Trends and Hospital Outcomes in HOSPITAL Admissions for Anaphylaxis in Children with and without Asthma in Spain (2016–2021)
Abstract
:1. Introduction
2. Materials and Methods
2.1. Statistical Analysis
2.2. Ethical Statement
3. Results
3.1. Temporal Trends in Hospital Admissions with Anaphylaxis in the Spanish Pediatric Population between 2016 and 2021
3.2. Temporal Trends and Characteristics of Hospital Admissions with Anaphylaxis in the Spanish Pediatric Population Based on the Presence of Asthma
3.3. Incidence of Hospital Admission Due to Anaphylactic Reaction According to the Presence of Asthma and Characteristics of Admission According to Age and Sex
3.4. Multivariable Analysis of Factors Associated with Severe Anaphylaxis during Hospital Admission with Anaphylaxis in the Pediatric Population with and without Asthma
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sampson, H.A.; Muñoz-Furlong, A.; Campbell, R.L.; Adkinson, N.F.; Bock, S.A.; Branum, A.; Brown, S.G.; Camargo, C.A.; Cydulka, R.; Galli, S.J.; et al. Second Symposium on the Definition and Management of Anaphylaxis: Summary Report—Second National Institute of Allergy and Infectious Disease/Food Allergy and Anaphylaxis Network Symposium. Ann. Emerg. Med. 2006, 47, 373–380. [Google Scholar] [CrossRef] [PubMed]
- Jares, E.J.; Cardona, V.; Gómez, R.M.; Bernstein, J.A.; Filho, N.A.R.; Cherrez-Ojeda, I.; Ensina, L.F.; De Falco, A.; Díaz, M.C.; Vereau, P.A.C.; et al. Latin American anaphylaxis registry. World Allergy Organ. J. 2023, 16, 100748. [Google Scholar] [CrossRef] [PubMed]
- Yao, T.-C.; Wu, A.C.; Huang, Y.-W.; Wang, J.-Y.; Tsai, H.-J. Increasing trends of anaphylaxis-related events: An analysis of anaphylaxis using nationwide data in Taiwan, 2001–2013. World Allergy Organ. J. 2018, 11, 23. [Google Scholar] [CrossRef]
- Lin, R.Y.; Anderson, A.S.; Shah, S.N.; Nurruzzaman, F. Increasing anaphylaxis hospitalizations in the first 2 decades of life: New York State, 1990–2006. Ann. Allergy Asthma Immunol. 2008, 101, 387–393. [Google Scholar] [CrossRef] [PubMed]
- Gurkha, D.; Podolsky, R.; Sethuraman, U.; Levasseur, K. Comparison of anaphylaxis epidemiology between urban and suburban pediatric emergency departments. BMC Pediatr. 2023, 23, 85. [Google Scholar] [CrossRef] [PubMed]
- Muraro, A.; Worm, M.; Alviani, C.; Cardona, V.; DunnGalvin, A.; Garvey, L.H.; Riggioni, C.; de Silva, D.; Angier, E.; Arasi, S.; et al. EAACI guidelines: Anaphylaxis (2021 update). Allergy 2022, 77, 357–377. [Google Scholar] [CrossRef]
- Wood, R.A.; Camargo, C.A.; Lieberman, P.; Sampson, H.A.; Schwartz, L.B.; Zitt, M.; Collins, C.; Tringale, M.; Wilkinson, M.; Boyle, J.; et al. Anaphylaxis in America: The prevalence and characteristics of anaphylaxis in the United States. J. Allergy Clin. Immunol. 2014, 133, 461–467. [Google Scholar] [CrossRef]
- Gaspar, Â.; Santos, N.; Faria, E.; Pereira, A.M.; Gomes, E.; Câmara, R.; Rodrigues-Alves, R.; Borrego, L.; Carrapatoso, I.; Carneiro-Leão, L.; et al. Anaphylaxis in children and adolescents: The Portuguese Anaphylaxis Registry. Pediatr. Allergy Immunol. 2021, 32, 1278–1286. [Google Scholar] [CrossRef]
- Anagnostou, K. Anaphylaxis in Children: Epidemiology, Risk Factors and Management. Curr. Pediatr. Rev. 2018, 14, 180–186. [Google Scholar] [CrossRef]
- Vetander, M.; Helander, D.; Flodström, C.; Östblom, E.; Alfvén, T.; Ly, D.H.; Hedlin, G.; Lilja, G.; Nilsson, C.; Wickman, M. Anaphylaxis and reactions to foods in children—A population-based case study of emergency department visits. Clin. Exp. Allergy 2012, 42, 568–577. [Google Scholar] [CrossRef]
- Jiang, N.; Xu, W.; Huang, H.; Hou, X.; Xiang, L. Anaphylaxis in Chinese Children: Different Clinical Profile Between Children with and without a History of Asthma/Recurrent Wheezing. J. Asthma Allergy 2022, 15, 1093–1104. [Google Scholar] [CrossRef] [PubMed]
- Campbell, R.L.; Li, J.T.; Nicklas, R.A.; Sadosty, A.T.; Members of the Joint Task Force; Practice Parameter Workgroup. Emergency department diagnosis and treatment of anaphylaxis: A practice parameter. Ann. Allergy Asthma Immunol. 2014, 113, 599–608. [Google Scholar] [CrossRef] [PubMed]
- Dribin, T.E.; Michelson, K.A.; Zhang, Y.; Schnadower, D.; Neuman, M.I. Are Children with a History of Asthma More Likely to Have Severe Anaphylactic Reactions? A Retrospective Cohort Study. J. Pediatr. 2020, 220, 159–164.e2. [Google Scholar] [CrossRef] [PubMed]
- Tejedor-Alonso, M.A.; Moro-Moro, M.; González, M.M.; Rodriguez-Alvarez, M.; Fernández, E.P.; Zamalloa, P.L.; Aquino, E.F.; Gil Prieto, R.; Gil De Miguel, A. Increased incidence of admissions for anaphylaxis in Spain 1998–2011. Allergy 2015, 70, 880–883. [Google Scholar] [CrossRef]
- Nieto-Nieto, A.; Tejedor-Alonso, M.; Farias-Aquino, E.; Moro-Moro, M.; Ingelmo, A.R.; Gonzalez-Moreno, A.; Gil de Miguel, A. Clinical profile of patients with severe anaphylaxis hospitalized in the spanish hospital system: 1997–2011. J. Investig. Allergol. Clin. Immunol. 2017, 27, 111–126. [Google Scholar] [CrossRef]
- Ministerio de Sanidad, Servicios Sociales e Igualdad. Real Decreto 69/2015, de 6 de Febrero, por el Que Se Regula el Registro de Actividad de Atención Sanitaria Especializada. (Spanish National Hospital Discharge Database). BOE 2015, 35, 10789–10809. Available online: https://www.mscbs.gob.es/estadEstudios/estadisticas/docs/BOE_RD_69_2015_RAE_CMBD.pdf (accessed on 19 January 2023).
- Ministerio de Sanidad. National Health Survey in Spain 2020 [Encuesta Nacional de Salud de España 2017]. Available online: https://www.sanidad.gob.es/estadEstudios/estadisticas/encuestaNacional/encuesta2017.htm (accessed on 28 July 2023).
- Ministerio de Sanidad, Consumo y Bienestar Social, Solicitud de Extracción de Datos—Extraction Request. (Spanish National Hospital Discharge Database). Available online: https://www.mscbs.gob.es/estadEstudios/estadisticas/estadisticas/estMinisterio/SolicitudCMBDdocs/2018_Formulario_Peticion_Datos_RAE_CMBD.pdf (accessed on 28 July 2023).
- Robinson, L.B.; Arroyo, A.C.; Faridi, M.K.; Rudders, S.A.; Camargo, C.A., Jr. Trends in US hospitalizations for anaphylaxis among infants and toddlers: 2006 to 2015. Ann. Allergy Asthma Immunol. 2021, 126, 168–174.e3. [Google Scholar] [CrossRef]
- Shrestha, P.; Dhital, R.; Poudel, D.; Donato, A.; Karmacharya, P.; Craig, T. Trends in hospitalizations related to anaphylaxis, angioedema, and urticaria in the United States. Ann. Allergy Asthma Immunol. 2019, 122, 401–406.e2. [Google Scholar] [CrossRef]
- Motosue, M.S.; Bellolio, M.F.; Van Houten, H.K.; Shah, N.D.; Campbell, R.L. National trends in emergency department visits and hospitalizations for food-induced anaphylaxis in US children. Pediatr. Allergy Immunol. 2018, 29, 538–544. [Google Scholar] [CrossRef]
- Dyer, A.A.; Lau, C.H.; Smith, T.L.; Smith, B.M.; Gupta, R.S. Pediatric emergency department visits and hospitalizations due to food-induced anaphylaxis in Illinois. Ann. Allergy Asthma Immunol. 2015, 115, 56–62. [Google Scholar] [CrossRef]
- Conrado, A.B.; Ierodiakonou, D.; Gowland, M.H.; Boyle, R.J.; Turner, P.J. Food anaphylaxis in the United Kingdom: Analysis of national data, 1998-2018. BMJ 2021, 372, n251. [Google Scholar] [CrossRef]
- Turner, P.J.; Campbell, D.E.; Motosue, M.S.; Campbell, R.L. Global Trends in Anaphylaxis Epidemiology and Clinical Implications. J. Allergy Clin. Immunol. Pract. 2020, 8, 1169–1176. [Google Scholar] [CrossRef]
- Gaffney, L.K.; Porter, J.; Gerling, M.; Schneider, L.C.; Stack, A.M.; Shah, D.; Michelson, K.A. Safely Reducing Hospitalizations for Anaphylaxis in Children Through an Evidence-Based Guideline. Pediatrics. 2022, 149, e2020045831. [Google Scholar] [CrossRef] [PubMed]
- Dribin, T.E.; Neuman, M.I.; Schnadower, D.; Sampson, H.A.; Porter, J.J.; Michelson, K.A. Trends and Variation in Pediatric Anaphylaxis Care From 2016 to 2022. J. Allergy Clin. Immunol. Pract. 2023, 11, 1184–1189. [Google Scholar] [CrossRef] [PubMed]
- Al Ali, A.; Gabrielli, S.; Colli, L.D.; Colli, M.D.; McCusker, C.; Clarke, A.E.; Morris, J.; Gravel, J.; Lim, R.; Chan, E.S.; et al. Temporal trends in anaphylaxis ED visits over the last decade and the effect of COVID-19 pandemic on these trends. Expert Rev. Clin. Immunol. 2023, 19, 341–348. [Google Scholar] [CrossRef] [PubMed]
- Abunada, T.; Al-Nesf, M.A.; Thalib, L.; Kurdi, R.; Khalil, S.; ElKassem, W.; Mobayed, H.M.; Zayed, H. Anaphylaxis triggers in a large tertiary care hospital in Qatar: A retrospective study. World Allergy Organ. J. 2018, 11, 20. [Google Scholar] [CrossRef] [PubMed]
- Okubo, Y.; Nochioka, K.; Testa, M.A. Nationwide Survey of Hospitalization Due to Pediatric Food-Induced Anaphylaxis in the United States. Pediatr. Emerg. Care 2019, 35, 769–773. [Google Scholar] [CrossRef]
- Dinakar, C. Anaphylaxis in Children: Current Understanding and Key Issues in Diagnosis and Treatment. Curr. Allergy Asthma Rep. 2012, 12, 641–649. [Google Scholar] [CrossRef]
- Ramsey, N.B.; Guffey, D.; Anagnostou, K.; Coleman, N.E.; Davis, C.M. Epidemiology of Anaphylaxis in Critically Ill Children in the United States and Canada. J. Allergy Clin. Immunol. Pract. 2019, 7, 2241–2249. [Google Scholar] [CrossRef]
- Krmpotic, K.; Weisser, C.; O’Hanley, A.; Soder, C. Incidence and Outcomes of Severe Anaphylaxis in Paediatric Patients in Atlantic Canada. J. Pediatr. Intensive Care 2019, 8, 113–116. [Google Scholar] [CrossRef]
- Sundquist, B.K.; Jose, J.; Pauze, D.; Pauze, D.; Wang, H.; Järvinen, K.M. Anaphylaxis risk factors for hospitalization and intensive care: A comparison between adults and children in an upstate New York emergency department. Allergy Asthma Proc. 2019, 40, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Turner, P.J.; Gowland, M.H.; Sharma, V.; Ierodiakonou, D.; Harper, N.; Garcez, T.; Pumphrey, R.; Boyle, R.J. Increase in anaphylaxis-related hospitalizations but no increase in fatalities: An analysis of United Kingdom national anaphylaxis data, 1992–2012. J. Allergy Clin. Immunol. 2015, 135, 956–963.e1. [Google Scholar] [CrossRef] [PubMed]
- Ma, L.; Danoff, T.M.; Borish, L. Case fatality and population mortality associated with anaphylaxis in the United States. J. Allergy Clin. Immunol. 2014, 133, 1075–1083. [Google Scholar] [CrossRef] [PubMed]
- Mullins, R.J.; Wainstein, B.K.; Barnes, E.H.; Liew, W.K.; Campbell, D.E. Increases in anaphylaxis fatalities in Australia from 1997 to 2013. Clin. Exp. Allergy 2016, 46, 1099–1110. [Google Scholar] [CrossRef] [PubMed]
- González-Pérez, A.; Aponte, Z.; Vidaurre, C.F.; Rodríguez, L.A.G. Anaphylaxis epidemiology in patients with and patients without asthma: A United Kingdom database review. J. Allergy Clin. Immunol. 2010, 125, 1098–1104.e1. [Google Scholar] [CrossRef] [PubMed]
- Simons, F.E.R.; Ardusso, L.R.; Bilò, M.B.; El-Gamal, Y.M.; Ledford, D.K.; Ring, J.; Sanchez-Borges, M.; Senna, G.E.; Sheikh, A.; Thong, B.Y.; et al. World Allergy Organization Guidelines for the Assessment and Management of Anaphylaxis. World Allergy Organ. J. 2011, 4, 13–37. [Google Scholar] [CrossRef]
- Muraro, A.; Roberts, G.; Worm, M.; Bilò, M.B.; Brockow, K.; Fernández Rivas, M.; Santos, A.F.; Zolkipli, Z.Q.; Bellou, A.; Beyer, K.; et al. Anaphylaxis: Guidelines from the European Academy of Allergy and Clinical Immunology. Allergy 2014, 69, 1026–1045. [Google Scholar] [CrossRef]
- Simons, F.E.R.; Ardusso, L.R.; Bilò, M.B.; Cardona, V.; Ebisawa, M.; El-Gamal, Y.M.; Lieberman, P.; Lockey, R.F.; Muraro, A.; Roberts, G.; et al. International consensus on (ICON) anaphylaxis. World Allergy Organ. J. 2014, 7, 9. [Google Scholar] [CrossRef]
- Greenhawt, M.; Gupta, R.S.; Meadows, J.A.; Pistiner, M.; Spergel, J.M.; Camargo, C.A.; Simons, F.E.R.; Lieberman, P.L. Guiding Principles for the Recognition, Diagnosis, and Management of Infants with Anaphylaxis: An Expert Panel Consensus. J. Allergy Clin. Immunol. Pract. 2019, 7, 1148–1156.e5. [Google Scholar] [CrossRef]
- Clark, S.; Wei, W.; Rudders, S.A.; Camargo, C.A., Jr. Risk factors for severe anaphylaxis in patients receiving anaphylaxis treatment in US emergency departments and hospitals. J. Allergy Clin. Immunol. 2014, 134, 1125–1130. [Google Scholar] [CrossRef]
- Motosue, M.S.; Bellolio, M.F.; Van Houten, H.K.; Shah, N.D.; Campbell, R.L. Risk factors for severe anaphylaxis in the United States. Ann. Allergy Asthma Immunol. 2017, 119, 356–361.e2. [Google Scholar] [CrossRef] [PubMed]
- Bock, S.A.; Muñoz-Furlong, A.; Sampson, H.A. Further fatalities caused by anaphylactic reactions to food, 2001–2006. J. Allergy Clin. Immunol. 2007, 119, 1016–1018. [Google Scholar] [CrossRef]
- Bock, S.; Muñoz-Furlong, A.; Sampson, H.A. Fatalities due to anaphylactic reactions to foods. J. Allergy Clin. Immunol. 2001, 107, 191–193. [Google Scholar] [CrossRef] [PubMed]
- Summers, C.W.; Pumphrey, R.S.; Woods, C.N.; McDowell, G.; Pemberton, P.W.; Arkwright, P.D. Factors predicting anaphylaxis to peanuts and tree nuts in patients referred to a specialist center. J. Allergy Clin. Immunol. 2008, 121, 632–638.e2. [Google Scholar] [CrossRef] [PubMed]
- Lieberman, P. The Risk and Management of Anaphylaxis in the Setting of Immunotherapy. Am. J. Rhinol. Allergy 2012, 26, 469–474. [Google Scholar] [CrossRef]
| 2016 | 2017 | 2018 | 2019 | 2020 | 2021 | Total | p Trend | |
|---|---|---|---|---|---|---|---|---|
| N | 431 | 421 | 439 | 432 | 346 | 504 | 2573 | NA |
| Age, mean (SD) | 6.9 (4.82) | 7 (4.86) | 6.35 (4.77) | 6.94 (4.95) | 6.78 (5.15) | 6.68 (4.99) | 6.77 (4.92) | 0.396 |
| 0–5 years old, n (%) | 189 (43.85) | 189 (44.89) | 214 (48.75) | 189 (43.75) | 159 (45.95) | 238 (47.22) | 1178 (45.78) | 0.558 |
| 6–11 years old, n (%) | 153 (35.5) | 130 (30.88) | 145 (33.03) | 149 (34.49) | 107 (30.92) | 165 (32.74) | 849 (33) | |
| 12–17 years old, n (%) | 89 (20.65) | 102 (24.23) | 80 (18.22) | 94 (21.76) | 80 (23.12) | 101 (20.04) | 546 (21.22) | |
| Boys, n (%) | 280 (64.97) | 245 (58.19) | 255 (58.09) | 250 (57.87) | 225 (65.03) | 305 (60.52) | 1560 (60.63) | 0.081 |
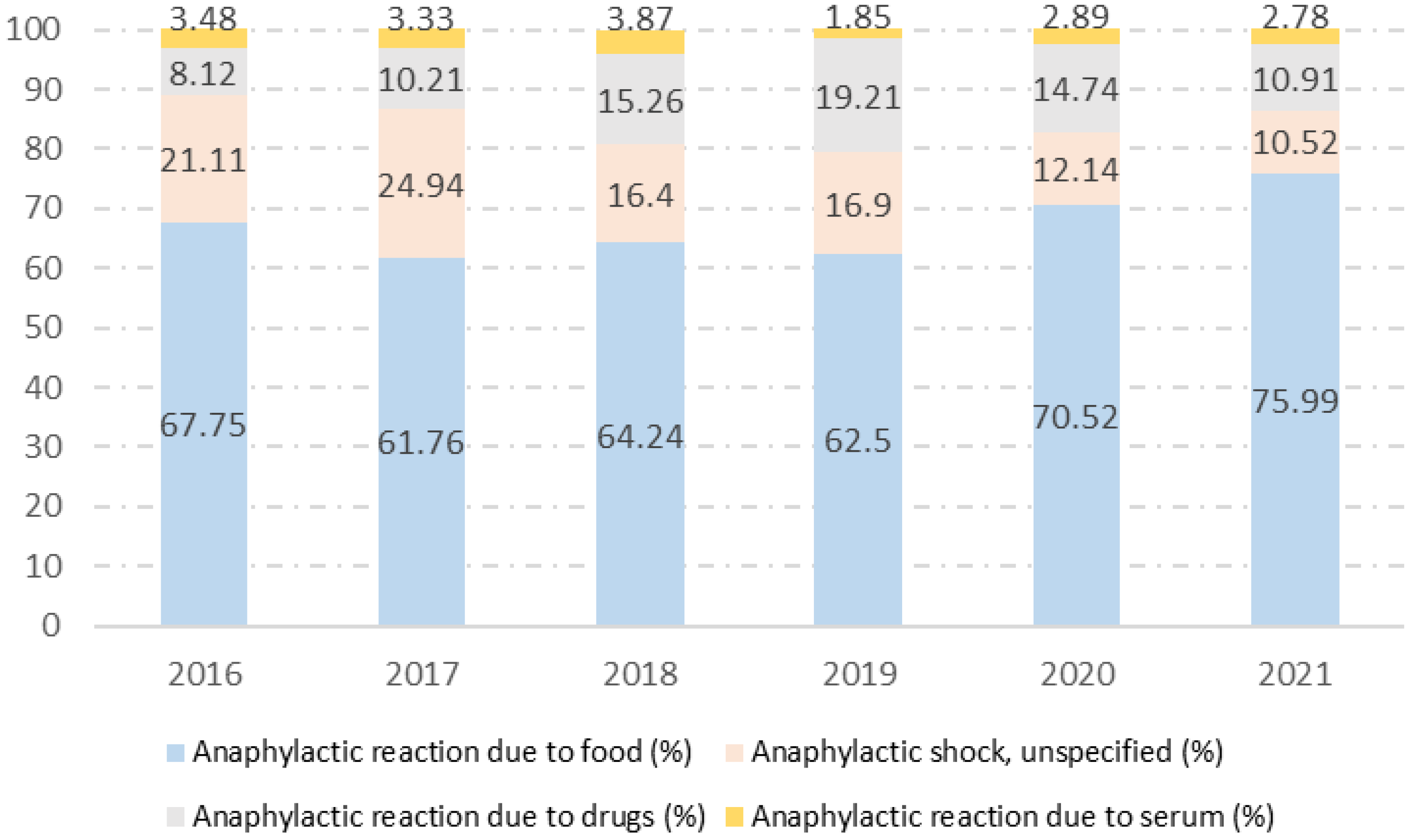
| Anaphylactic reaction due to food, n (%) | 292 (67.75) | 260 (61.76) | 282 (64.24) | 270 (62.5) | 244 (70.52) | 383 (75.99) | 1731 (67.28) | <0.001 |
| Anaphylactic reaction due to serum, n (%) | 15 (3.48) | 14 (3.33) | 17 (3.87) | 8 (1.85) | 10 (2.89) | 14 (2.78) | 78 (3.03) | 0.600 |
| Anaphylactic reaction due to drugs, n (%) | 35 (8.12) | 43 (10.21) | 67 (15.26) | 83 (19.21) | 51 (14.74) | 55 (10.91) | 334 (12.98) | <0.001 |
| Anaphylactic shock, unspecified, n (%) | 91 (21.11) | 105 (24.94) | 72 (16.4) | 73 (16.9) | 42 (12.14) | 53 (10.52) | 436 (16.95) | <0.001 |
| Invasive mechanical ventilation, n (%) | 11 (2.55) | 8 (1.9) | 12 (2.73) | 17 (3.94) | 9 (2.6) | 12 (2.38) | 69 (2.68) | 0.578 |
| Noninvasive mechanical ventilation, n (%) | 2 (0.46) | 4 (0.95) | 1 (0.23) | 8 (1.85) | 8 (2.31) | 11 (2.18) | 34 (1.32) | 0.021 |
| Admission to ICU, n (%) | 29 (6.73) | 55 (13.06) | 49 (11.16) | 59 (13.66) | 44 (12.72) | 36 (7.14) | 272 (10.57) | 0.001 |
| IHM, n (%) | 4 (0.93) | 2 (0.48) | 4 (0.91) | 3 (0.69) | 2 (0.58) | 2 (0.4) | 17 (0.66) | 0.890 |
| Admission to ICU or IHM, n (%) | 31 (7.19) | 55 (13.06) | 49 (11.16) | 60 (13.89) | 45 (13.01) | 37 (7.34) | 277 (10.77) | 0.001 |
| Asthma | 2016 | 2017 | 2018 | 2019 | 2020 | 2021 | Total | p Trend | p “with Asthma” vs. “without Asthma” | |
|---|---|---|---|---|---|---|---|---|---|---|
| N (%) | Yes | 60 (13.92) | 51 (12.11) | 50 (11.39) | 54 (12.5) | 38 (10.98) | 71 (14.09) | 324 (12.59) | 0.670 | NA |
| No | 371 (86.08) | 370 (87.89) | 389 (88.61) | 378 (87.5) | 308 (89.02) | 433 (85.91) | 2249 (87.41) | |||
| Age, mean (SD) | Yes | 9.97 (4.04) | 9.63 (3.39) | 9.08 (4.45) | 9.63 (3.81) | 10.5 (3.87) | 10.25 (3.5) | 9.85 (3.84) | 0.520 | <0.001 |
| No | 6.41 (4.76) | 6.64 (4.92) | 5.99 (4.7) | 6.55 (4.98) | 6.32 (5.1) | 6.1 (4.95) | 6.33 (4.9) | 0.399 | ||
| 0–5 years old, n (%) | Yes | 10 (16.67) | 6 (11.76) | 13 (26) | 6 (11.11) | 5 (13.16) | 6 (8.45) | 46 (14.2) | 0.194 | <0.001 |
| No | 179 (48.25) | 183 (49.46) | 201 (51.67) | 183 (48.41) | 154 (50) | 232 (53.58) | 1132 (50.33) | 0.496 | ||
| 6–11 years old, n (%) | Yes | 27 (45) | 25 (49.02) | 20 (40) | 31 (57.41) | 15 (39.47) | 42 (59.15) | 160 (49.38) | 0.194 | <0.001 |
| No | 126 (33.96) | 105 (28.38) | 125 (32.13) | 118 (31.22) | 92 (29.87) | 123 (28.41) | 689 (30.64) | 0.496 | ||
| 12–17 years old, n (%) | Yes | 23 (38.33) | 20 (39.22) | 17 (34) | 17 (31.48) | 18 (47.37) | 23 (32.39) | 118 (36.42) | 0.194 | <0.001 |
| No | 66 (17.79) | 82 (22.16) | 63 (16.2) | 77 (20.37) | 62 (20.13) | 78 (18.01) | 428 (19.03) | 0.496 | ||
| Boys, n (%) | Yes | 40 (66.67) | 26 (50.98) | 24 (48) | 35 (64.81) | 25 (65.79) | 38 (53.52) | 188 (58.02) | 0.186 | 0.305 |
| No | 240 (64.69) | 219 (59.19) | 231 (59.38) | 215 (56.88) | 200 (64.94) | 267 (61.66) | 1372 (61) | 0.165 | ||
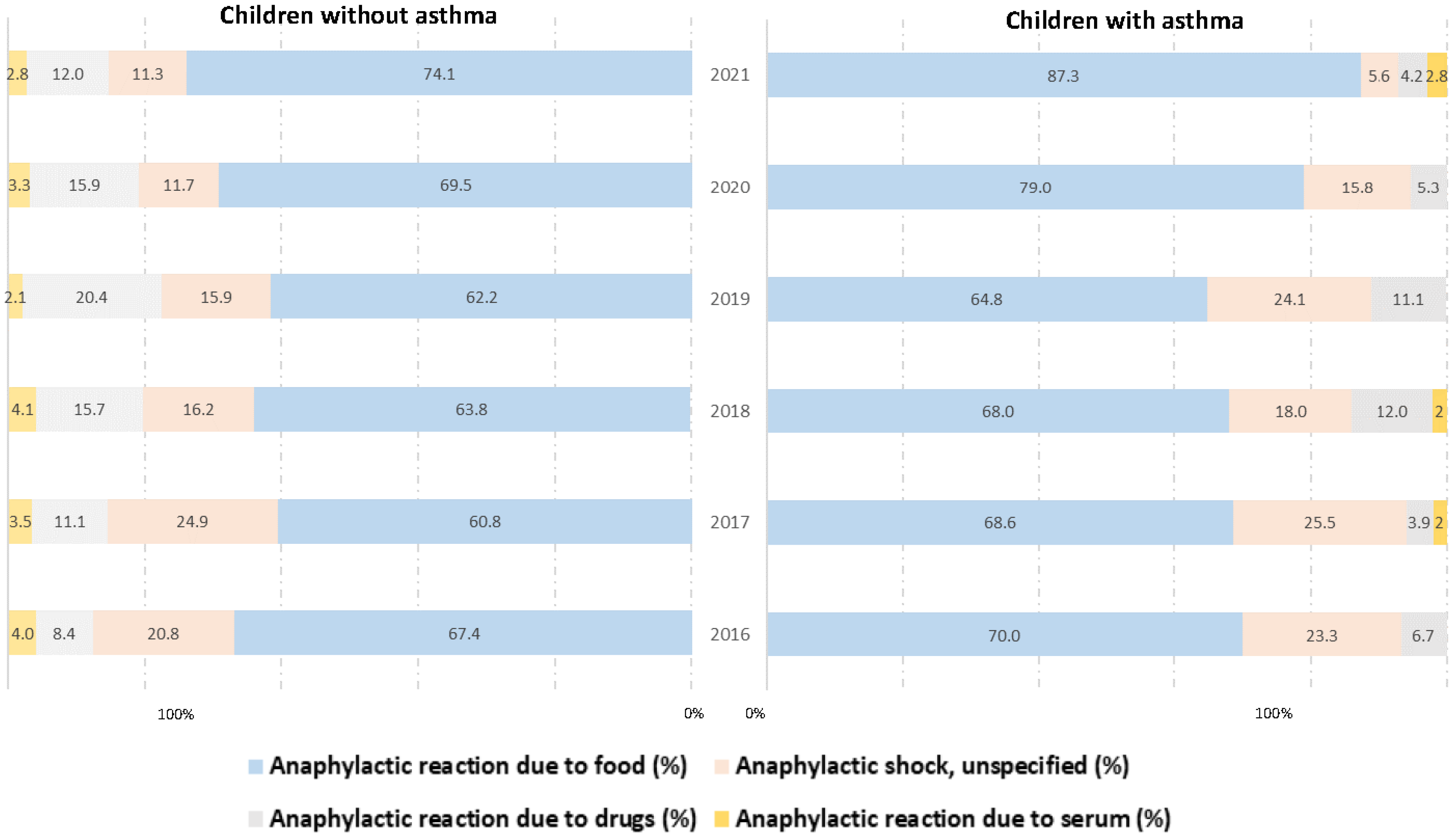
| Anaphylactic reaction due to food, n (%) | Yes | 42 (70) | 35 (68.63) | 34 (68) | 35 (64.81) | 30 (78.95) | 62 (87.32) | 238 (73.46) | 0.044 | 0.011 |
| No | 250 (67.39) | 225 (60.81) | 248 (63.75) | 235 (62.17) | 214 (69.48) | 321 (74.13) | 1493 (66.39) | <0.001 | ||
| Anaphylactic reaction due to serum, n (%) | Yes | 0 (0) | 1 (1.96) | 1 (2) | 0 (0) | 0 (0) | 2 (2.82) | 4 (1.23) | 0.576 | 0.053 |
| No | 15 (4.04) | 13 (3.51) | 16 (4.11) | 8 (2.12) | 10 (3.25) | 12 (2.77) | 74 (3.29) | 0.616 | ||
| Anaphylactic reaction due to drugs, n (%) | Yes | 4 (6.67) | 2 (3.92) | 6 (12) | 6 (11.11) | 2 (5.26) | 3 (4.23) | 23 (7.1) | 0.413 | 0.001 |
| No | 31 (8.36) | 41 (11.08) | 61 (15.68) | 77 (20.37) | 49 (15.91) | 52 (12.01) | 311 (13.83) | <0.001 | ||
| Anaphylactic shock, unspecified, n (%) | Yes | 14 (23.33) | 13 (25.49) | 9 (18) | 13 (24.07) | 6 (15.79) | 4 (5.63) | 59 (18.21) | 0.037 | 0.516 |
| No | 77 (20.75) | 92 (24.86) | 63 (16.2) | 60 (15.87) | 36 (11.69) | 49 (11.32) | 377 (16.76) | <0.001 | ||
| Invasive mechanical ventilation, n (%) | Yes | 2 (3.33) | 2 (3.92) | 0 (0) | 5 (9.26) | 1 (2.63) | 0 (0) | 10 (3.09) | 0.054 | 0.630 |
| No | 9 (2.43) | 6 (1.62) | 12 (3.08) | 12 (3.17) | 8 (2.6) | 12 (2.77) | 59 (2.62) | 0.803 | ||
| Noninvasive mechanical ventilation, n (%) | Yes | 0 (0) | 2 (3.92) | 0 (0) | 2 (3.7) | 2 (5.26) | 0 (0) | 6 (1.85) | 0.152 | 0.374 |
| No | 2 (0.54) | 2 (0.54) | 1 (0.26) | 6 (1.59) | 6 (1.95) | 11 (2.54) | 28 (1.24) | 0.018 | ||
| Admission to ICU, n (%) | Yes | 4 (6.67) | 8 (15.69) | 8 (16) | 10 (18.52) | 5 (13.16) | 6 (8.45) | 41 (12.65) | 0.336 | 0.193 |
| No | 25 (6.74) | 47 (12.7) | 41 (10.54) | 49 (12.96) | 39 (12.66) | 30 (6.93) | 231 (10.27) | 0.004 | ||
| IHM, n (%) | Yes | 1 (1.67) | 0 (0) | 1 (2) | 0 (0) | 0 (0) | 0 (0) | 2 (0.62) | 0.555 | 0.918 |
| No | 3 (0.81) | 2 (0.54) | 3 (0.77) | 3 (0.79) | 2 (0.65) | 2 (0.46) | 15 (0.67) | 0.986 | ||
| Admission to ICU or IHM, n (%) | Yes | 4 (6.67) | 8 (15.69) | 8 (16) | 10 (18.52) | 5 (13.16) | 6 (8.45) | 41 (12.65) | 0.336 | 0.241 |
| No | 27 (7.28) | 47 (12.7) | 41 (10.54) | 50 (13.23) | 40 (12.99) | 31 (7.16) | 236 (10.49) | 0.006 |
| Asthma | 0–5 Years Old | 6–11 Years Old | 12–17 Years Old | p | |
|---|---|---|---|---|---|
| Rate per 100,000 children per year | Yes | 49.72 | 82.56 | 46.10 | <0.001 |
| No | 45.48 | 24.56 | 15.60 | <0.001 | |
| Age, mean (SD) | Yes | 3.67 (1.25) | 8.63 (1.65) | 13.91 (1.63) | <0.001 |
| No | 2.22 (1.79) | 8.3 (1.76) | 14.02 (1.58) | <0.001 | |
| Boys, n (%) | Yes | 30 (65.22) | 97 (60.63) | 61 (51.69) | 0.186 |
| No | 709 (62.63) | 437 (63.43) | 226 (52.8) | 0.001 | |
| Anaphylactic reaction due to food, n (%) | Yes | 39 (84.78) | 119 (74.38) | 80 (67.8) | 0.081 |
| No | 852 (75.27) | 459 (66.62) | 182 (42.52) | <0.001 | |
| Anaphylactic reaction due to serum, n (%) | Yes | 0 (0) | 1 (0.63) | 3 (2.54) | 0.257 |
| No | 38 (3.36) | 19 (2.76) | 17 (3.97) | 0.534 | |
| Anaphylactic reaction due to drugs, n (%) | Yes | 0 (0) | 12 (7.5) | 11 (9.32) | 0.109 |
| No | 104 (9.19) | 97 (14.08) | 110 (25.7) | <0.001 | |
| Anaphylactic shock, unspecified, n (%) | Yes | 7 (15.22) | 28 (17.5) | 24 (20.34) | 0.708 |
| No | 142 (12.54) | 115 (16.69) | 120 (28.04) | <0.001 | |
| Invasive mechanical ventilation, n (%) | Yes | 0 (0) | 5 (3.13) | 5 (4.24) | 0.370 |
| No | 34 (3) | 13 (1.89) | 12 (2.8) | 0.340 | |
| Noninvasive mechanical ventilation, n (%) | Yes | 1 (2.17) | 3 (1.88) | 2 (1.69) | 0.979 |
| No | 16 (1.41) | 6 (0.87) | 6 (1.4) | 0.568 | |
| Admission to ICU, n (%) | Yes | 4 (8.7) | 21 (13.13) | 16 (13.56) | 0.680 |
| No | 105 (9.28) | 61 (8.85) | 65 (15.19) | 0.001 | |
| IHM, n (%) | Yes | 0 (0) | 2 (1.25) | 0 (0) | 0.357 |
| No | 8 (0.71) | 5 (0.73) | 2 (0.47) | 0.852 | |
| Admission to ICU or IHM, n (%) | Yes | 4 (8.7) | 21 (13.13) | 16 (13.56) | 0.680 |
| No | 109 (9.63) | 62 (9) | 65 (15.19) | 0.002 |
| Asthma | Boys | Girls | p | |
|---|---|---|---|---|
| Rate per 100,000 subjects per year | Yes | 60.19 | 59.14 | NA |
| No | 33.37 | 22.33 | NA | |
| Age, mean (SD) | Yes | 9.51 (3.84) | 10.32 (3.8) | 0.060 |
| No | 6.09 (4.74) | 6.7 (5.11) | 0.004 | |
| 0–5 years old, n (%) | Yes | 30 (15.96) | 16 (11.76) | 0.186 |
| No | 709 (51.68) | 423 (48.23) | 0.001 | |
| 6–11 years old, n (%) | Yes | 97 (51.6) | 63 (46.32) | 0.186 |
| No | 437 (31.85) | 252 (28.73) | 0.001 | |
| 12–17 years old, n (%) | Yes | 61 (32.45) | 57 (41.91) | 0.186 |
| No | 226 (16.47) | 202 (23.03) | 0.001 | |
| Anaphylactic reaction due to food, n (%) | Yes | 134 (71.28) | 104 (76.47) | 0.296 |
| No | 938 (68.37) | 555 (63.28) | 0.013 | |
| Anaphylactic reaction due to serum, n (%) | Yes | 4 (2.13) | 0 (0) | 0.087 |
| No | 38 (2.77) | 36 (4.1) | 0.083 | |
| Anaphylactic reaction due to drugs, n (%) | Yes | 13 (6.91) | 10 (7.35) | 0.880 |
| No | 181 (13.19) | 130 (14.82) | 0.274 | |
| Anaphylactic shock, unspecified, n (%) | Yes | 37 (19.68) | 22 (16.18) | 0.420 |
| No | 221 (16.11) | 156 (17.79) | 0.298 | |
| Invasive mechanical ventilation, n (%) | Yes | 5 (2.66) | 5 (3.68) | 0.601 |
| No | 35 (2.55) | 24 (2.74) | 0.788 | |
| Noninvasive mechanical ventilation, n (%) | Yes | 6 (3.19) | 0 (0) | 0.035 |
| No | 16 (1.17) | 12 (1.37) | 0.673 | |
| Admission to ICU, n (%) | Yes | 20 (10.64) | 21 (15.44) | 0.199 |
| No | 138 (10.06) | 93 (10.6) | 0.677 | |
| IHM, n (%) | Yes | 0 (0) | 2 (1.47) | 0.095 |
| No | 8 (0.58) | 7 (0.8) | 0.541 | |
| Admission to ICU or IHM, n (%) | Yes | 20 (10.64) | 21 (15.44) | 0.199 |
| No | 141 (10.28) | 95 (10.83) | 0.675 |
| No Asthma | Asthma | Both | |
|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| 0–5 years old | 1 | 1 | 1 |
| 6–11 years old | 0.97 (0.68–1.38) | 1.48 (0.43–5.16) | 1.03 (0.74–1.43) |
| 12–17 years old | 1.48 (1.02–2.15) | 1.22 (0.34–4.45) | 1.39 (0.98–1.99) |
| Girls | 0.97 (0.72–1.32) | 1.87 (0.87–4.03) | 1.05 (0.8–1.39) |
| Anaphylactic reaction due to drugs | 2.03 (1.33–3.11) | 1.77 (069–3.99) | 1.95 (1.3–2.91) |
| Invasive mechanical ventilation | 17.63 (9.5–32.73) | 27.59 (4.77–159.64) | 17.54 (9.87–31.15) |
| Noninvasive mechanical ventilation | 3.59 (1.34–9.64) | 42.5 (3.76–481.1) | 4.9 (2.07–11.6) |
| 2016 | 1 | 1 | 1 |
| 2017 | 2.17 (1.26–3.74) | 2.2 (0.5–9.56) | 2.25 (1.36–3.74) |
| 2018 | 1.58(0.9–2.77) | 3.64 (0.88–15.06) | 1.79 (1.06–3) |
| 2019 | 1.88 (1.09–3.25) | 2.41 (0.58–10.09) | 1.96 (1.18–3.26) |
| 2020 | 1.97 (1.11–3.48) | 2.26 (0.44–11.63) | 2.03 (1.19–3.47) |
| 2021 | 0.91 (0.5–1.67) | 1.97 (0.45–8.58) | 1.02 (0.58–1.78) |
| Asthma | NA | NA | 1.31 (0.88–1.96) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Miguel-Díez, J.; Lopez-de-Andres, A.; Caballero-Segura, F.J.; Jimenez-Garcia, R.; Hernández-Barrera, V.; Carabantes-Alarcon, D.; Zamorano-Leon, J.J.; Omaña-Palanco, R.; Cuadrado-Corrales, N. Trends and Hospital Outcomes in HOSPITAL Admissions for Anaphylaxis in Children with and without Asthma in Spain (2016–2021). J. Clin. Med. 2023, 12, 6387. https://doi.org/10.3390/jcm12196387
De Miguel-Díez J, Lopez-de-Andres A, Caballero-Segura FJ, Jimenez-Garcia R, Hernández-Barrera V, Carabantes-Alarcon D, Zamorano-Leon JJ, Omaña-Palanco R, Cuadrado-Corrales N. Trends and Hospital Outcomes in HOSPITAL Admissions for Anaphylaxis in Children with and without Asthma in Spain (2016–2021). Journal of Clinical Medicine. 2023; 12(19):6387. https://doi.org/10.3390/jcm12196387
Chicago/Turabian StyleDe Miguel-Díez, Javier, Ana Lopez-de-Andres, Francisco J. Caballero-Segura, Rodrigo Jimenez-Garcia, Valentin Hernández-Barrera, David Carabantes-Alarcon, Jose J. Zamorano-Leon, Ricardo Omaña-Palanco, and Natividad Cuadrado-Corrales. 2023. "Trends and Hospital Outcomes in HOSPITAL Admissions for Anaphylaxis in Children with and without Asthma in Spain (2016–2021)" Journal of Clinical Medicine 12, no. 19: 6387. https://doi.org/10.3390/jcm12196387
APA StyleDe Miguel-Díez, J., Lopez-de-Andres, A., Caballero-Segura, F. J., Jimenez-Garcia, R., Hernández-Barrera, V., Carabantes-Alarcon, D., Zamorano-Leon, J. J., Omaña-Palanco, R., & Cuadrado-Corrales, N. (2023). Trends and Hospital Outcomes in HOSPITAL Admissions for Anaphylaxis in Children with and without Asthma in Spain (2016–2021). Journal of Clinical Medicine, 12(19), 6387. https://doi.org/10.3390/jcm12196387







