The TG/HDL-c Lipid Ratio as a Cardiovascular Risk Marker in a Mexican Urban Middle-Class Population: Do We Need a Risk Score Tailored for Mexicans?
Abstract
:1. Introduction
2. Materials and Methods
Statistical Analysis
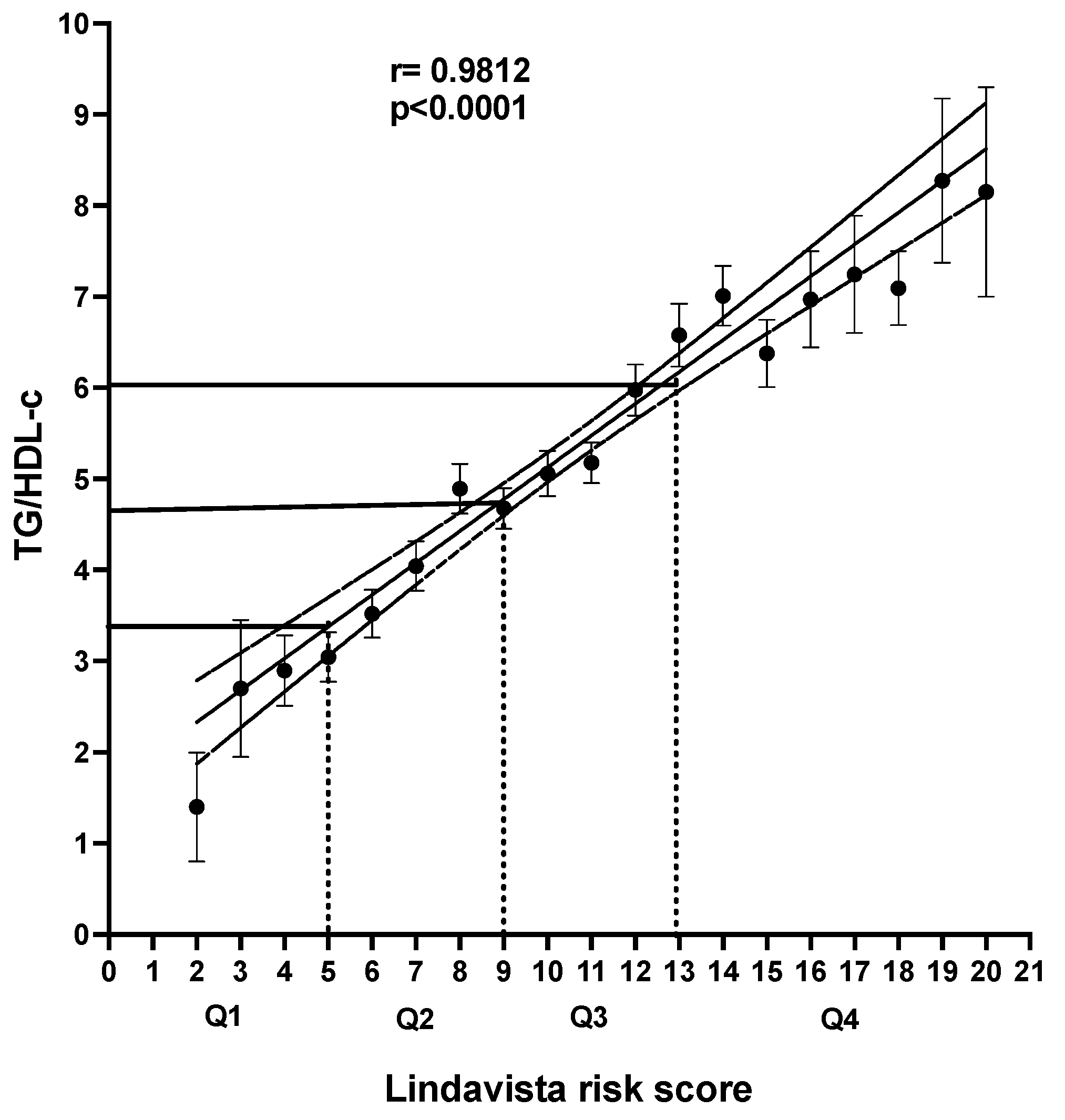
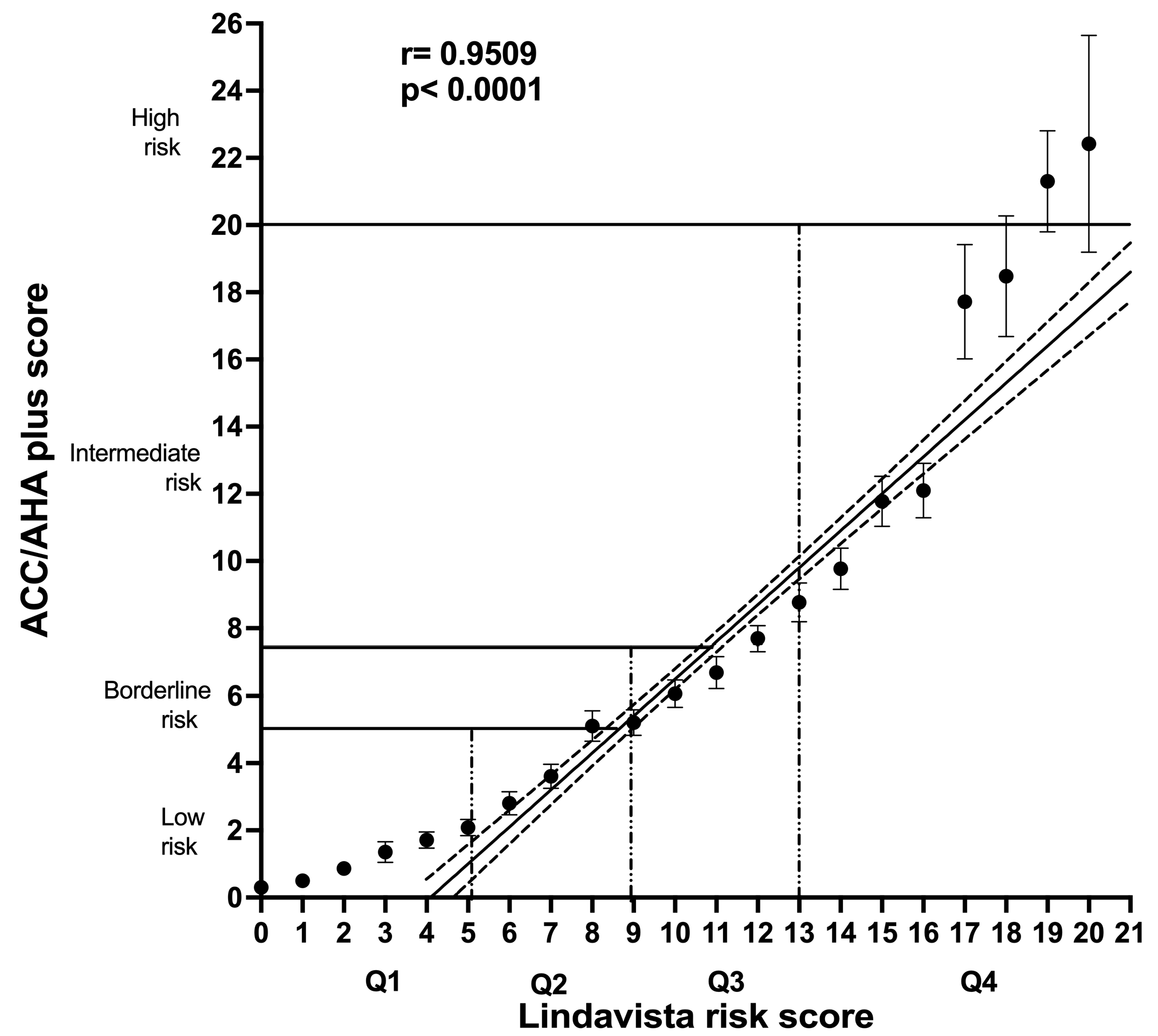
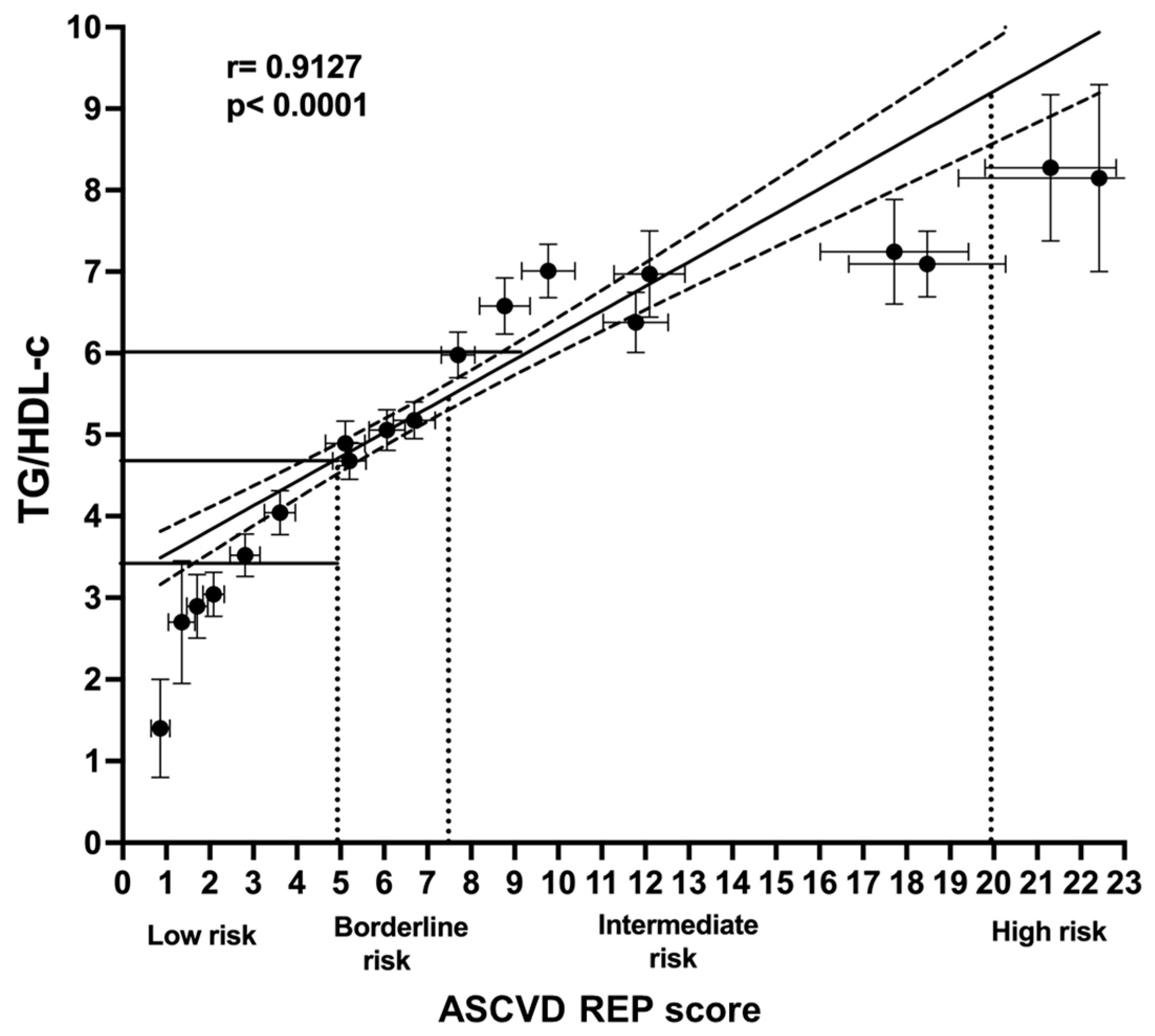
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. The Top 10 Causes of Death. Available online: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death (accessed on 12 July 2022).
- Mendoza, W.; Miranda, J.J. Global shifts in cardiovascular disease, the epidemiologic transition, and other contributing factors: Towards a new practice of Global Health Cardiology. Cardiol. Clin. 2017, 35, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Arroyo-Quiroz, C.; Barrientos-Gutierrez, T.; O’flaherty, M.; Guzman-Castillo, M.; Palacio-Mejia, L.; Osorio-Saldarriaga, E.; Rodriguez-Rodriguez, A.Y. Coronary heart disease mortality is decreasing in Argentina, and Colombia, but keeps increasing in Mexico: A time trend study. BMC Public Health 2020, 20, 162. [Google Scholar] [CrossRef] [PubMed]
- INEGI. Estadísticas de Defunciones Registradas 2021 (Preliminar). Available online: https://www.inegi.org.mx/contenidos/saladeprensa/boletines/2022/dr/dr2021_07.pdf (accessed on 12 July 2023).
- Ramos-Arellano, L.E.; Matia-Garcia, I.; Marino-Ortega, L.A.; Castro-Alarcón, N.; Muñoz-Valle, J.F.; Salgado-Goytia, L.; Salgado-Bernabé, A.B.; Parra-Rojas, I. Obesity, dyslipidemia, and high blood pressure are associated with cardiovascular risk, determined using high-sensitivity C-reactive protein concentration, in young adults. J. Int. Med. Res. 2020, 48, 0300060520980596. [Google Scholar] [CrossRef]
- Sánchez-Castillo, C.P.; Velásquez-Monroy, O.; Lara-Esqueda, A.; Berber, A.; Sepulveda, J.; Tapia-Conyer, R.; James, W.P.T. Diabetes and hypertension increases in a society with abdominal obesity: Results of the Mexican National Health Survey 2000. Public Health Nutr. 2005, 8, 53–60. [Google Scholar] [CrossRef]
- Rivera, J.A.; Barquera, S.; Campirano, F.; Campos, I.; Safdie, M.; Tovar, V. Epidemiological and nutritional transition in Mexico: Rapid increase of non-communicable chronic diseases and obesity. Public Health Nutr. 2002, 5, 113–122. [Google Scholar] [CrossRef]
- Meaney, E.; Lara-Esqueda, A.; Ceballos-Reyes, G.; Asbun, J.; Vela, A.; Martínez-Marroquín, Y.; López, V.; Meaney, A.; de la Cabada-Tamez, E.; Velázquez-Monroy, Y.; et al. Cardiovascular risk factors in the urban Mexican population: The FRIMEX study. Public Health 2007, 121, 378–384. [Google Scholar] [CrossRef]
- Fanghänel-Salmón, G.; Gutiérrez-Salmeán, G.; Samaniego, V.; Meaney, A.; Sánchez-Reyes, L.; Navarrete, U. Obesity phenotypes in urban middle-class cohorts; the PRIT-Lindavista merging evidence in Mexico: The OPUS PRIME study. Nutr. Hosp. 2015, 32, 182–188. [Google Scholar] [CrossRef] [PubMed]
- Aguilar-Salinas, C.A.; Gómez-Pérez, F.J.; Rull, J.; Villalpando, S.; Barquera, S.; Rojas, R. Prevalence of dyslipidemias in the Mexican National Health and Nutrition Survey 2006. Salud Pública Méx. 2010, 52 (Suppl. 1), 44–53. [Google Scholar] [CrossRef] [PubMed]
- Gutiérrez, J.P.; Rivera-Dommarco, J.; Shamah-Levy, T.; Villalpando-Hernández, S.; Franco, A.; Cuevas-Nasu, L. Encuesta Nacional de Salud y Nutrición 2012: Resultados Nacionales; Instituto Nacional de Salud Pública (MX): Cuernavaca, México, 2012; Available online: https://ensanut.insp.mx/encuestas/ensanut2012/doctos/informes/ENSANUT2012ResultadosNacionales.pdf (accessed on 10 January 2023).
- Shamah-Levy, T.; Vielma-Orozco, E.; Heredia-Hernández, O.; Romero-Martínez, M.; Mojica-Cuevas, J.; Cuevas-Nasu, L. En-cuesta Nacional de Salud y Nutrición 2018-19: Resultados Nacionales; Instituto Nacional de Salud Pública: Cuernavaca, México, 2020; Available online: https://www.saludpublica.mx/index.php/spm/article/view/12280 (accessed on 10 January 2023).
- Meaney, A.; Ceballos-Reyes, G.; Gutiérrez-Salmean, G.; Samaniego-Méndez, V.; Vela-Huerta, A.; Alcocer, L.; Zárate-Chavarría, E.; Mendoza-Castelán, E.; Olivares-Corichi, I.; García-Sánchez, R.; et al. Cardiovascular risk factors in a Mexican middle-class urban population. The Lindavista Study. Baseline data. Arch. Cardiol. Mex. 2013, 83, 249–256. [Google Scholar] [CrossRef]
- Campos-Nonato, I.; Galván-Valencia, Ó.; Hernández-Barrera, L.; Oviedo-Solís, C.; Barquera, S. Prevalencia de obesidad y factores de riesgo asociados en adultos mexicanos: Resultados de la Ensanut 2022. Salud Publica Mex. 2023, 65 (Suppl. 1), 238–247. [Google Scholar] [CrossRef]
- Basto-Abreu, A.; López-Olmedo, N.; Rojas-Martínez, R.; Aguilar-Salinas, C.A.; Moreno-Banda, G.L.; Carnalla, M.; Rivera, J.A.; Romero-Martinez, M.; Barquera, S.; Barrientos-Gutiérrez, T. Prevalencia de prediabetes y diabetes en México: Ensanut 2022. Salud Publica Mex. 2023, 65 (Suppl. 1), 163–168. [Google Scholar] [CrossRef] [PubMed]
- Rivas-Gomez, B.; Almeda-Valdés, P.; Tussié-Luna, M.T.; Aguilar-Salinas, C.A. Dyslipidemia in Mexico, a Call for Action. Rev. Investig. Clin. 2018, 70, 211–216. [Google Scholar] [CrossRef]
- Cooney, M.T.; Dudina, A.; D’Agostino, R.; Graham, I.M. Cardiovascular risk-estimation systems in primary prevention. Do they differ? Do they make a difference? Can we see the future? Circulation 2010, 122, 300–310. [Google Scholar] [CrossRef] [PubMed]
- Lloyd-Jones, D.M. Cardiovascular Risk Prediction. Basic concepts, current status, and future directions. Circulation 2010, 121, 1768–1777. [Google Scholar] [CrossRef] [PubMed]
- Meaney, E. The «Guidelines disease» («guidemania»). Rev. Mex. Cardiol. 2016, 27, 4–6. [Google Scholar]
- Millán, J.; Pintó, X.; Muñoz, A.; Zúñiga, M.; Rubiés-Prat, J.; Pallardo, L.F. Lipoprotein ratios: Physiological significance and clinical usefulness in cardiovascular prevention. Vasc. Health Risk Manag. 2009, 5, 757–765. [Google Scholar] [PubMed]
- Barbalho, S.M.; Tofano, R.J.; Bechara, M.D.; Quesada, K.; Coqueiro, D.P.; Mendes, C.G. Castelli Index and estimative of LDL-c particle size may still help in the clinical practice? J. Cardiovasc. Dis. Res. 2016, 7, 86–89. [Google Scholar] [CrossRef]
- Li, Y.-W.; Kao, T.-W.; Chang, P.-K.; Chen, W.-L.; Wu, L.-W. Atherogenic index of plasma as predictors for metabolic syndrome, hypertension and diabetes mellitus in Taiwan citizens: A 9-year longitudinal study. Sci. Rep. 2021, 11, 9900. [Google Scholar] [CrossRef]
- Bhardwaj, S.; Bhattacharjee, J.; Bhatnagar, M.K.; Tyagi, S. Atherogenic index of plasma, Castelli risk index and atherogenic coeffi-cient. New parameters in assessing cardiovascular risk. Int. J. Pharm. Bio. Sci. 2013, 3, 359–364. Available online: www.ijpbs.com (accessed on 1 November 2022).
- Gaziano, J.M.; Hennekens, C.H.; O’donnell, C.J.; Breslow, J.L.; Buring, J.E. Fasting triglycerides, high-density lipoprotein, and risk of myocardial infarction. Circulation 1997, 96, 2520–2525. [Google Scholar] [CrossRef]
- Dixon, J.R. Guidelines on Good Clinical Practice. Int. Digest Health Legis. 1999, 6, 65–74. [Google Scholar] [CrossRef]
- World Medical Association. Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- Diario de la Federación. Available online: http://www.salud.gob.mx/cnts/pdfs/LEY_GENERAL_DE_SALUD.pdf (accessed on 12 December 2022).
- Pickering, T.G.; Hall, J.E.; Appel, L.J.; Falkner, B.E.; Graves, J.; Hill, M.N.; Jones, D.W.; Kurtz, T.; Sheps, S.G.; Rocella, E.J. Recommendations for blood pressure measurement in humans and experimental animals: Part 1: Blood pressure measurement in humans: A statement for professionals from the Sub-committee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation 2005, 111, 697–716. [Google Scholar] [CrossRef] [PubMed]
- Friedewald, W.T.; Levy, R.I.; Fredrickson, D.S. Estimation of the concentration of low-density lipoprotein cholesterol in plasma without the use of the preparative ultracentrifuge. Clin. Chem. 1972, 18, 499–502. [Google Scholar] [CrossRef] [PubMed]
- Goff, D.C., Jr.; Lloyd-Jones, D.M.; Bennett, G.; Coady, S.; D’Agostino, R.B.; Gibbons, R.; Greenland, P.; Lackland, D.T.; Levy, D.; O’Donnell, C.J.; et al. 2013 ACC/AHA Guideline on the Assessment of Cardiovascular Risk: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 2014, 129 (Suppl. S2), S49–S73. [Google Scholar] [CrossRef] [PubMed]
- American College of Cardiology, American Heart Association. ASCVD Risk Estimator. Available online: https://tools.acc.org/ldl/ascvd_risk_estimator/index.html#!/calulate/estimator (accessed on 2 December 2022).
- Flores-Payan, L.; Hernández-Corona, D.M.; González-Heredia, T. Multidimensional analysis of health in Mexico: Implementation of fuzzy sets. BMC Public Health 2021, 21, 944. [Google Scholar] [CrossRef] [PubMed]
- Rojas-Martínez, R.; Aguilar-Salinas, C.A.; Romero-Martínez, M.; Castro-Porras, L.; Gómez-Velasco, D.; Mehta, R. Trends in the prevalence of metabolic syndrome and its components in Mexican adults, 2006–2018. Salud Publica Mex. 2021, 63, 713–724. [Google Scholar] [CrossRef]
- Health at a Glance 2021. OECD. Mortality following Acute Myocardial Infarction (AMI). Available online: https://www.oecd-ilibrary.org/sites/f17a2af6-en/index.html?itemId=/content/component/f17a2af6-en#:~:text=Case%20fatality%20rates%20for%20AMI,in%20and%20out%20of%20hospital (accessed on 20 February 2023).
- Cardiovascular Disease and Diabetes: Policies for Better Health and Quality of Care. OECD 2015. Available online: https://www.oecd.org/mexico/Cardiovascular-Disease-and-Diabetes-Policies-for-Better-Health-and-Quality-of-Care-Mexico.pdf (accessed on 28 March 2023).
- Estrada-Garcia, T.; Meaney, A.; López-Hernández, D.; Meaney, E.; Sánchez-Hernández, O.; Rodríguez-Arellano, E. Hyperten-sion and lipid triad are the most important attributable risks for myocardial infarction in a middle class urban Mexican popula-tion. Ann. Nutr. Metab. 2013, 63 (Suppl. 1), 1343. [Google Scholar]
- Ciruzzi, M.; Schargrodsky, H.; Pramparo, P.; Rivas Estany, E.; Rodriguez Naude, L.; De la Noval Garcia, R. Attributable risks for acute myocardial infarction in four countries of Latin America. Medicina 2003, 63, 697–703. [Google Scholar]
- Robins, S.J.; Lyass, A.; Zachariah, J.P.; Massaro, J.M.; Vasan, R.S. Insulin resistance and the relationship of a dyslipidemia to coronary heart disease. The Framingham Heart Study. Arter. Thromb. Vasc. Biol. 2011, 31, 1208–1214. [Google Scholar] [CrossRef]
- Mohammadi, H.; Ohm, J.; Discacciati, A.; Sundstrom, J.; Hambraeus, K.; Jernberg, T.; Svensson, P. Abdominal obesity and the risk of recurrent atherosclerotic cardiovascular disease after myocardial infarction. Eur. J. Prev. Cardiol. 2020, 27, 1944–1952. [Google Scholar] [CrossRef]
- Fan, H.; Li, X.; Zheng, L.; Chen, X.; Lan, Q.; Wu, H.; Ding, X.; Qian, D.; Shen, Y.; Yu, Z.; et al. Abdominal obesity is strongly associated with Cardiovascular Disease and its Risk Factors in Elderly and very Elderly Community-dwelling Chinese. Sci. Rep. 2016, 6, 21521. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Rexrode, K.M.; van Dam, R.M.; Li, T.Y.; Hu, F.B. Abdominal obesity and the risk of all-cause, cardiovascular, and cancer mortality. Sixteen years of follow-up in US women. Circulation 2008, 117, 1658–1667. [Google Scholar] [CrossRef] [PubMed]
- Hajifathalian, K.; Ueda, P.; Lu, Y.; Woodward, M.; Ahmadvand, A.; Aguilar-Salinas, C.A.; Azizi, F.; Cifkova, R.; Di Cesare, M.; Eriksen, L.; et al. A novel risk score to predict cardiovascular disease risk in national populations (Globorisk): A pooled analysis of prospective cohorts and health examination surveys. Lancet Diabetes Endocrinol. 2015, 3, 339–355. [Google Scholar] [CrossRef]
- Meaney, E.; Meaney, A. Conceptual semantics, ethnicities, demonyms, scientific language, and political correctness. Cardiovasc. Metab. Sci. 2023, 34, 4–7. [Google Scholar] [CrossRef]
- US Department of Health and Human Services, Office of Minority Health. Profile: Hispanic/Latino Americans. Available online: https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=3&lvlid=64#:~:text=According%20to%202020%20Census%20data,group%20after%20non%2DHispanic%20whites (accessed on 15 November 2022).
- Kakadiaris, I.A.; Vrigkas, M.; Yen, A.A.; Kuznetsova, T.; Budoff, M.; Naghavi, M. Machine Learning Outperforms ACC/AHA CVD Risk Calculator in MESA. J. Am. Heart Assoc. 2018, 7, e009476. [Google Scholar] [CrossRef]
- Kinosian, B.; Glick, H.; Garland, G. Cholesterol and coronary heart disease: Predicting risks by levels and ratios. Ann. Intern. Med. 1994, 121, 641–647. [Google Scholar] [CrossRef]
- Murguía-Romero, M.; Jiménez-Flores, J.R.; Sigrist-Flores, S.C.; Espinoza-Camacho, M.A.; Jiménez-Morales, M.; Piña, E.; Méndez-Cruz, A.R.; Villalobos-Molina, R.; Reaven, G.M. Plasma triglyceride/HDL-cholesterol ratio, insulin resistance, and cardiometabolic risk in young adults. J. Lipid Res. 2013, 54, 2795–2799. [Google Scholar] [CrossRef]
- Caselli, C.; De Caterina, R.; Smit, J.M.; Campolo, J.; El Mahdiui, M.; Ragusa, R.; Clemente, A.; Sampietro, T.; Clerico, A.; Liga, R.; et al. Triglycerides and low HDL cholesterol predict coronary heart disease risk in patients with stable angina. Sci. Rep. 2021, 11, 20714. [Google Scholar] [CrossRef] [PubMed]
- Ouchi, G.; Komiya, I.; Taira, S.; Wakugami, T.; Ohya, Y. Triglyceride/low-density-lipoprotein cholesterol ratio is the most valuable predictor for increased small, dense LDL in type 2 diabetes patients. Lipids Health Dis. 2022, 21, 4. [Google Scholar] [CrossRef]
- Jeppesen, J.; Hein, H.O.; Suadicani, P.; Gyntelberg, F. Relation of high TG-low HDL cholesterol and LDL cholesterol to the incidence of ischemic heart disease. An 8-year follow-up in the Copenhagen male study. Arter. Thromb. Vasc. Biol. 1997, 17, 1114–1120. [Google Scholar] [CrossRef] [PubMed]
- Dogan, C.; Bayram, Z.; Karagoz, A.; Bakal, R.B.; Erdogan, E.; Yilmaz, F.; Akbal, O.Y.; Acar, R.D.; Aktemur, T.; Guvendi, B.; et al. Is elevated triglyceride high density lipoprotein cholesterol ratio a risk factor that causes acute coronary syndrome to appear earlier? Bratisl. Med. J. 2019, 119, 770–775. [Google Scholar] [CrossRef] [PubMed]
- Vega, G.L.; Barlow, C.E.; Grundy, S.M.; Leonard, D.; DeFina, L.F. Triglyceride–to–high-density-lipoprotein-cholesterol ratio is an index of heart disease mortality and of incidence of type 2 diabetes mellitus in men. J. Investig. Med. 2014, 62, 345–349. [Google Scholar] [CrossRef] [PubMed]
- He, S.; Wang, S.; Chen, X.; Jiang, L.; Peng, Y.; Li, L.; Wan, L.; Cui, K. Higher ratio of triglyceride to high-density lipoprotein cholesterol may predispose to diabetes mellitus: 15-year prospective study in a general population. Metabolism 2012, 61, 30–36. [Google Scholar] [CrossRef] [PubMed]
- Babic, N.; Valjevac, A.; Zaciragic, A.; Avdagic, N.; Zukic, S.; Hasic, S. The Triglyceride/HDL ratio and triglyceride glucose index as predictors of glycemic control in patients with diabetes mellitus type 2. Med. Arch. 2019, 73, 163–168. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Cong, H.; Zhang, J.; Hu, Y.; Wei, A.; Zhang, Y.; Yang, H.; Ren, L.; Qi, W.; Li, W. predictive value of the triglyceride to high-density lipoprotein cholesterol ratio for all-cause mortality and cardiovascular death in diabetic patients with coronary artery disease treated with statins. Front. Cardiovasc. Med. 2021, 8, 718604. [Google Scholar] [CrossRef]
- Bittner, V.; Johnson, B.D.; Zineh, I.; Rogers, W.J.; Vido, D.; Marroquin, O.C.; Bairey-Merz, C.N.; Sopko, G. The TG/HDL cholesterol ratio predicts all cause mortality in women with suspected myocardial ischemia. A report from the Women’s Ischemia Syndrome Evaluation (WISE). Am. Heart J. 2009, 157, 548–555. [Google Scholar] [CrossRef]
- da Luz, P.L.; Favarato, D.; Junior, J.R.F.-N.; Lemos, P.; Chagas, A.C.P. High ratio of triglycerides to HDL-cholesterol predicts extensive coronary disease. Clinics 2008, 63, 427–432. [Google Scholar] [CrossRef]
- Wen, J.H.; Zhong, Y.Y.; Wen, Z.G.; Kuang, C.Q.; Liao, J.R.; Chen, L.H. Triglyceride to HDL-C ratio and increased arterial stiffness in apparently healthy individuals. Int. J. Clin. Exp. Med. 2015, 8, 4342–4348. [Google Scholar]
- Woo, M.-H.; Lee, K.O.; Chung, D.; Choi, J.W.; Kim, S.-H.; Oh, S.-H. Triglyceride/HDL-cholesterol ratio as an index of intracranial atherosclerosis in nonstroke individuals. Front Neurol. 2020, 11, 504219. [Google Scholar] [CrossRef]
- Quijada, Z.; Paoli, M.; Zerpa, Y.; Camacho, N.; Cichetti, R.; Villarroel, V.; Arata-Bellabarba, G.; Lanes, R. The triglyceride/HDL-cholesterol ratio as a marker of cardiovascular risk in obese children; association with traditional and emergent risk factors. Pediatr. Diabetes 2008, 9, 464–471. [Google Scholar] [CrossRef] [PubMed]
- Borrayo, G.; Basurto, L.; González-Escudero, E.; Diaz, A.; Vázquez, A.; Sánchez, L. Tg/Hdl-C Ratio as Cardio-Metabolic Biomarker even in Normal Weight Women. Acta Endocrinol. 2018, 14, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Baez-Duarte, B.G.; Zamora-Gínez, I.; González-Duarte, R.; Torres-Rasgado, E.; Ruiz-Vivanco, G.; Pérez-Fuentes, R. Triglycer-ide/high-density lipoprotein cholesterol (TG/HDL-C) index as a reference criterion of risk for metabolic syndrome (MetS) and low insulin sensitivity in apparently healthy subjects. Gac. Med. Mex. 2017, 153, 152–158. [Google Scholar] [PubMed]
- Marotta, T.; Russo, B.F.; Ferrara, L.A. Triglyceride-to-HDL-cholesterol Ratio and Metabolic Syndrome as Contributors to Cardiovascular Risk in Overweight Patients. Obesity 2010, 18, 1608–1613. [Google Scholar] [CrossRef]
- Wakabayashi, I.; Daimon, T. Comparison of discrimination for cardio-metabolic risk by different cut-off values of the ratio of triglycerides to HDL cholesterol. Lipids Health Dis. 2019, 18, 156. [Google Scholar] [CrossRef]
- Ferreira da Silva, E.; Minardi Mitre Cotta, R.; Toledo Mendonça, E.; Moura de Oliveira, D.; Almeida Cardoso, S.; Colodette, R.M. Optimal Cutoff of the TG/HDL-c ratio for Cardiovascular Risk in Hypertensive and Diabetic Patients Monitored by Primary Health Care in a city in Minas Gerais. Int. J. Cardiovasc. Sci. 2021, 34 (Suppl. 1), 55–65. [Google Scholar] [CrossRef]
- Xia, W.; Yao, X.; Chen, Y.; Lin, J.; Vielhauer, V.; Hu, H. Elevated TG/HDL-C, and non-HDL-C/HDL-C ratios predict mortality in peritoneal dialysis patients. BMC Nephrol. 2020, 21, 324. [Google Scholar] [CrossRef]
- Hadaegh, F.; Hatami, M.; Tohidi MSarbakhsh, P.; Saadt, N.; Azizi, F. Lipid ratios and appropriate cutoff values for prediction of diabetes: A cohort of Iranian men and women. Lipids Health Dis. 2010, 9, 85. [Google Scholar] [CrossRef]
- Ain, Q.U.; Asif, N.; Gilani, M.; Noreen Sheikh, W.; Akram, A. To determine cutoff value of triglycerides to HDL ratio in cardio-vascular risk factors. Biochem. Anal Biochem. 2018, 7, 2. [Google Scholar] [CrossRef]
- Assmann, G.; Schulte, H. Relation of high-density lipoprotein cholesterol and triglycerides to incidence of atherosclerotic coronary artery disease (The PROCAM Experience). Prospective Cardiovascular Münster Study. Am. J. Cardiol. 1992, 70, 733–737. [Google Scholar] [CrossRef]
- Rodríguez-Gutiérrez, N.; Vanoye Tamez, M.; Vázquez-Garza, E.; Villarreal-Calderón, J.R.; Castillo, E.C.; Laresgoiti-Servitje, E. Association of the triglyceride/high-density lipoprotein cholesterol index with insulin resistance in a pediatric population in Northeast Mexico. Metab. Syndr. Relat. Disord. 2020, 18, 333–340. [Google Scholar] [CrossRef] [PubMed]
- Murguía-Romero, M.; Jiménez-Flores, J.R.; Sigrist-Flores, S.C.; Tapia-Pancardo, D.C.; Ramos-Jiménez, A. Prevalence of metabolic syndrome in young Mexicans: A sensitivity analysis on its components. Nutr. Hosp. 2015, 32, 189–195. [Google Scholar] [CrossRef] [PubMed]
- González-Chávez, A.; Simental-Mendieta, L.E.; Elizondo-Argueta, S. Elevated triglycerides/HDL-cholesterol ratio associated with insulin resistance. Cir. Cir. 2011, 79, 126–131. [Google Scholar] [PubMed]
| Risk Factor Grading | Scoring |
|---|---|
| Age (years). Female | |
| <30 | −3 |
| 30–39 | −1 |
| 40–49 | 0 |
| 50–59 | 1 |
| >60 | 2 |
| Age (years). Male | |
| <30 | −1 |
| 30–39 | 0 |
| 40–49 | 1 |
| 50–59 | 2 |
| >60 | 3 |
| Smoking (daily consumption) | |
| Never smokers or former smokers (at least in the last year) | 0 |
| Cigarette consumption | |
| 1–5 per day | 1 |
| 6–10 per day | 2 |
| >10 per day | 3 |
| Body mass index (kg/m2) | |
| <25 | 0 |
| 25–29.9 | 1 |
| 30–34.9 | 2 |
| ≥35 | 3 |
| Abdominal circumference in women (cm) | |
| <80 | 0 |
| 80–84.9 | 1 |
| 85–89.9 | 2 |
| ≥90 | 3 |
| Abdominal circumference in men (cm) | |
| <90 cm | 0 |
| 90–94.9 cm | 1 |
| 95–99.9 cm | 2 |
| ≥100 cm | 3 |
| Systemic systolic blood pressure (mm Hg) | |
| <140 | 0 |
| 140–159 | 1 |
| 160–179 | 2 |
| ≥180 | 3 |
| Systemic diastolic blood pressure (mm Hg) | |
| <90 | 0 |
| 90–99 | 1 |
| 100–109 | 2 |
| ≥110 | 3 |
| Fasting glycemia (mg/dL) | |
| <100 | 0 |
| 100–126 | 1 |
| 127–140 | 2 |
| ≥140 | 3 |
| Total cholesterol (mg/dL) | |
| <200 | 0 |
| 200–239 | 1 |
| 240–279 | 2 |
| ≥280 | 3 |
| Triglycerides (mg/dL) | |
| <150 | 0 |
| 150–199 | 1 |
| 200–499 | 2 |
| ≥500 | 3 |
| HDL-c (mg/dL) | |
| ≥60 | 0 |
| 40–59 | 1 |
| 30–39 | 2 |
| <30 | 3 |
| LDL-c (mg/dL) | |
| <100 | 0 |
| 100–129 | 1 |
| 130–159 | 2 |
| ≥160 | 3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martínez-Marroquín, Y.; Meaney, A.; Samaniego-Méndez, V.; Nájera, N.; Ceballos, G.; Fernández-Barros, C.; Meaney, E. The TG/HDL-c Lipid Ratio as a Cardiovascular Risk Marker in a Mexican Urban Middle-Class Population: Do We Need a Risk Score Tailored for Mexicans? J. Clin. Med. 2023, 12, 6005. https://doi.org/10.3390/jcm12186005
Martínez-Marroquín Y, Meaney A, Samaniego-Méndez V, Nájera N, Ceballos G, Fernández-Barros C, Meaney E. The TG/HDL-c Lipid Ratio as a Cardiovascular Risk Marker in a Mexican Urban Middle-Class Population: Do We Need a Risk Score Tailored for Mexicans? Journal of Clinical Medicine. 2023; 12(18):6005. https://doi.org/10.3390/jcm12186005
Chicago/Turabian StyleMartínez-Marroquín, Yolanda, Alejandra Meaney, Virginia Samaniego-Méndez, Nayelli Nájera, Guillermo Ceballos, Carlos Fernández-Barros, and Eduardo Meaney. 2023. "The TG/HDL-c Lipid Ratio as a Cardiovascular Risk Marker in a Mexican Urban Middle-Class Population: Do We Need a Risk Score Tailored for Mexicans?" Journal of Clinical Medicine 12, no. 18: 6005. https://doi.org/10.3390/jcm12186005
APA StyleMartínez-Marroquín, Y., Meaney, A., Samaniego-Méndez, V., Nájera, N., Ceballos, G., Fernández-Barros, C., & Meaney, E. (2023). The TG/HDL-c Lipid Ratio as a Cardiovascular Risk Marker in a Mexican Urban Middle-Class Population: Do We Need a Risk Score Tailored for Mexicans? Journal of Clinical Medicine, 12(18), 6005. https://doi.org/10.3390/jcm12186005






