Dynamic Navigation System vs. Free-Hand Approach in Microsurgical and Non-Surgical Endodontics: A Systematic Review and Meta-Analysis of Experimental Studies
Abstract
:1. Introduction
2. Methods
2.1. Eligibility Criteria
2.2. Information Sources and Search Strategy
2.3. Selection and Data Collection Process
2.4. Data Items and Statistical Analysis
2.5. Risk of Bias Assessment
3. Results
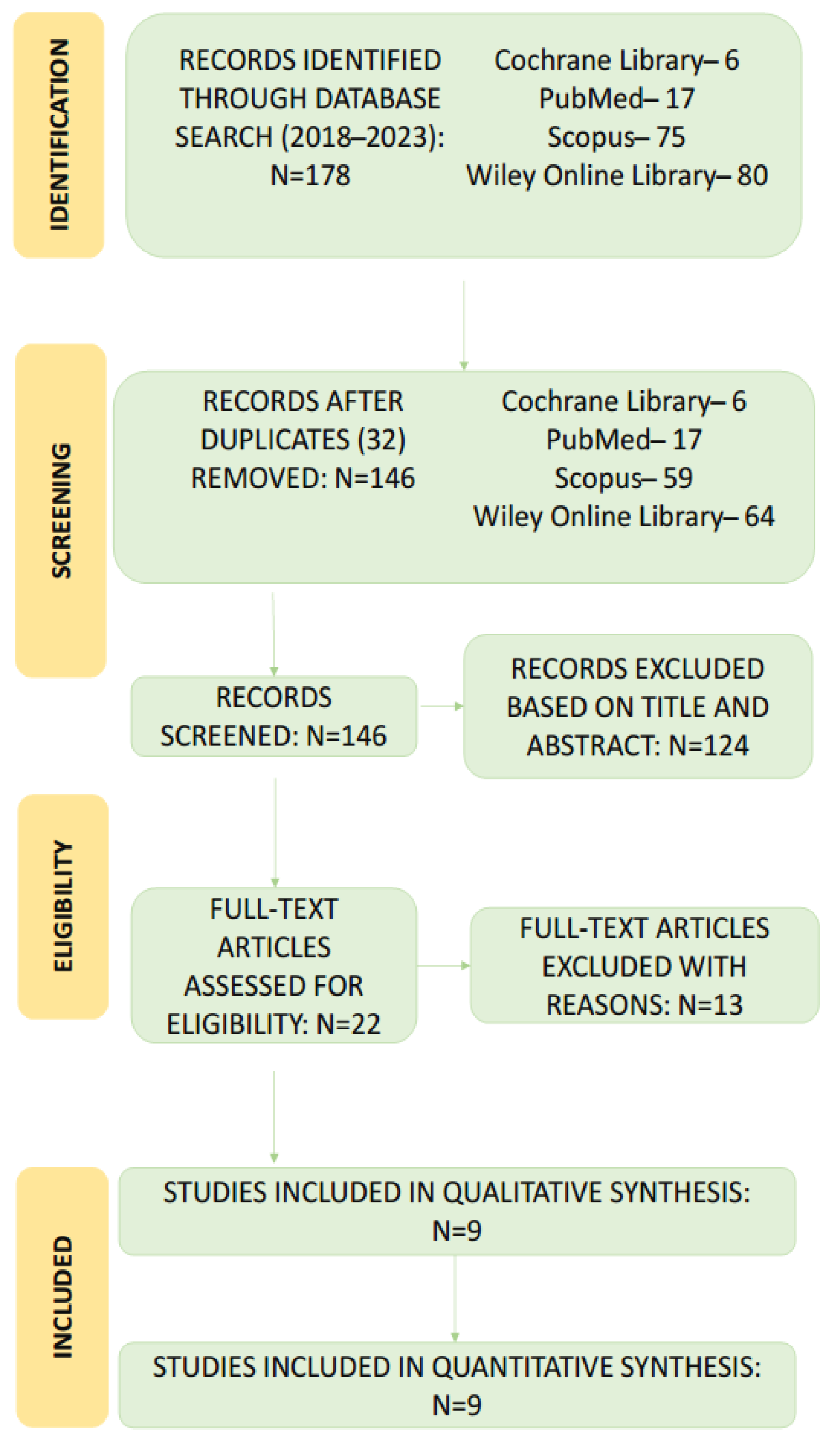
3.1. Study Selection
3.2. Study Characteristics
3.3. Risk of Bias in Studies
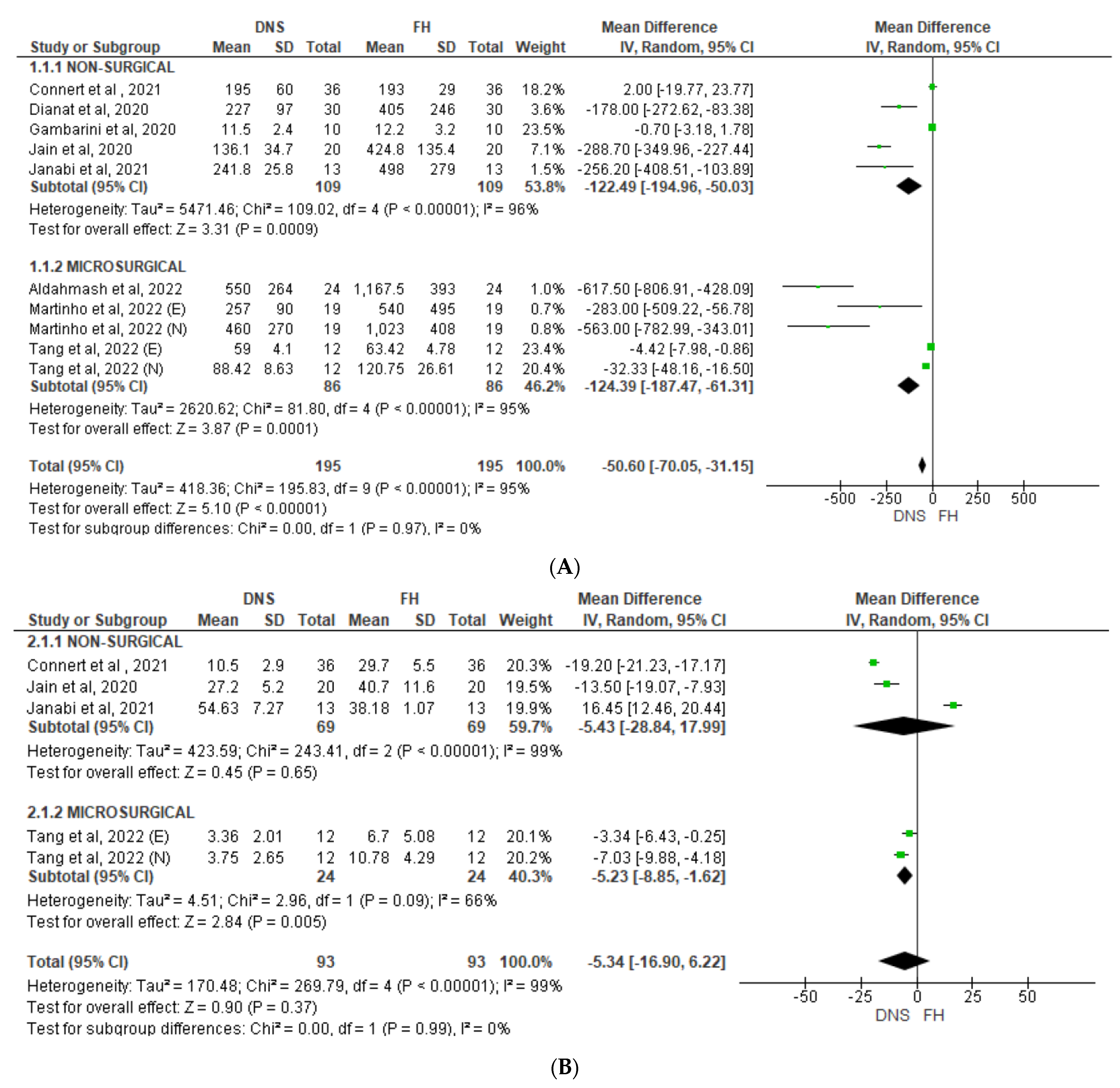
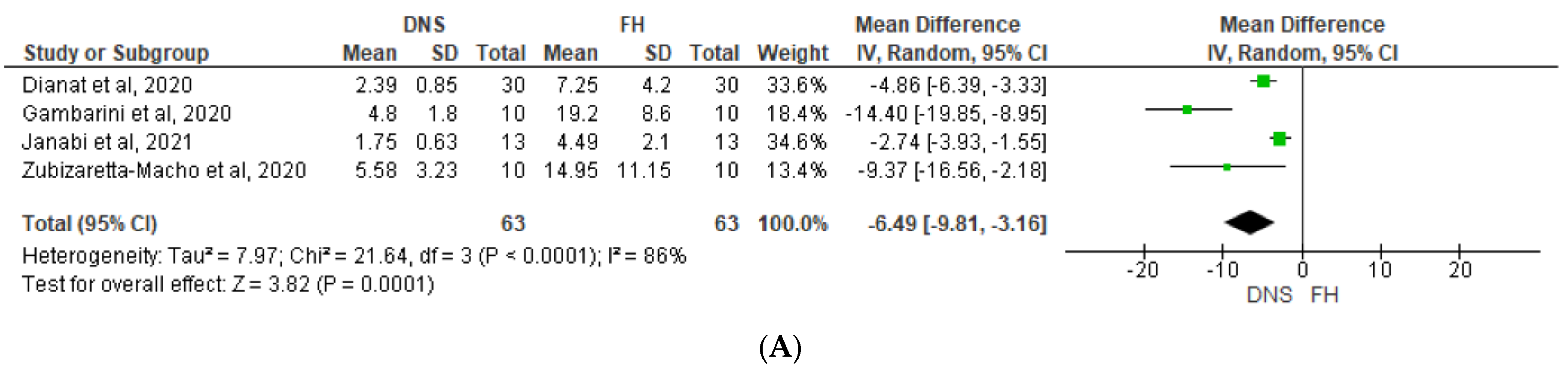
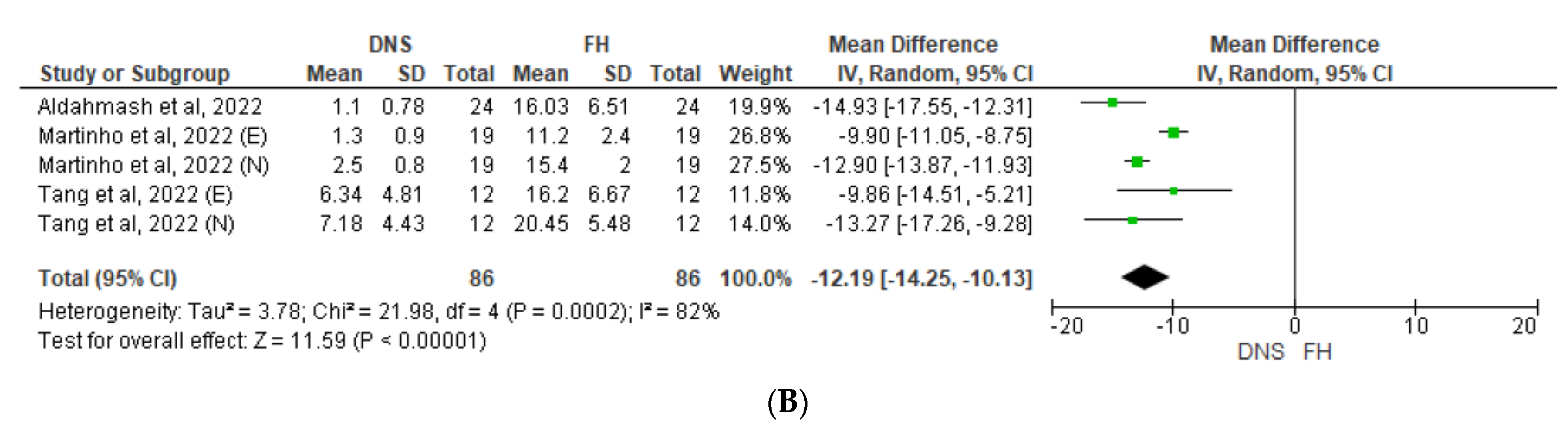
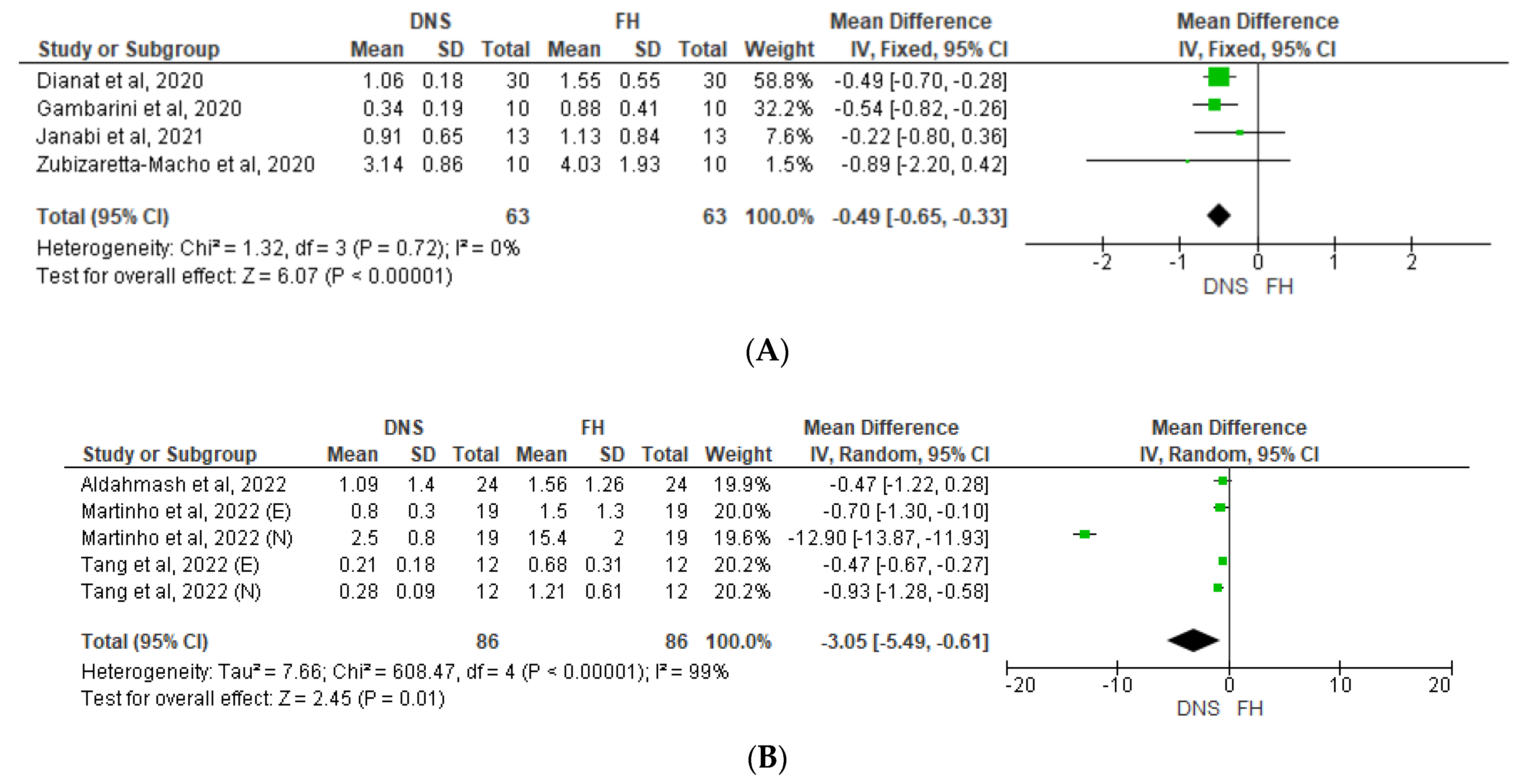
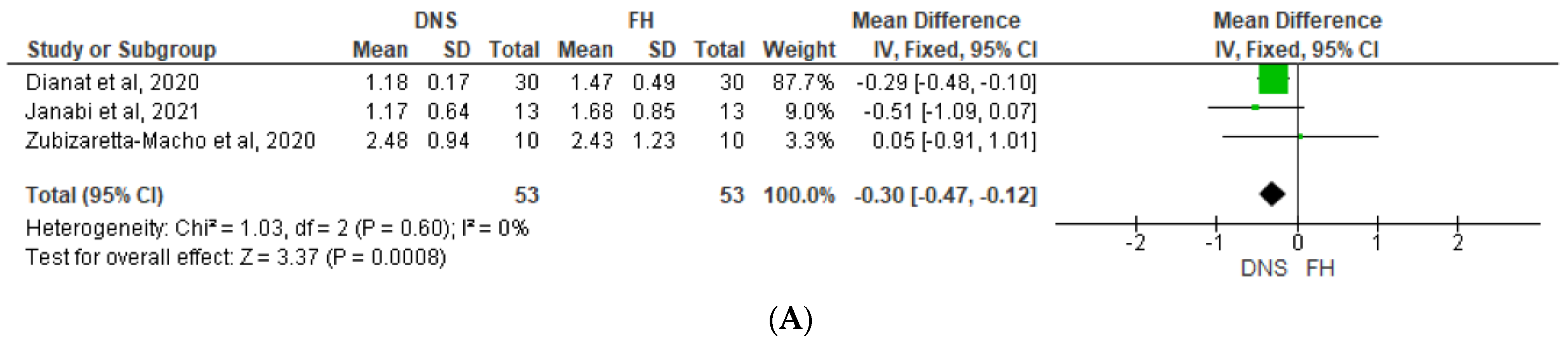
3.4. Results of Individual Studies and Syntheses: Meta-Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bardales-Alcocer, J.; Ramírez-Salomón, M.; Vega-Lizama, E.; López-Villanueva, M.; Alvarado-Cárdenas, G.; Serota, K.S.; Ramírez-Wong, J. Endodontic Retreatment Using Dynamic Navigation: A Case Report. J. Endod. 2021, 47, 1007–1013. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.D.; Carrico, C.K.; Bermanis, I.; Rehil, S. Intraosseous Anesthesia Using Dynamic Navigation Technology. J. Endod. 2020, 46, 1894–1900. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.D.; Carrico, C.K.; Bermanis, I. 3-Dimensional Accuracy of Dynamic Navigation Technology in Locating Calcified Canals. J. Endod. 2020, 46, 839–845. [Google Scholar] [CrossRef] [PubMed]
- Lara-Mendes, S.T.O.; Barbosa, C.d.F.M.; Machado, V.C.; Santa-Rosa, C.C. A New Approach for Minimally Invasive Access to Severely Calcified Anterior Teeth Using the Guided Endodontics Technique. J. Endod. 2018, 44, 1578–1582. [Google Scholar] [CrossRef] [PubMed]
- Pujol, M.L.; Vidal, C.; Mercadé, M.; Muñoz, M.; Ortolani-Seltenerich, S. Guided Endodontics for Managing Severely Calcified Canals. J. Endod. 2021, 47, 315–321. [Google Scholar] [CrossRef]
- Tavares, W.L.F.; Viana, A.C.D.; Machado, V.d.C.; Henriques, L.C.F.; Sobrinho, A.P.R. Guided Endodontic Access of Calcified Anterior Teeth. J. Endod. 2018, 44, 1195–1199. [Google Scholar] [CrossRef]
- Panchal, N.; Mahmood, L.; Retana, A.; Emery, R. Dynamic Navigation for Dental Implant Surgery. Oral Maxillofac. Surg. Clin. N. Am. 2019, 31, 539–547. [Google Scholar] [CrossRef]
- Zehnder, M.S.; Connert, T.; Weiger, R.; Krastl, G.; Kühl, S. Guided endodontics: Accuracy of a novel method for guided access cavity preparation and root canal location. Int. Endod. J. 2016, 49, 966–972. [Google Scholar] [CrossRef]
- Strbac, G.D.; Schnappauf, A.; Giannis, K.; Moritz, A.; Ulm, C. Guided Modern Endodontic Surgery: A Novel Approach for Guided Osteotomy and Root Resection. J. Endod. 2017, 43, 496–501. [Google Scholar] [CrossRef]
- Buchgreitz, J.; Buchgreitz, M.; Bjørndal, L. Guided root canal preparation using cone beam computed tomography and optical surface scans—An observational study of pulp space obliteration and drill path depth in 50 patients. Int. Endod. J. 2019, 52, 559–568. [Google Scholar] [CrossRef]
- Jain, S.D.; Saunders, M.W.; Carrico, C.K.; Jadhav, A.; Deeb, J.G.; Myers, G.L. Dynamically Navigated versus Freehand Access Cavity Preparation: A Comparative Study on Substance Loss Using Simulated Calcified Canals. J. Endod. 2020, 46, 1745–1751. [Google Scholar] [CrossRef]
- Simon, J.C.; Kwok, J.W.; Vinculado, F.; Fried, D. Computer-Controlled CO2 Laser Ablation System for Cone-beam Computed Tomography and Digital Image Guided Endodontic Access: A Pilot Study. J. Endod. 2021, 47, 1445–1452. [Google Scholar] [CrossRef] [PubMed]
- Dianat, O.; Nosrat, A.; Tordik, P.A.; Aldahmash, S.A.; Romberg, E.; Price, J.B.; Mostoufi, B. Accuracy and Efficiency of a Dynamic Navigation System for Locating Calcified Canals. J. Endod. 2020, 46, 1719–1725. [Google Scholar] [CrossRef] [PubMed]
- Leontiev, W.; Connert, T.; Weiger, R.; Krastl, G.; Magni, E. Dynamic Navigation in Endodontics: Guided Access Cavity Preparation by Means of a Miniaturized Navigation System. J. Vis. Exp. 2022, 183, e63687. [Google Scholar] [CrossRef]
- Liu, S.M.; Zhao, Y.J.; Wang, X.Y.; Wang, Z.H. In vitro evaluation of positioning accuracy of trephine bur at different depths by dynamic navigation. J. Peking. Univ. (Health Sci.) 2022, 54, 146–152. [Google Scholar] [CrossRef]
- Zubizarreta-Macho, Á.; Castaño, S.V.; Montiel-Company, J.M.; Mena-Álvarez, J. Effect of Computer-Aided Navigation Techniques on the Accuracy of Endodontic Access Cavities: A Systematic Review and Meta-Analysis. Biology 2021, 10, 212. [Google Scholar] [CrossRef]
- Plotino, G.; Grande, N.M.; Isufi, A.; Ioppolo, P.; Pedullà, E.; Bedini, R.; Gambarini, G.; Testarelli, L. Fracture Strength of Endodontically Treated Teeth with Different Access Cavity Designs. J. Endod. 2017, 43, 995–1000. [Google Scholar] [CrossRef]
- Connert, T.; Krug, R.; Eggmann, F.; Emsermann, I.; ElAyouti, A.; Weiger, R.; Kühl, S.; Krastl, G. Guided Endodontics versus Conventional Access Cavity Preparation: A Comparative Study on Substance Loss Using 3-dimensional–printed Teeth. J. Endod. 2019, 45, 327–331. [Google Scholar] [CrossRef]
- Connert, T.; Zehnder, M.S.; Amato, M.; Weiger, R.; Kühl, S.; Krastl, G. Microguided Endodontics: A method to achieve minimally invasive access cavity preparation and root canal location in mandibular incisors using a novel computer-guided technique. Int. Endod. J. 2018, 51, 247–255. [Google Scholar] [CrossRef]
- Chong, B.S.; Dhesi, M.; Makdissi, J. Computer-aided dynamic navigation: A novel method for guided endodontics. Quintessence Int. 2019, 50, 196–202. [Google Scholar] [CrossRef]
- Connert, T.; Weiger, R.; Krastl, G. Present status and future directions—Guided endodontics. Int. Endod. J. 2022, 55, 995–1002. [Google Scholar] [CrossRef] [PubMed]
- Gambarini, G.; Galli, M.; Stefanelli, L.V.; Di Nardo, D.; Morese, A.; Seracchiani, M.; De Angelis, F.; Di Carlo, S.; Testarelli, L. Endodontic Microsurgery Using Dynamic Navigation System: A Case Report. J. Endod. 2019, 45, 1397–1402. [Google Scholar] [CrossRef] [PubMed]
- Iandolo, A.; Iandolo, G.; Malvano, M.; Pantaleo, G.; Simeone, M. Modern technologies in Endodontics. Ital. Endod. 2016, 30, 2–9. [Google Scholar] [CrossRef]
- Tchorz, J.P.; Wrbas, K.-T.; Hellwig, E. Guided endodontic access of a calcified mandibular central incisor using a software-based three-dimensional treatment plan. Int. J. Comp. Dent. 2019, 22, 273–281. Available online: https://www.ncbi.nlm.nih.gov/pubmed/31463491 (accessed on 26 August 2019).
- Torres, A.; Boelen, G.; Lambrechts, P.; Pedano, M.S.; Jacobs, R. Dynamic navigation: A laboratory study on the accuracy and potential use of guided root canal treatment. Int. Endod. J. 2021, 54, 1659–1667. [Google Scholar] [CrossRef]
- Moreno-Rabié, C.; Torres, A.; Lambrechts, P.; Jacobs, R. Clinical applications, accuracy and limitations of guided endodontics: A systematic review. Int. Endod. J. 2022, 53, 214–223. [Google Scholar] [CrossRef]
- Connert, T.; Leontiev, W.; Dagassan-Berndt, D.; Kühl, S.; ElAyouti, A.; Krug, R.; Krastl, G.; Weiger, R. Real-Time Guided Endodontics with a Miniaturized Dynamic Navigation System Versus Conventional Freehand Endodontic Access Cavity Preparation: Substance Loss and Procedure Time. J. Endod. 2021, 10, 1651–1656. [Google Scholar] [CrossRef]
- Jonaityte, E.M.; Bilvinaite, G.; Drukteinis, S.; Torres, A. Accuracy of Dynamic Navigation for Non-Surgical Endodontic Treatment: A Systematic Review. J. Clin. Med. 2022, 11, 3441. [Google Scholar] [CrossRef]
- Sampath, D.T.; Natanasabapathy, V. Dynamic navigation in guided endodonticsA systematic review. Eur. Endod. J. 2022, 7, 81–91. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Nagendrababu, V.; Dilokthornsakul, P.; Jinatongthai, P.; Veettil, S.K.; Pulikkotil, S.J.; Duncan, H.F.; Dummer, P.M.H. Glossary for systematic reviews and meta-analyses. Int. Endod. J. 2020, 53, 232–249. [Google Scholar] [CrossRef] [PubMed]
- Nagendrababu, V.; Duncan, H.F.; Tsesis, I.; Sathorn, C.; Pulikkotil, S.J.; Dharmarajan, L.; Dummer, P.M.H. PRISMA for abstracts: Best practice for reporting abstracts of systematic reviews in Endodontology. Int. Endod. J. 2019, 52, 1096–1107. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. British. Med. J. (Clin. Res. Ed.) 2021, 372, n71. [Google Scholar] [CrossRef]
- Scholten, R.J.P.M.; Clarke, M.; Hetherington, J. The Cochrane Collaboration. Eur. J. Clin. Nutr. 2005, 59, S147–S149. [Google Scholar] [CrossRef] [PubMed]
- Sheth, V.H.; Shah, N.P.; Jain, R.; Bhanushali, N.; Bhatnagar, V. Development and validation of a risk-of-bias tool for assessing in vitro studies conducted in dentistry: The QUIN. J. Prosthet. Dent. 2022, 22, 345–346. [Google Scholar] [CrossRef]
- Dianat, O.; Gupta, S.; Price, J.B.; Mostoufi, B. Guided Endodontic Access in a Maxillary Molar Using a Dynamic Navigation System. J. Endod. 2021, 47, 658–662. [Google Scholar] [CrossRef]
- Chen, C.; Zhang, R.; Zhang, W.; Li, F.; Wang, Z.; Qin, L.; Chen, Y.; Bian, Z.; Meng, L. Clinical and radiological outcomes of dynamic navigation in endodontic microsurgery: A prospective study. Clin. Oral Investig. 2023. [Google Scholar] [CrossRef]
- Karim, M.H.; Faraj, B.M. Comparative Evaluation of a Dynamic Navigation System versus a Three-dimensional Microscope in Retrieving Separated Endodontic Files: An In Vitro Study. J. Endod. 2023. [Google Scholar] [CrossRef]
- Martinho, F.C.; Griffin, I.L.; Price, J.B.; Tordik, P.A. Augmented Reality and 3-Dimensional Dynamic Navigation System Integration for Osteotomy and Root-end Resection. J. Endod. 2023. [Google Scholar] [CrossRef]
- Aldahmash, S.A.; Price, J.B.; Mostoufi, B.; Griffin, I.L.; Dianat, O.; Tordik, P.A.; Martinho, F.C. Real-time 3d image-guided navigation system in endodontic microsurgery—A cadaver study. J. Endod. 2022, 48, 922–929. [Google Scholar] [CrossRef] [PubMed]
- Gambarini, G.; Galli, M.; Morese, A.; Stefanelli, L.V.; Abduljabbar, F.; Giovarruscio, M.; Di Nardo, D.; Seracchiani, M.; Testarelli, L. Precision of Dynamic Navigation to Perform Endodontic Ultraconservative Access Cavities: A Preliminary In Vitro Analysis. J. Endod. 2020, 46, 1286–1290. [Google Scholar] [CrossRef] [PubMed]
- Janabi, A.; Tordik, P.A.; Griffin, I.L.; Mostoufi, B.; Price, J.B.; Chand, P.; Martinho, F.C. Accuracy and Efficiency of 3-dimensional Dynamic Navigation System for Removal of Fiber Post from Root Canal–Treated Teeth. J. Endod. 2021, 47, 1453–1460. [Google Scholar] [CrossRef] [PubMed]
- Martinho, F.C.; Aldahmash, S.A.; Cahill, T.Y.; Gupta, S.; Dianat, O.; Mostoufi, B.; Price, J.B.; Griffin, I.; Tordik, P.A. Comparison of the accuracy and efficiency of a 3D dynamic navigation system for osteotomy root-end resection performed by novice and experienced endodontists. J. Endod. 2022, 48, 1327–1333. [Google Scholar] [CrossRef] [PubMed]
- Tang, W.; Jiang, H. Comparison of Static and Dynamic Navigation in Root End Resection Performed by Experienced and Inexperienced Operators: An In Vitro Study. J. Endod. 2022, 49, 294–300. [Google Scholar] [CrossRef]
- Zubizarreta-Macho, Á.; Muñoz, A.d.P.; Deglow, E.R.; Agustín-Panadero, R.; Álvarez, J.M. Accuracy of Computer-Aided Dynamic Navigation Compared to Computer-Aided Static Procedure for Endodontic Access Cavities: An In Vitro Study. J. Clin. Med. 2020, 9, 129. [Google Scholar] [CrossRef]

| # | Authors | Study | Reason of Exclusion |
|---|---|---|---|
| 1 | Chong et al., 2019 [20] | Computer-aided dynamic navigation: a novel method for guided endodontics http://doi.org/10.3290/j.qi.a41921 | No control (freehand) group |
| 2 | Torres et al., 2021 [25] | Dynamic navigation: a laboratory study on the accuracy and potential use of guided root canal treatment http://doi.org/10.1111/iej.13563 | No control (freehand) group |
| 3 | Bardales-Alcocer et al., 2021 [1] | Endodontic retreatment using dynamic navigation http://doi.org/10.1016/j.joen.2021.03.0005 | A case report |
| 4 | Leontiev et al., 2022 [14] | Dynamic navigation in endodontics: guided access cavity preparation by means of a miniaturized navigation system http://doi.org/10.3791/63687 | No control (freehand) group |
| 6 | Dianat et al., 2021 [37] | Guided endodontic access in a maxillary molar using a dynamic navigation system http://doi.org/10.1016/j.joen.2020.09.019 | A case report |
| 7 | Jain et al., 2020 [3] | 3-Dimensional accuracy of dynamic navigation technology in locating calcified canals http://doi.org/10.1016/j.joen.2020.03.014 | No control (freehand) group |
| 8 | Simon et al., 2019 [12] | Computer-controlled CO₂ laser ablation system for cone-beam computed tomography and digital image guided endodontic access: a pilot study http://doi.org/10.1016/j.joen.2021.06.004 | No control (freehand) group |
| 9 | Liu et al., 2022 [15] | In vitro evaluation of positioning accuracy of trephine bur at different depths by dynamic navigation http://doi.org/10.19723/j.issn.1671-167X.2022.01.023 | No control (freehand) group |
| 10 | Gambarini et al., 2019 [22] | Endodontic microsurgery using dynamic navigation system http://doi.org/10.1016/j.joen.2019.07.010 | A case report |
| 11 | Chen et al., 2023 [38] | Clinical and radiological outcomes of dynamic navigation in endodontic microsurgery: a prospective study https://doi.org/10.1007/s00784-023-05152-6 | A clinical study |
| 12 | Karim et al., 2023 [39] | Comparative Evaluation of a Dynamic Navigation System versus a Three-dimensional Microscope in Retrieving Separated Endodontic Files: An In Vitro Study https://doi.org/10.1016/j.joen.2023.06.014 | The study is focused on retrieving broken rotary files |
| 13 | Martinho et al., 2023 [40] | Augmented Reality and 3-Dimensional Dynamic Navigation System Integration for Osteotomy and Root-end Resection https://doi.org/10.1016/j.joen.2023.07.007 | No control (freehand) group |
| Study number | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
| First author | Dianat et al. [13] | Jain et al. [11] | Connert et al. [27] | Gambarini et al. [42] | Janabi et al. [43] | Zubizarreta-Macho et al. [46] | Martinho et al. [44] | Aldahmash et al. [41] | Tang et al. [45] |
| Year | 2020 | 2020 | 2021 | 2020 | 2021 | 2020 | 2022 | 2022 | 2022 |
| Country | USA, Saudi Arabia | USA | Switzerland, Germany | Italy, Saudi Arabia, Russian Federation | USA | Spain | USA, Saudi Arabia | Saudi Arabia, USA | China |
| Study design | IN VITRO | IN VITRO | IN VITRO | IN VITRO | IN VITRO | IN VITRO | IN VITRO | IN VITRO | IN VITRO |
| Teeth | Extracted | 3D printed | 3D printed | Artificial (resin) | Extracted | Extracted | Cadavers’ | Cadavers’ | 3D printed |
| Group | Anterior, premolars | Incisors | Anterior | Upper right first molars | Incisors, canines | Anterior | Anterior, posterior | Anterior, posterior | Anterior, posterior |
| DNS sample size | 30 | 20 | 36 | 10 | 13 | 10 | 19 | 24 | 12 |
| Freehand sample size | 30 | 20 | 36 | 10 | 13 | 10 | 19 | 24 | 12 |
| Operator skill level | E, N | N | E, N | E | E | E | E, N | E | E, N |
| Reported outcomes | |||||||||
| Substance loss | - | + | + | - | + | - | - | - | + |
| Procedural time | + | + | + | + | + | - | + | + | + |
| Angular deviation | + | - | - | + | + | + | + | + | + |
| Linear deviation coronal | + | - | - | + | + | + | + | + | + |
| Linear deviation apical | + | - | - | - | + | + | + | + | + |
| # | Criteria |
|---|---|
| 1 | Clearly stated aims/objectives |
| 2 | Detailed explanation of sample size calculation |
| 3 | Detailed explanation of sampling technique |
| 4 | Details of comparison group |
| 5 | Detailed explanation of methodology |
| 6 | Operator details |
| 7 | Randomization |
| 8 | Method of measurement of outcome |
| 9 | Outcome assessor details |
| 10 | Blinding |
| 11 | Statistical analysis |
| 12 | Presentation of results |
| Study | Score Line | Final Score | Risk of Bias |
|---|---|---|---|
| Aldahmash et al., 2022 [41] | 222222022022 | 83.33% | Low |
| Connert et al., 2021 [27] | 202222122022 | 79.17% | Low |
| Dianat et al., 2020 [13] | 222222022022 | 83.33% | Low |
| Gambarini et al., 2020 [42] | 202221122022 | 75.0% | Low |
| Jain et al., 2020 [11] | 201222022022 | 70.83% | Low |
| Janabi et al., 2021 [43] | 222221022022 | 79.17% | Low |
| Martinho et al., 2022 [44] | 202222222202 | 83.33% | Low |
| Tang et al., 2022 [45] | 202222222202 | 83.33% | Low |
| Zubizaretta-Macho et al., 2020 [46] | 202221022022 | 70.83% | Low |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mekhdieva, E.; Del Fabbro, M.; Alovisi, M.; Scotti, N.; Comba, A.; Berutti, E.; Pasqualini, D. Dynamic Navigation System vs. Free-Hand Approach in Microsurgical and Non-Surgical Endodontics: A Systematic Review and Meta-Analysis of Experimental Studies. J. Clin. Med. 2023, 12, 5845. https://doi.org/10.3390/jcm12185845
Mekhdieva E, Del Fabbro M, Alovisi M, Scotti N, Comba A, Berutti E, Pasqualini D. Dynamic Navigation System vs. Free-Hand Approach in Microsurgical and Non-Surgical Endodontics: A Systematic Review and Meta-Analysis of Experimental Studies. Journal of Clinical Medicine. 2023; 12(18):5845. https://doi.org/10.3390/jcm12185845
Chicago/Turabian StyleMekhdieva, Elina, Massimo Del Fabbro, Mario Alovisi, Nicola Scotti, Allegra Comba, Elio Berutti, and Damiano Pasqualini. 2023. "Dynamic Navigation System vs. Free-Hand Approach in Microsurgical and Non-Surgical Endodontics: A Systematic Review and Meta-Analysis of Experimental Studies" Journal of Clinical Medicine 12, no. 18: 5845. https://doi.org/10.3390/jcm12185845
APA StyleMekhdieva, E., Del Fabbro, M., Alovisi, M., Scotti, N., Comba, A., Berutti, E., & Pasqualini, D. (2023). Dynamic Navigation System vs. Free-Hand Approach in Microsurgical and Non-Surgical Endodontics: A Systematic Review and Meta-Analysis of Experimental Studies. Journal of Clinical Medicine, 12(18), 5845. https://doi.org/10.3390/jcm12185845










