Abdominal-Based Microsurgical Breast Reconstruction: How to Inset the Flap to Maximize the Aesthetic Result—A Systematic Review
Abstract
:1. Introduction
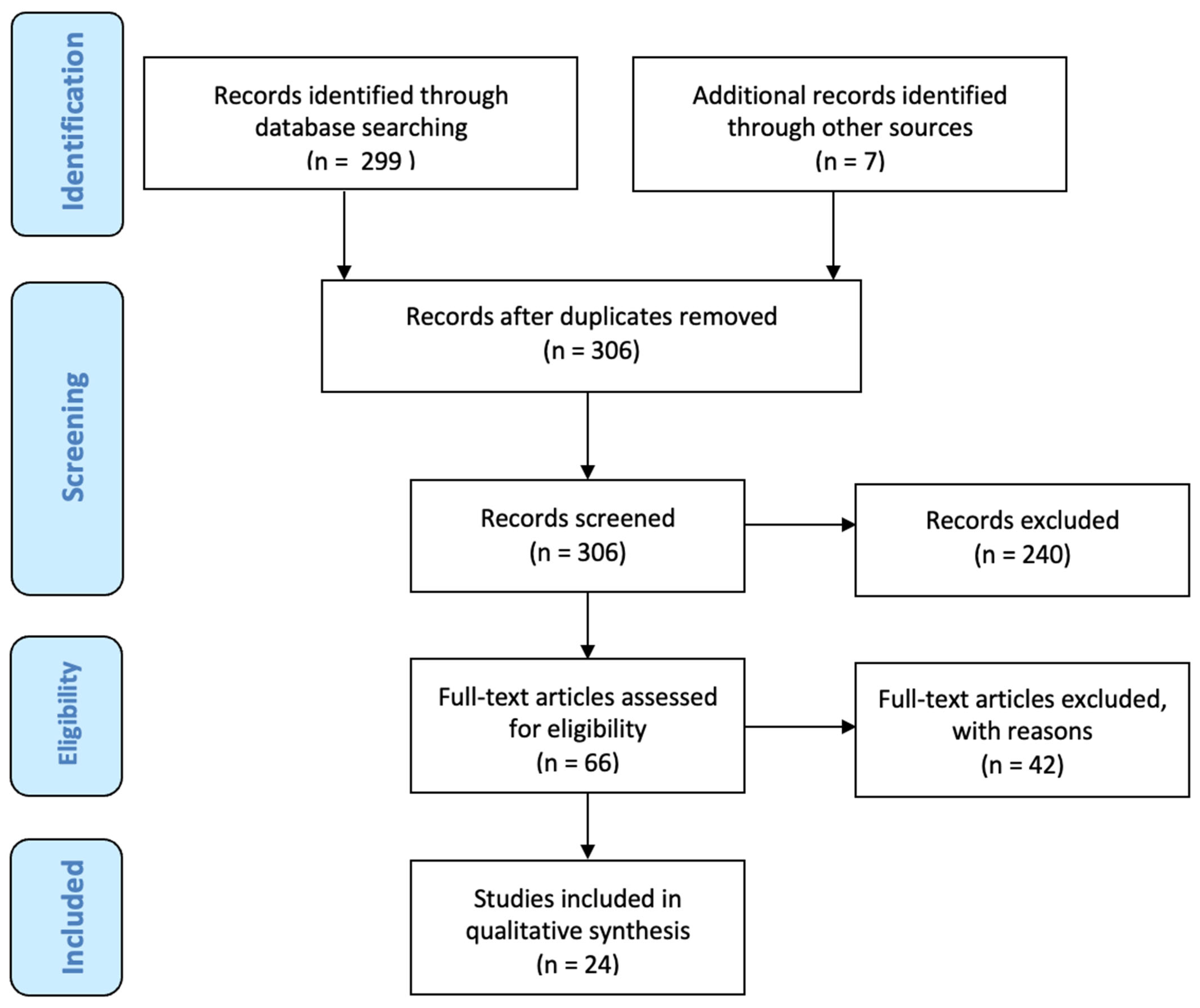
2. Materials and Methods
3. Results
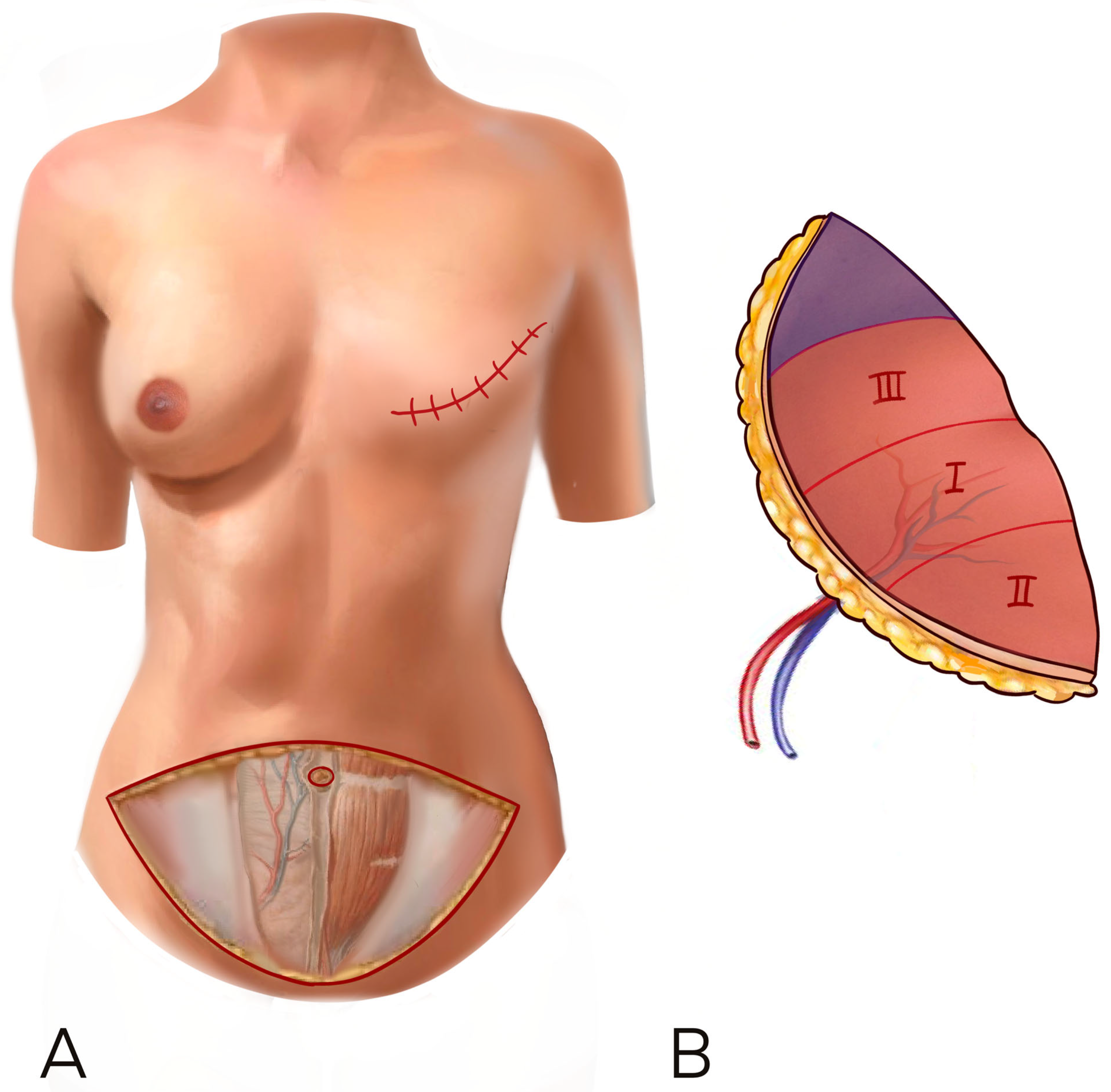
3.1. Delayed Reconstructions
3.2. Breast Key Features and Inset Rules
- breast width
- breast ptosis
- breast projection
- upper pole fullness
3.2.1. Breast Width
3.2.2. Breast Ptosis
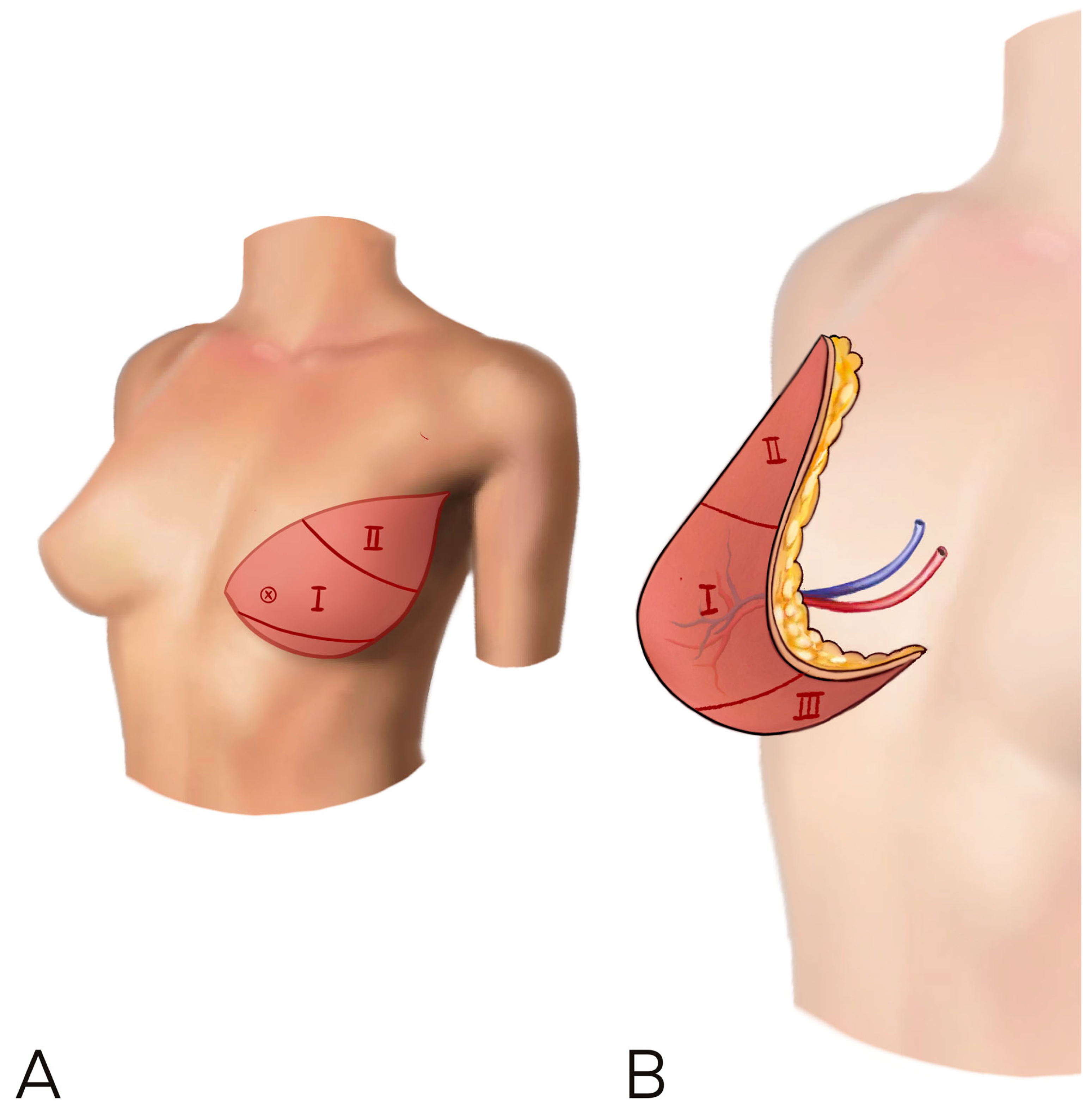
3.2.3. Breast Projection
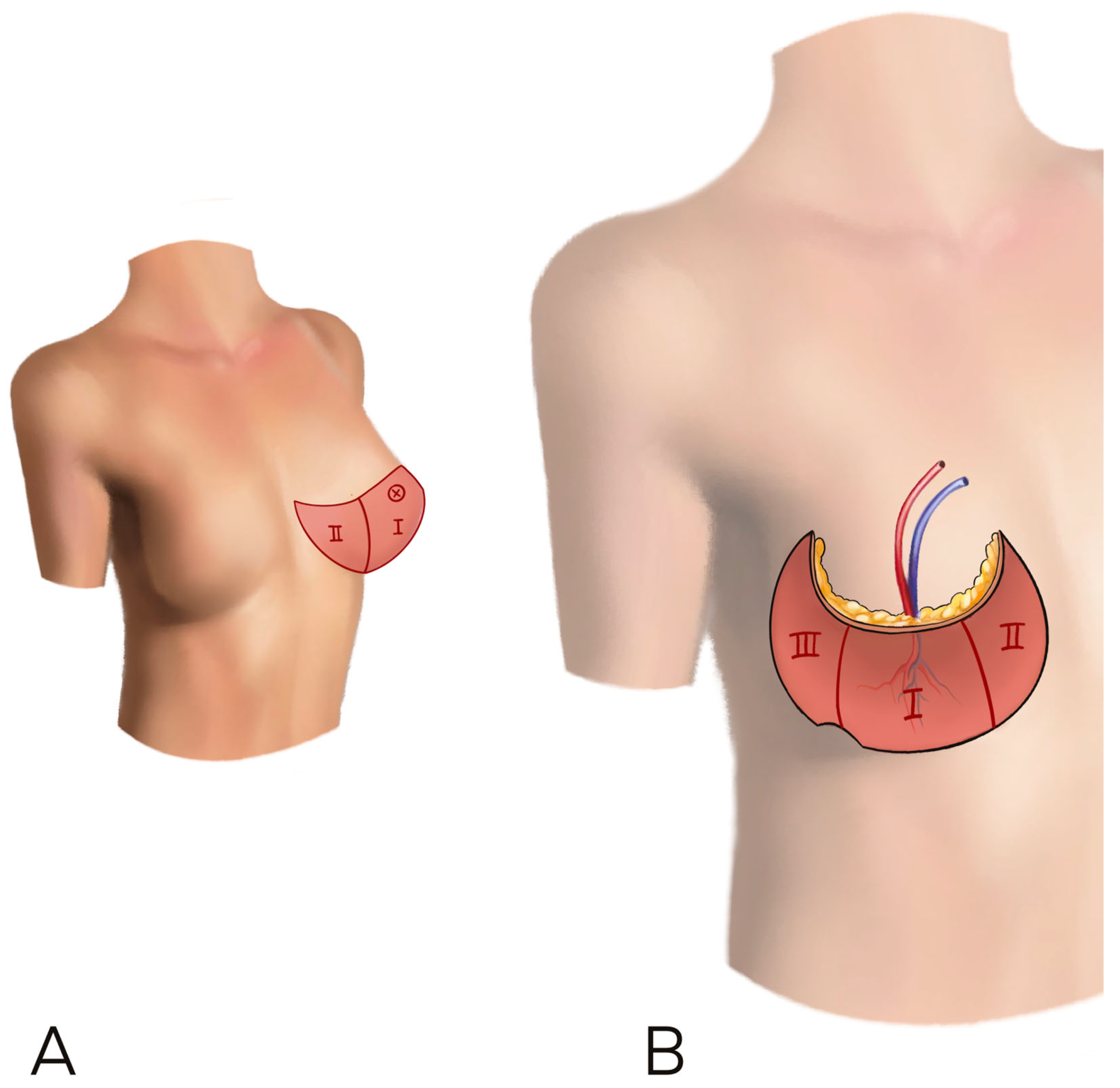
3.2.4. Upper Pole Fullness
3.3. Stacked/Conjoined Flaps
3.4. Patient Body Type
3.5. Predesigned Insetting
3.6. Complications
4. Discussion
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sadok, N.; Krabbe-Timmerman, I.S.; Buisman, N.H.; van Aalst, V.C.; de Bock, G.H.; Werker, P.M.N. Short-term Quality of Life after Autologous Compared to Alloplastic Breast Reconstruction: A Prospective Study. Plaaast Reconstr. Surg. 2023. online ahead of print. [Google Scholar] [CrossRef]
- Atamian, E.K.; Suydam, R.; Hardy, T.N.; Clappier, M.; Barnett, S.; Caulfield, D.; Jelavic, M.; Smith, M.L.; Tanna, N. Financial Implications of Enhanced Recovery After Surgery Protocols in Microsurgical Breast Reconstruction. Ann. Plast. Surg. 2023, 90, S607–S611. [Google Scholar] [CrossRef] [PubMed]
- Fracol, M.E.; Rodriguez, M.M.; Clemens, M.W. A Spectrum of Disease: Breast Implant-Associated Anaplastic Large Cell Lymphoma, Atypicals, and Other Implant Associations. Clin. Plast. Surg. 2023, 50, 249–257. [Google Scholar] [CrossRef] [PubMed]
- Martin, J.; di Summa, P.G.; Raffoul, W.; Koch, N. Breast Reconstruction: Economic Impact Swiss Health Insurance System. Medicines 2022, 9, 64. [Google Scholar] [CrossRef]
- Fertsch, S.; Munder, B.; Andree, C.; Witzel, C.; Stambera, P.; Schulz, T.; Hagouan, M.; Gruter, L.; Aufmesser, B.; Staemmler, K.; et al. Risk Factor Analysis for Flap and Donor Site Related Complications in 1274 DIEP Flaps—Retrospective Single Center Study. Chirurgia 2021, 116 (Suppl. S2), 5–15. [Google Scholar] [CrossRef]
- Patel, N.G.; Rozen, W.M.; Chow, W.T.; Chowdhry, M.; Fitzgerald O’Connor, E.; Sharma, H.; Griffiths, M.; Ramakrishnan, V.V. Stacked and bipedicled abdominal free flaps for breast reconstruction: Considerations for shaping. Gland. Surg. 2016, 5, 115–121. [Google Scholar] [PubMed]
- Blondeel, P.N.; Hijjawi, J.; Depypere, H.; Roche, N.; Van Landuyt, K. Shaping the breast in aesthetic and reconstructive breast surgery: An easy three-step principle. Part IV—Aesthetic breast surgery. Plast. Reconstr. Surg. 2009, 124, 372–382. [Google Scholar] [CrossRef]
- Chae, M.P.; Rozen, W.M.; Patel, N.G.; Hunter-Smith, D.J.; Ramakrishnan, V. Enhancing breast projection in autologous reconstruction using the St Andrew’s coning technique and 3D volumetric analysis. Gland. Surg. 2017, 6, 706–714. [Google Scholar] [CrossRef]
- Razzano, S.; Marongiu, F.; Wade, R.; Figus, A. Optimizing DIEP Flap Insetting for Immediate Unilateral Breast Reconstruction: A Prospective Cohort Study of Patient-Reported Aesthetic Outcomes. Plast. Reconstr. Surg. 2019, 143, 261e–270e. [Google Scholar] [CrossRef]
- Holm, C.; Mayr, M.; Hofter, E.; Ninkovic, M. Perfusion zones of the DIEP flap revisited: A clinical study. Plast. Reconstr. Surg. 2006, 117, 37–43. [Google Scholar] [CrossRef]
- Ali, R.S.; Garrido, A.; Ramakrishnan, V. Stacked free hemi-DIEP flaps: A method of autologous breast reconstruction in a patient with midline abdominal scarring. Br. J. Plast. Surg. 2002, 55, 351–353. [Google Scholar] [CrossRef] [PubMed]
- Pulzl, P.; Schoeller, T.; Wechselberger, G. Respecting the aesthetic unit in autologous breast reconstruction improves the outcome. Plast. Reconstr. Surg. 2006, 117, 1685–1691; discussion 1683–1692. [Google Scholar] [CrossRef] [PubMed]
- Liao, H.T.; Cheng, M.H.; Ulusal, B.G.; Wei, F.C. Deep inferior epigastric perforator flap for successful simultaneous breast and chest wall reconstruction in a Poland anomaly patient. Ann. Plast. Surg. 2005, 55, 422–426. [Google Scholar] [CrossRef]
- Cheng, M.H.; Robles, J.A.; Ulusal, B.G.; Wei, F.C. Reliability of zone IV in the deep inferior epigastric perforator flap: A single center’s experience with 74 cases. Breast 2006, 15, 158–166. [Google Scholar] [CrossRef]
- Williams, E.H.; Rosenberg, L.Z.; Kolm, P.; de la Torre, J.I.; Fix, R.J. Immediate nipple reconstruction on a free TRAM flap breast reconstruction. Plast. Reconstr. Surg. 2007, 120, 1115–1124. [Google Scholar] [CrossRef] [PubMed]
- Patel, A.J.; Kulkarni, M.; O’Broin, E.S. A TRAM flap design refinement for use in delayed breast reconstruction. J. Plast. Reconstr. Aesthet. Surg. 2009, 62, 1135–1139. [Google Scholar] [CrossRef]
- Scholz, T.; Kretsis, V.; Kobayashi, M.R.; Evans, G.R.D. Long-term outcomes after primary breast reconstruction using a vertical skin pattern for skin-sparing mastectomy. Plast Reconstr. Surg. 2008, 122, 1603–1611. [Google Scholar] [CrossRef]
- Bozikov, K.; Arnez, T.; Hertl, K.; Arnez, Z.M. Fat necrosis in free DIEAP flaps: Incidence, risk, and predictor factors. Ann. Plast. Surg. 2009, 63, 138–142. [Google Scholar] [CrossRef]
- DellaCroce, F.J.; Sullivan, S.K.; Trahan, C. Stacked deep inferior epigastric perforator flap breast reconstruction: A review of 110 flaps in 55 cases over 3 years. Plast. Reconstr. Surg. 2011, 127, 1093–1099. [Google Scholar] [CrossRef]
- Dionyssiou, D.; Demiri, E.; Tsimponis, A.; Boorman, J. Predesigned breast shaping assisted by multidetector-row computed tomographic angiography in autologous breast reconstruction. Plast. Reconstr. Surg. 2014, 133, 100e–108e. [Google Scholar] [CrossRef]
- Gravvanis, A.; Samouris, G.; Galani, E.; Tsoutsos, D. Dual plane diep flap inset: Optimizing esthetic outcome in delayed autologous breast reconstruction. Microsurgery 2015, 35, 432–440. [Google Scholar] [CrossRef]
- Uda, H.; Yoshimura, K.; Asahi, R.; Sarukawa, S.; Sunaga, A.; Kamochi, H.; Sugawara, Y. Vertically Set Sombrero-shaped Abdominal Flap for Asian Breast Reconstruction after Skin-sparing Mastectomy. Plast. Reconstr. Surg. Glob. Open 2016, 4, e1123. [Google Scholar] [CrossRef] [PubMed]
- Jeong, W.S.; Han, W.; Eom, J.S. Comparison of Aesthetic Outcomes Between Vertical and Horizontal Flap Insets in Breast Reconstruction with the TRAM or DIEP Flaps. Aesthetic Plast. Surg. 2017, 41, 19–25. [Google Scholar] [CrossRef] [PubMed]
- Gravvanis, A.; Smith, R.W. Shaping the breast in secondary microsurgical breast reconstruction: Single- vs. two-esthetic unit reconstruction. Microsurgery 2016, 30, 509–516. [Google Scholar] [CrossRef] [PubMed]
- Marquez, M.P.; Fernandez-Riera, R.; Cardona, H.V.; Flores, J.M.R. Immediate implant replacement with DIEP flap: A single-stage salvage option in failed implant-based breast reconstruction. World J. Surg. Oncol. 2018, 16, 80. [Google Scholar] [CrossRef]
- Yu, Y.H.; Ghorra, D.; Bojanic, C.; Aria, O.N.; MacLennan, L.; Malata, C.M. Orienting the superficial inferior epigastric artery (SIEA) pedicle in a stacked SIEA-deep inferior epigastric perforator free flap configuration for unilateral tertiary breast reconstruction. Arch. Plast. Surg. 2020, 47, 473–482. [Google Scholar] [CrossRef] [PubMed]
- Chang, E.I.; Chang, E.I.; Soto-Miranda, M.A.; Zhang, H.; Nosrati, N.; Ghali, S.; Chang, D.W. Evolution of Bilateral Free Flap Breast Reconstruction over 10 Years: Optimizing Outcomes and Comparison to Unilateral Reconstruction. Plast. Reconstr. Surg. 2015, 135, 946e–953e. [Google Scholar] [CrossRef]
- Suh, Y.C.; Ahn, M.R.; Kim, S.Y.; Kim, Y.J.; Lee, J.H. Superficial inferior epigastric artery-supercharged deep inferior epigastric artery perforator flap-based breast reconstruction for a thin patient: A case report. Microsurgery 2019, 39, 651–654. [Google Scholar] [CrossRef]
- Salibian, A.A.; Bekisz, J.M.; Frey, J.D.; Nolan, I.T.; Kaoutzanis, C.; Yu, J.W.; Levine, J.P.; Karp, N.S.; Choi, M.; Thanik, V.D. Comparing outcomes between stacked/conjoined and non-stacked/conjoined abdominal microvascular unilateral breast reconstruction. Microsurgery 2021, 41, 240–249. [Google Scholar] [CrossRef]
- Pompei, B.; Farhadi, J. Diep Flap Volume Augmentation: Literature Review and “Calzone” Flap Shaping Technique. J. Plast. Reconstr. Aesthet. Surg. 2020, 73, 1933–1939. [Google Scholar] [CrossRef]
- Gelati, C.; Lozano Miralles, M.E.; Morselli, P.G.; Fabbri, E.; Cipriani, R. Deep Inferior Epigastric Perforator Breast Reconstruction With Computer-Aided Design/Computer-Aided Manufacturing Sizers. Ann. Plast. Surg. 2020, 84, 24–29. [Google Scholar] [CrossRef] [PubMed]
- Blondeel, P.N.; Hijjawi, J.; Depypere, H.; Roche, N.; Van Landuyt, K. Shaping the breast in aesthetic and reconstructive breast surgery: An easy three-step principle. Plast. Reconstr. Surg. 2009, 123, 455–462. [Google Scholar] [CrossRef] [PubMed]
- Blondeel, P.N.; Hijjawi, J.; Depypere, H.; Roche, N.; Van Landuyt, K. Shaping the breast in aesthetic and reconstructive breast surgery: An easy three-step principle. Part II—Breast reconstruction after total mastectomy. Plast. Reconstr. Surg. 2009, 123, 794–805. [Google Scholar] [CrossRef] [PubMed]
- Nanhekhan, L.; Vandervoort, M. New approach to shaping a ptotic breast in secondary autologous breast reconstruction. Aesthetic Plast. Surg. 2012, 36, 1144–1150. [Google Scholar] [CrossRef]
- Di Summa, P.G.; Oranges, C.M.; Watfa, W.; Sapino, G.; Keller, N.; Tay, S.K.; Chew, B.K.; Schaefer, D.J.; Raffoul, W. Systematic review of outcomes and complications in nonimplant-based mastopexy surgery. J. Plast. Reconstr. Aesthet. Surg. 2019, 72, 243–272. [Google Scholar] [CrossRef]
- Blondeel, P. Re: Successful breast reconstruction with a perforator-to-deep inferior epigastric perforator flap. Ann. Plast. Surg. 2002, 48, 214. [Google Scholar] [CrossRef]
- Blondeel, P.N.; Boeckx, W.D. Refinements in free flap breast reconstruction: The free bilateral deep inferior epigastric perforator flap anastomosed to the internal mammary artery. Br. J. Plast. Surg. 1994, 47, 495–501. [Google Scholar] [CrossRef]
- Haddock, N.T.; Cho, M.J.; Teotia, S.S. Comparative Analysis of Single versus Stacked Free Flap Breast Reconstruction: A Single-Center Experience. Plast. Reconstr. Surg. 2019, 144, 369e–377e. [Google Scholar] [CrossRef]
- Razzano, S.; Taylor, R.; Schonauer, F.; Figus, A. How to assess the volume of a DIEP flap using a free online calculator: The DIEP V (volume) method. J. Plast. Reconstr. Aesthet. Surg. 2018, 71, 1410–1416. [Google Scholar] [CrossRef]
- Pirro, O.; Mestak, O.; Vindigni, V.; Sukop, A.; Hromadkova, V.; Nguyenova, A.; Vitova, L.; Bassetto, F. Comparison of Patient-reported Outcomes after Implant Versus Autologous Tissue Breast Reconstruction Using the BREAST-Q. Plast. Reconstr. Surg. Glob. Open 2017, 5, e1217. [Google Scholar] [CrossRef]
- Nahabedian, M.Y. Achieving ideal breast aesthetics with autologous reconstruction. Gland. Surg. 2015, 4, 134–144. [Google Scholar] [PubMed]
- Greer, M.J.; Pestana, I.A. The Lateral Breast Flap Sling: A Novel Technique for the Revision of Autologous Breast Reconstructions. Cureus 2020, 12, e10323. [Google Scholar] [CrossRef] [PubMed]
- Cogliandro, A.; Barone, M.; Tenna, S.; Morelli Coppola, M.; Persichetti, P. The Role of Lipofilling After Breast Reconstruction: Evaluation of Outcomes and Patient Satisfaction with BREAST-Q. Aesthetic Plast. Surg. 2017, 41, 1325–1331. [Google Scholar] [CrossRef] [PubMed]
- Watfa, W.; Zaugg, P.; Baudoin, J.; Bramhall, R.J.; Raffoul, W.; di Summa, P.G. Dermal Triangular Flaps to Prevent Pseudoptosis in Mastopexy Surgery: The Hammock Technique. Plast. Reconstr. Surg. Glob. Open 2019, 7, e2473. [Google Scholar] [CrossRef]
- Mortada, H.; AlNojaidi, T.F.; AlRabah, R.; Almohammadi, Y.; AlKhashan, R.; Aljaaly, H. Morbidity of the Donor Site and Complication Rates of Breast Reconstruction with Autologous Abdominal Flaps: A Systematic Review and Meta-Analysis. Breast J. 2022, 2022, 7857158. [Google Scholar] [CrossRef]
- Xu, F.; Sun, H.; Zhang, C.; Jiang, H.; Guan, S.; Wang, X.; Wen, B.; Li, J.; Li, X.; Geng, C.; et al. Comparison of surgical complication between immediate implant and autologous breast reconstruction after mastectomy: A multicenter study of 426 cases. J. Surg. Oncol. 2018, 118, 953–958. [Google Scholar] [CrossRef]

| Author (First Listed), Year | Study Design | No. of Patients | Geographic Location | Age of Patients (y), | Delayed-Immed | Type of Flap | Flap Insetting | Recipient Vessels | Indications Proposed by the Authors | General Outcome Including Satisfaction |
|---|---|---|---|---|---|---|---|---|---|---|
| Blondeel et al., 1994 [5] | Case Report | 1 patient, 2 stacked flaps | Belgium | 37 | 1 delayed | bipedicled “stacked” DIEP | IMA | Midline abdominal scar in patient | good shape, size and projection | |
| Garrido and Ramakrishnan 2002 [11] | Case Report | 1 patient, 2 stacked flaps | UK | 69 | 1 immediate | Stacked hemi-DIEPs | Second flap on top of the first totally buried flap. Fixation with absorbable sutures. | TDA and intraflap | Midline abdominal scar in patients with a D cup or more | Excellent cosmetic outcome and final volume. Microsurgical complexity. Serial anastomoses curb the necessity of monitoring the buried flap |
| Pülzl et al., 2005 [12] | Retrospective study | 12 patients, 12 flaps | Austria | 51 | 12 delayed | MS-TRAM 6 DIEP 1 SIEA flaps | Deepithelialized tissue from scar to IMF. Flap instead of the IMF. Ptosis adjusted by insetting a lower or greater amount of flap skin. Rest of flap buried under the mastectomy flap | IMA | All secondary reconstructions, including contralateral moderate ptosis | 10 good, 2 fair aesthetic outcomes (evaluation by 2 independent surgeons) |
| Liao et al., 2005 [13] | Case Report | 1 patient, 1 flap | Taiwan | 52 | 1 delayed | DIEP flap | Flap turned 180 degrees, with the cranial part facing the new IMF. Cranial part of the flap is undermined. Skin paddle relocated superiorly to shift the NAC inferiorly. | IMA | Poland Syndrome, types B and D (chest depression) | Satisfactory aspect recreating lat axillary line and IMF |
| Cheng MH et al., 2006 [14] | Retrospective study | 73 patients, 74 flaps | Taiwan | 44.2 | 25 immediate, 49 delayed | DIEP (with zone IV) | Downward inset with croissant shape: the cephalic border of the flap points downward, pointing to the inframammary fold, with the umbilical located on the lateral end of the IMF. Zone IV (never discharged except for one case) located in the superior-lateral area | IMA 69; TDA 5 | Thin patients or patients with controlateral breast pendulus and large breasts (with no desire of breast reduction) | Inclusion of zone IV is highly reliable and provides superior aesthetic outcomes and high satisfaction |
| Williams et al., 2008 [15] | Retrospective study | 10 | USA | 53.7 years (range, 44.1–61.4) | 10 immediate 2 delayed | free TRAM with immediate nipple reconstruction | Inset with a wrapping flap into the cone, umbilical downwards/lateral, zone III (according to Harp) in the axilla. DIEP inset oblique center of cone (most projected part) will be used for nipple recon bilobed with fishtail flap | IMA | Spares an additional surgery for nipple recon (minimizing the number of procedures,) | No difference in subjective cosmetic ratings between delayed and immediate NAC reconstruction |
| Patel et al., 2008 [16] | Retrospective study | 21 | UK | N/A | Delayed | Free TRAM | Pre-design the flap using a template created from the opposite breast. Triangular caudally-based mastectomy flap, the cranial skin of the DIEP is sutured to the triangle | IMA | Large ptotic breasts, natura Minimize abdominal wound morbidity (less vertical height) | without the need to raise a very large abdominal flap |
| Scholz T et al., 2008 [17] | Retrospective study | 72 patients, 106 flaps | USA | 51.5 | Immediate | Free TRAM (94), DIEP (12) | Insetting the flap into a vertical skin pattern of skin sparing-mastectomy. All flap is di-epithelized except for a monitor on the neo-areola | IMA | Stage 0, I, II of AJCC Cancer Staging | Improvement of the aesthetic outcome without compromising oncologic safety Elimination of the disharmony between skin flap and breast volume in the vertical direction while respecting the inframammary crease. Produces a youthful, symmetrical conical breast shape with medial fullness |
| Bozikov K et al., 2009 [18] | Retrospective study, Single surgeon | 100 patients, 100 flaps | Slovenia | NA | 57 Immediate, 43 Delayed | DIEP based on contralateral deep inferior epigastric vessels (from 1 to 4 perforators) | Horizontal straight inset: the umbilical border of the flap was positioned at the cranial part of the chest defect, zone III being inset medially and zone II laterally. Entire zone IV discarded (Hartrampf’s classification) | IMA | Harvesting flap on multiple perforators reduces flap fat necrosis. BMI> or = 30 is a risk factor for fat necrosis. Flap zone III fat necrosis related to harvesting on a single lateral row perforator (and vice versa, zone II-medial row) | 94% flap success |
| DellaCroce et al., 2010 [19] | Retrospective study | 55 patients, 110 flaps | USA | 48 | 27 immediate 19 delayed | 55 bipedicled stacked DIEPs | Stacked flap in series. Flap 1 connects to IMAV, and flap 2 is connected to flap 1 by intra-flap “chain” anastomosis through a branch. Primary flap is kept outside, and flap 2 is buried. Flaps are generally separated, especially in delayed, to avoid a squared-off lower pole | IMA | Patients where single hemi-abdomen is bw 1/3 and ½ of desired final breast volume, need for zone IV | Superlative aesthetic outcomes with high patient satisfaction |
| Dionyssiou et al., 2014 [20] | Case Report | 1 | UK | 52 | 1 delayed | DIEP flap | Pre- or post-operative mirroring of the opposite breast template performed, and the template is transposed over the abdomen and centralized around the selected perforators according to CT scan + angiography | IMA | (1) operative time spent for shaping and insetting is significantly reduced, (2) early excision of the unnecessary parts of the abdominal flap avoids the intraoperative and postoperative flap congestion , (3) decreasing the overall operative time reduces complications , and (4) the immediately produced breast symmetry significantly reduces the need for secondary symmetrization operations. | Group A: very good and good = 53.3% Group B: very good and good = 88.8% |
| Gravanis et al., 2015 [21] | Retrospective study | 50 (Group a = 25; Group b = 25) | Greece | Group A: 41.1 +/− 1.5 B: 41.8 +/− 1.1 | Delayed | DIEP | (a) Single Plane: Only upper pole of DIEP is de-epitheliazed. Insetting above the muscle, and the lower part of mastectomy skin is de-epeithelized. Three key sutures (upper-lateral, midclavicular, and lower-medial) Dual Plane (b) (upper part of flap is de-epitheized under the pec muscle) | IMA | Delayed Unilateral reconstruction Prevents ptosis Increases upper pole fullness | Dual plane group achieved a significantly higher score for a non-disruptive superior scar and non-disruptive superior mastectomy skin (Less scar/diep demarcation line) The outline of the breast is smooth and natural in appearance. Overall breast appearance,” the dual plane reconstruction group scored 86 +/− 1.5, and the single plane reconstructions scored 72.2 +/− 1.9. This difference was extremely statistically significant (p < 0.0001). |
| Uda et al., 2016 [22] | Retrospective study | 62 patients | Japan | 49 | Immediate (only Skin sparing mastectomy) | 35 DIEP and 27 bipedicled DIEP | Flap placed 90 degrees medially and mounted vertically. The thickest portion of the flap around the umbilicus is set at the nipple and areolar region, and the ipsilateral lateral portion of the flap fill the defect of décolleté and axillary tail. The contralateral portion of the flap is folded inward to create lower pole fullness. If double-pedicled flaps: intraflap crossover anastomosis before anterograde end-to-end anastomosis OR anterograde and retrograde double end-to-end anastomosis. | IMA | Slender Asian patients: vertical flap setting with S-flap (medial fan-shaped adipose flap) West patients: C-flap | the vertical flap setting imposes the use of nearly the entirety of zone II and sometimes zone IV and the flap must often be elevated as a double-pedicled flap Good satisfaction comparative to conventional flap only for morbidity donor site |
| Patel et al., 2016 [6] | Retrospective study | 25 patients | USA | 48 | Immediate | Bipedicled (14) and Stacked (11) DIEP | Folded: flap left undivided but folded at the midline (symmetrically) or off midline (asymmetrically) Divided: abdominal pannus is divided and skin paddle layered on top of each other Coned: cranial margin of abdominal tissue sutured togheter Divided and folded: abdominal pannus divided and each flap folded | TDA 67%, IMA 32%, | Folded: tall narrow breast, more volume in the inferior pole Divided: if set horizontally -> increased breast base Coned: projected breast with large inferior pole Divided and coned: moderate projection | Stacked and bipedicled flaps are more demanding but less fat necrosis is seen |
| Jeong et al., 2016 [23] | Retrospective study | 274 patients | South Korea | 45 | 250 immediate, 24 delayed | DIEP | Horizontal inset: umbilical site flap directed downwards, zone II medial Vertical inset: umbilical side lateral, zone II lowest part of the breast | IMA and TDA | Horizontal inset: more volume at the lower pole Vertical inset: balanced volume distribution, | Higher symmetry in vertical inset, lateral excess in horizontal inset with volume deficiency in upper pole |
| Gravannis et al., 2016 [24] | Prospective study, single surgeon | 42 patients | Greece | 42 | Delayed, RT | DIEP | Dual plane: the flap in inset over the di-epithelized mastectomy lower flap and at the upper pole under a myocutaneous flap including the pec maj. PDS sutures (parasternal, midline and ant axil line) between flap scarpa fascia and undersurface of pec major | IMA | Replacement of poor quality mastectomy skin, optimal IMF position, reduced skin problems at the upper mastectomy flap | Fullness upper pole and minimal ptosis overtime. Improved social and sexual life, high satisfaction for aesthetic result |
| De La Parra Marquez. 2018 [25] | Retrospective study | 8 | Mexico | Mean 45 years old, (42–50 years; SD = 3.30) | Delayed (after failed immediate implant) (Immediate tertiary DIEP) | Deepithelialized DIEP | Deepithelialized flap is placed in the same pocket where the previous implant was; no new pocket or change of plane | IMA | Salvage for failed implant based reconstruction | Results in a soft and natural final breast shape. |
| Yu et al., 2020 [26] | Case Report | 1 patient, 2 flaps | UK | 47 | 1 delayed (tertiary) | DIEP + SIEA stacked | Both flaps vertically oriented (lat edge cranial) Controlat DIEP outside (antegrade micro on IMA/V), buried ipsilateral SIEA with dermis facing down to allow reaching IMA/V (retrograde) | IMA (anterograde and retrograde) | Pleasant result due to ideal flap orientation (both flaps with lateral part cranial and bulgy part in the lower pole) | |
| Chang et al., 2016 [27] | Retrospective study | 57 pt, 114 flaps | USA | 49 | 21 immediate, 36 delayed | Dual pedicle flap (TRAM 42, DIEP 59, SIEA 12) | Lateral ends of the flap folded onto themselves, no rotation, horizontal | IMA antegrade and retrograde removing the rib, TDA (8) | Dual pedicle flap increases confort with free tissue transfer and high success rate | Valuable option when more volume is needed |
| Suh et al., 2019 [28] | Case report | 1 | South Korea | 48 | immediate | DIEP + SIEA contralat stacked | elliptical-shaped flap was inset with a 90° counterclockwise rotation, and the lower one-third of the flap was folded to create a projection | DIEA to IMA, SIEA to TDA | Large and ptotic breast in thin patient | Avoid bilateral abdominal fascia incision. SIEA short pedicle. LD flap can still be performed as salvage option. |
| Razzano et al., 2019 [9] | Prospective study | 70 | UK | 55 | 70 immediate | DIEP (5 bipedicled) | Depending on contralat breast: If ptotic: vertical inset folding the inferior portion of the flap with 90° rotation If projected: horizontal inset, 0° rotation if ipsilateral DIEP, 180° rotation if contralateral, with lateral and inferior folding Fat abdomen: horizontal inset Slim abdomen: vertical inset | IMA and intraflap anastomosis | Flap inset changes depending on the controlat breast, perf position and type of abdomen | 180-degree rotation provides the best possible projection, with the position of the umbilical vertical scar placed inferiorly 90-degree flap counterclockwise rotation allows the pedicle to be placed in a more medial position. When the breast base is large or projection and fullness of the upper pole are needed, rotate the flap 0 or 180 degrees, depending on the position of the perforators. When 90 degrees of rotation is chosen, better ptosis could be achieved by deepithelializing and folding the inferior marg |
| Salibian et al., 2020 [29] | Retrospective study | 182 patients | USA | 52 | 105 immediate, 77 delayed | DIEP stacked/conjoined (36), non-stacked (146) | In stacked: hemiflaps in the inferior and superior breast pole In conjoined: coning the flap while maintaining the base, flap rotation based on native footprint | IMA | Conjoined flap in lower BMI and prior irradiation | Patient with stacked flaps lower contralaterl simmetrisation |
| Pompei et al., 2020 [30] | Review + retrospective | 28 flaps | UK | 50 | Immediate | Stacked DIEP flap | Calzone technique: flap folded in two in the back table on the horizontal axis, posterior side de-epitelized, other side partially or totally de-epit depending on skin envelop. The folded part stays inferior. | IMA antegrade and retrograde | Flap augmentation technique, enhancing lower pole projection | |
| Gelati et al., 2020 [31] | Retrospective study | 24 pt with DIEP sizers vs. 24 | Italy | 50 | 21 Delayed, 3 immediate | DIEP | Virtual model using Geomagic Xsoftware to construct the DIEP sizers. the abdominal flap is located inside the DIEP sizer. The flap is fixed onto the thorax skin, the anastomoses are made, and afterwards, proceed to modeling by trimming the flap in the DIEP sizer | IMA | 10 different DIEP sizers were created based on the anthropometric measures of 15 patients who previously underwent DIEP reconstruction. Ideally, the contralat breast can be used as a 3D model to build the sizer. | Significative OP time difference between groups (faster with sizers). |
| Author | Number of Patients | Number of Flaps | Type | Complication | Complication |
|---|---|---|---|---|---|
| Breast | Donor Site | ||||
| Blondeel et al., 1994 [5] | 1 | 2 | Bipediceld stacked DIEP | 0 | - |
| Garrido and Ramakrishnan 2002 [11] | 1 | 2 | Stacked hemi-DIEPs | 1 venous congestion solved | - |
| Pülzl et al., 2005 [12] | 12 | 12 | 5 MS-TRAM,6 DIEP, 1 SIEA | 1 hematoma | - |
| Liao et al., 2005 [13] | 1 | 1 | DIEP flap | 0 | - |
| Cheng MH et al., 2006 [14] | 73 | 74 | DIEP flap | 2 partial flap loss | - |
| 10 Liponecrosis | |||||
| 1 venous congestion solved | |||||
| Williams et al., 2008 [15] | 10 | 12 | Free TRAM | 0 | - |
| Patel et al., 2008 [16] | 21 | 21 | Free TRAM | 0 | 3 cases of minor abdominal wound infection |
| Santanelli et al., 2008 | 4 | 4 | Free vertical DIEP flap | 0 | - |
| Scholz T et al., 2008 [17] | 72 | 106 (34 BILATERAL) | Free TRAM (94), DIEP (12) | 4 fat necrosis | 3 Fat necrosis |
| 1 flap site infection | 2 Wound dehiscence | ||||
| 1 venous occlusion requiring revision | 3 Wound infection | ||||
| 1 Seroma | |||||
| Bozikov K et al., 2009 [18] | 100 | 100 | DIEP | 6 total flap Loss | - |
| 37 liponecrosis | |||||
| 20 anastomosis revision | |||||
| DellaCroce et al., 2010 [19] | 55 | 110 | 55 bipedicled stacked DIEPs | 3 hematoma including 1 requiring surgical evacuation | - |
| Dionyssiou et al., 2014 [20] | 32 | 32 | MS-TRAM(7) DIEP(25) | 3 venous thrombosis (all in DIEP) | - |
| Gravanis et al., 2015 [21] | 50 | 50 | DIEP | none | - |
| Uda et al., 2016 [22] | 62 | 89 | 35 DIEP and 27 bipedicled DIEP | 2 total flap loss | 2 abdominal wound healing |
| 3 partial flap loss | 14 abdominal seroma | ||||
| 8 partial fat necrosis | 5 bulging | ||||
| 3 hematomas | |||||
| 3 infections | |||||
| 2 mastectomy flap necrosis | |||||
| Patel et al., 2016 [6] | 25 | 50 | Bipedicled (14) and Stacked (11) DIEP | 1 Flap loss | - |
| 2 Hematoma | |||||
| Jeong et al., 2016 [23] | 274 | 274 | DIEP and MS-TRAM | NR | - |
| Gravannis et al., 2016 [24] | 42 | 42 | DIEP | 0 | - |
| De La Parra Marquez. 2018 [25] | 8 | 10 | DIEP | 3 seroma | - |
| Yu et al., 2020 [26] | 1 | 2 | DIEP + SIEA stacked | 0 | - |
| Chang et al., 2016 [27] | 57 | 103 | Bipedicled flap (TRAM, DIEP, SIEA) | 4 Fat necrosis (all pedicled TRAM) | 2 seroma |
| (46 dual) | 1 Seroma | 2 Abdominal bulge (from pedicled TRAM) | |||
| 11 p-TRAM + freeflap | 1 Hematoma | 1 infection | |||
| 6 Wound healing | 2 wound healing | ||||
| 1 Partial flap loss (dual pedicle) | |||||
| 3 Infection | |||||
| Suh et al., 2019 [28] | 1 | 2 | DIEP + SIEA contralat | 0 | - |
| Razzano et al., 2019 [9] | 70 | 75 | DIEP (5 bipedicled) | 4 Fat necrosis | - |
| 14 Revision surgery | |||||
| Salibian et al., 2020 [29] | 182 | 218 | DIEP and MS-TRAM stacked/conjoined (36), non-stacked (146) | 3 Fat necrosis (8%) in conjoined | - |
| 37 fat necrosis (25%) in non-conjoined | |||||
| Pompei et al., 2020 [30] | 28 | 56 | Bipedicled DIEP | 0 flap necrosis | - |
| 4 fat necrosis | |||||
| Gelati et al., 2020 [31] | 48 | 59 | DIEP | 0 | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sapino, G.; Tay, S.K.; Maruccia, M.; Nanhekhan, L.; Watfa, W.; Mantovani, G.P.; Guillier, D.; Tedeschi, P.; Bramhall, R.; Di Summa, P.G. Abdominal-Based Microsurgical Breast Reconstruction: How to Inset the Flap to Maximize the Aesthetic Result—A Systematic Review. J. Clin. Med. 2023, 12, 6135. https://doi.org/10.3390/jcm12196135
Sapino G, Tay SK, Maruccia M, Nanhekhan L, Watfa W, Mantovani GP, Guillier D, Tedeschi P, Bramhall R, Di Summa PG. Abdominal-Based Microsurgical Breast Reconstruction: How to Inset the Flap to Maximize the Aesthetic Result—A Systematic Review. Journal of Clinical Medicine. 2023; 12(19):6135. https://doi.org/10.3390/jcm12196135
Chicago/Turabian StyleSapino, Gianluca, Sherilyn K. Tay, Michele Maruccia, Lloyd Nanhekhan, William Watfa, Gian Piero Mantovani, David Guillier, Pasquale Tedeschi, Russell Bramhall, and Pietro Giovanni Di Summa. 2023. "Abdominal-Based Microsurgical Breast Reconstruction: How to Inset the Flap to Maximize the Aesthetic Result—A Systematic Review" Journal of Clinical Medicine 12, no. 19: 6135. https://doi.org/10.3390/jcm12196135
APA StyleSapino, G., Tay, S. K., Maruccia, M., Nanhekhan, L., Watfa, W., Mantovani, G. P., Guillier, D., Tedeschi, P., Bramhall, R., & Di Summa, P. G. (2023). Abdominal-Based Microsurgical Breast Reconstruction: How to Inset the Flap to Maximize the Aesthetic Result—A Systematic Review. Journal of Clinical Medicine, 12(19), 6135. https://doi.org/10.3390/jcm12196135







