ProCESS and ProGReSS-AKI Investigators. The Effects of Alternative Resuscitation Strategies on Acute Kidney Injury in Patients with Septic Shock. Am. J. Respir. Crit. Care Med. 2016, 193, 281–287. [Google Scholar] [CrossRef]
- Ronco, C.; Bellomo, R.; Kellum, J.A. Acute Kidney Injury. Lancet 2019, 394, 1949–1964. [Google Scholar] [CrossRef]
- Bellomo, R.; Kellum, J.A.; Ronco, C.; Wald, R.; Martensson, J.; Maiden, M.; Bagshaw, S.M.; Glassford, N.J.; Lankadeva, Y.; Vaara, S.T.; et al. Acute Kidney Injury in Sepsis. Intensive Care Med. 2017, 43, 816–828. [Google Scholar] [CrossRef] [PubMed]
- Joffre, J.; Hellman, J.; Ince, C.; Ait-Oufella, H. Endothelial Responses in Sepsis. Am. J. Respir. Crit. Care Med. 2020, 202, 361–370. [Google Scholar] [CrossRef]
- Petejova, N.; Martinek, A.; Zadrazil, J.; Kanova, M.; Klementa, V.; Sigutova, R.; Kacirova, I.; Hrabovsky, V.; Svagera, Z.; Stejskal, D. Acute Kidney Injury in Septic Patients Treated by Selected Nephrotoxic Antibiotic Agents-Pathophysiology and Biomarkers-A Review. Int. J. Mol. Sci. 2020, 21, 7115. [Google Scholar] [CrossRef]
- Morrell, E.D.; Kellum, J.A.; Pastor-Soler, N.M.; Hallows, K.R. Septic Acute Kidney Injury: Molecular Mechanisms and the Importance of Stratification and Targeting Therapy. Crit. Care 2014, 18, 501. [Google Scholar] [CrossRef] [PubMed]
- Chelazzi, C.; Villa, G.; Mancinelli, P.; De Gaudio, A.R.; Adembri, C. Glycocalyx and Sepsis-Induced Alterations in Vascular Permeability. Crit. Care 2015, 19, 26. [Google Scholar] [CrossRef] [PubMed]
- Okada, H.; Takemura, G.; Suzuki, K.; Oda, K.; Takada, C.; Hotta, Y.; Miyazaki, N.; Tsujimoto, A.; Muraki, I.; Ando, Y.; et al. Three-Dimensional Ultrastructure of Capillary Endothelial Glycocalyx Under Normal and Experimental Endotoxemic Conditions. Crit. Care 2017, 21, 261. [Google Scholar] [CrossRef]
- Peerapornratana, S.; Manrique-Caballero, C.L.; Gómez, H.; Kellum, J.A. Acute Kidney Injury from Sepsis: Current Concepts, Epidemiology, Pathophysiology, Prevention and Treatment. Kidney Int. 2019, 96, 1083–1099. [Google Scholar] [CrossRef]
- Evans, L.; Rhodes, A.; Alhazzani, W.; Antonelli, M.; Coopersmith, C.M.; French, C.; Machado, F.R.; McIntyre, L.; Ostermann, M.; Prescott, H.C.; et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock 2021. Intensive Care Med. 2021, 47, 1181–1247. [Google Scholar] [CrossRef]
- Egi, M.; Ogura, H.; Yatabe, T.; Atagi, K.; Inoue, S.; Iba, T.; Kakihana, Y.; Kawasaki, T.; Kushimoto, S.; Kuroda, Y.; et al. The Japanese Clinical Practice Guidelines for Management of Sepsis and Septic Shock 2020 (J-SSCG 2020). J. Intensive Care 2021, 9, 53. [Google Scholar] [CrossRef]
- Zarbock, A.; Kellum, J.A.; Schmidt, C.; Van Aken, H.; Wempe, C.; Pavenstädt, H.; Boanta, A.; Gerß, J.; Meersch, M. Effect of Early vs Delayed Initiation of Renal Replacement Therapy on Mortality in Critically Ill Patients with Acute Kidney Injury: The ELAIN Randomized Clinical Trial. JAMA 2016, 315, 2190–2199. [Google Scholar] [CrossRef]
- Gaudry, S.; Hajage, D.; Schortgen, F.; Martin-Lefevre, L.; Pons, B.; Boulet, E.; Boyer, A.; Chevrel, G.; Lerolle, N.; Carpentier, D.; et al. Initiation Strategies for Renal-Replacement Therapy in the Intensive Care Unit. N. Engl. J. Med. 2016, 375, 122–133. [Google Scholar] [CrossRef]
- Barbar, S.D.; Clere-Jehl, R.; Bourredjem, A.; Hernu, R.; Montini, F.; Bruyère, R.; Lebert, C.; Bohé, J.; Badie, J.; Eraldi, J.P. Timing of Renal-Replacement Therapy in Patients with Acute Kidney Injury and Sepsis. N. Engl. J. Med. 2018, 379, 1431–1442. [Google Scholar] [CrossRef]
- STARRT-AKI Investigators; Canadian Critical Care Trials Group; Australian and New Zealand Intensive Care Society Clinical Trials Group; United Kingdom Critical Care Research Group; Canadian Nephrology Trials Network; Irish Critical Care Trials Group; Bagshaw, S.M.; Wald, R.; Adhikari, N.K.J.; Bellomo, R.; et al. Timing of Initiation of Renal-Replacement Therapy in Acute Kidney Injury. N. Engl. J. Med. 2020, 383, 240–251. [Google Scholar] [PubMed]
- Gaudry, S.; Hajage, D.; Martin-Lefevre, L.; Lebbah, S.; Louis, G.; Moschietto, S.; Titeca-Beauport, D.; Combe, B.; Pons, B.; de Prost, N.; et al. Comparison of Two Delayed Strategies for Renal Replacement Therapy Initiation for Severe Acute Kidney Injury (AKIKI 2): A Multicentre, Open-Label, Randomised, Controlled Trial. Lancet 2021, 397, 1293–1300. [Google Scholar] [CrossRef] [PubMed]
- Ronco, C.; Bellomo, R.; Homel, P.; Brendolan, A.; Dan, M.; Piccinni, P.; La Greca, G. Effects of Different Doses in Continuous Veno-Venous Haemofiltration on Outcomes of Acute Renal Failure: A Prospective Randomised Trial. Lancet 2000, 356, 26–30. [Google Scholar] [CrossRef] [PubMed]
- VA/NIH Acute Renal Failure Trial Network; Palevsky, P.M.; Zhang, J.H.; O’Connor, T.Z.; Chertow, G.M.; Crowley, S.T.; Choudhury, D.; Finkel, K.; Kellum, J.A.; Paganini, E.; et al. Intensity of Renal Support in Critically Ill Patients with Acute Kidney Injury. N. Engl. J. Med. 2008, 359, 7–20. [Google Scholar]
- RENAL Replacement Therapy Study Investigators; Bellomo, R.; Cass, A.; Cole, L.; Finfer, S.; Gallagher, M.; Lo, S.; McArthur, C.; McGuinness, S.; Myburgh, J.; et al. Intensity of Continuous Renal-Replacement Therapy in Critically Ill Patients. N. Engl. J. Med. 2009, 361, 1627–1638. [Google Scholar]
- Fayad, A.I.; Buamscha, D.G.; Ciapponi, A. Intensity of Continuous Renal Replacement Therapy for Acute Kidney Injury. Cochrane Database Syst. Rev. 2016, 10, CD010613. [Google Scholar] [CrossRef]
- Thomas, M.; Moriyama, K.; Ledebo, I. AN69: Evolution of the World’s First High Permeability Membrane. Contrib. Nephrol. 2011, 173, 119–129. [Google Scholar]
- Désormeaux, A.; Moreau, M.E.; Lepage, Y.; Chanard, J.; Adam, A. The Effect of Electronegativity and Angiotensin-Converting Enzyme Inhibition on the Kinin-Forming Capacity of Polyacrylonitrile Dialysis Membranes. Biomaterials 2008, 29, 1139–1146. [Google Scholar] [CrossRef][Green Version]
- Hellman, T.; Uusalo, P.; Järvisalo, M.J. Renal Replacement Techniques in Septic Shock. Int. J. Mol. Sci. 2021, 22, 10238. [Google Scholar] [CrossRef]
- Cole, L.; Bellomo, R.; Hart, G.; Journois, D.; Davenport, P.; Tipping, P.; Ronco, C. A Phase II Randomized, Controlled Trial of Continuous Hemofiltration in Sepsis. Crit. Care Med. 2002, 30, 100–106. [Google Scholar] [CrossRef]
- Haase, M.; Silvester, W.; Uchino, S.; Goldsmith, D.; Davenport, P.; Tipping, P.; Boyce, N.; Bellomo, R. A Pilot Study of High-Adsorption Hemofiltration in Human Septic Shock. Int. J. Artif. Organs 2007, 30, 108–117. [Google Scholar] [CrossRef]
- Peng, Z.; Pai, P.; Hong-Bao, L.; Rong, L.; Han-Min, W.; Chen, H. The Impacts of Continuous Veno-Venous Hemofiltration on Plasma Cytokines and Monocyte Human Leukocyte Antigen-DR Expression in Septic Patients. Cytokine 2010, 50, 186–191. [Google Scholar] [CrossRef] [PubMed]
- Peng, Z.; Pai, P.; Han-Min, W.; Jun, Z.; Hong-Bao, L.; Rong, L.; Chen, H. Evaluation of the Effects of Pulse High-Volume Hemofiltration in Patients with Severe Sepsis: A Preliminary Study. Int. J. Artif. Organs 2010, 33, 505–511. [Google Scholar] [CrossRef]
- Peng, Y.; Yuan, Z.; Li, H. Removal of Inflammatory Cytokines and Endotoxin by Veno-Venous Continuous Renal Replacement Therapy for Burned Patients with Sepsis. Burns 2005, 31, 623–628. [Google Scholar] [CrossRef] [PubMed]
- Broman, M.E.; Hansson, F.; Vincent, J.L.; Bodelsson, M. Endotoxin and Cytokine Reducing Properties of the oXiris Membrane in Patients with Septic Shock: A Randomized Crossover Double-Blind Study. PLoS ONE 2019, 14, e0220444. [Google Scholar] [CrossRef] [PubMed]
- Moriyama, K.; Kato, Y.; Hasegawa, D.; Kurimoto, Y.; Kawaji, T.; Nakamura, T.; Kuriyama, N.; Shimomura, Y.; Nishida, O. Involvement of Ionic Interactions in Cytokine Adsorption of Polyethyleneimine-Coated Polyacrylonitrile and Polymethyl Methacrylate Membranes In Vitro. J. Artif. Organs 2020, 23, 240–246. [Google Scholar] [CrossRef]
- Kishikawa, T.; Fujieda, H.; Sakaguchi, H. Comprehensive Analysis of Cytokine Adsorption Properties of Polymethyl Methacrylate (PMMA) Membrane Material. J. Artif. Organs 2022, 25, 343–349. [Google Scholar] [CrossRef]
- Nakada, T.A.; Oda, S.; Matsuda, K.; Sadahiro, T.; Nakamura, M.; Abe, R.; Hirasawa, H. Continuous Hemodiafiltration with PMMA Hemofilter in the Treatment of Patients with Septic Shock. Mol. Med. 2008, 14, 257–263. [Google Scholar] [CrossRef] [PubMed]
- Matsuda, K.; Moriguchi, T.; Harii, N.; Yanagisawa, M.; Harada, D.; Sugawara, H. Comparison of Efficacy between Continuous Hemodiafiltration with a PMMA High-Performance Membrane Dialyzer and a PAN Membrane Hemofilter in the Treatment of Septic Shock Patients with Acute Renal Failure. Contrib. Nephrol. 2011, 173, 182–190. [Google Scholar] [PubMed]
- Sakamoto, Y.; Mashiko, K.; Obata, T.; Matsumoto, H.; Hara, Y.; Kutsukata, N.; Yamamoto, Y. Effectiveness of Continuous Hemodiafiltration Using a Polymethylmethacrylate Membrane Hemofilter after Polymyxin B-Immobilized Fiber Column Therapy of Septic Shock. Crit. Care 2008, 54, 129–132. [Google Scholar] [CrossRef] [PubMed]
- Kobashi, S.; Maruhashi, T.; Nakamura, T.; Hatabayashi, E.; Kon, A. The 28-Day Survival Rates of Two Cytokine-Adsorbing Hemofilters for Continuous Renal Replacement Therapy: A Single-Center Retrospective Comparative Study. Acute Med. Surg. 2019, 6, 60–67. [Google Scholar] [CrossRef]
- Tanaka, A.; Inaguma, D.; Nakamura, T.; Watanabe, Y.; Ito, E.; Kamegai, N.; Shimogushi, H.; Murata, M.; Shinjo, H.; Koike, K. Effect of Continuous Hemodiafiltration Using an AN69ST Membrane in Patients with Sepsis. Ren. Replace. Ther. 2017, 3, 12. [Google Scholar] [CrossRef]
- Schädler, D.; Pausch, C.; Heise, D.; Meier-Hellmann, A.; Brederlau, J.; Weiler, N.; Marx, G.; Putensen, C.; Spies, C.; Jörres, A.; et al. The Effect of a Novel Extracorporeal Cytokine Hemoadsorption Device on IL-6 Elimination in Septic Patients: A Randomized Controlled Trial. PLoS ONE 2017, 12, e0187015. [Google Scholar] [CrossRef] [PubMed]
- Hawchar, F.; László, I.; Öveges, N.; Trásy, D.; Ondrik, Z.; Molnar, Z. Extracorporeal Cytokine Adsorption in Septic Shock: A Proof of Concept Randomized, Controlled Pilot Study. J. Crit. Care 2019, 49, 172–178. [Google Scholar] [CrossRef]
- Diab, M.; Lehmann, T.; Bothe, W.; Akhyari, P.; Platzer, S.; Wendt, D.; Deppe, A.C.; Strauch, J.; Hagel, S.; Günther, A.; et al. Cytokine Hemoadsorption during Cardiac Surgery versus Standard Surgical Care for Infective Endocarditis (REMOVE): Results from a Multicenter Randomized Controlled Trial. Circulation 2022, 145, 959–968. [Google Scholar] [CrossRef]
- Cruz, D.N.; Antonelli, M.; Fumagalli, R.; Foltran, F.; Brienza, N.; Donati, A.; Malcangi, V.; Petrini, F.; Volta, G.; Bobbio Pallavicini, F.M.; et al. Early Use of Polymyxin B Hemoperfusion in Abdominal Septic Shock: The EUPHAS Randomized Controlled Trial. JAMA 2009, 301, 2445–2452. [Google Scholar] [CrossRef]
- Kellum, J.A.; Uchino, S. International Differences in the Treatment of Sepsis: Are They Justified? JAMA 2009, 301, 2496–2497. [Google Scholar] [CrossRef]
- Payen, D.M.; Guilhot, J.; Launey, Y.; Lukaszewicz, A.C.; Kaaki, M.; Veber, B.; Pottecher, J.; Joannes-Boyau, O.; Martin-Lefevre, L.; Jabaudon, M.; et al. Early Use of Polymyxin B Hemoperfusion in Patients with Septic Shock Due to Peritonitis: A Multicenter Randomized Control Trial. Intensive Care Med. 2015, 41, 975–984. [Google Scholar] [CrossRef]
- Ronco, C.; Klein, D.J. Polymyxin B Hemoperfusion: A Mechanistic Perspective. Crit. Care 2014, 18, 309. [Google Scholar] [CrossRef] [PubMed]
- Rhodes, A.; Evans, L.E.; Alhazzani, W.; Levy, M.M.; Antonelli, M.; Ferrer, R.; Kumar, A.; Sevransky, J.E.; Sprung, C.L.; Nunnally, M.E.; et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Med. 2017, 43, 304–377. [Google Scholar] [CrossRef] [PubMed]
- Dellinger, R.P.; Bagshaw, S.M.; Antonelli, M.; Foster, D.M.; Klein, D.J.; Marshall, J.C.; Palevsky, P.M.; Weisberg, L.S.; Schorr, C.A.; Trzeciak, S.; et al. Effect of Targeted Polymyxin B Hemoperfusion on 28-Day Mortality in Patients with Septic Shock and Elevated Endotoxin Level: The Euphrates Randomized Clinical Trial. JAMA 2018, 320, 1455–1463. [Google Scholar] [CrossRef] [PubMed]
- Klein, D.J.; Foster, D.; Walker, P.M.; Bagshaw, S.M.; Mekonnen, H.; Antonelli, M. Polymyxin B Hemoperfusion in Endotoxemic Septic Shock Patients Without Extreme Endotoxemia: A Post hoc Analysis of the Euphrates Trial. Intensive Care Med. 2018, 44, 2205–2212. [Google Scholar] [CrossRef] [PubMed]
- Iba, T.; Klein, D.J. The Wind Changed Direction and the Big River Still Flows: From Euphrates to TIGRIS. J. Intensive Care 2019, 7, 31. [Google Scholar] [CrossRef]
- Chang, T.; Tu, Y.K.; Lee, C.T.; Chao, A.; Huang, C.H.; Wang, M.J.; Yeh, Y.C. Effects of Polymyxin B Hemoperfusion on Mortality in Patients with Severe Sepsis and Septic Shock: A Systemic Review, Meta-Analysis Update, and Disease Severity Subgroup Meta-Analysis. Crit. Care Med. 2017, 45, e858–e864. [Google Scholar] [CrossRef] [PubMed]
- Monard, C.; Rimmelé, T.; Ronco, C. Extracorporeal Blood Purification Therapies for Sepsis. Blood Purif. 2019, 47 (Suppl. S3), 205. [Google Scholar] [CrossRef]
- Honore, P.M.; Hoste, E.; Molnár, Z.; Jacobs, R.; Joannes-Boyau, O.; Malbrain, M.L.N.G.; Forni, L.G. Cytokine Removal in Human Septic Shock: Where Are We and Where Are We Going? Ann. Intensive Care 2019, 9, 56. [Google Scholar] [CrossRef]
- Feng, Y.; Peng, J.Y.; Peng, Z. Blood Purification in Sepsis and Systemic Inflammation. Curr. Opin. Crit. Care 2021, 27, 582–586. [Google Scholar] [CrossRef] [PubMed]
| RIFLE [14] | AKIN [15] | KDIGO [16] | |
|---|---|---|---|
| Diagnostic criteria | NA | Increase in serum creatinine level of ≥0.3 mg/dL or ≥50% within 48 h | Increase in serum creatinine level of ≥0.3 mg/dL within 48 h or ≥50% within 7 days |
| OR | OR | ||
| Urine output of <0.5 mL/kg/h for >6 h | Urine output of <0.5 mL/kg/h for > 6 h | ||
| Staging criteria | |||
| Risk (RIFLE) or stage 1 (AKIN/KDIGO) | Increase in serum creatinine level to 1.5 times the baseline value | Increase in serum creatinine level of ≥ 0.3 mg/dL or to 150–200% of the baseline value | Increase in serum creatinine level of ≥ 0.3 mg/dL or 1.5–1.9 times the baseline value |
| OR | OR | OR | |
| Urine output of < 0.5 mL/kg/h for 6–12 h | Urine output of < 0.5 mL/kg/h for 6–12 h | Urine output of < 0.5 mL/kg/h for 6–12 h | |
| Injury (RIFLE) or stage 2 (AKIN/KDIGO) | Increase in serum creatinine level to 2 times the baseline value | Increase in serum creatinine level to 200–300% of the baseline value | Increase in serum creatinine level to 2.0–2.9 times the baseline value |
| OR | OR | OR | |
| Urine output of < 0.5 mL/kg/h for 12–24 h | Urine output of < 0.5 mL/kg/h for 12–24 h | Urine output of < 0.5 mL/kg/h for 12–24 h | |
| Failure (RIFLE) or stage 3 (AKIN/KDIGO) | Increase in serum creatinine level to 3 times the baseline value | Increase in serum creatinine level to > 300% of the baseline value | Increase in serum creatinine level to ≥ 3.0 times the baseline value |
| OR | OR | OR | |
| Increase in serum creatinine level of 0.5 mg/dL to > 4.0 mg/dL | Increase in serum creatinine level by > 0.5 mg/dL to ≥ 4.0 mg/dL | Increase in serum creatinine level of ≥ 0.3 mg/dL to ≥ 4.0 mg/dL | |
| OR | OR | OR | |
| Urine output of < 0.3 mL/kg/h for > 24 h or anuria for > 12 h | Urine output of < 0.3 mL/kg/h for > 24 h or anuria for > 12 h | Urine output of < 0.3 mL/kg/h for ≥ 24 h or anuria for ≥ 12 h | |
| OR | OR | OR | |
| Initiation of kidney replacement therapy | Initiation of kidney replacement therapy | Initiation of kidney replacement therapy | |
| Loss (RIFLE) | Need for kidney replacement therapy for > 4 weeks | ||
| End stage (RIFLE) | Need for kidney replacement therapy for > 3 months |
| Study | Design | Year | n | KRT Indication | Mortality | Difference | Consideration | |
|---|---|---|---|---|---|---|---|---|
| ELAIN [39] | RCT | 2016 | 231 | Early | KDIGO stage 2 within 8 h | At 90 days | 39.3% p = 0.03 54.7% | CKRT only |
| Delayed | KDIGO stage 3 within < 12 h Absolute indication | |||||||
| AKIKI [40] | RCT | 2016 | 620 | Early | KDIGO stage 3 within 6 h, | At 60 days | 48.5% n.s 49.7% | CRBSI higher in early group than in the late group |
| Delayed | hyperkalemia, metabolic acidosis, pulmonary edema, BUN level > 40 mg/dL, or oliguria for > 72 h | |||||||
| IDEAL-ICU [41] | RCT | 2018 | 488 | Early | RIFLE-Failure within 12 h | At 90 days | 58% n.s 54% | Hyperkalemia greater in the delayed group than in the non-delayed group Septic shock: 100% |
| Delayed | Absence of kidney recovery after 48 h | |||||||
| STARRT-AKI [42] | RCT | 2020 | 2927 | Early | KDIGO stage 2 or 3 within 12 h | At 90 days | 43.9% n.s 43.7% | |
| Delayed | K > 6.0 mmol/L, pH < 7.20, HCO3- level < 12 mmol/L, pulmonary edema with P/F < 200 for ≥ 72 h | |||||||
| AKIKI-2 [43] | RCT | 2021 | 278 | Early | KDIGO stage 3 with oliguria > 72 h or BUN level 40–50 mmol/L within 12 h | At 60 days | 44% n.s 55% | |
| Delayed | BUN level > 140 mg/dL Absolute indication | |||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kamei, J.; Kanamoto, M.; Igarashi, Y.; Suzuki, K.; Fujita, K.; Kuwana, T.; Ogura, T.; Mochizuki, K.; Banshotani, Y.; Ishikura, H.; et al. Blood Purification in Patients with Sepsis Associated with Acute Kidney Injury: A Narrative Review. J. Clin. Med. 2023, 12, 6388. https://doi.org/10.3390/jcm12196388
Kamei J, Kanamoto M, Igarashi Y, Suzuki K, Fujita K, Kuwana T, Ogura T, Mochizuki K, Banshotani Y, Ishikura H, et al. Blood Purification in Patients with Sepsis Associated with Acute Kidney Injury: A Narrative Review. Journal of Clinical Medicine. 2023; 12(19):6388. https://doi.org/10.3390/jcm12196388
Chicago/Turabian StyleKamei, Jun, Masafumi Kanamoto, Yutaka Igarashi, Kodai Suzuki, Kensuke Fujita, Tsukasa Kuwana, Takayuki Ogura, Katsunori Mochizuki, Yuki Banshotani, Hiroyasu Ishikura, and et al. 2023. "Blood Purification in Patients with Sepsis Associated with Acute Kidney Injury: A Narrative Review" Journal of Clinical Medicine 12, no. 19: 6388. https://doi.org/10.3390/jcm12196388
APA StyleKamei, J., Kanamoto, M., Igarashi, Y., Suzuki, K., Fujita, K., Kuwana, T., Ogura, T., Mochizuki, K., Banshotani, Y., Ishikura, H., Nakamura, Y., & J-STAD (Japan Sepsis Treatment and Diagnosis) Study Group. (2023). Blood Purification in Patients with Sepsis Associated with Acute Kidney Injury: A Narrative Review. Journal of Clinical Medicine, 12(19), 6388. https://doi.org/10.3390/jcm12196388






