1. Introduction
Pain is a common and complex experience following surgical procedures that varies in intensity and duration across individuals and surgical interventions [
1]. However, pain intensity on the first day after surgery is the highest in many surgical procedures [
2,
3]. Understanding the factors influencing postoperative pain on the first postoperative day is crucial for improving patient outcomes, optimizing pain management strategies, and enhancing overall patient satisfaction [
4,
5,
6]. Pain management in the immediate postoperative period is critical because it can significantly affect recovery, patient comfort, and overall healthcare costs [
7,
8,
9].
Among the various factors that can influence postoperative pain perception, age has been identified as a significant predictor [
10,
11,
12]. However, in some studies, there were no differences in pain perception based on age [
13,
14]. However, the surgical incision, size of the surgical wound, method of anesthesia, and pain control differ according to the type of surgery. Therefore, it may be difficult to generalize the association between age and pain intensity. However, the results of these previous studies are limited [
5,
10,
13,
14].
This study investigated the association between age and pain intensity experienced on the first day after surgery in 10 distinct surgical procedures. The 10 surgeries under examination included arthroscopic rotator cuff repair (ARCR), cesarean section (C/sec), cholecystectomy, hip hemiarthroplasty, laparoscopic herniorrhaphy, open hernia repair, hysterectomy, lumbar spine fusion, total hip arthroplasty (THA), and total knee arthroplasty (TKA). By identifying the potential associations between age and pain intensity in various surgical contexts in five South Korean hospitals, we aimed to clarify age-related differences in postoperative pain perception, paving the way for tailored pain management strategies based on patient age and specific surgical procedures. The surgical types were determined based on previous studies; we extended our analysis to expand the scope of surgeries, encompassing obstetric and gynecologic surgeries—including cesarean sections and hysterectomies—and herniorrhaphies, a surgical procedure commonly performed on elderly patients.
2. Materials and Methods
2.1. Data Collection
The Clinical Research Ethics Committee of Chuncheon Sacred Heart Hospital, Hallym University, approved this retrospective cohort study. The need for informed consent was waived due to the study’s retrospective design. All data were collected from five hospitals at Hallym Medical Center through electronic medical records. Our dataset included patients’ baseline characteristics and records of anesthesia, surgery, laboratory examination, and prescription between 1 January 2013, and 30 June 2023.
2.2. Inclusion and Exclusion Criteria
This study included adult patients aged ≥ 18 who underwent one of the 10 surgical procedures between 1 January 2013, and 30 June 2023. The 10 surgical procedures were as follows: ARCR, C/sec, laparoscopic cholecystectomy, hip hemiarthroplasty, laparoscopic inguinal herniorrhaphy, open inguinal herniorrhaphy, hysterectomy, lumbar spine fusion, THA, and TKA. Surgery types were classified according to the Health Insurance Charge Code of the Republic of Korea (
Appendix A). Laparoscopic surgery is classified based on surgical records because the codes for laparoscopic and open surgery are identical.
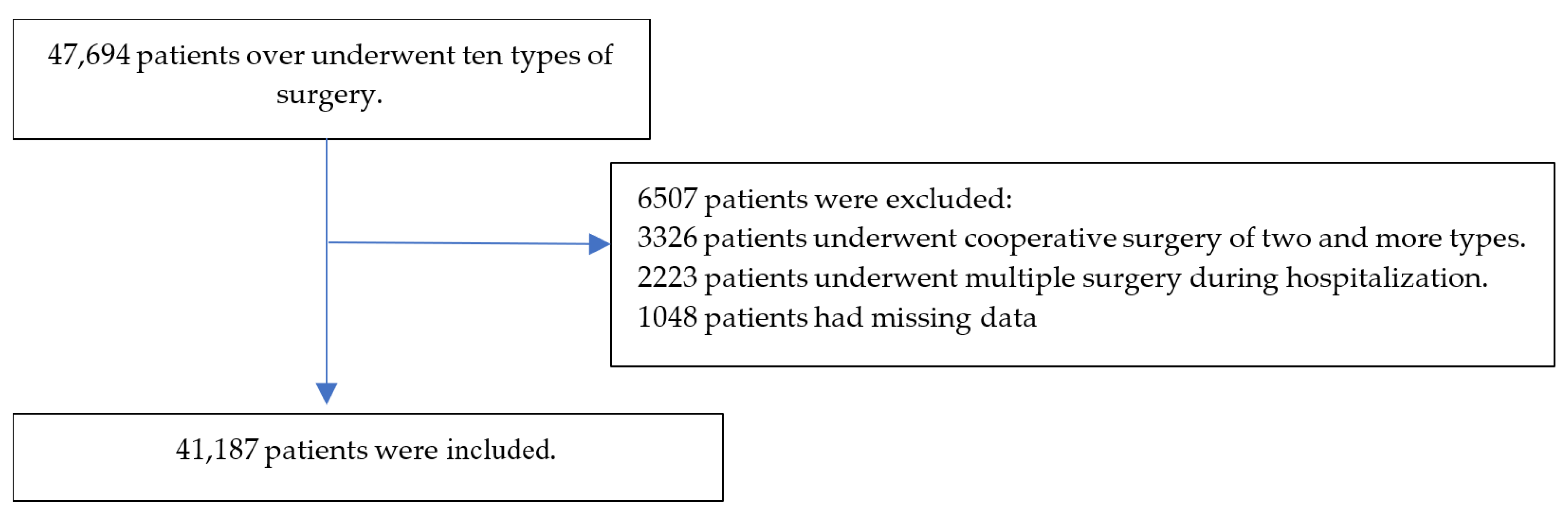
This study excluded patients with cooperative surgery, missing data, or multiple surgeries.
2.3. Exposure and Primary and Secondary Outcomes
The exposure was the age (years) of the patients. The primary outcome was the worst pain intensity during the 24 h after surgery. Pain intensity was determined using a numeric rating scale (NRS) ranging from 0 (least) to 10 (worst). Secondary outcomes were the dose of opioids used during the postoperative 24 h. Opioids included morphine, oxycodone, meperidine, nalbuphine, tramadol, transdermal fentanyl patch, transdermal buprenorphine patch, fentanyl, and alfentanil. Because several types of opioids were included, the conversion dose was calculated based on morphine. The ratio of the conversion dose is presented in
Appendix B.
2.4. Covariates
The covariates included patient characteristics, such as body mass index, comorbidities (hypertension, diabetes, tuberculosis, hepatitis, cardiac disease, cerebral vascular accident, cancer, hyperlipidemia, and sleep disorder), history of alcohol consumption, smoking, and medication (opioid, sleeping pills, and psychotropic drugs), and perioperative factors, such as physical status, emergency, anesthesia, surgery time, fluid balance, intraoperative monitoring (arterial and central venous pressures, Foley catheter, and Levin tube), and patient-controlled analgesia (route, adjuvant, and rate).
2.5. Statistics
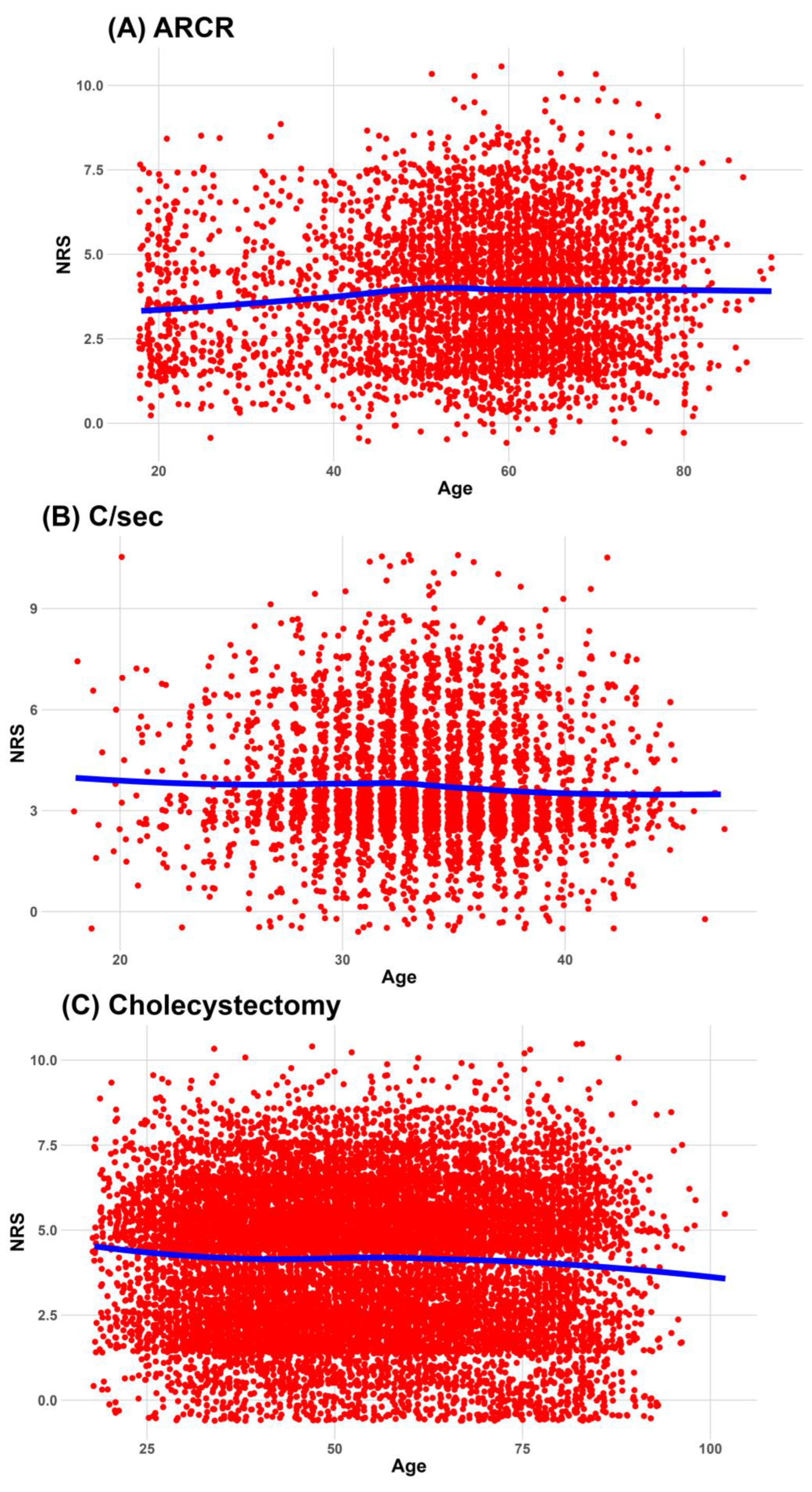
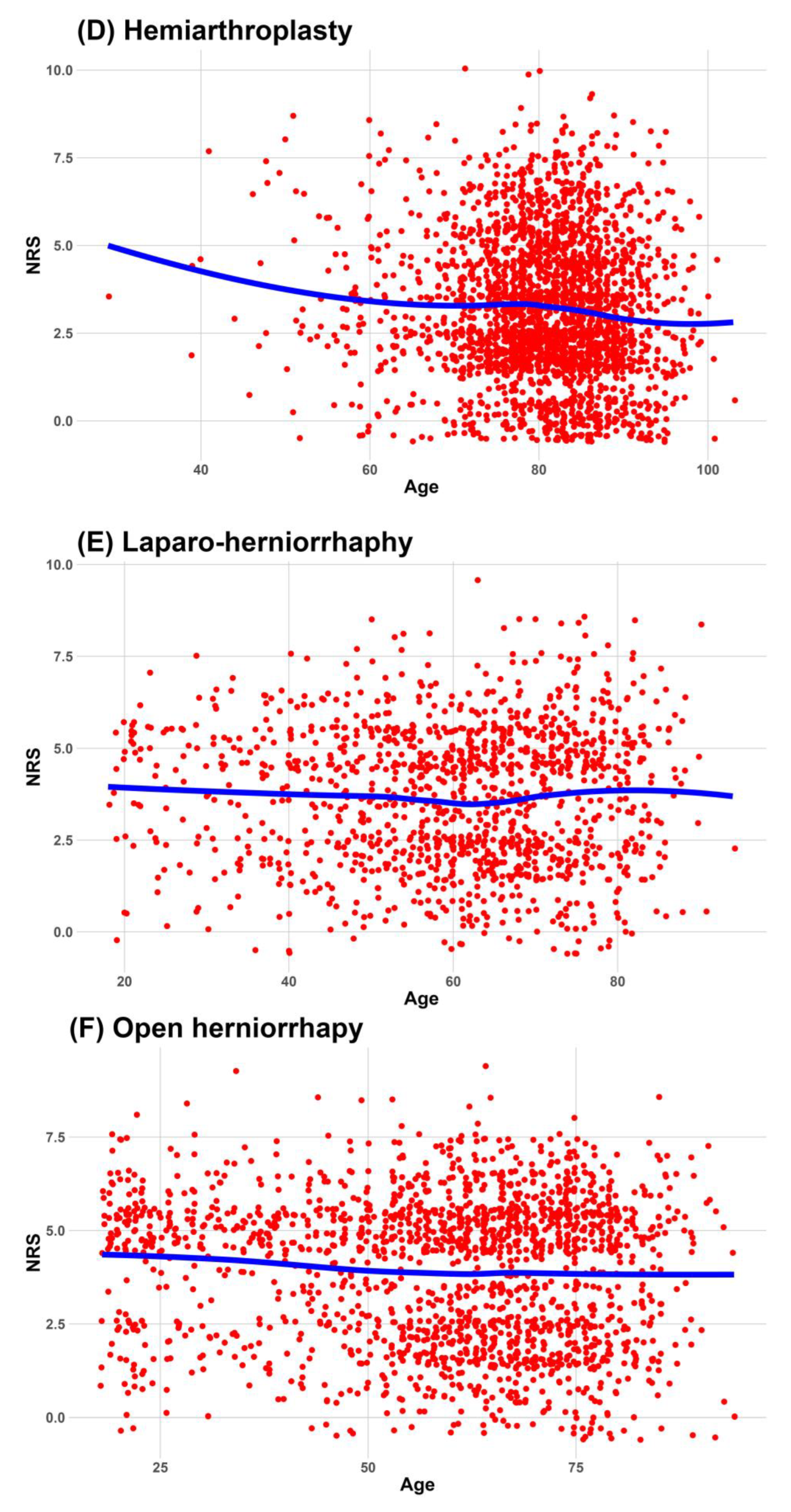
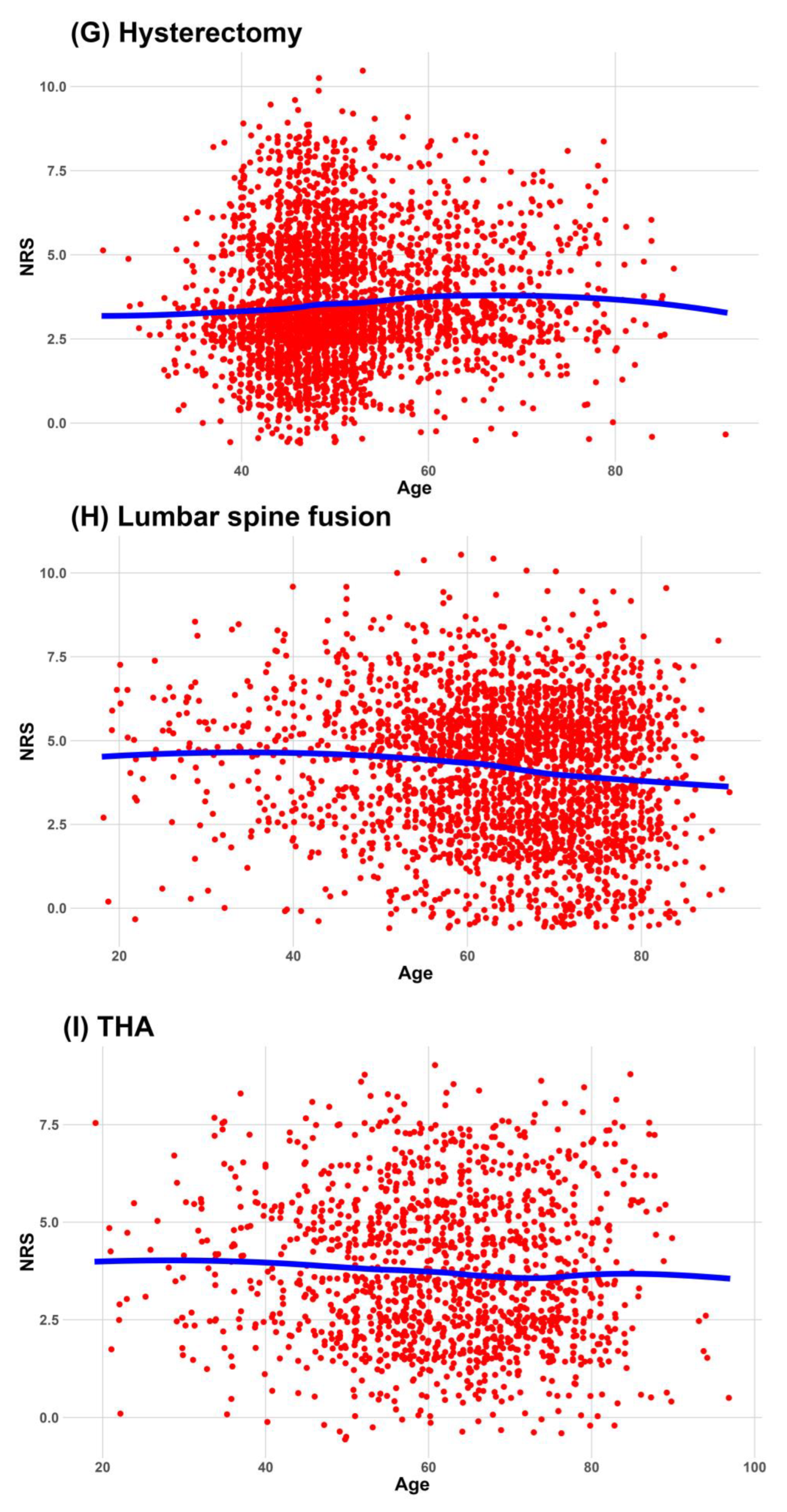
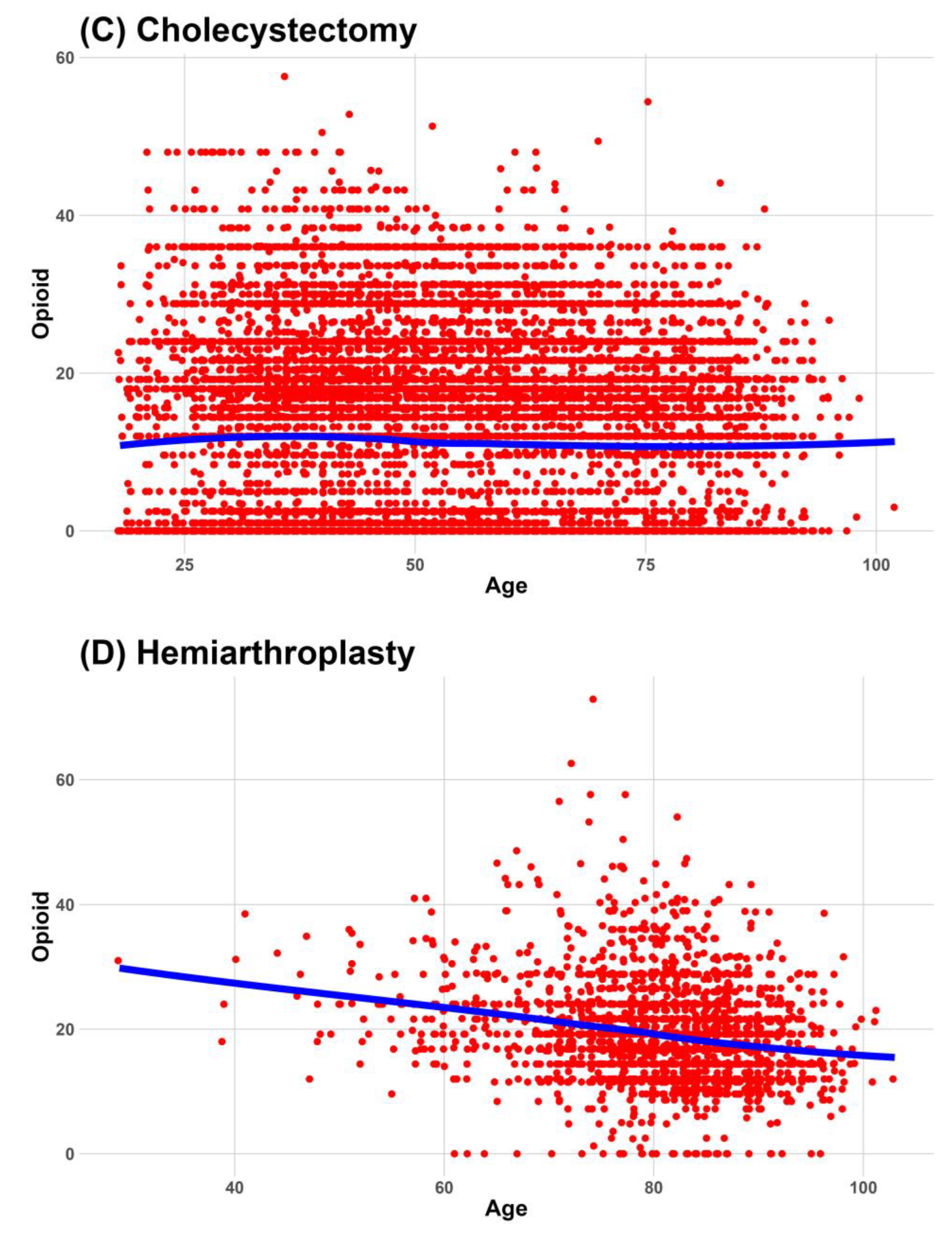
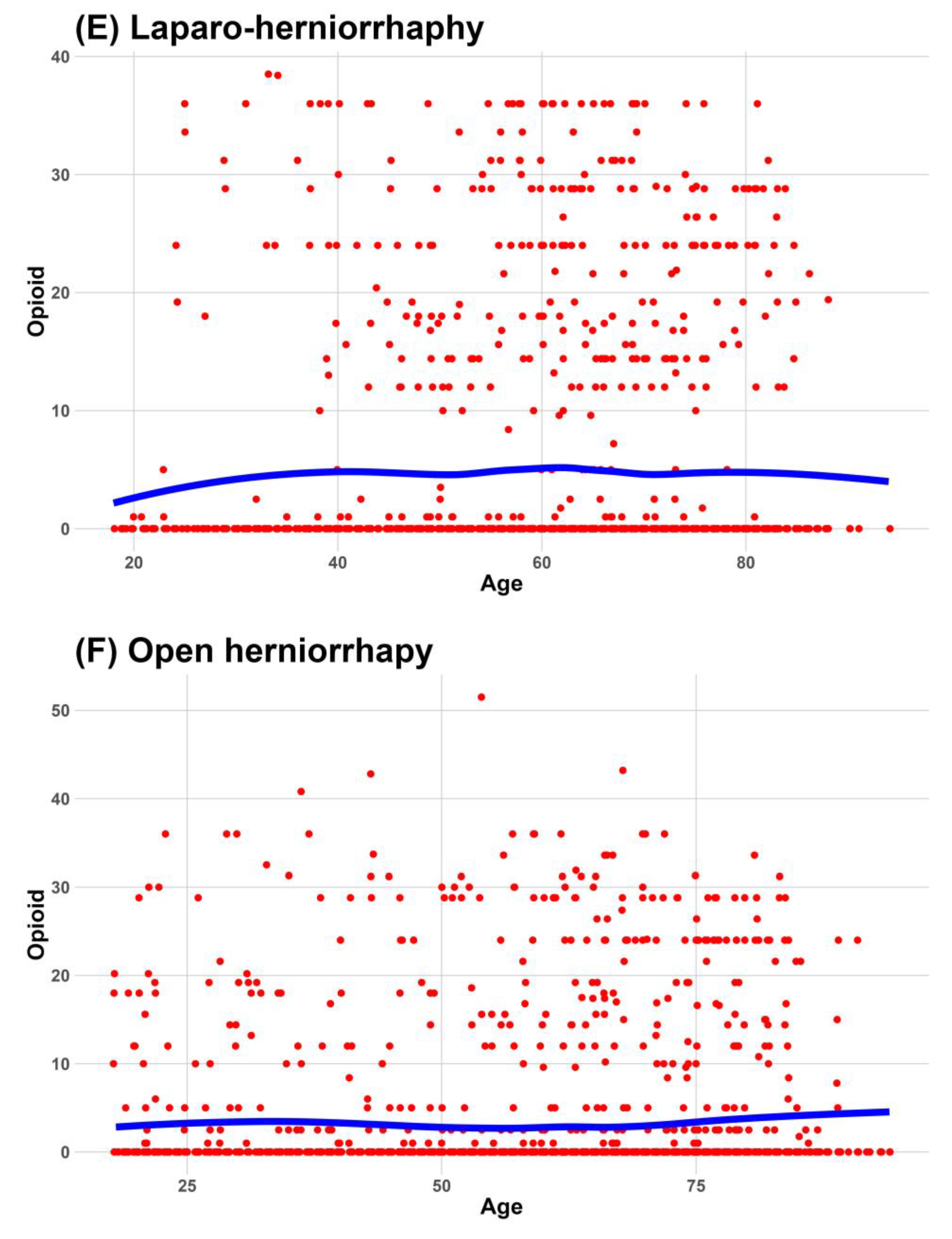
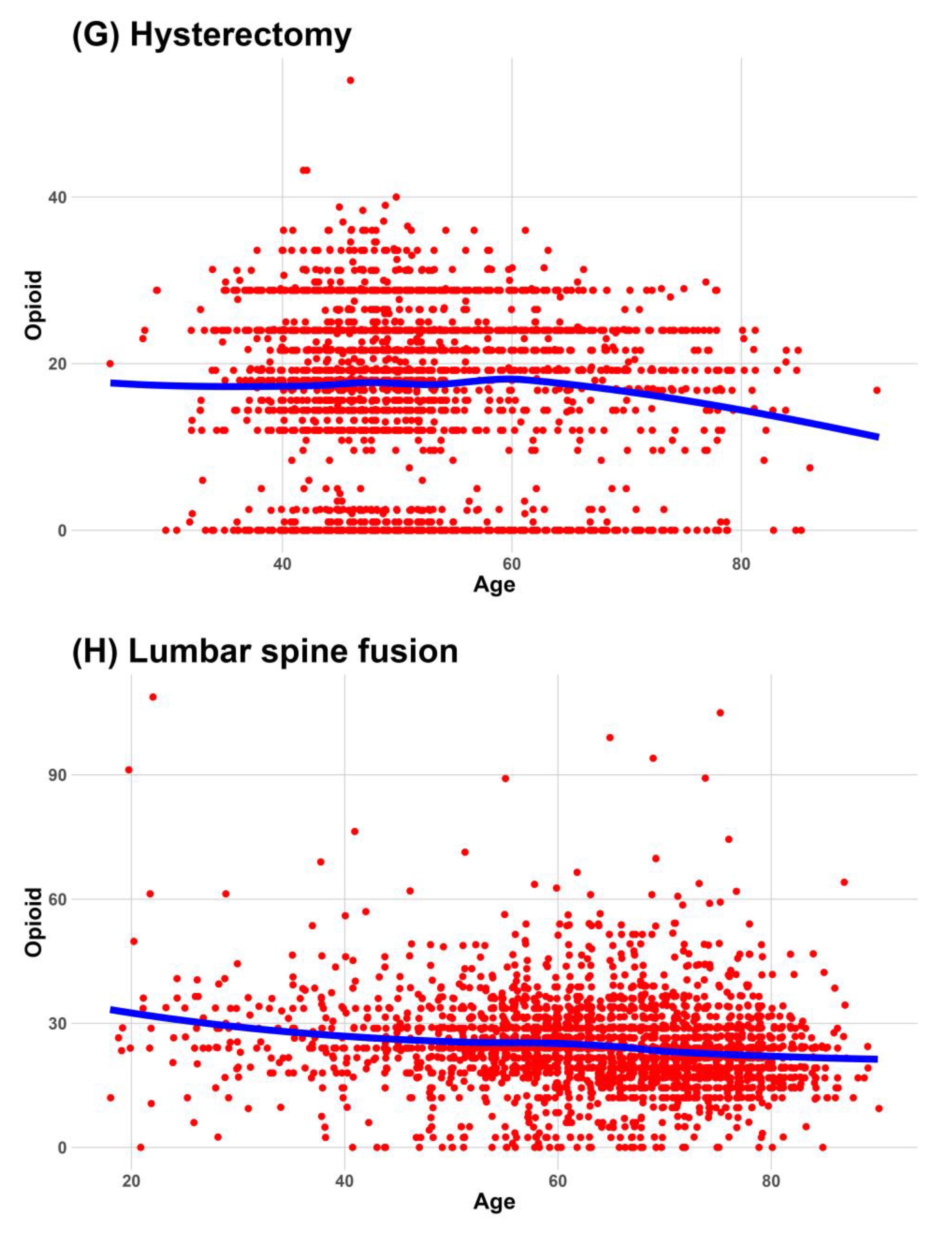
Continuous data were expressed as medians and interquartile ranges, and categorical data were expressed as frequencies and percentages. We used a locally estimated scatterplot smoothing line to fit a smooth curve through the scatterplot of age and NRS. Visualizing the relationship between age and NRS as an optimal-fit curve makes it easier for readers to understand.
Considering the covariates, we analyzed the adjusted association between age and worst pain at 24 h postoperatively using linear regression. The partial R2 between age and NRS score was also calculated. For the subgroup analysis, we analyzed the adjusted association between age and worst pain 24 h postoperatively depending on sex and patient-controlled analgesia (PCA) administration.
Using Bonferroni correction, a
p-value ≤ 0.005 was considered statistically significant. SPSS version 26.0 (IBM, Armonk, NY, USA) was used for all analyses, and graphs were drawn using R version 4.2.3 (R Foundation for Statistical Computing,
www.r-project.org [accessed on 10 September 2023]).
4. Discussion
This study investigated the relationship between age and the worst postoperative pain during the 24 h after surgery in 10 surgical procedures. The worst pain associated with cholecystectomy and lumbar spine fusion decreased consistently and significantly with increasing age in all analyses, including the subgroup analysis. These were also included in six surgeries (ARCR, cholecystectomy, hip hemiarthroplasty, lumbar spine fusion, THA, and TKA), which decreased the administered dose of opioids with age. However, considering a 2.4 unit reduction in the NRS is required for clinically meaningful pain relief in moderate or severe pain [
15], only lumbar spine fusion showed clinical and statistical decreases in pain with age consistently and significantly in several analyses.
Jacqueline et al. reported an association between postoperative pain and age using an international database of hip replacement, knee replacement, spinal fusion, and laparoscopic surgery [
12]. Their study included various pain measurements such as worst pain, pain associated with moving, breathing/coughing, and sleeping, and the worst postoperative pain decreased with increasing age in all four types of surgeries. Our study included the types of surgeries used in their study; however, there were several differences between them. Our analyses did not all consistently show a decrease in worst pain with increasing age in hip hemiarthroplasty, THA, TKA, or laparoscopic cholecystectomy, except for lumbar spine fusion. Their worst NRS scores were generally higher than those in our study. The patients in our study who underwent lumbar spinal fusion, THA, TKA, or hip hemiarthroplasty had a worst NRS score approximately 1–2 units lower than others in their study. Considering their higher NRS scores, information on postoperative pain control modalities was insufficient. TKA, THA, hemiarthroplasty, and lumbar spinal fusion have long skin incisions and comparable surgical wounds, and several postoperative pain control modalities, including PCA, can be applied. Therefore, it is difficult to generalize the results without knowing how pain was controlled.
However, two studies reported an association between age and postoperative pain in patients using analgesic methods. Koh JC et al. investigated postoperative pain in young (age 20–39 years) and older adult (age ≥ 70 years) patients with patient-controlled epidural analgesia application [
11]. Although they did not analyze the type of surgery, the mean NRS score for pain intensity within 24 h was 3–5. Young patients had significantly more severe pain than older adult patients 6 h after surgery. Barrington et al. studied postoperative pain after TKA in patients who received local analgesic injections [
10]. They investigated average pain intensity using the visual analog scale (VAS) and age-reduced pain intensity using multivariate regression analysis for overall average VAS pain scores. Our study also showed that increasing age decreased pain intensity in patients who received PCA. However, the two previous studies did not investigate the worst pain separately, and the overall pain intensity of patients with pain control was not high. One study showed that the differences in NRS scores between old and young patients were <1 unit [
11]. In our study, the median worst pain intensity in patients who received PCA was <4 in several surgeries. In patients with low pain intensity, the clinical effect of age on pain intensity was not statistically significant.
In our study, we found that the median NRS worst pain score was the same in all patients and in patients who received PCA in seven surgeries that had a high percentage of PCA administration, such as ARCR, C/sec, hip hemiarthroplasty, hysterectomy, lumbar spine fusion, THA, and TKA. In contrast, in surgeries with a low percentage of PCA administration, such as cholecystectomy and herniorrhaphy, the median NRS worst pain score in patients who received PCA was lower than that in all patients. These results were consistent with the order of the administered median doses of opioids according to surgery. According to the administered opioid dose, the top seven surgeries were those that had the same median NRS for patients with and without PCA, while the bottom three surgeries were those that had different median NRS for patients with and without PCA. However, to clarify the association between opioids and the worst pain, further studies that consider the adverse effects of high doses of opioids are needed.
The effects of aging on pain intensity should be considered based on several factors. Aging is associated with anatomical and neurochemical changes [
16] affecting pain perception. Aging is associated with increased pain thresholds [
17,
18] and reflects reduced pain sensitivity [
19]. It has been reported that pain intensity in chronic pain does not vary with age [
20,
21,
22]; however, acute pain can be caused by damage, such as surgery, and is related to skeletal muscle spasms and sympathetic nervous system activation [
23]. An experimental study showed that aging affects the fast initial pain response but does not affect the sustained pain response [
24]. The effect of age on pain intensity may differ according to surgery as pain threshold differs according to the size of the surgery and the peripheral cutaneous or visceral sites [
17].
The relationship observed between age and postoperative pain intensity in various surgical procedures should be considered the potential role of pharmacokinetics, especially in the context of opioids. Opioids are commonly used analgesics for postoperative pain management, and their pharmacokinetic profiles can vary with age, which could potentially impact pain outcomes in the elderly [
25]. Elderly patients often show a decrease in hepatic enzyme activity, which can lead to an extended half-life of opioids [
26], which can impact pain relief. Aging is also associated with changes in receptor sensitivity, including opioid receptors, so elderly patients may respond differently to opioids than younger patients [
27,
28]. Given these pharmacokinetic considerations, the variable effects of age on postoperative pain intensity observed in this study may be partly due to differences in the way opioids are metabolized and utilized in elderly patients compared to younger individuals.
The strength of this study is that it focused on 10 types of surgeries, which may represent the various spectra of surgical procedures, and investigated patients using pain control modalities, such as PCA. However, this study has some limitations:
The present study used the NRS to assess pain intensity. Although the NRS is a commonly used tool, it is subjective and may not capture the full complexity of pain experiences. Nonetheless, it provides a structured format, has good sensitivity, and generates data that can be statistically analyzed for audit purposes compared to the VAS, which may reduce variability in interpretation [
29,
30,
31].
This study focused on postoperative pain within 24 h after surgery. Pain experiences might change over an extended period, and considering pain trajectories beyond the first 24 h could provide additional insights.
This study acknowledges that various pain control modalities may have been used and that some data may be heterogeneous, except for PCA, which could have influenced pain intensity. Recently, multimodal analgesic methods are used, even in minor surgeries such as laparoscopic cholecystectomy and inguinal hernia repair [
29,
30]. Specific details regarding the types of analgesic methods and their dosages, except for included factors, are yet to be discussed, making it challenging to understand their full impact on the results.
While our intention was to assemble a diverse dataset to bolster the generalizability of our results, this study may be susceptible to potential biases stemming from variations in hospital protocols, patient populations, and data-collection methodologies. Moreover, these variations may potentially influence the observed outcomes.
In conclusion, this study provided valuable insights into the relationship between patient age and postoperative pain during various surgical procedures. Although age influences postoperative pain intensity in some surgeries, the findings are inconsistent across all procedures. They can differ according to the type of surgery and PCA administration. These findings suggest that the impact of pain control modalities emphasizes the importance of personalized pain management approaches. Future research should address the limitations of this study and explore additional factors that might influence postoperative pain to enable better pain management practices and improve patient outcomes.