Different Types of Vasculitis Complicated by Heparin-Induced Thrombocytopenia—Analysis of Four Cases and Literature Review
Abstract
1. Introduction
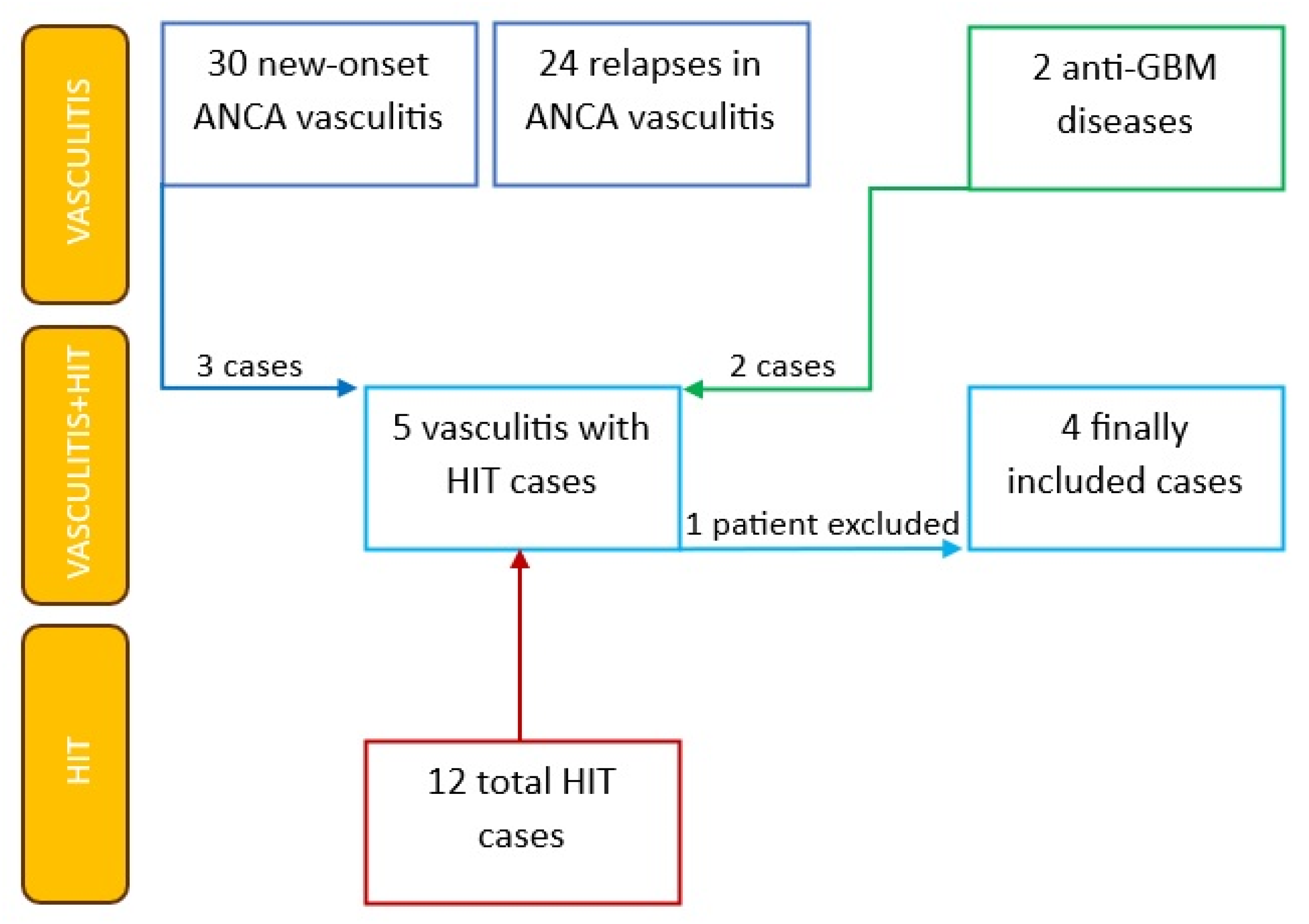
2. Materials and Methods
3. Results
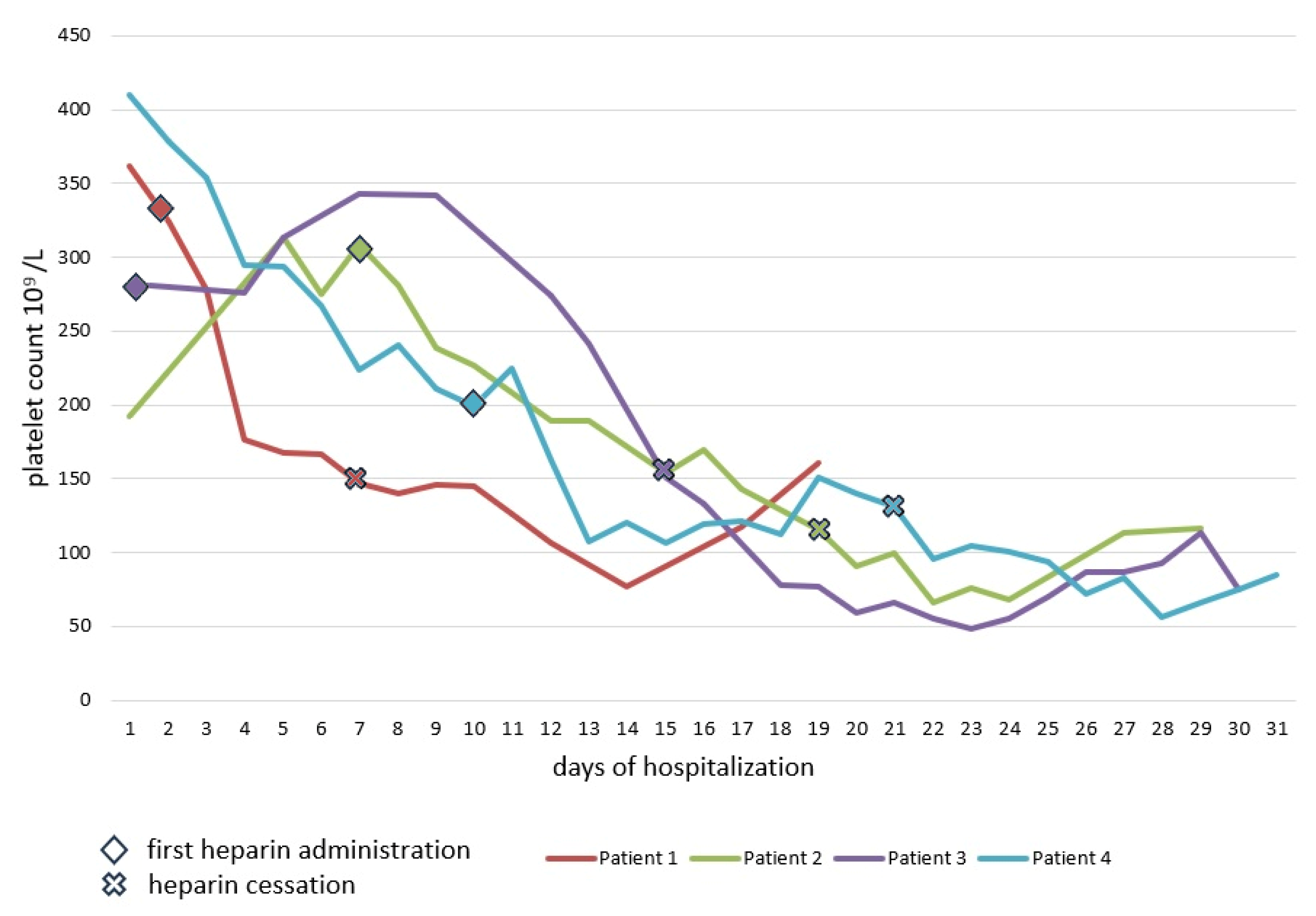
3.1. Case 1
3.2. Case 2
3.3. Case 3
3.4. Case 4
4. Discussion
4.1. Literature Review
4.2. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lee, G.M.; Arepally, G.M. Heparin-induced thrombocytopenia. Hematol. Am. Soc. Hematol. Educ. Program 2013, 2013, 668–674. [Google Scholar] [CrossRef]
- Hogan, M.; Berger, J.S. Heparin-induced thrombocytopenia (HIT): Review of incidence, diagnosis, and management. Vasc. Med. 2020, 25, 160–173. [Google Scholar] [CrossRef]
- Jennette, J.C.; Falk, R.J.; Bacon, P.A.; Basu, N.; Cid, M.C.; Ferrario, F.; Flores-Suarez, L.F.; Gross, W.L.; Guillevin, L.; Hagen, E.C.; et al. 2012 revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum. 2013, 65, 37715. [Google Scholar] [CrossRef] [PubMed]
- McKinney, E.F.; Willcocks, L.C.; Broecker, V.; Smith, K.G. The immunopathology of ANCA-associated vasculitis. Semin. Immunopathol. 2014, 36, 461–478. [Google Scholar] [CrossRef] [PubMed]
- Kaur, J.; Arsene, C.; Yadav, S.K.; Ogundipe, O.; Malik, A.; Sule, A.A.; Krishnamoorthy, G. Risk Factors in Hospitalized Patients for Heparin-Induced Thrombocytopenia by Real World Database: A New Role for Primary Hypercoagulable States. J. Hematol. 2021, 10, 171–177. [Google Scholar] [CrossRef]
- Klinkhammer, B.; Gruchalla, M. Is There an Association Between Heparin-Induced Thrombocytopenia (HIT) and Autoimmune Disease? WMJ 2018, 117, 13–17. [Google Scholar]
- Roe, S.; Cassidy, M.; Haynes, A.; Byrne, J. Heparin-induced thrombocytopenia (HIT) and thrombosis syndrome in a haemodialysis-dependent patient with systemic vasculitis. Nephrol. Dial. Transplant. 1998, 13, 3226–3229. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Balasubramanian, S.K.; Tiruvoipati, R.; Chatterjee, S.; Sosnowski, A.; Firmin, R.K. Extracorporeal Membrane Oxygenation with Lepirudin Anticoagulation for Wegener’s Granulomatosis with Heparin-Induced Thrombocytopenia. ASAIO J. 2005, 51, 477–479. [Google Scholar] [CrossRef]
- Kaneda, K.; Fukunaga, N.; Kudou, A.; Ohno, E.; Imagawa, Y.; Ohishi, K.; Tajima, M.; Aoki, K.; Kikuchi, H.; Yasuda, T.; et al. Heparin-induced thrombocytopenia (HIT) in an acute uremic patient with ANCA-associated glomerulonephritis. Nihon Toseki Igakkai Zasshi 2009, 42, 453–458. [Google Scholar] [CrossRef]
- Thong, K.M.; Toth, P.; Khwaja, A. Management of heparin-induced thrombocytopenia (HIT) in patients with systemic vasculitis and pulmonary haemorrhage. Clin. Kidney J. 2013, 6, 622–625. [Google Scholar] [CrossRef][Green Version]
- Nonaka, T.; Harada, M.; Sumi, M.; Ishii, W.; Ichikawa, T.; Kobayashi, M. A Case of Heparin-Induced Thrombocytopenia That Developed in the Therapeutic Course of Anti-Neutrophil Cytoplasmic Antibody-Associated Vasculitis. Case Rep. Rheumatol. 2019, 2019, 2724304. [Google Scholar] [CrossRef] [PubMed]
- Furuto, Y.; Kawamura, M.; Yamashita, J.; Yoshikawa, T.; Namikawa, A.; Isshiki, R.; Takahashi, H.; Shibuya, Y. Anti-neutrophil cytoplasmic antibody-associated vasculitis accompanied by type II heparin-induced thrombocytopenia resulting in asymptomatic cerebral infarction: A case report. BMC Nephrol. 2021, 22, 220. [Google Scholar] [CrossRef] [PubMed]
- Mandai, S.; Nagahama, K.; Tsuura, Y.; Hirai, T.; Yoshioka, W.; Takahashi, D.; Aki, S.; Aoyagi, M.; Tanaka, H.; Tamura, T. Recovery of renal function in a dialysis-dependent patient with microscopic polyangiitis and both myeloperoxidase anti-neutrophil cytoplasmic antibodies and anti-glomerular basement membrane antibodies. Intern. Med. 2011, 50, 1599–1603. [Google Scholar] [CrossRef] [PubMed]
- Miki, T.; Akimoto, T.; Sugase, T.; Numata, A.; Otani, N.; Iwazu, Y.; Takeshima, E.; Morishita, Y.; Muto, S.; Kusano, E. Anti-glomerular basement membrane glomerulonephritis complicated by thrombocytopenia. Intern. Med. 2012, 51, 3395–3399. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Micarelli, D.; Ranalli, T.V.; Taddei, A.R.; Solazzo, A.; Moccia, F.; Feriozzi, S. Rapid progressive anti-GBM glomerulonephritis with multiple auto-antibodies. J. Nephropathol. 2020, 9, e30. [Google Scholar] [CrossRef]
- Xu, R.; Dang, M.H. A rare occurrence of anti-glomerular basement membrane glomerulonephritis complicated by heparin-induced thrombocytopenia. Int. J. Case Rep. Images 2020, 11, 101112Z01RX2020. [Google Scholar] [CrossRef]
- Sugawara, H.; Takizawa, H.; Shimamura, Y.; Moniwa, N.; Hasegawa, K.; Ogawa, Y. Anti-glomerular basement membrane disease accompanied by systemic lupus erythematosus presenting central nervous system involvement. CEN Case Rep. 2017, 6, 1–4. [Google Scholar] [CrossRef]
- Favaloro, E.J.; Pasalic, L.; Lippi, G. Antibodies against Platelet Factor 4 and Their Associated Pathologies: From HIT/HITT to Spontaneous HIT-Like Syndrome, to COVID-19, to VITT/TTS. Antibodies 2022, 11, 7. [Google Scholar] [CrossRef]
- Kitching, A.R.; Anders, H.J.; Basu, N.; Brouwer, E.; Gordon, J.; Jayne, D.R.; Kullman, J.; Lyons, P.A.; Merkel, P.A.; Savage, C.O.; et al. ANCA-associated vasculitis. Nat. Rev. Dis. Primers 2020, 6, 71. [Google Scholar] [CrossRef]
- McAdoo, S.P.; Pusey, C.D. Anti-Glomerular Basement Membrane Disease. Clin. J. Am. Soc. Nephrol. 2017, 12, 1162–1172. [Google Scholar] [CrossRef]
- Kato, S.; Takahashi, K.; Ayabe, K.; Samad, R.; Fukaya, E.; Friendmann, P.; Varma, M.; Bergmann, S.R. Heparin-induced thrombocytopenia: Analysis of risk factor in medical in-patients. Br. J. Haematol. 2011, 154, 373–377. [Google Scholar] [CrossRef] [PubMed]
- Arepally, G.M.; Padmanabhan, A. Heparin-Induced Thrombocytopenia: A Focus on Thrombosis. Arterioscler. Thromb. Vasc. Biol. 2021, 41, 141–152. [Google Scholar] [CrossRef] [PubMed]
- Misra, D.P.; Thomas, K.N.; Gasparyan, A.Y.; Zimba, O. Mechanisms of thrombosis in ANCA-associated vasculitis. Clin. Rheumatol. 2021, 40, 4807–4815. [Google Scholar] [CrossRef] [PubMed]
- Pishko, A.M.; Lefler, D.S.; Gimotty, P.; Paydary, K.; Fardin, S.; Arepally, G.M.; Crowther, M.; Rice, L.; Vega, R.; Cines, D.B.; et al. The risk of major bleeding in patients with suspected heparin-induced thrombocytopenia. J. Thromb. Haemost. 2019, 17, 1956–1965. [Google Scholar] [CrossRef] [PubMed]
- Sreih, A.G.; Cronin, K.; Shaw, D.G.; Young, K.; Burroughs, C.; Kullman, J.; Machireddy, K.; McAlear, C.A.; Merkel, P.A. Diagnostic delays in vasculitis and factors associated with time to diagnosis. Orphanet J. Rare Dis. 2021, 16, 184. [Google Scholar] [CrossRef]
- Borcheni, M.; Abdelazeem, B.; Malik, B.; Gurugubelli, S.; Kunadi, A. Primary Central Nervous System Vasculitis as an Unusual Cause of Intracerebral Hemorrhage: A Case Report. Cureus 2021, 13, e13847. [Google Scholar] [CrossRef]
- Martel, N.; Lee, J.; Wells, P.S. Risk for heparin-induced thrombocytopenia with unfractionated and low-molecular-weight heparin thromboprophylaxis: A meta-analysis. Blood 2005, 106, 2710–2715. [Google Scholar] [CrossRef]
- Morris, T.A.; Castrejon, S.; Devendra, G.; Gamst, A.C. No difference in risk for thrombocytopenia during treatment of pulmonary embolism and deep venous thrombosis with either low-molecular-weight heparin or unfractionated heparin: A meta analysis. Chest 2007, 132, 1131–1139. [Google Scholar] [CrossRef]
- Warkentin, T.E.; Sheppard, J.A.; Sigouin, C.S.; Kohlmann, T.; Eichler, P.; Greinacher, A. Gender imbalance and risk factor interactions in heparin-induced thrombocytopenia. Blood 2006, 108, 2937–2941. [Google Scholar] [CrossRef]
- Onuoha, C.; Barton, K.D.; Wong, E.C.C.; Raval, J.S.; Rollins-Raval, M.A.; Ipe, T.S.; Kiss, J.E.; Boral, L.I.; Adamksi, J.; Zantek, N.D.; et al. Therapeutic plasma exchange and intravenous immune globulin in the treatment of heparin-induced thrombocytopenia: A systematic review. Transfusion 2020, 60, 2714–2736. [Google Scholar] [CrossRef]
- Warkentin, T.E.; Sheppard, J.A.I.; Chu, F.V.; Kapoor, A.; Crowther, M.A.; Gangji, A. Plasma exchange to remove HIT antibodies: Dissociation between enzyme-immunoassay and platelet activation test reactivities. Blood 2015, 125, 195–198. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kang, M.; Alahmadi, M.; Sawh, S.; Kovacs, M.J.; Lazo-Langner, A. Fondaparinux for the treatment of suspected heparin-induced thrombocytopenia: A propensity score-matched study. Blood 2015, 125, 924–929. [Google Scholar] [CrossRef] [PubMed]
- Colarossi, G.; Maffulli, N.; Trivellas, A.; Schnöring, H.; Hatam, N.; Tingart, M.; Migliorini, F. Superior outcomes with Argatroban for heparin-induced thrombocytopenia: A Bayesian network meta-analysis. Int. J. Clin. Pharm. 2021, 43, 825–838. [Google Scholar] [CrossRef] [PubMed]
| Author and Year | Sex | Age | Vasculitis Type | Heparin Type | Days to 50% Drop in Platelet Count after First Exposure to Heparin | Treatment |
|---|---|---|---|---|---|---|
| ANCA vasculitis | ||||||
| Roe et al., 1998 [7] | M | 65 | PR3 | UFH | 9 days | GCs, CP, HD |
| Balasubramanian et al., 2005 [8] | M | 52 | PR3 | unspecified heparin | - | GCs, CP, CVVH, TPE, ECMO |
| Kaneda et al., 2009 [9] | F | 91 | MPO | UFH | 13 days | GCs, HD |
| Thong et al., 2013 [10] | M | 71 | PR3 | UFH and dalteparin | 7 days | GCs, CP, HD |
| Nonaka et al., 2019 [11] | F | 87 | MPO | UFH | 8 days | GCs, HD |
| Furuto et al., 2021 [12] | M | 76 | MPO | UFH | 14 days | GCs, CP, HD |
| Case 1 * | F | 71 | MPO | UFH | 6 days | GCs, CP, TPE |
| Case 3 * | M | 39 | MPO | LMWH | 14 days | GCs, CP, HD |
| anti-GBM vasculitis | ||||||
| Thong et al., 2013 [10] | M | 80 | anti-GBM | UFH and dalteparin | 8 days | GCs, CP, TPE, HD |
| Mandai et al., 2011 [13] | M | 40 | anti-GBM + MPO | UFH | 5 days | GCs, CP, TPE, HD |
| Miki et al., 2012 [14] | M | 69 | anti-GBM | unspecified heparin | 15 days | GCs, TPE, HD |
| Micarelli et al., 2020 [15] | F | 71 | anti-GBM + MPO | LMWH | 14 days | GCs, CP, TPE, HD |
| Xu et al., 2020 [16] | M | 59 | anti-GBM | LMWH | 12 days | GCs, CP, TPE, HD |
| Sugawara et al., 2017 [17] | M | 32 | anti-GBM | unspecified heparin | 7 days | GCs, TPE, HD |
| Case 2 * | M | 58 | anti-GBM | UFH | 10 days | GCs, CP, TPE |
| Case 4 * | F | 74 | anti-GBM + MPO | UFH | 14 days | GCs, CP, TPE, HD |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rytel, A.; Nowak, M.; Kukawska-Rytel, M.; Morawiec, K.; Niemczyk, S. Different Types of Vasculitis Complicated by Heparin-Induced Thrombocytopenia—Analysis of Four Cases and Literature Review. J. Clin. Med. 2023, 12, 6176. https://doi.org/10.3390/jcm12196176
Rytel A, Nowak M, Kukawska-Rytel M, Morawiec K, Niemczyk S. Different Types of Vasculitis Complicated by Heparin-Induced Thrombocytopenia—Analysis of Four Cases and Literature Review. Journal of Clinical Medicine. 2023; 12(19):6176. https://doi.org/10.3390/jcm12196176
Chicago/Turabian StyleRytel, Adam, Mateusz Nowak, Monika Kukawska-Rytel, Katarzyna Morawiec, and Stanisław Niemczyk. 2023. "Different Types of Vasculitis Complicated by Heparin-Induced Thrombocytopenia—Analysis of Four Cases and Literature Review" Journal of Clinical Medicine 12, no. 19: 6176. https://doi.org/10.3390/jcm12196176
APA StyleRytel, A., Nowak, M., Kukawska-Rytel, M., Morawiec, K., & Niemczyk, S. (2023). Different Types of Vasculitis Complicated by Heparin-Induced Thrombocytopenia—Analysis of Four Cases and Literature Review. Journal of Clinical Medicine, 12(19), 6176. https://doi.org/10.3390/jcm12196176







