The Slavcleft: A Three-Center Study of the Outcome of Treatment of Cleft Lip and Palate Considering Palatal Shape
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
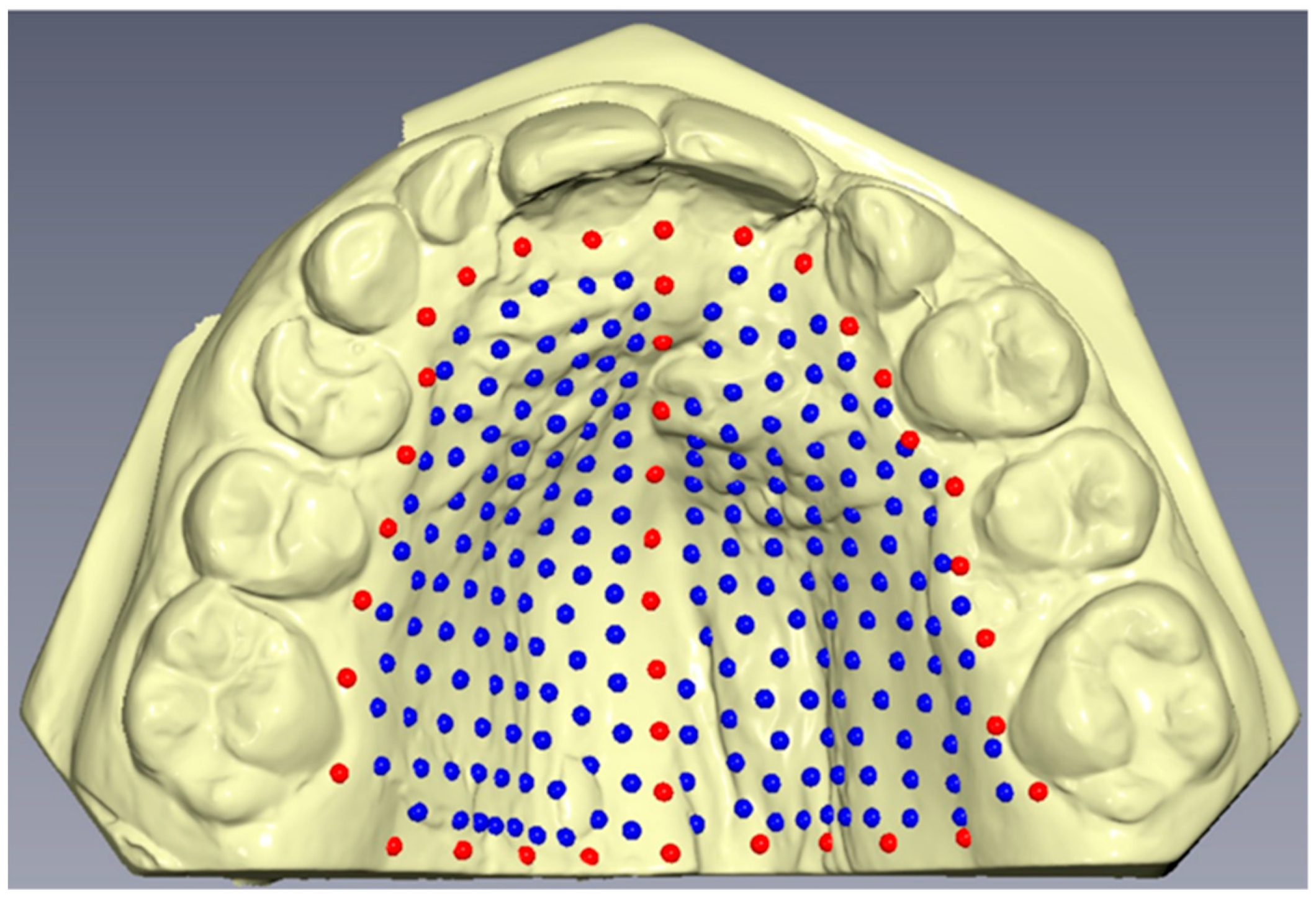
2.2. Methods
2.3. Statistical Analysis
2.4. Method Error
3. Results
3.1. Demographic Data and Method Error
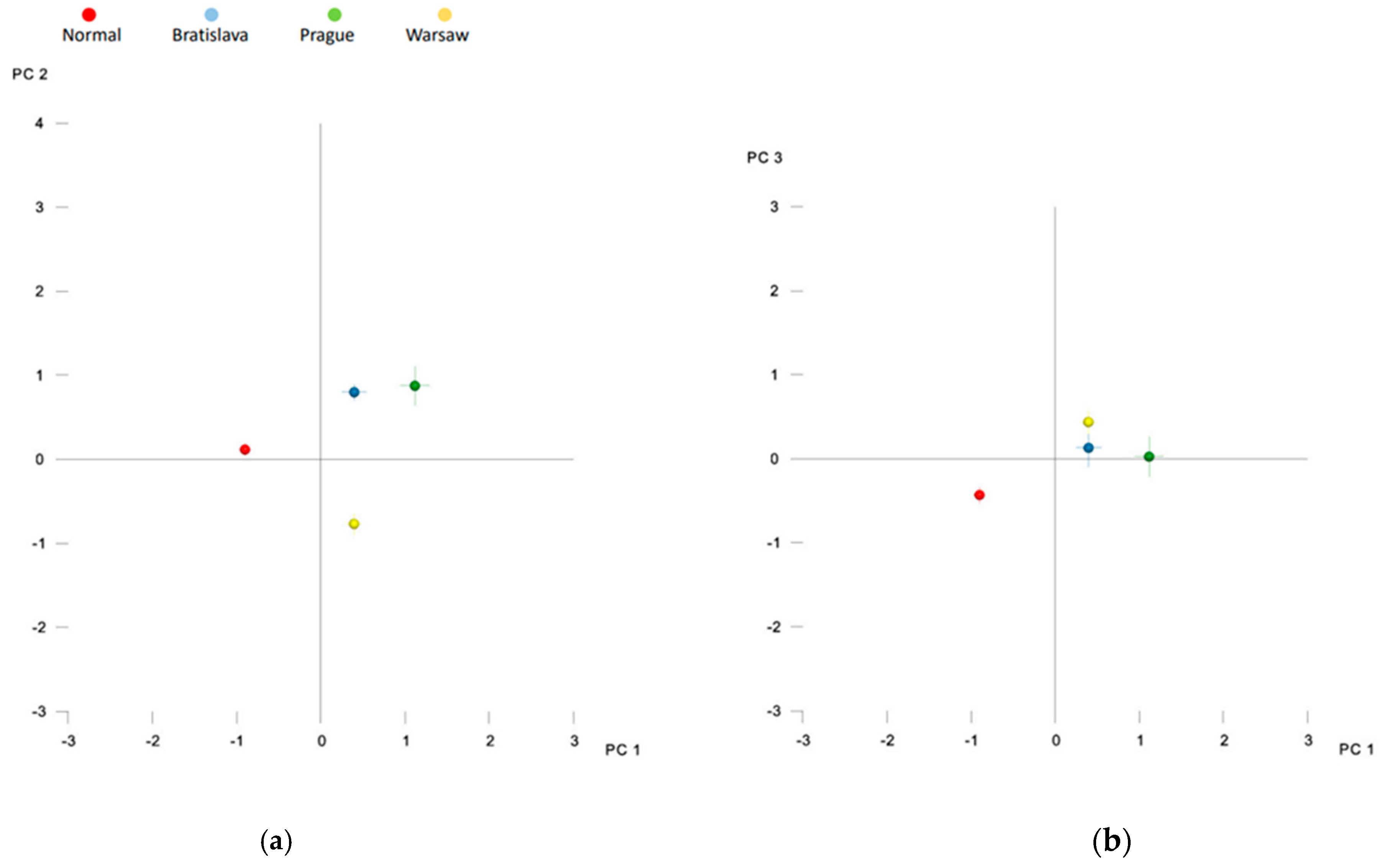
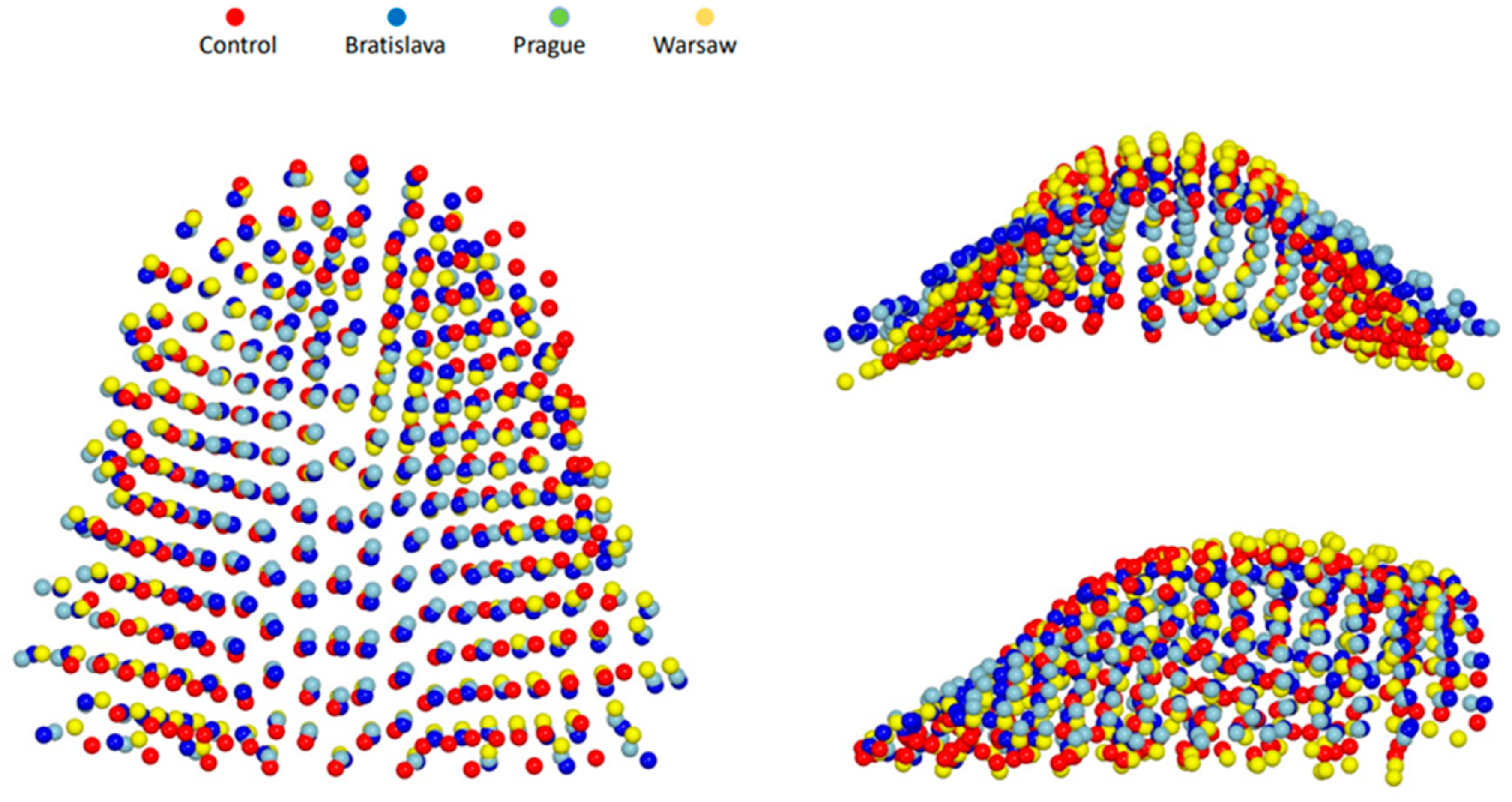
3.2. Procrustes Superimposition and PCA
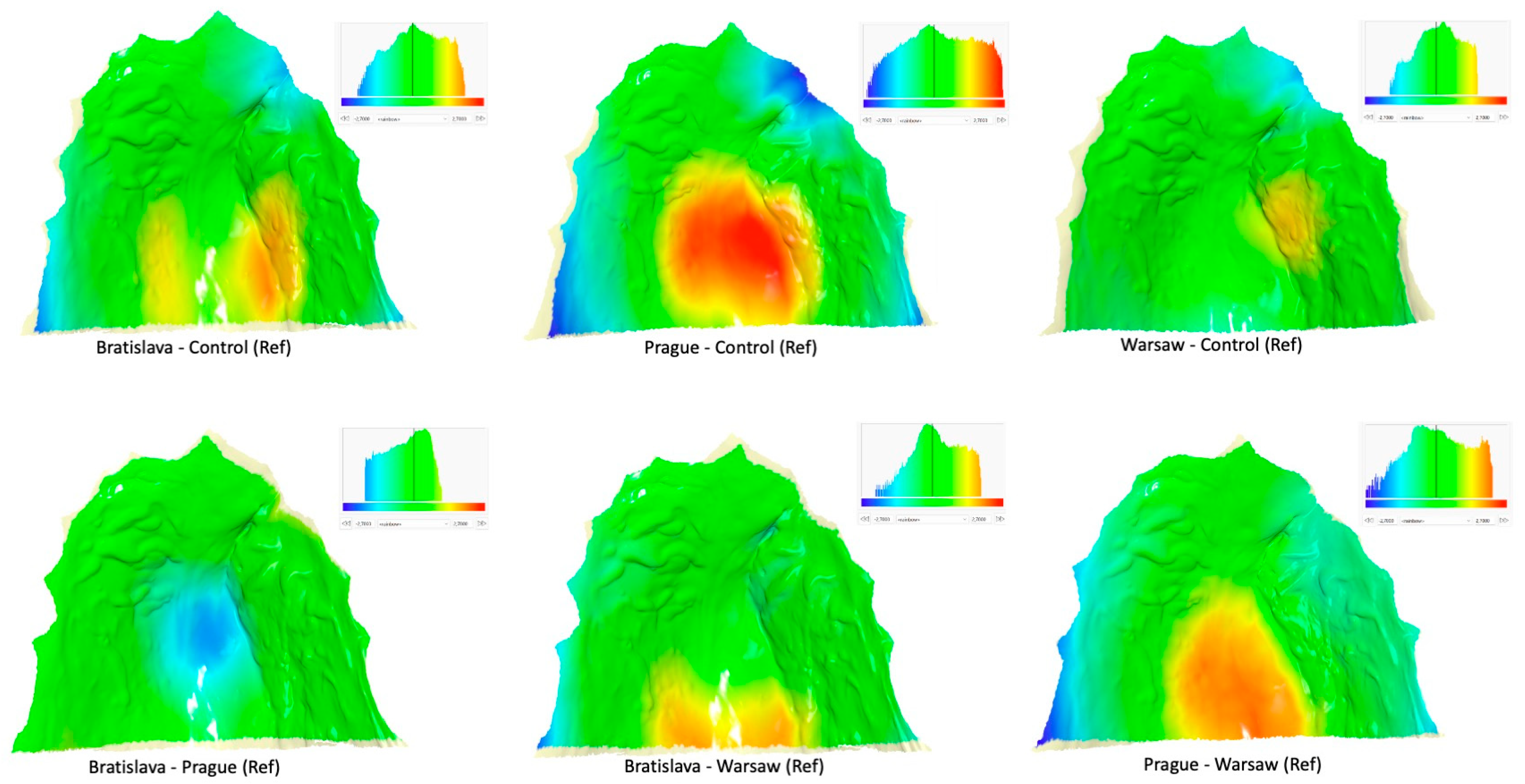
3.3. Inter-Group Differences
4. Discussion
4.1. Limitations
4.2. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kermenak, J.; Huffman, W.C.; Olin, W.H. Maxillary growth inhibition by mucoperiosteal denudation of palatal shelf bone in non-cleft beagles. Cleft Palate J. 1970, 7, 817–825. [Google Scholar]
- Wijdeveld, M.G.M.M.; Grupping, E.M.; Kuijpers-Jagtman, A.M.; Maltha, J.C. Maxillary Arch Dimensions after Palatal Surgery at Different Ages on Beagle Dogs. J. Dent. Res. 1989, 68, 1105–1109. [Google Scholar] [CrossRef] [PubMed]
- Wijdeveld, M.; Maltha, J.C.; Grupping, E.M.; De Jonge, J.; Kuijpers-Jagtman, A.M. A histological study of tissue response to simulated cleft palate surgery at different ages in beagle dogs. Arch. Oral Biol. 1991, 36, 837–843. [Google Scholar] [CrossRef] [PubMed]
- Von den Hoff, J.W.; Maltha, J.C.; Kuijpers-Jagtman, A.M. Palatal wound healing: The effects of scarring on growth. In Cleft Lip and Palate; Springer: Berlin/Heidelberg, Germany, 2013; pp. 309–324. [Google Scholar]
- Wallace, A.F. A history of the repair of cleft lip and palate in Britain before World War II. Ann. Plast. Surg. 1987, 19, 266–275. [Google Scholar] [CrossRef] [PubMed]
- Lindsay, W.K.; Witzel, M.A. Cleft palate repair: Von Langenbeck technique, Multidiscip. In Multidisciplinary Management of Cleft Lip and Palate; WB Saunders Co.: Philadelphia, PA, USA, 1990; p. 303. [Google Scholar]
- Bardach, J.; Salyer, K.E. Surgical Techniques in Cleft Lip and Palate; Year Book Medical Publishers: Chicago, IL, USA, 1987. [Google Scholar]
- Bardach, J. Two-Flap palatoplasty: Bardach’s technique. Oper. Tech. Plast. Reconstr. Surg. 1995, 2, 211–214. [Google Scholar] [CrossRef]
- Schweckendiek, W. Primary veloplasty: Long-term results without maxillary deformity. A twenty-five year report. Cleft Palate J. 1978, 15, 268–274. [Google Scholar]
- Markus, A.F.; Smith, W.P.; Delaire, J. Primary closure of cleft palate: A functional approach. Br. J. Oral Maxillofac. Surg. 1993, 31, 71–77. [Google Scholar] [CrossRef]
- Kriens, O.B. An anatomical approach to veloplasty. Plast. Reconstr. Surg. 1969, 43, 29–41. [Google Scholar] [CrossRef]
- Sommerlad, B.C. A Technique for Cleft Palate Repair. Plast. Reconstr. Surg. 2003, 112, 1542. [Google Scholar] [CrossRef]
- Furlow, L.T. Cleft palate repair by double opposing Z-plasty. Plast. Reconstr. Surg. 1986, 78, 724–738. [Google Scholar] [CrossRef]
- Fudalej, P.; Katsaros, C.; Bongaarts, C.; Dudkiewicz, Z.; Kuijpers-Jagtman, A.M. Dental arch relationship in children with complete unilateral cleft lip and palate following one-stage and three-stage surgical protocols. Clin. Oral Investig. 2011, 15, 503–510. [Google Scholar] [CrossRef] [PubMed]
- Sabelis, A.J.; Kuijpers, M.A.R.; Nada, R.M.; Chiu, Y.-T.; Bronkhorst, E.M.; Kuijpers-Jagtman, A.M.; Fudalej, P.S. Rating dental arch relationships and palatal morphology with the EUROCRAN index on three different formats of dental casts in children with unilateral cleft lip and palate. Clin. Oral Investig. 2016, 20, 943–950. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Heliövaara, A.; Küseler, A.; Skaare, P.; Bellardie, H.; Mølsted, K.; Karsten, A.; Marcusson, A.; Rizell, S.; Brinck, E.; Sæle, P.; et al. Scandcleft randomized trials of primary surgery for unilateral cleft lip and palate: Comparison of dental arch relationships and dental indices at 5, 8, and 10 years. Eur. J. Orthod. 2022, 44, 258–267. [Google Scholar] [CrossRef]
- Urbanova, W.; Klimova, I.; Brudnicki, A.; Polackova, P.; Kroupova, D.; Dubovska, I.; Rachwalski, M.; Fudalej, P.S. The Slav-cleft: A three-center study of the outcome of treatment of cleft lip and palate. Part 1: Craniofacial morphology. J. Cranio-Maxillofac. Surg. 2016, 44, 1767–1776. [Google Scholar] [CrossRef]
- Fudalej, P.S.; Urbanova, W.; Klimova, I.; Dubovska, I.; Brudnicki, A.; Polackova, P.; Kroupova, D.; Kotova, M.; Rachwalski, M. The Slavcleft: A three-center study of the outcome of treatment of cleft lip and palate. Part 2: Dental arch relationships. J. Cranio-Maxillofac. Surg. 2019, 47, 1092–1095. [Google Scholar] [CrossRef] [PubMed]
- Nollet, P.J.P.M.; Katsaros, C.; van’t Hof, M.A.; Kuijpers-Jagtman, A.M. Treatment Outcome in Unilateral Cleft Lip and Palate Evaluated with the GOSLON Yardstick: A Meta-Analysis of 1236 Patients. Plast. Reconstr. Surg. 2005, 116, 1255. [Google Scholar] [CrossRef] [PubMed]
- Salgado, K.R.; Wendt, A.R.; Fernandes Fagundes, N.C.; Maia, L.C.; Normando, D.; Leão, P.B. Early or delayed palatoplasty in complete unilateral cleft lip and palate patients? A systematic review of the effects on maxillary growth. J. Cranio-Maxillofac. Surg. 2019, 47, 1690–1698. [Google Scholar] [CrossRef]
- Reddy, R.R.; Gosla Reddy, S.; Vaidhyanathan, A.; Bergé, S.J.; Kuijpers-Jagtman, A.M. Maxillofacial growth and speech outcome after one-stage or two-stage palatoplasty in unilateral cleft lip and palate. A systematic review. J. Cranio-Maxillofac. Surg. 2017, 45, 995–1003. [Google Scholar] [CrossRef]
- Semb, G.; Enemark, H.; Friede, H.; Paulin, G.; Lilja, J.; Rautio, J.; Andersen, M.; Åbyholm, F.; Lohmander, A.; Shaw, W.; et al. Worthington, Scandcleft randomised trials of primary surgery for unilateral cleft lip and palate: 1. Planning and management. J. Plast. Surg. Hand Surg. 2017, 51, 2–13. [Google Scholar] [CrossRef]
- Primožič, J.; Perinetti, G.; Richmond, S.; Ovsenik, M. Three-dimensional longitudinal evaluation of palatal vault changes in growing subjects. Angle Orthod. 2012, 82, 632–636. [Google Scholar] [CrossRef]
- Yang, S.T.; Kim, H.K.; Lim, Y.S.; Chang, M.S.; Lee, S.P.; Park, Y.S. A three dimensional observation of palatal vault growth in children using mixed effect analysis: A 9 year longitudinal study. Eur. J. Orthod. 2013, 35, 832–840. [Google Scholar] [CrossRef] [PubMed]
- Mitteroecker, P.; Schaefer, K. Thirty years of geometric morphometrics: Achievements, challenges, and the ongoing quest for biological meaningfulness. Am. J. Biol. Anthropol. 2022, 178, 181–210. [Google Scholar] [CrossRef] [PubMed]

| Age in Years at Palatoplasty (Mean, SD, min, max) | Age in Years at Collection of Models (Mean, SD, min, max) | |
|---|---|---|
| Prague | ||
| males (n =17) | 2.6; 0.5; 1.5–3.3 | 9; 0.8; 7.3–10.1 |
| females (n = 7) | 3.9; 1.2; 2.7–6.4 | 8.7; 0.9; 7.3–10 |
| males and females (n = 24) | 3; 1; 1.5–6.4 | 8.9; 0.8; 7.3–10.1 |
| Bratislava | ||
| males (n = 11) | 0.9; 0.4; 0.6–1.8 | 8.3; 1.3; 6.1–10.3 |
| females (n = 5) | 0.9; 0.4; 0.7–1.7 | 8; 1.3; 6.3–9.5 |
| males and females (n = 16) | 0.9; 0.4; 0.6–1.8 | 8.2; 1.3; 6.1–10.3 |
| Warsaw | ||
| males (n = 37) | 0.6; 0.1; 0.4–1 | 10.3; 1.5; 8–13.9 |
| females (n = 16) | 0.7; 0.2; 0.5–1.2 | 10.1; 1.2; 8–13.9 |
| males and females (n = 53) | 0.7; 0.2; 0.4–1.2 | 10.3; 1.4; 8–13.9 |
| Control | ||
| males (n = 25) | N/A | 8.5; 1; 6.8–11.6 |
| females (n = 35) | N/A | 8.6; 1.4; 6.3–11.8 |
| males and females (n = 60) | N/A | 8.6; 1.2; 6.3–11.8 |
| Bratislava | Prague | Warsaw | Control | |
|---|---|---|---|---|
| Bratislava | - | 0.0667 * | 0.0929 * | 0.0993 * |
| Prague | 0.002 ** | - | 0.0981 * | 0.1278 * |
| Warsaw | <0.001 ** | <0.001 ** | - | 0.0964 * |
| Control | <0.001 ** | <0.001 ** | <0.001 ** | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Petrova, T.; Brudnicki, A.; Kotova, M.; Urbanova, W.; Dubovska, I.; Polackova, P.; Voborna, I.; Fudalej, P.S. The Slavcleft: A Three-Center Study of the Outcome of Treatment of Cleft Lip and Palate Considering Palatal Shape. J. Clin. Med. 2023, 12, 5985. https://doi.org/10.3390/jcm12185985
Petrova T, Brudnicki A, Kotova M, Urbanova W, Dubovska I, Polackova P, Voborna I, Fudalej PS. The Slavcleft: A Three-Center Study of the Outcome of Treatment of Cleft Lip and Palate Considering Palatal Shape. Journal of Clinical Medicine. 2023; 12(18):5985. https://doi.org/10.3390/jcm12185985
Chicago/Turabian StylePetrova, Tereza, Andrzej Brudnicki, Magdalena Kotova, Wanda Urbanova, Ivana Dubovska, Petra Polackova, Iva Voborna, and Piotr S. Fudalej. 2023. "The Slavcleft: A Three-Center Study of the Outcome of Treatment of Cleft Lip and Palate Considering Palatal Shape" Journal of Clinical Medicine 12, no. 18: 5985. https://doi.org/10.3390/jcm12185985
APA StylePetrova, T., Brudnicki, A., Kotova, M., Urbanova, W., Dubovska, I., Polackova, P., Voborna, I., & Fudalej, P. S. (2023). The Slavcleft: A Three-Center Study of the Outcome of Treatment of Cleft Lip and Palate Considering Palatal Shape. Journal of Clinical Medicine, 12(18), 5985. https://doi.org/10.3390/jcm12185985







