Abstract
Background: One aspect of the distancing measures imposed in response to the COVID-19 pandemic is that telemedicine consultations have increased exponentially. Among these consultations, the assessment and follow-up of patients with chronic diseases in a non-presential setting has been strengthened considerably. Nevertheless, some controversy remains about the most suitable means of patient follow-up. Objective: To analyze the impact of the telemedicine measures implemented during the COVID-19 period on chronic patients. Material and Methods: A systematic review was carried out using the following databases: PubMed, Pro-Quest, and Scopus. The systematic review followed the guidelines outlined in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). The search equation utilized descriptors sourced from the Medical Subject Headings (MeSH) thesaurus. The search equation was: “hypertension AND older AND primary care AND (COVID-19 OR coronavirus)” and its Spanish equivalent. Results: The following data were obtained: 14 articles provided data on 6,109,628 patients and another 4 articles focused on a study population of 9684 physicians. Telemedicine was less likely to be used by elderly patients (OR 0.85; 95% C.I. 0.83–0.88; p = 0.05), those of Asian race (OR 0.69; 95% C.I. 0.66–0.73; p = 0.05), and those whose native language was not English (OR 0.89; 95% C.I. 0.78–0.9; p = 0.05). In primary care, lower use of telemedicine was associated with residents of rural areas (OR 0.81; p = 0.05), patients of African American race (OR 0.65, p = 0.05), and others (OR 0.64; p = 0.05). A high proportion (40%) of physicians had no prior training in telemedicine techniques. The highest quality in terms of telephone consultation was significantly associated with physicians who did not increase their prescription of antibiotherapy during the pandemic (OR = 0.30, p = 0.05) or prescribe more tests (OR 0.06 p = 0.05), i.e., who maintained their former clinical criteria despite COVID-19. Conclusions: Telemedicine is of proven value and has been especially useful in the COVID-19 pandemic. A mixed remote–presential model is most efficient. Appropriate training in this area for physicians and patients, together with correct provision, is essential to prevent errors in implementation and use.
1. Introduction
COVID-19 appeared in late 2019 in Wuhan (China), produced by a newly discovered coronavirus called SARS-CoV-2, and leading to the declaration of a health alert and pandemic in the first quarter of 2020 [1]. From the outset, social distancing was among the main measures employed to prevent infection [2,3]. This scenario has led to the development of non-presential consultations for the resolution of health problems while minimizing exposure to the virus, thus generating a boom in telemedicine [4].
Telemedicine had been employed before the appearance of the SARS-CoV-2, as an efficient form of medical consultation. An example of this is the advanced triage service, or teleconsultation, that had been operational for many years in American hospitals such as Jefferson Health, Mount Sinai, Cleveland Clinic, and Providence [5], a development that has been facilitated by technical and technological advances in medical science [6]. The first non-presential consultation was performed in 1905 by William Einthoven, who performed tele-electrocardiography and telephonic cardiac auscultation from his laboratory and from Leyden Hospital [7]. The technique is now widely used for patients with diabetes [8], chronic disease, or even mental health problems. In rural and semi-urban areas, access to medical services may be limited; elsewhere, access to consultations can also be restricted in order to avoid the spread of infection. The generalized lockdowns imposed during the recent pandemic compounded the problem [9]. For example, patients with hypertension experienced severe negative consequences for the control of their disease during the first months of the pandemic due to the restrictions imposed on mobility [10].
For all these reasons, technological solutions are increasingly being used to monitor patients remotely, especially for chronic patients and as a means of triaging potential patients with coronaviruses or other diseases in order to minimize the spread of infection [11]. Hypertension, the most prevalent chronic disease, is present in one third of the European population and in over 60% of patients aged 80 years or more, and is a risk factor for severe COVID-19 [12]. Home blood pressure monitoring enables telematically assessable follow-up, as an example of the practical value of non-presential healthcare [13]. However, despite its advantages, especially in the pandemic circumstances described, there remain areas in which telemedicine has little or no implementation, due to insufficient training or knowledge among healthcare professionals and/or users. Interestingly, chronic patients with hypertension have been among the least affected by the pandemic compared to patients with other conditions [14].
In view of these considerations, the use of telemedicine is expected to increase significantly to help manage the acute and chronic diseases experienced by an aging population whose longer life expectancy and better survival from cardiovascular events are reflected in a greater health burden. The use of remote consultations has played a major role among the healthcare measures implemented during the COVID-19 pandemic. Thanks to the establishment of classification and rapid response protocols, access and care for patients have been facilitated, minimizing the occurrence of complications and protecting the chronically ill and those over 80 years of age [15]. In the specific case of patients with hypertension, remote blood pressure monitoring has been highly successful, enabling faster patient follow-up and maintaining pre-pandemic levels of care [16].
The main aim of the present study is to analyze the use of telemedicine on the diagnosis, medical monitoring, and treatment of chronic hypertensive patients during the COVID-19 pandemic.
2. Materials and Methods
2.1. Design and Search Strategy
The review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [17]. The following databases were consulted: PubMed, Pro-Quest, and Scopus. The Mesh terms employed in the search strategy were “hypertension AND older AND primary care AND (COVID-19 OR coronavirus)” and their equivalent in Spanish. The search was conducted in June 2023. Two reviewers participated in the screening process (see Figure 1). The study was registered (ID: 462362) in the PROSPERO database (International Prospective Register of Systematic Reviews).
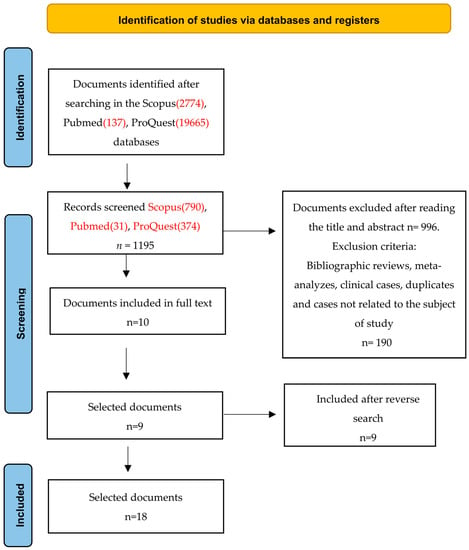
Figure 1.
Flow diagram of the publication search process [17].
2.2. Eligibility Criteria
Inclusion criteria: Primary quantitative studies investigating the impact of telemedicine on COVID respiratory syndrome pathology in hypertensive patients within a primary care setting, and published in either English or Spanish, were included without imposing any limitations on the publication year.
Exclusion criteria: Doctoral theses, articles without statistical information, duplicate studies, those not carried out in adults, or those whose main objective was not to investigate the relationship between telemedicine and its relationship with the consequences of the SARS-CoV-2.
2.3. Study Selection Process
Two team members (M.Q.-C. and A.M.C.-M.) conducted the search and study selection autonomously. If a discrepancy arose, a third researcher (A.C.-G.) was brought in for consultation. The article selection process involved four stages: (1) reviewing the title and abstract, (2) excluding articles not meeting the inclusion criteria, (3) examining the complete text, and (4) conducting a reverse search.
2.4. Data Extraction and Data Analysis
For data extraction from each study, a dedicated data collection notebook was crafted. This notebook encompassed essential information such as the primary author, publication year, study country, research design, sample details, the intervention upon which the study was centered, mean and standard deviation (SD), main results, and level of evidence. A descriptive analysis was done for the systematic review and two prevalence meta-analyses were performed, one about the satisfaction with the service of telemedicine and one about the prevalence of hypertension. The heterogeneity was assessed with I2 and publication bias with Egger test. The analysis was performed with the software StatsDirect.
2.5. Risk of Bias Assessment and Level of Evidence
The assessment of bias risk utilized the elimination questions derived from the CASP (Critical Appraisal Skills Program) specifically designed for cohort studies (Supplementary Table S1), including the studies with positive response to the three questions. In addition, we carried out the Egger test to assess the risk of bias. The evaluation of the quality of the studies incorporated into this review adhered to the levels of evidence and recommendation grades outlined by the Oxford Center for Evidence-Based Medicine (OCEBM) [18].
3. Results
3.1. Characteristic of the Studies Included
The initial search obtained 22,576 studies (PubMed 137; ProQuest 19,665; Scopus 2774), of which 323 were duplicates and discarded. After reading the title and abstract of each paper, 1195 (PubMed 31; ProQuest 374; Scopus 790) articles were selected for further analysis. Of these, 996 were not quantitative studies and a further 189 were unrelated to the subject of our investigation; all were excluded. Of the remaining 10 articles, 1 was excluded because it did not have access to full text, leaving 9. The reverse search procedure of the references cited obtained a further 9 eligible articles, resulting in a final total of 18 papers included in the definitive analysis [19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36] (see Figure 1).
These studies were carried out in the USA (six studies), Israel (three studies), Canada (two studies), and in Portugal, Norway, United Kingdom (UK), Chile, Saudi Arabia, Republic of Korea, and Spain (one study in each). Eight were cohort studies and eleven were transversal studies. Information on the characteristics of each study is shown in Table 1.

Table 1.
Information on the selected studies.
In total, 6,109,628 patients were included in these studies, but 5,791,812 corresponded to a single study [18]. In four papers [19,25,28,29,35], the study population was composed of doctors (total 9684, of which 7742 corresponded to a single study [28]).
In every case, hypertensive patients were included in the study samples analyzed, and in one paper they were exclusively analyzed as representative of patients with chronic disease [19].
3.2. Telemedicine, Consult Perception
According to the articles that considered patients’ opinions, most were highly satisfied with the telemedicine process. Thus, Gomes Almeida et al. (2020) found that 70.6% preferred this approach; Rodriguez-Fortúnez et al. [23] reported that 73.5% believed it optimized the management of their disease; and Zanaboni et al. [27] informed that for 72% of patients, telemedicine enhanced follow-up and for 58%, it improved the quality of treatment.
Eberly et al. [21] generated a patient profile according to which telemedicine was less commonly used by older patients (OR = 0.85; 95% C.I. 0.83–0.88; p = 0.05), those of Asian race (OR = 0.69; 95% C.I. 0.66–0.73; p = 0.05, those whose native language was not English (OR 0.89; 95% C.I. 0.78–0.9; p = 0.05), and those whose health insurance was provided by Medicaid (OR 0.93; C.I. 0.89–0.97; p = 0.05).
Ufholz et al. [33] reported that older patients showed less use of telemedicine (23%) despite near to 80% having access to technology.
Barayev et al. [25] observed that, for 60.7% of primary care physicians, WhatsApp® consultations reduced the need for in-person visits at least once a week.
Chang et al. [26] observed more barriers to the use of telemedicine consultation in patients with a high Social Vulnerability Index (p = 0.001). Similarly, Dopelt et al. [24] established an association between literacy and patient satisfaction with the use of telemedicine (rp = 0.39 p = 0.001).
3.3. Telemedicine in COVID-19 Context
Gomes-de Almeida et al. [22] reported a reduction of 94.1% in face-to-face consultations by patients with hypertension and of 50.1% by patients with diabetes, while the use of telemedicine rose by 61.9%. Eberly et al. [21] focused on 148,402 appointment requests for telemedicine, of which 80,780 appointments actually took place; in 78,539 of these cases, the visit modality was specified.
Summers et al. [20] observed that many patients expressed concern about who might have access to their personal health data and about its future use (R = 0.916; p = 0.01). In addition, a strong correlation was recorded between people who wanted stronger data protection legislation and those who were worried about the re-use of the health data collected (R = 0.636; p = 0.01). Kaufman-Shriqui et al. [29] indicated that the majority of doctors who participated in their study (59.7%) carried out mixed (presential and telephone) counselling.
Lee et al. [19] observed a statistically significant decrease (p = 0.0001) in the continuity of care measured per physician and also in the number of physician visit days after the outbreak of COVID-19. The latter value decreased by 0.293 days, which, excluding the effects of telemedicine, amounts to 0.3330 days (p = 0.0001).
Dopelt et al. [24] addressed an 85% Internet-literate population, of whom 93% claimed to be well versed in e-health issues (in areas such as booking appointments and renewing prescriptions). However, only 38% of this population made use of the Internet for consultation or treatment sessions.
Dalbosco-salas et al. [36] showed that the telerehabilitation program implemented within primary healthcare has demonstrated feasibility and led to enhancements in physical capacity, quality of life, and symptom relief among adult COVID-19 survivors.
3.4. Telephone vs. Video Consultation
In a study of 78,539 telemedicine consultations, Eberly et al. [21] found that 54% were conducted by telephone and 46% by video call. The lower rate of video call use was associated with the following characteristics: patients of advanced age (OR = 0.79; p = 0.05), female sex (OR = 0.92; p = 0.05), African American race (OR = 0.65; p = 0.05), Hispanic race (OR 0.9; p = 0.05), and low socioeconomic status (OR = 0.57, p = 0.05 for income of <50,000 USD per year and OR 0.89, p = 0.05 for income of 50,000–100,000 USD per year).
Pierce and Stevermer [28] generated the following population profile for higher video call use: female sex (OR = 1.15, p = 0.05), age over 65 years (OR = 0.27, p = 0.05), African American race (OR = 0.72, p = 0.05), self-pay for healthcare (OR = 1.26, p = 0.05), or Medicaid (OR = 0.3,6 p = 0.05) or Medicare (OR = 0.79, p = 0.05). The authors also profiled a lower use of telemedicine consultation by patients living in rural areas (OR = 0.81, p = 0.05), those of African American race (OR = 0.65, p = 0.05), and those of other races (OR = 0.64, p = 0.05).
Chang et al. [26] reported that tele-calling was the main telehealth modality for the low Social Vulnerability Index (SVI) population, at 41.7% compared to 23.8% for the high SVI population (p = 0.01). Video calling, however, was the preferred modality in low SVI areas, at 33.7% (p = 0.01) compared to 18.7% in high SVI areas.
Juergens et al. [31] noted a total of 86,676 (41.5%) video consultations and 122,051 (58.5%) telephone consultations. Skin and soft tissue conditions exhibited the highest proportion of video visits (59.7%), while mental health conditions had the highest proportion of telephone visits (71.1%). Upon covariate adjustment, the overall rates of medication orders (46.6% vs. 44.5%), imaging orders (17.3% vs. 14.9%), lab orders (19.5% vs. 17.2%), and antibiotic orders (7.5% vs. 5.2%) were higher during video visits compared to telephone visits (p < 0.05). The most significant difference within the diagnostic groups was observed in skin and soft tissue conditions, where the rate of medication orders was 9.1% higher during video visits compared to telephone visits (45.5% vs. 36.5%, p < 0.05).
3.5. Doctors’ Use of Telemedicine vs. Presential Attention
Kaufman-Shriqui et al. [29], in a study focused on primary care, found that among physicians providing both in-person consultations and telemedicine during the COVID-19 pandemic, 40% had no prior training in the latter modality. They also reported that a higher quality of telephone consultation was significantly associated with doctors who did not increase their rates of antibiotherapy relative to the pre-pandemic situation (OR = 0.30, p = 0.05). Higher online quality was also associated with doctors who did not prescribe more tests than previously (OR = 0.06, p = 0.05).
Pierce and Stevermer [28] studied family doctors providing primary care in an out-of-hospital setting. These authors generated a user profile in which the lower use of telemedicine was associated with patients who were rural residents (OR 0.81, p = 0.05), of African American race (OR 0.65, p = 0.05), or of other races (OR = 0.64, p = 0.05).
Barayev et al. [25] analyzed 153 out-of-hospital family doctors and 48 in-hospital doctors, 86.9% and 86.5%, respectively, of whom used WhatsApp® on a daily basis in a professional environment. Additional workload, possible breach of patient confidentiality, and lack of documentation on consultations were the main concerns among both groups of doctors. Nevertheless, 60.7% of primary care doctors and 95.7% of hospital specialists agreed that telemedicine is a useful tool for reducing the number of face-to-face appointments required. Finally, Chang et al. [26] studied the use of telemedicine in primary care in New York City in 2020 during the pandemic. These authors observed that telemedicine was provided unevenly and faced both patient- and provider-related barriers.
In a primary care investigation, Singer et al. [30] stated that there was no notable distinction in the quantity of follow-up visits administered in a clinic visit compared to a virtual care visit (8.7% vs. 5.8%) (p = 0.6496).
3.6. Meta-Analysis
The meta-analysis of random effects about the prevalence of hypertension included 6 studies with a sample of n =10,464 and a meta-analytical estimation of 52%, CI 95% (39%, 66%) (Figure 2) and I2 value of 99.2%. The Egger test result was −3.97 (p > 0.5).
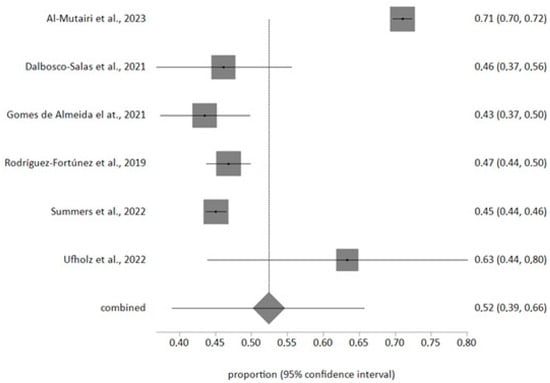
Figure 2.
Forest plot of hypertension prevalence [20,22,23,32,33,36].
The meta-analysis of random effects about the satisfaction with telemedicine included 2 studies with a sample of n = 1969 and a meta-analytical estimation of 89%, CI 95% (85%, 92%) (Figure 3), and I2 value of 69.3%. The Egger test result was −8.12 (p > 0.2). One included study analyzed the satisfaction with telemedicine with a Likert scale from 1 to 5 and the other analyzed satisfaction assessing the satisfaction comparing telemedicine quality with in-person visits.
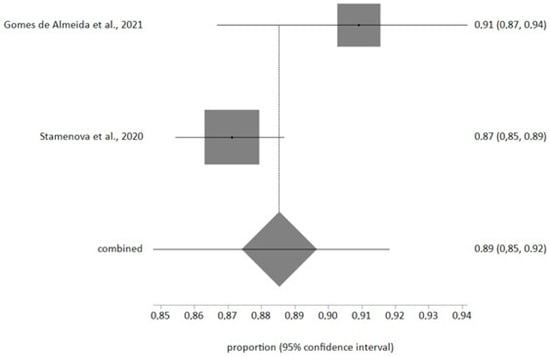
Figure 3.
Forest plot of patients’ satisfaction with telemedicine prevalence [22,35].
4. Discussion
In this study, we analyze the role of telemedicine in its different formats. This form of healthcare had, to some extent, been employed previously, but became indispensable during the COVID-19 pandemic, as health systems worldwide struggled to meet the needs of users. Telemedicine was seen as the best way to minimize risks to healthcare staff and patients, and its use expanded exponentially [37,38].
In the last 50 years, medical care has undergone major changes, with the parallel provision of urgent and programmed care, together with novel processes to optimize treatments and follow-up. Primary healthcare, as the first link in the care chain, activates patient care and follow-up, while referral to specialists is the final step, whether or not an intervention finally takes place. In the latter case, depending on the severity of the illness, there must be subsequent re-evaluation and, if necessary, the continuation of treatment and/or prevention of recurrence. This is the case, for example, with acute or chronic processes such as cardiovascular problems, for which telematic monitoring, based on new technologies, provides a valuable treatment option [39,40,41].
The incorporation of a telematics approach can speed up healthcare processes by facilitating treatment continuity and follow-up in a non-presential manner, especially by means of telephone and video-call consultations [42]. The first approach is the most accessible, the cheapest, and the most widely used. It allows fast and efficient communication for simple consultations and is recommended for bureaucratic consultations such as prescription renewals, work incapacity reports, or requests for diagnostic tests for follow-up [43]. Video consultations have the advantage that the patient can be visualized, thus enabling a diagnosis to be more accurately approximated. This channel is objectively superior, and the equipment required is not complicated; nevertheless, the economic cost per consultation is higher and it is less widely used [44]. However, neither method is ideal for making a new diagnosis, as they do not allow the physician to conduct a complete exploration or to fully assess the patient’s non-verbal language, elements that can only be achieved in a face-to-face consultation [45].
The emergence of social networks and apps that expand the facilities available for human contact has given a new impetus to the use of remote communication, and their incorporation into telemedicine has facilitated the greater use of this approach. However, this must always be done with full regard for patient privacy and in compliance with data protection legislation, restrictions that can sometimes limit its use [46]. Currently, telemedicine is well accepted by patients, who find it as valid as in-person consultation, in part because the physician can attend more patients in a given period, and waiting times are reduced. Furthermore, telemedicine increases accessibility for patients with contagious diseases, as is the case with COVID-19 [47].
After the initial diagnosis, patients with hypertension can be monitored effectively by means of telemedicine [48]. However, although patient records and monitoring are acceptable with this approach, the quality of measurements obtained may decrease [49]. Smartphone apps, in conjunction with the self-monitoring of blood pressure, already form part of telemedicine, and have proven to be effective in providing discreet monitoring; their supervised use, in parallel with routine treatment, is recommended [50].
Finally, sufficient resources are currently available for the provision of telemedicine (mainly by telephone) throughout Europe, both in primary care and in hospitals. The studies reviewed are generally in accordance with this conclusion, although most have been carried out in western Europe, Canada, and the USA, while fewer data are available with respect to the use of telemedicine in eastern Europe. In fact, the trend worldwide and in the countries analyzed in this study demonstrates the growing interest in telehealth. Thanks to the study conducted during the pandemic in these countries, better health strategies and policies can be designed [51], which is much needed as previous studies show that telehealth infrastructures are inadequate [52]. The impact of the action protocols implemented in response to the COVID-19 pandemic has highlighted the remarkable value offered by the correct use of telemedicine [53]. On the other hand, in some medical specialties, its implementation has been less successful, with discrepancies between users’ expectations and the results obtained. One such case is the rehabilitation service, where treatment with inadequate equipment and/or materials can hinder rather than assist the patient’s recovery [54]. Therefore, the implementation of telemedicine must be carefully tailored to the needs of the healthcare system and to facilitate treatment, making sure that it is never the cause of under-diagnosis, misdiagnosis, or mistreatment. In other words, telemedicine should be applied to make the system more dynamic without losing the essence of the medical consultation.
The meta-analysis reported a prevalence estimation of 52%; this is in agreement with previous studies [55] but the American prevalence is high in older patient [56]. This situation may be due to there being new hypertensive limits in North America, 130/80 mmHg instead of 140/90 mmHg [57,58]; therefore, older patients do not have complete access to telemedicine and this is the population range with less telematic media use. Satisfaction has a very high level in our study and is similar to that in other similar articles [22,59]. The use of telemedicine improves the control and the contact with our patients and can be the reason for this high acceptance.
This study faced certain limitations. Initially, despite focusing on primary studies that analyzed the impact of telemedicine during the COVID-19 era, the diverse array of study designs and differing characteristics introduced heterogeneity in the outcomes. In addition, the fact that the studies were conducted in health systems in different countries may influence the variability of results. A meta-analysis was conducted; however, incorporating all the selected studies was unfeasible due to the substantial variability in parameters and analyzed variables.
Therefore, for future research, it is necessary to carry out more studies with larger samples and to analyze the evolution over time. It is also recommended that randomized clinical trials be conducted to explore in more depth how this care activity could benefit users.
5. Conclusions
The results imply that the utilization of telemedicine is an efficient means of diagnosis and follow-up, as has been demonstrated during the COVID-19 pandemic. Telephone consultation is the most widely used form of telemedicine, due to widespread telephone access and it being cheaper than other telematic medicine options.
However, appropriate provision and training for professionals and patients is needed in order to avoid problems in the implementation and application of resources. In-person consultations must continue to exist and will never be entirely replaced by telemedicine, which can be of great assistance, for example by facilitating follow-up, but also presents significant shortcomings that cannot be overcome.
Because of this, it is advisable to create more guidelines for telemedicine, improve knowledge, and improve telemedicine implementation, and future investigation will be necessary for a correct medical assistance.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm12196160/s1, Table S1: Critical reading of included studies.
Author Contributions
Conceptualization, M.Q.-C. and G.A.C.-D.l.F.; Methodology, G.A.C.-D.l.F., A.M.C.-M. and J.L.R.-B.; Software, S.C.-P.; Validation, G.A.C.-D.l.F. and J.L.R.-B.; Formal analysis, M.Q.-C., A.C.-G. and A.M.C.-M.; Investigation, S.C.-P.; Resources, O.F.-M.; Data curation, A.M.C.-M. and S.C.-P.; Writing—original draft preparation, M.Q.-C. and A.C.-G.; Writing—review and editing, O.F.-M., M.Q.-C. and A.C.-G.; Visualization, G.A.C.-D.l.F.; Supervision, J.L.R.-B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Acknowledgments
This study forms part of the doctoral thesis of the first-named author within the Clinical Medicine and Public Health Doctoral Program at the University of Granada.
Conflicts of Interest
The authors declare no conflict of interest.
References
- WHO. Guidance on Routine Immunization Services during COVID-19 Pandemic in the WHO European Region, 20 March 2020 n.d. Available online: https://www.who.int/europe/publications/i/item/WHO-EURO-2020-1059-40805-55114 (accessed on 13 July 2022).
- CDC. How to Protect Yourself and Others|CDC n.d. Available online: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fprevent-getting-sick%2Fsocial-distancing.html#stay6ft (accessed on 23 October 2022).
- Guillem, F.C. Opportunities and threats for prevention and health promotion and the PAPPS in the context of the COVID-19 pandemic. Aten. Prim. 2020, 52, 449–451. [Google Scholar] [CrossRef] [PubMed]
- Magoon, V. Operationalizing virtual visits during a public health emergency. Fam. Pract. Manag. 2020, 27, 5–12. [Google Scholar] [PubMed]
- Hollander, J.E.; Carr, B.G. Virtually Perfect? Telemedicine for COVID-19. N. Engl. J. Med. 2020, 382, 1679–1681. [Google Scholar] [CrossRef] [PubMed]
- Jagarapu, J.; Savani, R.C. A brief history of telemedicine and the evolution of teleneonatology. Semin. Perinatol. 2021, 45, 151416. [Google Scholar] [CrossRef]
- Hjelm, N.M.; Julius, H.W. Centenary of tele-electrocardiography and telephonocardiography. J. Telemed. Telecare 2005, 11, 336–338. [Google Scholar] [CrossRef]
- Horton, M.B.; Brady, C.J.; Cavallerano, J.; Abramoff, M.; Barker, G.; Chiang, M.F.; Crockett, C.H.; Garg, S.; Karth, P.; Liu, Y.; et al. Practice Guidelines for Ocular Telehealth-Diabetic Retinopathy, Third Edition—PubMed (nih.gov). Telemed. J. e-Health 2020, 26, 495–543. [Google Scholar] [CrossRef]
- Cullington, H.; Kitterick, P.; Darnton, P.; Finch, T.; Greenwell, K.; Riggs, C.; Weal, M.; Walker, D.M.; Sibley, A. Telemedicine for Adults with Cochlear Implants in the United Kingdom (CHOICE): Protocol for a Prospective Interventional Multisite Study. JMIR Res. Protoc. 2022, 11, e27207. [Google Scholar] [CrossRef]
- Gotanda, H.; Liyanage-Don, N.; Moran, A.E.; Krousel-Wood, M.; Green, J.B.; Zhang, Y.; Nuckols, T.K. Changes in blood pressure outcomes among hypertensive individuals during the COVID-19 pandemic: A time series analysis in three US healthcare organizations. Hypertension 2022, 79, 2733–2742. [Google Scholar] [CrossRef]
- Mandrioli, J.; Santangelo, M.; Luciani, A.; Toscani, S.; Zucchi, E.; Giovannini, G.; Martinelli, I.; Cecoli, S.; Bigliardi, G.; Scanavini, S.; et al. TeleNeurological evaluation and Support for the Emergency Department (TeleNS-ED): Protocol for an open-label clinical trial. BMJ Open 2021, 11, e048293. [Google Scholar] [CrossRef]
- Underlying Medical Conditions Associated with Higher Risk for Severe COVID-19, Information for Healthcare Professionals|CDC n.d. Available online: https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/underlyingconditions.html (accessed on 14 July 2022).
- Reuter, H.; Jordan, J. Status of hypertension in Europe. Curr. Opin. Cardiol. 2019, 34, 342–349. [Google Scholar] [CrossRef]
- Varandani, S.; Nagib, N.D. Evaluating the impact of the COVID-19 pandemic on monthly trends in primary care. Cureus 2022, 14, e28353. [Google Scholar] [CrossRef] [PubMed]
- Omboni, S.; McManus, R.J.; Bosworth, H.B.; Chappell, L.C.; Green, B.B.; Kario, K.; Logan, A.G.; Magid, D.J.; Mckinstry, B.; Margolis, K.L.; et al. Evidence and recommendations on the use of telemedicine for the management of arterial hypertension: An international expert position paper. Hypertension 2020, 76, 1368–1383. [Google Scholar] [CrossRef] [PubMed]
- Armitage, L.C.; Lawson, B.K.; Roman, C.; Thompson, B.; Biggs, C.; Rutter, H.; Lewis-Jones, M.; Ede, J.; Tarassenko, L.; Farmer, A.; et al. Ambulatory blood pressure monitoring using telemedicine: Proof-of-concept cohort and failure modes and effects analyses. Wellcome Open Res. 2022, 7, 39. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, 71. [Google Scholar] [CrossRef]
- Howick, J.; Chalmers, I.; Glasziou, P.; Greenhalg, T.; Heneghan, C.; Liberati, A.; Moschetti, I.; Phillips, B.; Thornton, H. The Oxford Levels of Evidence. 2011. Available online: https://www.cebm.net/2016/05/ocebmlevels-of-evidence (accessed on 14 November 2022).
- Lee, S.Y.; Chun, S.Y.; Park, H. The impact of COVID-19 protocols on the continuity of care for patients with hypertension. Int. J. Environ. Res. Public Health 2022, 19, 1735. [Google Scholar] [CrossRef]
- Summers, C.; Griffiths, F.; Cave, J.; Panesar, A. Understanding the security and privacy concerns about the use of identifiable health data in the context of the COVID-19 pandemic: Survey study of public attitudes toward COVID-19 and data-sharing. JMIR Form. Res. 2022, 6, e29337. [Google Scholar] [CrossRef]
- Eberly, L.A.; Kallan, M.J.; Julien, H.M.; Haynes, N.; Khatana, S.A.M.; Nathan, A.S.; Snider, C.; Chokshi, N.P.; Eneanya, N.D.; Takvorian, S.U.; et al. Patient characteristics associated with telemedicine access for primary and specialty ambulatory care during the COVID-19 pandemic. JAMA Netw. Open 2020, 3, e2031640. [Google Scholar] [CrossRef]
- Gomes-de Almeida, S.; Marabujo, T.; do Carmo-Gonçalves, M. Telemedicine satisfaction of primary care patients during COVID-19 pandemics. Semergen 2021, 47, 248–255. [Google Scholar] [CrossRef]
- Rodríguez-Fortúnez, P.; Franch-Nadal, J.; Fornos-Pérez, J.A.; Martínez-Martínez, F.; de Paz, H.D.; Orera-Peña, M.L. Cross-sectional study about the use of telemedicine for type 2 diabetes mellitus management in Spain: Patient’s perspective. The EnREDa2 Study. BMJ Open 2019, 9, e028467. [Google Scholar] [CrossRef]
- Dopelt, K.; Avni, N.; Haimov-Sadikov, Y.; Golan, I.; Davidovitch, N. Telemedicine and eHealth literacy in the era of COVID-19: A cross-sectional study in a peripheral clinic in Israel. Int. J. Environ. Res. Public Health 2021, 18, 9556. [Google Scholar] [CrossRef]
- Barayev, E.; Shental, O.; Yaari, D.; Zloczower, E.; Shemesh, I.; Shapiro, M.; Glassberg, E.; Magnezi, R. WhatsApp Tele-Medicine—Usage patterns and physicians views on the platform. Isr. J. Health Policy Res. 2021, 10, 34. [Google Scholar] [CrossRef]
- Chang, J.E.; Lai, A.Y.; Gupta, A.; Nguyen, A.M.; Berry, C.A.; Shelley, D.R. Rapid transition to telehealth and the digital divide: Implications for primary care access and equity in a post-COVID era. Milbank Q. 2021, 99, 340–368. [Google Scholar] [CrossRef]
- Zanaboni, P.; Fagerlund, A.J. Patients’ use and experiences with e-consultation and other digital health services with their general practitioner in Norway: Results from an online survey. BMJ Open 2020, 10, e034773. [Google Scholar] [CrossRef]
- Pierce, R.P.; Stevermer, J.J. Disparities in use of telehealth at the onset of the COVID-19 public health emergency. J. Telemed. Telecare 2020, 29, 3–9. [Google Scholar] [CrossRef]
- Kaufman-Shriqui, V.; Shani, M.; Boaz, M.; Lahad, A.; Vinker, S.; Birk, R. Opportunities and challenges in delivering remote primary care during the Coronavirus outbreak. BMC Prim. Care 2022, 23, 135. [Google Scholar] [CrossRef]
- Singer, A.; Kosowan, L.; LaBine, L.; Shenoda, D.; Katz, A.; Abrams, E.M.; Halas, G.; Wong, S.T.; Talpade, S.; Kirby, S.; et al. Characterizing the use of virtual care in primary care settings during the COVID-19 pandemic: A retrospective cohort study. BMC Prim. Care 2022, 23, 320. [Google Scholar] [CrossRef] [PubMed]
- Juergens, N.; Huang, J.; Gopalan, A.; Muelly, E.; Reed, M. The association between video or telephone telemedicine visit type and orders in primary care. BMC Med. Inform. Decis. Mak. 2022, 22, 302. [Google Scholar] [CrossRef] [PubMed]
- Al-Mutairi, A.M.; Alshabeeb, M.A.; Abohelaika, S.; Alomar, F.A.; Bidasee, K.R. Impact of telemedicine on glycemic control in type 2 diabetes mellitus during the COVID-19 lockdown period. Front. Endocrinol. 2023, 14, 1068018. [Google Scholar] [CrossRef]
- Ufholz, K.; Sheon, A.; Bhargava, D.; Rao, G. Telemedicine Preparedness Among Older Adults with Chronic Illness: Survey of Primary Care Patients. JMIR Form. Res. 2022, 6, e35028. [Google Scholar] [CrossRef] [PubMed]
- Khairat, S.; Meng, C.; Xu, Y.; Edson, B.; Gianforcaro, R. Interpreting COVID-19 and Virtual Care Trends: Cohort Study. JMIR Public Health Surveill. 2020, 6, e18811. [Google Scholar] [CrossRef]
- Stamenova, V.; Agarwal, P.; Kelley, L.; Fujioka, J.; Nguyen, M.; Phung, M.; Wong, I.; Onabajo, N.; Bhatia, R.S.; Bhattacharyya, O. Uptake and patient and provider communication modality preferences of virtual visits in primary care: A retrospective cohort study in Canada. BMJ Open 2020, 10, e037064. [Google Scholar] [CrossRef]
- Dalbosco-Salas, M.; Torres-Castro, R.; Rojas Leyton, A.; Morales Zapata, F.; Henríquez Salazar, E.; Espinoza Bastías, G.; Beltrán Díaz, M.E.; Tapia Allers, K.; Mornhinweg Fonseca, D.; Vilaró, J. Effectiveness of a Primary Care Telerehabilitation Program for Post-COVID-19 Patients: A Feasibility Study. J. Clin. Med. 2021, 10, 4428. [Google Scholar] [CrossRef]
- Reed, M.; Huang, J.; Graetz, I.; Muelly, E.; Millman, A.; Lee, C. Treatment and follow-up care associated with patient-scheduled primary care telemedicine and in-person visits in a large integrated health system. JAMA Netw. Open 2021, 4, e2132793. [Google Scholar] [CrossRef] [PubMed]
- Laddu, D.; Ma, J.; Kaar, J.; Ozemek, C.; Durant, R.W.; Campbell, T.; Welsh, J.; Turrise, S. Health behavior change programs in primary care and community practices for cardiovascular disease prevention and risk factor management among midlife and older adults: A scientific statement from the American Heart Association. Circulation 2021, 144, E533–E549. [Google Scholar] [CrossRef]
- Gulati, M.; Levy, P.D.; Mukherjee, D.; Amsterdam, E.; Bhatt, D.L.; Birtcher, K.K.; Blankstein, R.; Boyd, J.; Bullock-Palmer, R.P.; Conejo, T.; et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the Evaluation and Diagnosis of Chest Pain: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2021, 78, e187–e285. [Google Scholar] [CrossRef] [PubMed]
- Kelsey, M.D.; Nelson, A.J.; Green, J.B.; Granger, C.B.; Peterson, E.D.; McGuire, D.K.; Pagidipati, N.J. Guidelines for cardiovascular risk reduction in patients with type 2 diabetes: JACC Guideline Comparison. J. Am. Coll. Cardiol. 2022, 79, 1849–1857. [Google Scholar] [CrossRef] [PubMed]
- Han, X.; Chen, W.; Gao, Z.; Lv, X.; Sun, Y.; Yang, X.; Shan, H. Effectiveness of telemedicine for cardiovascular disease management: Systematic review and meta-analysis. Ann. Palliat. Med. 2021, 10, 12831–12844. [Google Scholar] [CrossRef]
- Jiang, W.; Majumder, S.; Kumar, S.; Subramaniam, S.; Li, X.; Khedri, R.; Mondal, T.; Abolghasemian, M.; Satia, I.; Deen, M.J. A wearable tele-health system towards monitoring COVID-19 and chronic diseases. IEEE Rev. Biomed. Eng. 2022, 15, 61–84. [Google Scholar] [CrossRef]
- Fisher, K.; Davey, A.R.; Magin, P. Telehealth for Australian general practice: The present and the future. Aust. J. Gen. Pract. 2022, 51, 626–629. [Google Scholar] [CrossRef]
- Carrillo de Albornoz, S.; Sia, K.L.; Harris, A. The effectiveness of teleconsultations in primary care: Systematic review. Fam. Pract. 2022, 39, 168–182. [Google Scholar] [CrossRef]
- Hammersley, V.; Donaghy, E.; Parker, R.; McNeilly, H.; Atherton, H.; Bikker, A.; Campbell, J.; McKinstry, B. Comparing the content and quality of video, telephone, and face-to-face consultations: A non-randomised, quasi-experimental, exploratory study in UK primary care. Br. J. Gen. Pract. 2019, 69, E595–E604. [Google Scholar] [CrossRef]
- Morris, C.; Scott, R.E.; Mars, M. WhatsApp in clinical practice-the challenges of record keeping and storage. A scoping review. Int. J. Environ. Res. Public Health 2021, 18, 13426. [Google Scholar] [CrossRef] [PubMed]
- Pallarés Carratalá, V.; Górriz-Zambrano, C.; Llisterri Caro, J.L.; Gorriz, J.L. The COVID-19 pandemic: An opportunity to change the way we care for our patients. Semergen 2020, 46, 3–5. [Google Scholar] [CrossRef]
- Taylor, P.; Berg, C.; Thompson, J.; Dean, K.; Yuan, T.; Nallamshetty, S.; Tong, I. Effective access to care in a crisis period: Hypertension control during the COVID-19 pandemic by telemedicine. Mayo Clin. Proc. Innov. Qual. Outcomes 2022, 6, 19–26. [Google Scholar] [CrossRef]
- Ye, S.; Anstey, D.E.; Grauer, A.; Metser, G.; Moise, N.; Schwartz, J.; Kronish, I.; Abdalla, M. The impact of telemedicine visits on the controlling high blood pressure quality measure during the COVID-19 pandemic: Retrospective cohort study. JMIR Form. Res. 2022, 6, e32403. [Google Scholar] [CrossRef] [PubMed]
- Kassavou, A.; Wang, M.; Mirzaei, V.; Shpendi, S.; Hasan, R. The association between smartphone app-based self-monitoring of hypertension-related behaviors and reductions in high blood pressure: Systematic review and meta-analysis. JMIR mHealth uHealth 2022, 10, e34767. [Google Scholar] [CrossRef] [PubMed]
- Arshad Ali, S.; Bin Arif, T.; Maab, H.; Baloch, M.; Manazir, S.; Jawed, F.; Kumar Ochani, R. Global Interest in Telehealth During COVID-19 Pandemic: An Analysis of Google Trends™. Cureus 2020, 12, e10487. [Google Scholar] [CrossRef] [PubMed]
- Coronavirus Disease (COVID-19) Weekly Epidemiological Updates and Monthly Operational Updates. 2020. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports (accessed on 14 September 2023).
- Saigí-Rubió, F.; Nascimento, I.J.B.D.; Robles, N.; Ivanovska, K.; Katz, C.; Azzopardi-Muscat, N.; Ortiz, D.N. The current status of telemedicine technology use across the World Health Organization European Region: An overview of systematic reviews. J. Med. Internet Res. 2022, 24, e40877. [Google Scholar] [CrossRef]
- Peterson, S.; Young, J.; King, V.; Meadows, J. Patient expectations for synchronous telerehabilitation visits: A survey study of telerehabilitation-naive patients. Telemed. J. e-Health 2022, 28, 422–432. [Google Scholar] [CrossRef]
- Fakhri, G.; Assaad, S.; Chaaya, M. Hypertension prevalence and control among community-dwelling lebanese older adults. J. Clin. Hypertens. 2020, 22, 1727–1731. [Google Scholar] [CrossRef] [PubMed]
- Muli, S.; Meisinger, C.; Heier, M.; Thorand, B.; Peters, A.; Amann, U. Prevalence, awareness, treatment, and control of hypertension in older people: Results from the population-based KORA-age 1 study. BMC Public Health 2020, 20, 1049. [Google Scholar] [CrossRef] [PubMed]
- Rabi, D.M.; McBrien, K.A.; Sapir-Pichhadze, R.; Nakhla, M.; Ahmed, S.B.; Dumanski, S.M.; Butalia, S.; Leung, A.A.; Harris, K.C.; Cloutier, L.; et al. Hypertension Canada’s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Can. J. Cardiol. 2020, 36, 596–624. [Google Scholar] [CrossRef] [PubMed]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E., Jr.; Collins, K.J.; Dennison Himmelfarb, C.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018, 71, e13–e115, Erratum in Hypertension 2018, 71, e140–e144. [Google Scholar] [CrossRef] [PubMed]
- Lahat, A.; Shatz, Z. Telemedicine in clinical gastroenterology practice: What do patients prefer? Ther. Adv. Gastroenterol. 2021, 14, 1756284821989178. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).