Liver-Support Therapies in Critical Illness—A Comparative Analysis of Procedural Characteristics and Safety
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Data Collection and Definitions
2.3. Statistical Analysis
3. Results
3.1. Patient and Treatment Characteristics
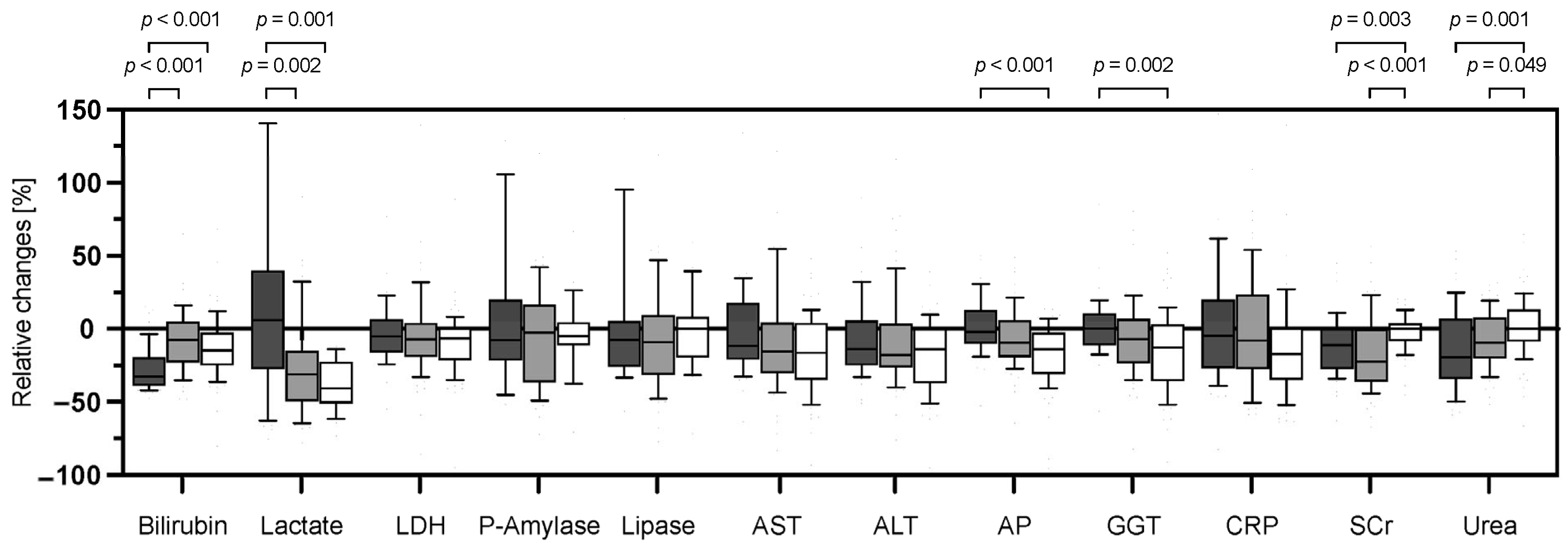
3.2. Changes of Routine Laboratory Parameters in Response to Extracorporeal Liver Support Therapies
3.3. Concentration-Dependent Clearance of Different Liver-Support Modalities
| CytoSorb | MARS | TPE | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Parameter | r | 95% CI | p Value | R2 | r | 95% CI | p Value | R2 | r | 95% CI | p Value | R2 |
| Total bilirubin | −0.79 | −0.86–−0.70 | 0.001 | 0.63 | −0.61 | −0.75–−0.43 | 0.001 | 0.37 | −0.55 | −0.69–−0.37 | 0.001 | 0.44 |
| Lactate | −0.23 | −0.42–−0.01 | 0.034 | 0.13 | −0.54 | −0.71–−0.32 | 0.001 | 0.29 | −0.70 | −0.87–−0.40 | 0.001 | 0.47 |
| LDH | 0.15 | −0.09–0.37 | 0.200 | 0.01 | −0.42 | −0.61–−0.20 | 0.001 | 0.18 | −0.50 | −0.65–−0.29 | 0.001 | 0.44 |
| P-Amylase | −0.41 | −0.61–−0.16 | 0.002 | 0.56 | −0.35 | −0.55–−0.11 | 0.006 | 0.12 | −0.47 | −0.75–−0.06 | 0.022 | 0.55 |
| Lipase | −0.30 | −0.54–−0.01 | 0.035 | 0.93 | −0.49 | −0.66–−0.27 | 0.001 | 0.24 | −0.20 | −0.57–+0.23 | 0.346 | 0.27 |
| AST | −0.45 | −0.61–−0.24 | 0.001 | 0.57 | −0.45 | −0.63–−0.23 | 0.001 | 0.21 | −0.68 | −0.78–−0.52 | 0.001 | 0.99 |
| ALT | −0.51 | −0.66–−0.32 | 0.001 | 0.71 | −0.65 | −0.77–−0.47 | 0.001 | 0.42 | −0.77 | −0.85–−0.65 | 0.001 | 0.95 |
| AP | −0.35 | −0.54–−0.14 | 0.001 | 0.08 | −0.63 | −0.76–−0.45 | 0.001 | 0.40 | −0.71 | −0.81–−0.58 | 0.001 | 0.94 |
| GGT | −0.16 | −0.37–+0.06 | 0.141 | 0.14 | −0.54 | −0.69–−0.33 | 0.001 | 0.29 | −0.71 | −0.81–−0.58 | 0.001 | 0.93 |
| CRP | −0.34 | −0.53–−0.12 | 0.002 | 0.03 | −0.18 | −0.42–+0.09 | 0.200 | 0.03 | −0.67 | −0.78–−0.51 | 0.001 | 0.44 |
| SCr | −0.18 | −0.45–+0.13 | 0.232 | 0.07 | −0.57 | −0.72–−0.37 | 0.001 | 0.23 | −0.41 | −0.58–−0.20 | 0.001 | 0.35 |
| Urea | −0.13 | −0.42–+0.17 | 0.378 | 0.02 | −0.47 | −0.65–−0.25 | 0.001 | 0.37 | −0.31 | 0.51–−0.09 | 0.005 | 0.17 |
| CytoSorb | MARS | TPE | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Cut-Off Bilirubin | N | Median [%] | IQR [%] | N | Median [%] | IQR [%] | N | Median [%] | IQR [%] |
| >20 mg/dL | 36 | −33.8 | −41.2–−24.3 | 5 | −39.3 | −48.1–−33.7 | 9 | −28.4 | −37.4–−23.7 |
| >15–20 mg/dL | 11 | −32.0 | −39.9–−23.0 | 16 | −15.2 | −28.3–−1.5 | 21 | −17.2 | −23.6–−2.1 |
| >10–15 mg/dL | 4 | −14.4 | −22.1–+5.5 | 33 | −4.9 | −12.7–+6.3 | 18 | −20.3 | −32.3–+8.2 |
| ≤10 mg/dL | 6 | +2.5 | −9.9–+13.6 | 8 | −0.9 | −9.6–+9.8 | 29 | −10.5 | −20.9–−2.3 |
3.4. Complications and Safety Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Halpern, N.A.; Pastores, S.M. Critical Care Medicine in the United States 2000–2005: An Analysis of Bed Numbers, Occupancy Rates, Payer Mix, and Costs. Crit. Care Med. 2010, 38, 65–71. [Google Scholar] [CrossRef] [PubMed]
- Vaara, S.T.; Pettilä, V.; Reinikainen, M.; Kaukonen, K.-M.; Consortium, F.I.C. Population-Based Incidence, Mortality and Quality of Life in Critically Ill Patients Treated with Renal Replacement Therapy: A Nationwide Retrospective Cohort Study in Finnish Intensive Care Units. Crit. Care 2012, 16, R13. [Google Scholar] [CrossRef] [PubMed]
- Hoste, E.A.J.; Bagshaw, S.M.; Bellomo, R.; Cely, C.M.; Colman, R.; Cruz, D.N.; Edipidis, K.; Forni, L.G.; Gomersall, C.D.; Govil, D.; et al. Epidemiology of Acute Kidney Injury in Critically Ill Patients: The Multinational AKI-EPI Study. Intensive Care Med. 2015, 41, 1411–1423. [Google Scholar] [CrossRef]
- Nusshag, C.; Weigand, M.A.; Zeier, M.; Morath, C.; Brenner, T. Issues of Acute Kidney Injury Staging and Management in Sepsis and Critical Illness: A Narrative Review. Int. J. Mol. Sci. 2017, 18, 1387. [Google Scholar] [CrossRef]
- Gaudry, S.; Hajage, D.; Martin-Lefevre, L.; Lebbah, S.; Louis, G.; Moschietto, S.; Titeca-Beauport, D.; Combe, B.L.; Pons, B.; de Prost, N.; et al. Comparison of Two Delayed Strategies for Renal Replacement Therapy Initiation for Severe Acute Kidney Injury (AKIKI 2): A Multicentre, Open-Label, Randomised, Controlled Trial. Lancet 2021, 397, 1293–1300. [Google Scholar] [CrossRef] [PubMed]
- Kellum, J.A.; Prowle, J.R. Paradigms of Acute Kidney Injury in the Intensive Care Setting. Nat. Rev. Nephrol. 2018, 307, 217–230. [Google Scholar] [CrossRef] [PubMed]
- Saliba, F.; Bañares, R.; Larsen, F.S.; Wilmer, A.; Parés, A.; Mitzner, S.; Stange, J.; Fuhrmann, V.; Gilg, S.; Hassanein, T.; et al. Artificial Liver Support in Patients with Liver Failure: A Modified DELPHI Consensus of International Experts. Intensive Care Med. 2022, 48, 1352–1367. [Google Scholar] [CrossRef] [PubMed]
- Pickkers, P.; Darmon, M.; Hoste, E.; Joannidis, M.; Legrand, M.; Ostermann, M.; Prowle, J.R.; Schneider, A.; Schetz, M. Acute Kidney Injury in the Critically Ill: An Updated Review on Pathophysiology and Management. Intensive Care Med. 2021, 47, 835–850. [Google Scholar] [CrossRef]
- Chris-Olaiya, A.; Kapoor, A.; Ricci, K.S.; Lindenmeyer, C.C. Therapeutic Plasma Exchange in Liver Failure. World J. Hepatol. 2021, 13, 904–915. [Google Scholar] [CrossRef]
- William, B.; Julia, W. Acute Liver Failure. N. Engl. J. Med. 2013, 369, 2525–2534. [Google Scholar] [CrossRef]
- Bernal, W. The Liver in Systemic Disease: Sepsis and Critical Illness. Clin. Liver Dis. 2016, 7, 88–91. [Google Scholar] [CrossRef] [PubMed]
- Wendon, J.; Cordoba, J.; Dhawan, A.; Larsen, F.S.; Manns, M.; Nevens, F.; Samuel, D.; Simpson, K.J.; Yaron, I.; Bernardi, M. EASL Clinical Practical Guidelines on the Management of Acute (Fulminant) Liver Failure. J. Hepatol. 2017, 66, 1047–1081. [Google Scholar] [CrossRef]
- Horvatits, T.; Trauner, M.; Fuhrmann, V. Hypoxic Liver Injury and Cholestasis in Critically Ill Patients. Curr. Opin. Crit. Care 2013, 19, 128–132. [Google Scholar] [CrossRef]
- Horvatits, T.; Drolz, A.; Trauner, M.; Fuhrmann, V. Liver Injury and Failure in Critical Illness. Hepatology 2019, 70, 2204–2215. [Google Scholar] [CrossRef] [PubMed]
- Vitek, L.; Hubacek, J.A.; Pajak, A.; Doryńska, A.; Kozela, M.; Eremiasova, L.; Danzig, V.; Stefler, D.; Bobak, M. Association between Plasma Bilirubin and Mortality. Ann. Hepatol. 2019, 18, 379–385. [Google Scholar] [CrossRef] [PubMed]
- Kramer, L.; Jordan, B.; Druml, W.; Bauer, P.; Metnitz, P.G.H. Incidence and Prognosis of Early Hepatic Dysfunction in Critically Ill Patients—A Prospective Multicenter Study. Crit. Care Med. 2007, 35, 1099-e7. [Google Scholar] [CrossRef]
- Larsen, F.S.; Schmidt, L.E.; Bernsmeier, C.; Rasmussen, A.; Isoniemi, H.; Patel, V.C.; Triantafyllou, E.; Bernal, W.; Auzinger, G.; Shawcross, D.; et al. High-Volume Plasma Exchange in Patients with Acute Liver Failure: An Open Randomised Controlled Trial. J. Hepatol. 2016, 64, 69–78. [Google Scholar] [CrossRef]
- de Garibay, A.P.R.; Kortgen, A.; Leonhardt, J.; Zipprich, A.; Bauer, M. Critical Care Hepatology: Definitions, Incidence, Prognosis and Role of Liver Failure in Critically Ill Patients. Crit. Care 2022, 26, 289. [Google Scholar] [CrossRef]
- Ocskay, K.; Kanjo, A.; Gede, N.; Szakács, Z.; Pár, G.; Erőss, B.; Stange, J.; Mitzner, S.; Hegyi, P.; Molnár, Z. Uncertainty in the Impact of Liver Support Systems in Acute-on-Chronic Liver Failure: A Systematic Review and Network Meta-Analysis. Ann. Intensive Care 2021, 11, 10. [Google Scholar] [CrossRef]
- Gerth, H.U.; Pohlen, M.; Thölking, G.; Pavenstädt, H.; Brand, M.; Hüsing-Kabar, A.; Wilms, C.; Maschmeier, M.; Kabar, I.; Torner, J.; et al. Molecular Adsorbent Recirculating System Can Reduce Short-Term Mortality Among Patients with Acute-on-Chronic Liver Failure—A Retrospective Analysis. Crit. Care Med. 2017, 45, 1616–1624. [Google Scholar] [CrossRef]
- Bañares, R.; Nevens, F.; Larsen, F.S.; Jalan, R.; Albillos, A.; Dollinger, M.; Saliba, F.; Sauerbruch, T.; Klammt, S.; Ockenga, J.; et al. Extracorporeal Albumin Dialysis with the Molecular Adsorbent Recirculating System in Acute-on-Chronic Liver Failure: The RELIEF Trial. Hepatology 2013, 57, 1153–1162. [Google Scholar] [CrossRef] [PubMed]
- Saliba, F.; Camus, C.; Durand, F.; Mathurin, P.; Letierce, A.; Delafosse, B.; Barange, K.; Perrigault, P.F.; Belnard, M.; Ichaï, P.; et al. Albumin Dialysis with a Noncell Artificial Liver Support Device in Patients with Acute Liver Failure: A Randomized, Controlled Trial. Ann. Intern. Med. 2013, 159, 522–531. [Google Scholar] [CrossRef] [PubMed]
- Kantola, T.; Koivusalo, A.; Höckerstedt, K.; Isoniemi, H. The Effect of Molecular Adsorbent Recirculating System Treatment on Survival, Native Liver Recovery, and Need for Liver Transplantation in Acute Liver Failure Patients*. Transpl. Int. 2008, 21, 857–866. [Google Scholar] [CrossRef] [PubMed]
- Bañares, R.; Ibáñez-Samaniego, L.; Torner, J.M.; Pavesi, M.; Olmedo, C.; Catalina, M.V.; Albillos, A.; Larsen, F.S.; Nevens, F.; Hassanein, T.; et al. Meta-Analysis of Individual Patient Data of Albumin Dialysis in Acute-on-Chronic Liver Failure: Focus on Treatment Intensity. Ther. Adv. Gastroenter. 2019, 12, 1756284819879565. [Google Scholar] [CrossRef] [PubMed]
- Pufal, K.; Lawson, A.; Hodson, J.; Bangash, M.; Patel, J.; Weston, C.; van Gulik, T.; Dasari, B.V. Role of Liver Support Systems in the Management of Post Hepatectomy Liver Failure: A Systematic Review of the Literature. Ann. Hepato Biliary Pancreat. Surg. 2021, 25, 171–178. [Google Scholar] [CrossRef]
- Mehta, Y.; Mehta, C.; Kumar, A.; George, J.V.; Gupta, A.; Nanda, S.; Kochhar, G.; Raizada, A. Experience with Hemoadsorption (CytoSorb®) in the Management of Septic Shock Patients. World J. Crit. Care Med. 2020, 9, 1–12. [Google Scholar] [CrossRef]
- Kogelmann, K.; Jarczak, D.; Scheller, M.; Drüner, M. Hemoadsorption by CytoSorb in Septic Patients: A Case Series. Crit. Care 2017, 21, 74. [Google Scholar] [CrossRef]
- Ocskay, K.; Tomescu, D.; Faltlhauser, A.; Jacob, D.; Friesecke, S.; Malbrain, M.; Kogelmann, K.; Bogdanski, R.; Bach, F.; Fritz, H.; et al. Hemoadsorption in ‘Liver Indication’—Analysis of 109 Patients’ Data from the CytoSorb International Registry. J. Clin. Med. 2021, 10, 5182. [Google Scholar] [CrossRef]
- Tomescu, D.; Popescu, M.; David, C.; Sima, R.; Dima, S. Haemoadsorption by CytoSorb® in Patients with Acute Liver Failure: A Case Series. Int. J. Artif. Organs 2020, 44, 560–564. [Google Scholar] [CrossRef]
- Dhokia, V.; Madhavan, D.; Austin, A.; Morris, C.G. Novel Use of CytosorbTM Haemadsorption to Provide Biochemical Control in Liver Impairment. J. Intensive Care Soc. 2019, 20, 174–181. [Google Scholar] [CrossRef]
- Dominik, A.; Stange, J. Similarities, Differences, and Potential Synergies in the Mechanism of Action of Albumin Dialysis Using the MARS Albumin Dialysis Device and the CytoSorb Hemoperfusion Device in the Treatment of Liver Failure. Blood Purif. 2021, 50, 119–128. [Google Scholar] [CrossRef] [PubMed]
- Popescu, M.; David, C.; Marcu, A.; Olita, M.R.; Mihaila, M.; Tomescu, D. Artificial Liver Support with CytoSorb and MARS in Liver Failure: A Retrospective Propensity Matched Analysis. J. Clin. Med. 2023, 12, 2258. [Google Scholar] [CrossRef] [PubMed]
- Scharf, C.; Liebchen, U.; Paal, M.; Becker-Pennrich, A.; Irlbeck, M.; Zoller, M.; Schroeder, I. Successful Elimination of Bilirubin in Critically Ill Patients with Acute Liver Dysfunction Using a Cytokine Adsorber and Albumin Dialysis: A Pilot Study. Sci. Rep. 2021, 11, 10190. [Google Scholar] [CrossRef] [PubMed]
- Sparrelid, E.; Gilg, S.; van Gulik, T.M. Systematic Review of MARS Treatment in Post-Hepatectomy Liver Failure. Hpb 2020, 22, 950–960. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, A.J.; Subramanian, R.M.; Olson, J.C.; Speiser, J.L.; Durkalski-Mauldin, V.L.; Abraldes, J.G.; Bigam, D.L.; Flynn, M.M.; Rapaka, B.; Shropshire, B.M.; et al. Use of the Molecular Adsorbent Recirculating System in Acute Liver Failure: Results of a Multicenter Propensity Score-Matched Study. Crit. Care Med. 2022, 50, 286–295. [Google Scholar] [CrossRef]
- Liebchen, U.; Paal, M.; Gräfe, C.; Zoller, M.; Scharf, C.; Frank, S.; Greimel, A.; Maciuga, N.; Brozat, C.; Bruegel, M. The Cytokine Adsorber Cytosorb® Does Not Reduce Ammonia Concentrations in Critically Ill Patients with Liver Failure. Intensive Care Med. 2023, 49, 360–362. [Google Scholar] [CrossRef]
- Tampe, D.; Korsten, P.; Bremer, S.C.B.; Winkler, M.S.; Tampe, B. Kinetics of Bilirubin and Ammonia Elimination during Hemadsorption Therapy in Secondary Sclerosing Cholangitis following ECMO Therapy and Severe COVID-19. Biomedicines 2021, 9, 1841. [Google Scholar] [CrossRef]
- Calabrò, M.G.; Febres, D.; Recca, G.; Lembo, R.; Fominskiy, E.; Scandroglio, A.M.; Zangrillo, A.; Pappalardo, F. Blood Purification with CytoSorb in Critically Ill Patients: Single-Center Preliminary Experience. Artif. Organs 2019, 43, 189–194. [Google Scholar] [CrossRef]
- Maiwall, R.; Bajpai, M.; Singh, A.; Agarwal, T.; Kumar, G.; Bharadwaj, A.; Nautiyal, N.; Tevethia, H.; Jagdish, R.K.; Vijayaraghavan, R.; et al. Standard-Volume Plasma Exchange Improves Outcomes in Patients with Acute Liver Failure: A Randomized Controlled Trial. Clin. Gastroenterol. H 2022, 20, e831–e854. [Google Scholar] [CrossRef]
- Horvatits, T.; Drolz, A.; Rutter, K.; Roedl, K.; Langouche, L.; den Berghe, G.V.; Fauler, G.; Meyer, B.; Hülsmann, M.; Heinz, G.; et al. Circulating Bile Acids Predict Outcome in Critically Ill Patients. Ann. Intensive Care 2017, 7, 48. [Google Scholar] [CrossRef]
- Fickert, P.; Rosenkranz, A.R. Cholemic Nephropathy Reloaded. Semin Liver Dis. 2019, 40, 091–100. [Google Scholar] [CrossRef] [PubMed]
- Watchko, J.F. Bilirubin-Induced Neurotoxicity in the Preterm Neonate. Clin. Perinatol. 2016, 43, 297–311. [Google Scholar] [CrossRef] [PubMed]
- Perez, M.J.; Briz, O. Bile-Acid-Induced Cell Injury and Protection. World J. Gastroentero. 2009, 15, 1677–1689. [Google Scholar] [CrossRef] [PubMed]
- Knaup, H.; Stahl, K.; Schmidt, B.M.W.; Idowu, T.O.; Busch, M.; Wiesner, O.; Welte, T.; Haller, H.; Kielstein, J.T.; Hoeper, M.M.; et al. Early Therapeutic Plasma Exchange in Septic Shock: A Prospective Open-Label Nonrandomized Pilot Study Focusing on Safety, Hemodynamics, Vascular Barrier Function, and Biologic Markers. Crit. Care 2018, 22, 285. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, F.S.; Gottfried, M.; Tujios, S.; Olson, J.C.; Karvellas, C.J.; US Acute Liver Failure Study Group. Continuous Renal Replacement Therapy Is Associated with Reduced Serum Ammonia Levels and Mortality in Acute Liver Failure. Hepatology 2018, 67, 711–720. [Google Scholar] [CrossRef] [PubMed]
- Moutachakkir, M.; Hanchi, A.L.; Baraou, A.; Boukhira, A.; Chellak, S. Immunoanalytical Characteristics of C-Reactive Protein and High Sensitivity C-Reactive Protein. Ann. Biol. Clin. 2017, 75, 225–229. [Google Scholar] [CrossRef]
- Stasia, M.J.; Surla, A.; Renversez, J.C.; Pene, F.; Morel-Femelez, A.; Morel, F. Aspartate Aminotransferase Macroenzyme Complex in Serum Identified and Characterized. Clin. Chem. 1994, 40, 1340–1343. [Google Scholar] [CrossRef]
- Mason, J.E.; Starke, R.D.; Kirk, J.E.V. Gamma-Glutamyl Transferase: A Novel Cardiovascular Risk BioMarker. Prev. Cardiol. 2010, 13, 36–41. [Google Scholar] [CrossRef]
- Ghosh, N.K.; Fishman, W.H. Purification and Properties of Molecular-Weight Variants of Human Placental Alkaline Phosphatase. Biochem. J. 1968, 108, 779–792. [Google Scholar] [CrossRef]
- Caro, A.D.; Figarella, C.; Amic, J.; Michel, R.; Guy, O. Human Pancreatic Lipase: A Glycoprotein. Biochim. Biophys. Acta Bba Protein Struct. 1977, 490, 411–419. [Google Scholar] [CrossRef]
- Sky-Peck, H.H.; Thuvasethakul, P. Human Pancreatic Alpha-Amylase. I. Purification and Characterization. Ann. Clin. Lab. Sci. 1977, 7, 298–309. [Google Scholar] [PubMed]
- Jafary, F.; Ganjalikhany, M.R.; Moradi, A.; Hemati, M.; Jafari, S. Novel Peptide Inhibitors for Lactate Dehydrogenase A (LDHA): A Survey to Inhibit LDHA Activity via Disruption of Protein-Protein Interaction. Sci. Rep. 2019, 9, 4686. [Google Scholar] [CrossRef] [PubMed]
- Honore, P.M.; Gutierrez, L.B.; Kugener, L.; Redant, S.; Attou, R.; Gallerani, A.; Bels, D.D. Plasma Exchange in Critically Ill COVID-19 Patients Improved Inflammation, Microcirculatory Clot Formation, and Hypotension, Thereby Improving Clinical Outcomes: Fact or Fiction? Crit. Care 2020, 24, 551. [Google Scholar] [CrossRef] [PubMed]
- Kapoor, D. Molecular Adsorbent Recirculating System: Albumin Dialysis-based Extracorporeal Liver Assist Device. J. Gastroen. Hepatol. 2002, 17, S280–S286. [Google Scholar] [CrossRef]
- Stadlbauer, V.; Krisper, P.; Beuers, U.; Haditsch, B.; Schneditz, D.; Jung, A.; Putz-Bankuti, C.; Holzer, H.; Trauner, M.; Stauber, R.E. Removal of Bile Acids by Two Different Extracorporeal Liver Support Systems in Acute-on-Chronic Liver Failure. Asaio J. 2007, 53, 187–193. [Google Scholar] [CrossRef]
- Malard, B.; Lambert, C.; Kellum, J.A. In Vitro Comparison of the Adsorption of Inflammatory Mediators by Blood Purification Devices. Intensive Care Med. Exp. 2018, 6, 12. [Google Scholar] [CrossRef]
- Meijers, B.; Laleman, W.; Vermeersch, P.; Nevens, F.; Wilmer, A.; Evenepoel, P. A Prospective Randomized Open-Label Crossover Trial of Regional Citrate Anticoagulation vs. Anticoagulation Free Liver Dialysis by the Molecular Adsorbents Recirculating System. Crit. Care 2012, 16, R20. [Google Scholar] [CrossRef]
- Nusshag, C.; Morath, C.; Speer, C.; Kaelble, F.; Zeier, M.; Boxberger, M.; Schulze-Schleithoff, E.; Fiedler, M.O.; Weigand, M.A.; Merle, U. Plasma Exchange in Patients with Severe Coronavirus Disease 2019: A Single-Center Experience. Crit. Care Explor. 2021, 3, e0517. [Google Scholar] [CrossRef]

| CytoSorb | MARS | TPE | p Value | |
|---|---|---|---|---|
| Patients [n] | 21 | 14 | 18 | |
| Total treatments [n] | 60 | 61 | 80 | |
| Age [years] | 54.0 (46.0–65.5) | 58.5 (45.0–63.5) | 58.5 (41.5–68.8) | 0.955 |
| Gender [male/female; %] | 71.0/29.0 | 64.3/35.7 | 61.1/38.9 | 0.313 |
| SOFA Score prior to first treatment | 15.0 (9.0–16.5) | 14.0 (11.0–17.3) | 11.0 (5.0–17.0) | 0.368 |
| MELD Score prior to first treatment | 34.0 (33.0–36.5) | 34.0 (29.0–36.0) | 29.0 (22.8–33.5) | 0.005 |
| Vasopressors prior to first treatment [n, (%)] | 12 (57) | 12 (86) | 10 (56) | 0.145 |
| Systolic blood pressure prior to treatment [mmHg] | 120.0 (101.5–140.5) | 117.0 (104.8–134.3) | 108.5 (96.3–135.5) | 0.227 |
| Acute liver failure [n, (%)] | 9 (42.9%) | 6 (42.9%) | 8 (44.4%) | 0.994 |
| Liver parameter maximum | ||||
| Total bilirubin [mg/dL] | 25.5 (19.8–36.6) | 17.8 (13.1–21.3) | 19.1 (10.9–23.7) | 0.011 |
| AST [U/L] | 727.0 (184.5–4729.0) | 5228.0 (1492.0–10,916.0) | 615.0 (241.0–5548.0) | 0.032 |
| ALT [U/L] | 269.0 (91.0–1424.0) | 3288.0 (467.0–4715.0) | 430.0 (204.3–3413.0) | 0.038 |
| AP [U/L] | 257.5 (168.0–408.3) | 333.5 (245.3–658.0) | 297.5 (156.0–502.5) | 0.408 |
| GGT [U/L] | 153.0 (78.5–355.5) | 150.0 (102.0–670.3) | 132.0 (82.0–373.5) | 0.816 |
| INR | 1.96 (1.48–3.38) | 2.97 (2.06–3.57) | 2.08 (1.45–2.82) | 0.094 |
| Etiology of liver dysfunction | ||||
| Septic shock [n, (%)] | 10 (48) | 7 (50) | 8 (44) | 0.951 |
| Pulmonary focus | 2 (20) | 2 (29) | 2 (25) | 0.918 |
| Abdominal focus | 5 (50) | 5 (71) | 6 (75) | 0.487 |
| Urogenital focus | 1 (10) | 0 (0) | 0 (0) | 0.458 |
| Unknown focus | 2 (20) | 0 (0) | 0 (0) | 0.196 |
| Hypoxic liver injury [n, (%)] | 6 (29) | 3 (21) | 2 (11) | 0.608 |
| Cardiogenic shock | 3 (50) | 1 (33) | 0 (0) | 0.441 |
| Hemorrhagic shock | 3 (50) | 0 (0) | 1 (50) | 0.308 |
| Vascular occlusion | 0 (0) | 2 (66) | 1 (50) | 0.087 |
| Liver transplant failure [n, (%)] | 0 (0) | 0 (0) | 4 (22) | 0.015 |
| Hemihepatectomy [n, (%)] | 2 (10) | 4 (29) | 1 (6) | 0.132 |
| Toxic [n, (%)] | 1 (5) | 0 (0) | 0 (0) | 0.460 |
| Autoimmune hepatitis [n, (%)] | 0 (0) | 0 (0) | 2 (11) | 0.133 |
| Cryptogenic [n, (%)] | 2 (1) | 0 (0) | 1 (6) | 0.490 |
| Laboratory parameters prior to first treatment | ||||
| Total bilirubin [mg/dL] | 22.2 (18.3–29.3) | 14.2 (8.6–17.9) | 15.3 (10.8–20.0) | 0.002 |
| Lactate [mg/dL] | 19.0 (12.6–31.9) | 32.1 (23.6–48.7) | 28.4 (23.9–39.0) | 0.072 |
| LDH [U/L] | 424.5 (272.3–739.5) | 447.0 (269.0–1005.0) | 407.0 (308.0–666.5) | 0.947 |
| P-Amylase [U/L] | 20.0 (12.0–75.0) | 38.5 (24.8–149.8) | 35.0 (12.5–96.0) | 0.316 |
| Lipase [U/L] | 42.5 (20.3–77.0) | 82.5 (25.5–200.3) | 35.0 (26.5–140.3) | 0.470 |
| AST [U/L] | 113.5 (75.8–506.3) | 231.5 (105.0–758.3) | 235.0 (99.0–1113.0) | 0.406 |
| ALT [U/L] | 120.0 (69.0–277.0) | 163.0 (53.5–709.8) | 202.0 (74.5–1056.0) | 0.551 |
| AP [U/L] | 188.0 (135.0–292.0) | 193.5 (89.3–356.5) | 226.0 (130.5–370.5) | 0.816 |
| GGT [U/L] | 93.5 (54.0–208.5) | 127.5 (62.8–451.8) | 83.0 (49.0–234.5) | 0.660 |
| CRP [mg/L] | 69.6 (42.7–123.3) | 52.4 (40.0–94.6) | 29.9 (9.3–127.0) | 0.464 |
| SCr [mg/dL] | 1.4 (0.7–2.8) | 1.6 (1.1–2.3) | 1.0 (0.6–1.7) | 0.101 |
| Urea [mg/dL] | 63.0 (44.0–175.5) | 69.0 (50.3–90.8) | 51.5 (25.8–80.0) | 0.169 |
| Platelets [/nL] | 52.5 (39.5–115.5) | 62.5 (47.5–137.8) | 74.0 (34.5–135.5) | 0.693 |
| Albumin [g/L] | 28.4 (24.2–35.1) | 30.6 (28.2–32.5) | 29.6 (24.8–31.4) | 0.498 |
| INR | 1.3 (1.2–1.7) | 1.6 (1.3–1.8) | 1.4 (1.2–2.2) | 0.359 |
| PTT [s] | 32.8 (29.8–44.3) | 34.4 (27.6–43.0) | 30.8 (26.8–39.5) | 0.596 |
| Associated outcomes | ||||
| Length of ICU stay [days] | 21.0 (13.0–49.0) | 25.0 (12.3–34.5) | 21.0 (12.0–32.0) | 0.840 |
| Mortality in ICU [n, (%)] | 16 (76.2) | 9 (64.3) | 8 (44.4) | 0.128 |
| RRT requirement [n, (%)] | 15 (71) | 12 (86) | 8 (44) | 0.040 |
| Treatment Parameter | CytoSorb | MARS | TPE | p Value |
|---|---|---|---|---|
| Duration of treatment [hours] | 12.0 (8.4–17.0) | 14.5 (8.0–19.0) | 2.2 (1.8–2.3) | <0.001 |
| Blood pump flow rate [mL/min] | 200.0 (160.0–200.0) | 150.0 (150.0–150.0) | 47.0 (43.0–50.0) | <0.001 |
| Albumin flow rate [mL/min] | - | 150.0 (150.0–150.0) | - | |
| Centrifuge plasma flow rate [mL/min] | - | - | 31.0 (30.0–32.0) | |
| Exchanged plasma volume [L] | - | - | 3.6 (3.6–3.9) | |
| Anticoagulation with heparin [n] | 60 (100%) | 25 (41%) | 0 (0%) | <0.001 |
| Anticoagulation with argatroban [n] | 0 (0%) | 27 (44%) | 0 (0%) | <0.001 |
| Anticoagulation with citrate [n] | 0 (0%) | 0 (0%) | 80 (100%) | <0.001 |
| No anticoagulation [n] | 0 (0%) | 9 (15%) | 0 (0%) | <0.001 |
| PTT during treatment | 64.0 (37.2–113.2) | 47.3 (39.8–54.7) | 27.7 (24.4–30.1) | <0.001 |
| INR during treatment | 1.3 (1.2–1.8) | 1.8 (1.4–2.1) | 1.3 (1.2–1.4) | <0.001 |
| Treatments per patient [n] | 2.0 (1.0–4.5) | 2.5 (1.0–5.0) | 3.0 (1.0–6.5) | 0.353 |
| Combination with RRT [n] | 43 (71%) | 61 (100%) | 0 (0%) | <0.001 |
| Time from ICU admission to first treatment [days] | 12.0 (5.5–37.0) | 6.5 (2.0–16.3) | 7.0 (2.0–13.0) | 0.132 |
| Parameters | CytoSorb | MARS | TPE | p Value |
|---|---|---|---|---|
| Clotting [n] | 13 (21%) | 16 (26%) | 2 (3%) | <0.001 |
| Hypotension [n] | 2 (1.8%) | 2 (3%) | 1 (1%) | 0.657 |
| Hypocalcemia [n] | 0 (0%) | 0 (0%) | 10 (13%) | 0.001 |
| Hypokalemia [n] | 0 (0%) | 0 (0%) | 16 (20%) | 0.001 |
| Bleeding [n] | 0 (0%) | 0 (0%) | 0 (0%) | |
| Transfusion reaction | - | - | 0 (0%) | |
| Platelet reduction | ||||
| Absolute changes [/nL] | −17.0 (−33.0–−7.0) | −10.5 (31.0–+2.5) | −7.0 (−19.0–+1.0) | 0.071 |
| Relative changes [%] | −26.5 (−41.2–−6.8) | −18.4 (−35.5–+7.6) | −8.0 (−25.0–+1.6) | 0.024 |
| INR changes | ||||
| Absolute changes | +0.1 (0–+0.5) | +0.03 (−0.3–+0.2) | −0.02 (−0.1–0) | 0.241 |
| Relative changes [%] | +5.5 (+0.7–+31.6) | +9.1 (−7.5–+39.6) | −1.6 (−5.0–+1.6) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Göth, D.; Mahler, C.F.; Kälble, F.; Speer, C.; Benning, L.; Schmitt, F.C.F.; Dietrich, M.; Krautkrämer, E.; Zeier, M.; Merle, U.; et al. Liver-Support Therapies in Critical Illness—A Comparative Analysis of Procedural Characteristics and Safety. J. Clin. Med. 2023, 12, 4669. https://doi.org/10.3390/jcm12144669
Göth D, Mahler CF, Kälble F, Speer C, Benning L, Schmitt FCF, Dietrich M, Krautkrämer E, Zeier M, Merle U, et al. Liver-Support Therapies in Critical Illness—A Comparative Analysis of Procedural Characteristics and Safety. Journal of Clinical Medicine. 2023; 12(14):4669. https://doi.org/10.3390/jcm12144669
Chicago/Turabian StyleGöth, Daniel, Christoph F. Mahler, Florian Kälble, Claudius Speer, Louise Benning, Felix C. F. Schmitt, Maximilian Dietrich, Ellen Krautkrämer, Martin Zeier, Uta Merle, and et al. 2023. "Liver-Support Therapies in Critical Illness—A Comparative Analysis of Procedural Characteristics and Safety" Journal of Clinical Medicine 12, no. 14: 4669. https://doi.org/10.3390/jcm12144669
APA StyleGöth, D., Mahler, C. F., Kälble, F., Speer, C., Benning, L., Schmitt, F. C. F., Dietrich, M., Krautkrämer, E., Zeier, M., Merle, U., Morath, C., Fiedler, M. O., Weigand, M. A., & Nusshag, C. (2023). Liver-Support Therapies in Critical Illness—A Comparative Analysis of Procedural Characteristics and Safety. Journal of Clinical Medicine, 12(14), 4669. https://doi.org/10.3390/jcm12144669










