Abstract
Post-partum, women can suffer from urinary and faecal incontinence. It is important to assess interventions to prevent this problem. Cochrane systematic reviews summarize the data available from systematic reviews of randomized trials assessing interventions. We conducted an umbrella overview of Cochrane systematic reviews encompassing antenatal, intrapartum and postpartum interventions for preventing postpartum urinary and faecal incontinence. We searched the Cochrane Database of Systematic Reviews on the 9 May 2023. Results: Our search identified nine Cochrane reviews providing results. Data for urinary and faecal incontinence were available from 77 (72%) trials and included 51,113 women. The reviews assessed antenatal digital perineal massage, pelvic floor muscle training, techniques for repairing anal sphincter tears, routine use of episiotomy, use of endoanal ultrasound prior to repairing perineal tears, caesarean versus vaginal delivery (overall, for breech and for twins), and vaginal delivery with forceps or vacuum. Only the use of a vacuum instead of forceps if an assisted vaginal delivery is needed, the use of an endo-anal ultrasound prior to repairing perineal tears and postpartum pelvic floor muscle training suggest a reduction in postpartum incontinence. Due to the small number of relevant reviews, a consequence of the relatively small number of primary studies, the effect of almost all the tested interventions was found to be imprecise.
1. Introduction
What Is the Issue
The prevalence of stress urinary incontinence in the first three months following delivery is approximately 8% for the primiparous patients and about 20% for the multiparous women [1].
Faecal incontinence at three months postpartum may be 19% to 46% for flatus and 2.4% to 8.0% for the involuntary loss of formed stool [2]. In the longer term, these rates seem to persist, with about 31% of primiparous women reporting involuntary loss of flatus at six and twelve years after delivery and 9% to 12% reporting loss of formed stool [3]. One systematic review suggested that the etiological factor most strongly associated with postpartum faecal incontinence is a third- or fourth-degree rupture of the external anal sphincter [4].
Managing incontinence after pregnancy is not only important for the individuals themselves but can also have considerable costs to individuals and for healthcare systems.
Due to the fact that there are various risk factors for urinary or faecal incontinence, different interventions can help to prevent incontinence in postpartum. This summary provides an overview of the findings from Cochrane reviews on interventions during pregnancy and childbirth aimed at preventing urinary or faecal incontinence in the postpartum period.
2. Materials and Methods
2.1. Objectives
The aim of this summary was to provide an overview of the evidence found in Cochrane reviews concerning the impact of interventions during pregnancy, labour and the postpartum period on the prevention of urinary and faecal incontinence.
2.2. Criteria for Inclusion
We incorporated Cochrane reviews that examined antenatal, intrapartum or postpartum interventions with outcomes reporting on postpartum urinary or faecal incontinence. The postpartum period under consideration was immediately after the delivery and up to 3 years.
We listed the reviews that specified urinary or faecal incontinence as an outcome but had no data reported (see Appendix B: Reviews awaiting further classification). These reviews will be taken into account in future updates of the overview if additional data becomes available.
2.3. Participants
We examined reviews that evaluated interventions for pregnant women during the antenatal (that is to say during the pregnancy), childbirth or postpartum (up to 3 years after the delivery) phases.
2.4. Interventions
We examined all interventions employed during the antenatal, peripartum and postpartum period compared with an alternative intervention.
2.5. Outcomes of Interest
Urinary and faecal incontinence were the main outcomes. When urinary and faecal incontinence were assessed after more than one period of time, the last assessment was considered.
2.6. Search Strategy
We conducted a search in the Cochrane Database of Systematic Reviews, employing the terms “incontinence or perineum or episiotomy” AND “pregnancy or birth or delivery or partum or labour or natal” in the title, abstract or keywords. Word variations have been searched (last searched on 9 May 2023). We conducted our search with “all text”, without imposing restrictions on “title, abstract, or keywords”. We imposed no limitations regarding language or publication date, and we did not explore any additional databases.
2.7. Data Collection and Analysis
2.7.1. Selection of Reviews
Two overview authors independently assessed all potential reviews we identified. We resolved any disagreement through discussion, or if required, we consulted a third author.
2.7.2. Data Extraction and Management
Two authors independently extracted data from the reviews using a pre-defined data extraction form. We resolved discrepancies through discussion.
We extracted information on the following:
Review characteristics:
- review title and authors;
- date that the review was last assessed as up-to-date;
- number of included trials;
- number of participants in the trials and their characteristics;
- quality of the included trials (as reported by the review authors);
- interventions pertinent to this overview;
- all predetermined outcomes pertinent to this overview.
Statistical summaries:
- number of studies and participants contributing data relevant to this overview;
- the summary intervention effects: risk ratios (RR) or odds ratios (OR) with 95% confidence intervals (CI);
- data needed to evaluate the quality of evidence regarding the intervention’s impact.
2.7.3. Assessment of Methodological Quality of Included Reviews
Quality of Included Reviews
Two overview authors independently assessed the quality of the included reviews; another overview author verified this assessment. We resolved differences through discussion.
Methodological Quality
We assessed the methodological quality of each review using the AMSTAR 2 (A Measurement Tool to Assess Reviews) tool. AMSTAR 2 evaluates the methods used and assesses the extent to which review methods exhibit impartiality. The criteria are assessed as either yes, no, partially yes, or not applicable. These criteria are summarized in Appendix C.
A review that has all 16 criteria was considered of high quality. The ratings for overall confidence in the results of the reviews are the following:
- High
No or one non-critical weakness: the systematic review provides an accurate and comprehensive summary of the results;
- Moderate
More than one non-critical weakness: the systematic review has more than one weakness but no critical flaws. It may provide an accurate summary of the results;
- Low
One critical flaw with or without non-critical weaknesses: the review has a critical flaw and may not provide an accurate and comprehensive summary;
- Critically low
More than one critical flaw with or without non-critical weaknesses: the review has more than one critical flaw and should not be relied on to provide an accurate and comprehensive summary of the available studies.
Risk of Bias
To assess the systematic reviews, we used the ROBIS (Risk OF Bias In Systematic reviews) tool. It considers four domains:
- Study eligibility criteria;
- Identification and selection of studies;
- Data collection and study appraisal;
- Synthesis and findings.
Once the assessors have appraised these queries (low, high or unclear), they weigh the review’s collective risk of bias.
Quality of Included Studies within Reviews
We did not assess the quality of included studies within reviews but reported study quality according to the review authors’ assessment.
Quality of Evidence in Included Reviews
We evaluated the robustness of evidence pertaining to our key outcome (urinary and faecal incontinence) using the GRADE approach. We reported the quality of evidence based on the assessments made by the researchers conducting the reviews, using ‘Summary of findings’ tables when available. The GRADE system examines the following aspects:
- Study limitations: internal validity of the evidence;
- Inconsistency: discrepancy or fluctuation in the effect measurements across studies;
- Indirectness: extent of disparities among populations;
- Imprecision (random error): the level of confidence in the effect estimate to make informed decisions;
- Publication bias: the degree to which studies with certain results are selectively published.
The GRADE system scores the quality of the evidence as follows:
- High: additional research is highly improbable to alter our level of confidence in the effect estimate;
- Moderate: additional studies are likely to substantially influence our level of confidence in the effect estimate and could potentially lead to revisions in the estimate;
- Low: further research is highly likely to significantly impact our confidence in the effect estimate and is likely to change the estimate;
- Very low: the effect estimate is highly uncertain.
Data Synthesis
- We summarized the main results of the included reviews by organizing by intervention topic.
- Effective interventions: the review provided strong evidence supporting their effectiveness;
- Potentially effective interventions: the review provided reasonable evidence supporting their effectiveness;
- Ineffective interventions: the review provided strong evidence showing they are not effective;
- Probably ineffective interventions: the review provided reasonable evidence suggesting they are not effective;
- No conclusion possible: the review had limited or very uncertain evidence.
We determined the category for each intervention by assessing the quality of evidence pertaining to the management of urinary or faecal incontinence.
3. Results
Our search of the Cochrane Database of Systematic Reviews identified 72 reviews that could be potentially relevant.
After reviewing the titles and abstracts, we eliminated 26 reviews and conducted an in-depth analysis of 46 protocols and reviews by examining their full texts.
We excluded 28 reviews because they did not include urinary or faecal incontinence as an outcome (Table 1: Characteristics of excluded reviews).

Table 1.
Characteristics of excluded reviews.
We enumerated 13 reviews that mentioned urinary or faecal incontinence as an outcome, but the trials included in these reviews did not provide any data. We will consider these reviews for possible incorporation in future revisions of the overview if additional data becomes available (see Appendix A: reviews awaiting further classification).
Two reviews, that specify urinary or faecal incontinence as outcomes, are currently awaiting classification because they have not yet identified eligible trials (Appendix B).
Nine reviews were incorporated into this overview.
See Figure 1. Review flow diagram.
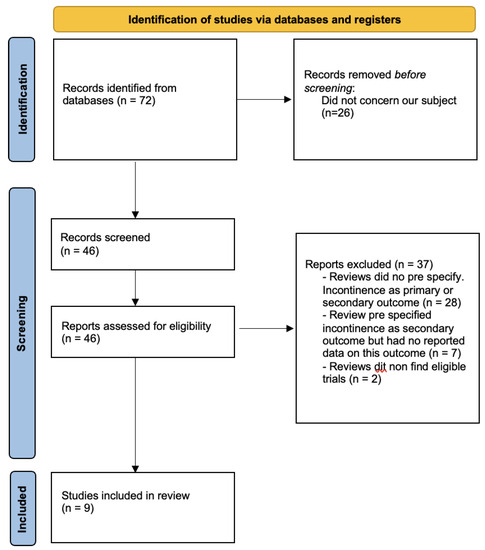
Figure 1.
Review flow diagram.
Description of included reviews.
About the nine included reviews:
- Three evaluated vaginal delivery versus caesarean delivery:
- ○
- In a global population of pregnant women [5];
- ○
- In women with breech presentation [6];
- ○
- In women with twin pregnancy [7].
- One compared instruments (forceps and vacuum) for assisted delivery [8].
- One evaluated the effects of antenatal perineal massage [9].
- One evaluated the effects of antenatal or postnatal pelvic floor muscle training [10].
- One compared performing episiotomy only if needed versus routine episiotomy [11].
- Two evaluated the repair of perineal tears:
- ○
- One compared the use of endoanal ultrasound prior to repairing perineal tears versus routine care [12];
- ○
- One compared two repairing techniques for obstetrics anal sphincter injuries: overlap versus end-to-end [13].
The count of randomized controlled trials (RCT) in the 9 reviews varied from 1 [5,12] to 46 [10]. One review included twenty non-randomized but controlled studies [5].
The number of women in each study varied, ranging from 588 [13] to 31,698 [5]. In the complete count, we had 127 trials involving over 64,401 women.
The reviews conducted searches at different times, spanning from July 2009 to August 2019. See Table 2, characteristics of included reviews.

Table 2.
Characteristics of included reviews.
3.1. Methodological Quality of Included Reviews
According to AMSTAR criteria:
- All reviews indicated the components of PICO;
- All reviews predetermined their study design;
- All reviews pre-specified which study design will be included, but only four explain why they choose this design;
- All reviews used a comprehensive search strategy;
- All reviews reported that study selection and data extraction were conducted independently by different people;
- All reviews presented lists of studies that were excluded;
- All reviews provided detailed characteristics of the studies that were included;
- All reviews used an appropriate and satisfactory method for evaluating the risk of bias in the included studies;
- Six reviews included the sources of funding for the studies [6,7,10,11,12,13];
- Eight reviews used appropriate methods for the statistical combination of results and assessment of the potential impact of risk of bias on the results of the meta-analysis. The last review conducted no meta-analysis because only one trial was included [12];
- All the reviews took into account the risk of bias in individual studies when interpreting the results;
- All the reviews provided a satisfactory explanation for the heterogeneity observed in the results;
- None of the reviews carried out an adequate investigation of publication bias;
- Only one review did not report any potential sources of conflict of interest [11].
See Table 3: AMSTAR assessments for included reviews, for further details.

Table 3.
AMSTAR assessment for included reviews.
With the ROBIS tool, it was determined that all reviews exhibited a low risk of bias. See Table 4 ROBIS assessments for included reviews, for further details.

Table 4.
ROBIS assessment.
3.2. Effects of Interventions
Below, we have provided a summary of the main findings from the reviews we included. These findings are categorized by intervention topic, considering the quality of evidence for their impact on urinary or faecal incontinence.
For additional information and the ‘Summary of findings’ table for the outcomes of interest, see Table 5.

Table 5.
Summary of findings.
No conclusion possible: low-quality evidence.
The review on selective or routine episiotomy [11] showed no evidence of a difference for the prevention of urinary incontinence (RR 0.98, 95% CI 0.67 to 1.44; three trials; 1107 women).
The review on techniques for repairing anal sphincter injuries [13] showed no evidence of a difference between end-to-end repair and overlap repair for the prevention of faecal incontinence at 6 weeks (RR 0.65, 95% CI 0.20 to 2.07, 1 trial, 63 women), 3 months (RR 0.84 95% CI 0.06 to 12.73, 2 trials, 201 women), 6 months (RR 0.48 95% CI 0.02 to 12.89, 2 trials, 205 women), 12 months (RR 0.37 95% CI 0.03 to 4.68, 3 trials, 256 women), 24 months (RR 0.88, 95% CI 0.32 to 2.41, 1 trial, 95 women) and 36 months (RR 1.01, 95% CI 0.34 to 2.98, 1 trial, 68 women).
The review comparing planned caesarean or planned vaginal delivery for women with a breech presentation [6] showed a decrease in urinary incontinence at 3 months (RR 0.62 95% CI 0.41 to 0.93, 1 trial with 1595 women) but no difference was detected for faecal incontinence at 3 months (RR 0.54 95% CI 0.18 to 1.62, 1 study, 1226 women) and no evidence of a difference was detected at 2 years for both urinary incontinence (RR 1.14, 95% CI 0.81 to 1.61) and faecal incontinence (RR 1.11 95% CI 0.47 to 2.58, 1 study, 917 women).
3.3. Probably Ineffective Interventions: Moderate-Quality Evidence
The review on antenatal digital perineal massage [9] did not show a difference in urinary incontinence (RR 0.90 95% CI 0.74 to 1.08) or faecal incontinence (RR 0.70 95% CI 0.27 to 1.80, four trials, 2497 women).
The review comparing planned caesarean and a planned vaginal delivery for women with a twin pregnancy [7] did not show a difference in urinary (RR 0.87 95% CI 0.64 to 1.18) or faecal incontinence (RR 1.02 95% CI 0.69 to 1.85, 2 trials, 2864 women).
The review comparing caesarean delivery and vaginal delivery [5] did not find a benefit for faecal incontinence (OR 0.93 95% CI 0.77 to 1.13, 20 observational studies, 1 trial, 31,698 women).
3.4. Probably Effective Interventions: Moderate-Quality Evidence
Performing an endo-anal ultrasound after childbirth and prior to repairing any perineal tears [12] probably reduced severe faecal incontinence before 6 months postpartum (RR 0.48 95% CI 0.24 to 0.97, 1 trial, 752 women) and from 6 to 12 months post-partum (RR 0.38; 95% CI 0.20–0.72). However, it seems to not be effective for non-severe faecal incontinence before and after 6 months (RR 0.95, 95% CI 0.73–1.22).
Pelvic floor muscle training [10] may reduce urinary incontinence in early and mid-postnatal periods (RR 0.38 95% CI 0.17 to 0.83, 5 trials, 439 women for early postnatal period; RR 0.71 95% CI 0.54 to 0.95, 5 trials, 673 women for mid-postnatal period) but no evidence of a difference was provided in the late postnatal period (RR 1.20 95% CI 0.65 to 2.21, 1 trial, 44 women for late postnatal period).
Using a vacuum instead of forceps in the case of assisted vaginal delivery [8] seems to cause less faecal incontinence (RR 0.56 95% CI 0.61 to 0.84, 1 trial, 130 women).
4. Discussion
4.1. Summary of Main Results
Nine Cochrane reviews were included in this overview, encompassing 67 randomized controlled trials (21,355) and 20 non-randomized controlled studies (29,758).
Probably effective interventions: a possible reduction in faecal incontinence was found for the following:
- When performing an endo-anal ultrasound after childbirth and prior to repairing any perineal tears (moderate-quality evidence);
- When using a vacuum instead of forceps for instrumented vaginal deliveries (moderate-quality evidence);
- When pelvic floor muscle training is performed postpartum (moderate-quality evidence).
Probably ineffective interventions:
No evidence of a difference in urinary or faecal incontinence when antenatal perineal massage is performed (moderate-quality evidence), a planned caesarean delivery instead of a planned vaginal delivery for women (overall, for twins and for breech) (moderate-quality evidence). There was a short-term decrease in faecal incontinence in the case of a planned caesarean for breech, but no effect in the longer term.
No conclusion possible:
No clear difference in preventing urinary or faecal incontinence when performing a routine or selective episiotomy or when using the overlap or end-to-end repair for obstetrics anal sphincter injuries (low quality evidence).
4.2. Overall Completeness and Applicability of Evidence
This overview presents a summary of Cochrane reviews that have evaluated various antenatal, intrapartum and postpartum interventions and their effects on urinary and faecal incontinence.
We included a total of nine reviews, which reported data on the primary outcome and urinary and faecal incontinence. Additionally, we found seven protocols that have already specified urinary or faecal incontinence as secondary outcomes. These protocols will be taken into account for potential integration in upcoming revisions of the overview once they are published as full reviews. These protocols are designed to examine interventions related to urinary and faecal incontinence including perineal techniques during the second stage of labour for reducing perineal trauma, planned elective repeat caesarean section versus planned vaginal birth for women with a previous caesarean birth, surgical repair of spontaneous perineal tears that occur during childbirth versus no intervention, position in the second stage of labour for women without epidural analgesia, symphysiotomy for feto-pelvic disproportion, discontinuation of epidural analgesia late in labour and hyaluronidase for reducing perineal trauma. See Appendix A, Ongoing reviews.
We could not involve two more reviews that assessed urinary or faecal incontinence as the primary or secondary outcome, because no trial met the inclusion criteria (despite the fact that they recognized the possible influence of the interventions on incontinence by including it as an outcome in their review).
We have summarized the main conclusions of these reviews in Appendix B (Reviews awaiting further classification). These reviews will be reconsidered for inclusion in future updates of the overview.
4.3. Quality of the Evidence
Each of the reviews evaluated the potential bias in the randomized trials they included.
Four out of the nine reviews employed the GRADE approach to appraise the quality of evidence regarding their review outcomes [6,7,10,11]. For the remaining reviews, we employed the GRADE score to assess the quality of evidence, taking into account the study constraints (risk of bias) as indicated by the authors of the reviews. Regarding the primary outcome, urinary and faecal incontinence, the quality of the evidence ranged from low to moderate. The low quality frequently came from inaccuracies arising from limited sample sizes, a scarcity of occurrences and expansive confidence intervals.
Because our overview’s data were derived from longer-term follow-up antenatal, intrapartum or postpartum interventions, we meticulously examined potential biases associated with attrition (where some women were lost to follow-up, possibly leading to differences from those who were followed-up).
Table 5 displays the summary of findings regarding the quality of evidence for our outcomes.
4.4. Potential Biases in the Overview Procedure
When studies talked about urinary or faecal incontinence as an outcome, there was little data reported by the patients. This lack of date did not allow us to have complete and detailed information about it.
The subjective nature of the outcomes (self-questionnaires) may limit the quality of the assessment. Symptoms reported by women may be seen, however, as more important compared to any objective measurement (e.g., sphincter tone).
Moreover, all reviews have a low quality of evidence according to the GRADE score.
We only searched in the Cochrane Database of Systematic Reviews. We only chose this one because this is a highly demanding database (see [1]). Using only one database could be a limitation for our review, but the Cochrane Database has rigorous methodology in order to limit the risk of bias guaranteeing a reliable understanding of the evidence [14]. However, it is clear that the heterogeneity of the interventions in some reviews can have a negative impact on the results.
4.5. Consensus and Disparities with Other Studies
No other systematic review or overview about interventions for the prevention of urinary or faecal incontinence were identified.
Regarding perineal trauma and urinary and faecal incontinence prevention:
- Some recommendations included that routine episiotomy does not prevent severe perineal trauma [10];
- A vaginal delivery with vacuum resulted in less damage to the perineum than the forceps [7];
- The systematic search of obstetrical anal sphincter injury is necessary after vaginal delivery to adapt the repair [12];
- Antenatal pelvic floor muscle training seems to be beneficial to prevent incontinence postpartum [9];
- Caesarean delivery could be beneficial to prevent incontinence post-partum compared to vaginal delivery [4].
Incontinence and prolapse are seen as consequences of vaginal delivery, and a caesarean section may be requested by women to protect the pelvic floor, despite the fact that it is a major surgical procedure with significant complications. Ref. [15] reported data on possible adverse health outcomes for children delivered by caesarean, compared to those delivered vaginally. This includes respiratory illness, atopic conditions, obesity, diabetes and other severe auto-immune diseases. It highlights the need to warn women about these risks and to discuss if caesarean delivery is acceptable only to prevent possible pelvic floor damage. Furthermore, ref. [16] did not show a difference in short-term pelvic floor muscle strength after childbirth between primiparous women who underwent caesarean section or vaginal delivery, which highlights the need to discuss the indication of a caesarean delivery in order to prevent possible pelvic floor damage.
A study [17] suggested that women want to know their risk of developing pelvic floor dysfunction to help make decisions about childbirth. They also report that knowing their risks would motivate them to undertake preventative strategies, such as pelvic floor muscle training. This desire for information is further supported by [17] as part of a “care bundle” that has been shown to reduce the risk of obstetric anal sphincter injury, with no increase in caesarean section rate. This “care bundle” consists in four elements: antenatal information for women about OASIS, use of a manual perineal protection, performing an episiotomy only if needed, performing it mediolaterally with a 60-degree angle at crowning, and a systematic examination of the vagina and ano-rectum after childbirth. Ref. [18] studied women’s experience of the OASIS Care Bundle. Their findings suggest that the four elements of the OASIS Care Bundle are acceptable to women. This highlights the need for antenatal risk assessment and providing women with information on which to make informed choices.
5. Authors’ Conclusions
5.1. Implications for Practice
This overview summarizes the evidence from Cochrane reviews of randomized controlled trials and non-randomized controlled trials regarding the effects of antenatal, intrapartum and postpartum interventions on urinary and faecal incontinence.
There were no interventions with high-quality evidence of a benefit in this overview.
There were interventions with moderate-quality evidence showing a possible reduction in urinary or faecal incontinence: (1) performing an endo-anal ultrasound after childbirth and prior to repair of any perineal tears, (2) using a vacuum instead of forceps for assisted vaginal deliveries and (3) performing pelvic floor muscle training.
There were interventions with moderate-quality evidence showing no clear difference in urinary or faecal incontinence: (1) performing an antenatal perineal massage and (2) performing a planned caesarean delivery instead of a planned vaginal delivery for women with a twin pregnancy or performing a caesarean delivery instead of a vaginal delivery.
For other interventions examined in this overview, we could not draw any conclusions due to either low-quality evidence or a lack of evidence altogether.
5.2. Implications for Research
This overview emphasizes the lack of sufficient evidence to make conclusive statements relative to the impact of different antenatal, intrapartum, and postpartum interventions on urinary and faecal incontinence. It may be attributed to the following:
- A shortage of primary research exists, with few long-term, follow-up studies on women involving randomized trials of antenatal, intrapartum and postpartum interventions.
- Insufficient reporting on urinary and faecal incontinence by randomized trials.
- Insufficient reporting on incontinence postpartum by relevant Cochrane reviews (probably because it was not predefined as an outcome).
- The absence of a Cochrane review evaluating potentially relevant interventions.
Considering our enhanced comprehension of the various risk factors and etiologies contributing to postpartum urinary and faecal incontinence, there is a pressing demand for conducting long-term, follow- up studies on interventions that target these risk factors. These studies should adhere to rigorous design principles and strive for uniformity in measuring and reporting outcomes related to urinary and faecal incontinence. This approach will enable the pooling of outcome data and, as a result, inform research endeavors focused on preventing postpartum incontinence.
Author Contributions
Conceptualization, J.S. and S.P.; methodology, J.S.; validation, D.L.F., M.B. and A.F.; writing—original draft preparation, J.S.; writing—review and editing, J.S.; visualization, J.S.; supervision, D.L.F. and M.B., A.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Acknowledgments
We thank the assistance provided by the Cochrane Central Editorial Service and their suggested corrections.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A. Ongoing Reviews
| Review Citation | Overview of Pre-Specified Outcomes in the Protocol |
| Aasheim et al. | Secondary outcomes included
|
| Dodd et al. | Secondary outcomes included
|
| Elharmeel et al. | Secondary outcomes included
|
| Gupta et al. | Secondary outcomes included
|
| Hofmeyr et al. | Secondary outcomes included
|
| Torvaldsen et al. | Secondary outcomes included
|
| Zhou F et al. | Secondary outcomes
|
|
Appendix B. Reviews Awaiting Further Classification
| Review Citation | Overview of Pre-Specified Outcomes in Review with No Outcome Data | Main Conclusion of Review |
| Farrar et al. | Primary outcome included
| No included trials. “No completed trials that met the inclusion criteria of the review were identified”. |
| Hofmeyr et al. | Secondary outcomes included
| No included trials. “We found no randomized or quasi-randomized trials of symphysiotomy for either inclusion or exclusion”. |
Appendix C. AMSTAR 2 Criteria
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
References
- Pollock, M.; Fernandes, R.M.; Becker, L.A.; Pieper, D.; Hartling LChapter, V. Overviews of Reviews. In Cochrane Handbook for Systematic Reviews of Interventions Version 6.4 (Updated August 2023); Higgins, J.P.T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M.J., Welch, V.A., Eds.; Available online: https://training.cochrane.org/handbook/current/chapter-v.2023 (accessed on 6 September 2023).
- Brown, J.; Alwan, N.A.; West, J.; Brown, S.; McKinlay, C.J.; Farrar, D.; Crowther, C.A. Lifestyle interventions for the treatment of women with gestational diabetes. Cochrane Database Syst. Rev. 2017, 5, CD011970. [Google Scholar] [CrossRef] [PubMed]
- Glazener, C.M.; MacArthur, C.; Hagen, S.; Elders, A.; Lancashire, R.; Herbison, G.P.; Wilson, P.D.; ProLong Study Group. Twelve-year follow-up of conservative management of postnatal urinary and faecal incontinence and prolapse outcomes: Randomised controlled trial. BJOG Int. J. Obstet. Gynaecol. 2014, 121, 112–120. [Google Scholar] [CrossRef] [PubMed]
- Bols, E.M.J.; Hendriks, E.J.M.; Berghmans, B.C.M.; Baeten, C.G.M.I.; Nijhuis, J.G.; de Bie, R.A. A systematic review of etiological factors for postpartum fecal incontinence. Acta Obstet. Gynecol. Scand. 2010, 89, 302–314. [Google Scholar] [CrossRef] [PubMed]
- Nelson, R.L.; Furner, S.E.; Westercamp, M.; Farquhar, C. Cesarean delivery for the prevention of anal incontinence. Cochrane Database Syst. Rev. 2010, 2. [Google Scholar] [CrossRef] [PubMed]
- Hofmeyr, G.J.; Hannah, M.; Lawrie, T.A. Planned caesarean section for term breech delivery. Cochrane Database Syst. Rev. 2015. [Google Scholar] [CrossRef] [PubMed]
- Hofmeyr, G.; Barrett, J.; Crowther, C. Planned caesarean section for women with a twin pregnancy. Cochrane Database Syst. Rev. 2015. [Google Scholar] [CrossRef] [PubMed]
- O’Mahony, F.; Hofmeyr, G.J.; Menon, V. Choice of instruments for assisted vaginal delivery. Cochrane Database Syst. Rev. 2010. [Google Scholar] [CrossRef] [PubMed]
- Beckmann, M.M.; Stock, O.M. Antenatal perineal massage for reducing perineal trauma. Cochrane Database Syst. Rev. 2013. [Google Scholar] [CrossRef] [PubMed]
- Woodley, S.J.; Lawrenson, P.; Boyle, R.; Cody, J.D.; Mørkved, S.; Kernohan, A.; Hay-Smith, E.J.C. Pelvic floor muscle training for preventing and treating urinary and faecal incontinence in antenatal and postnatal women. Cochrane Database Syst. Rev. 2020, 5. [Google Scholar] [CrossRef]
- Jiang, H.; Qian, X.; Carroli, G.; Garner, P. Selective versus routine use of episiotomy for vaginal birth. Cochrane Database Syst. Rev. 2017. [Google Scholar] [CrossRef] [PubMed]
- Walsh, K.A.; Grivell, R.M. Use of endoanal ultrasound for reducing the risk of complications related to anal sphincter injury after vaginal birth. Cochrane Database Syst. Rev. 2015. [Google Scholar] [CrossRef] [PubMed]
- Fernando, R.J.; Sultan, A.H.; Kettle, C.; Thakar, R. Methods of repair for obstetric anal sphincter injury. Cochrane Database Syst. Rev. 2013. [Google Scholar] [CrossRef] [PubMed]
- Harvey, L.A. Summaries of Cochrane Systematic Reviews: Making high-quality evidence accessible. Spinal Cord 2018, 56, 185. [Google Scholar] [CrossRef] [PubMed]
- King, J. Are there adverse outcomes for child health and development following caesarean section delivery? Can we justify using elective caesarean section to prevent obstetric pelvic floor damage? Int. Urogynecol. J. 2021, 32, 1963–1969. [Google Scholar] [CrossRef] [PubMed]
- Driusso, P.; Beleza, A.C.S.; Mira, D.M.; de Oliveira Sato, T.; de Carvalho Cavalli, R.; Ferreira, C.H.J.; de Fátima Carreira Moreira, R. Are there differences in short-term pelvic floor muscle function after cesarean section or vaginal delivery in primiparous women? A systematic review with meta-analysis. Int. Urogynecol. J. 2020, 31, 1497–1506. [Google Scholar] [CrossRef] [PubMed]
- Jurczuk, M.; Bidwell, P.; Gurol-Urganci, I.; van der Meulen, J.; Sevdalis, N.; Silverton, L.; Thakar, R. The OASI care bundle quality improvement project: Lessons learned and future direction. Int. Urogynecol. J. 2021, 32, 1989–1995. [Google Scholar] [CrossRef] [PubMed]
- Bidwell, P.; Sevdalis, N.; Silverton, L.; Harris, J.; Gurol-Urganci, I.; Hellyer, A.; Freeman, R.; van der Meulen, J.; Thakar, R. Women’s experiences of the OASI Care Bundle; a package of care to reduce severe perineal trauma. Int. Urogynecol. J. 2021, 32, 1807–1816. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).