Functional (Re)Development of SYNTAX Score II 2020: Predictive Performance and Risk Assessment
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Anatomic Versus Functional Syntax Score II 2020
3.2. Prognostic Stratification of Anatomic and Functional Syntax Score II 2020
4. Discussion
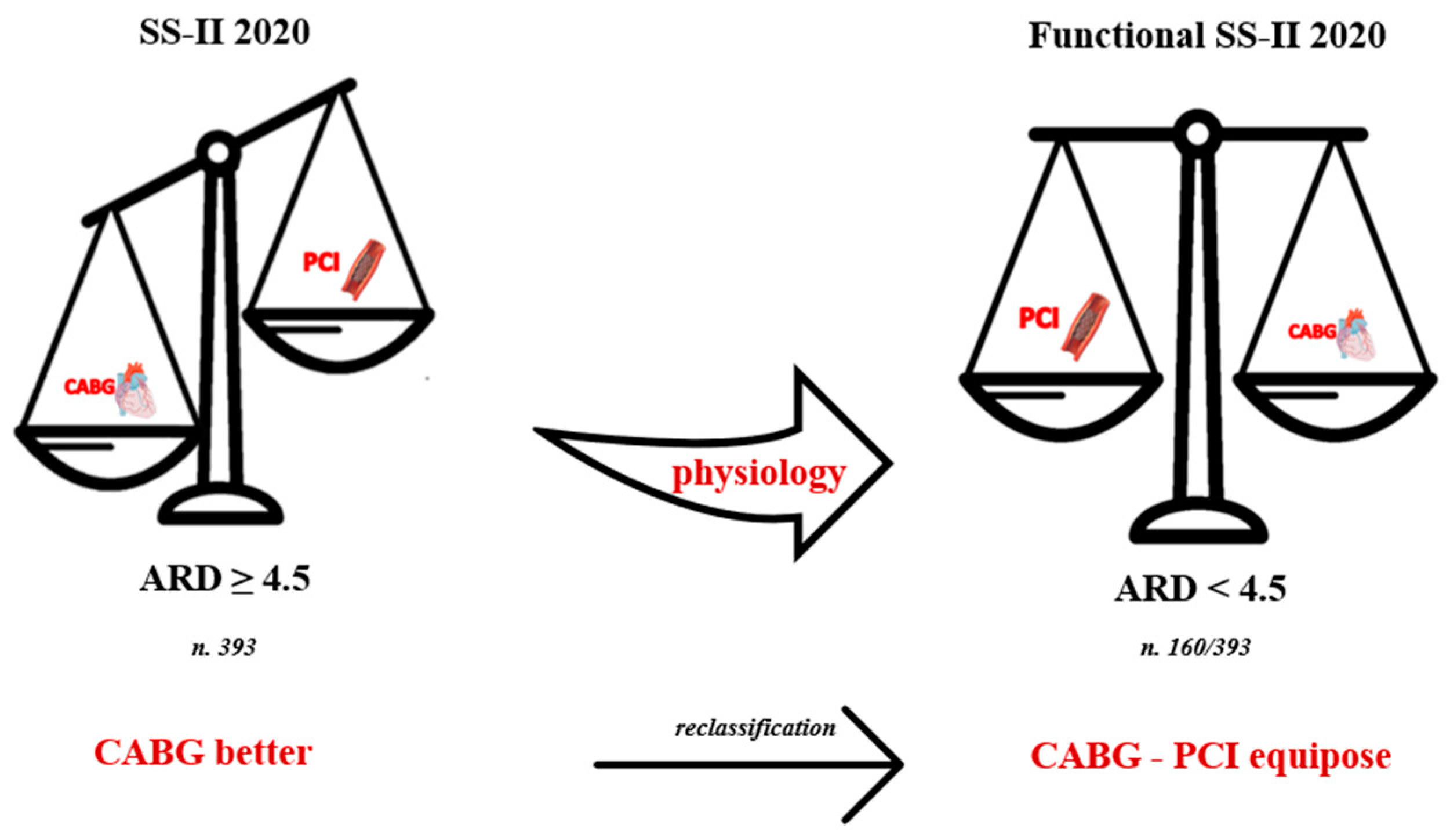
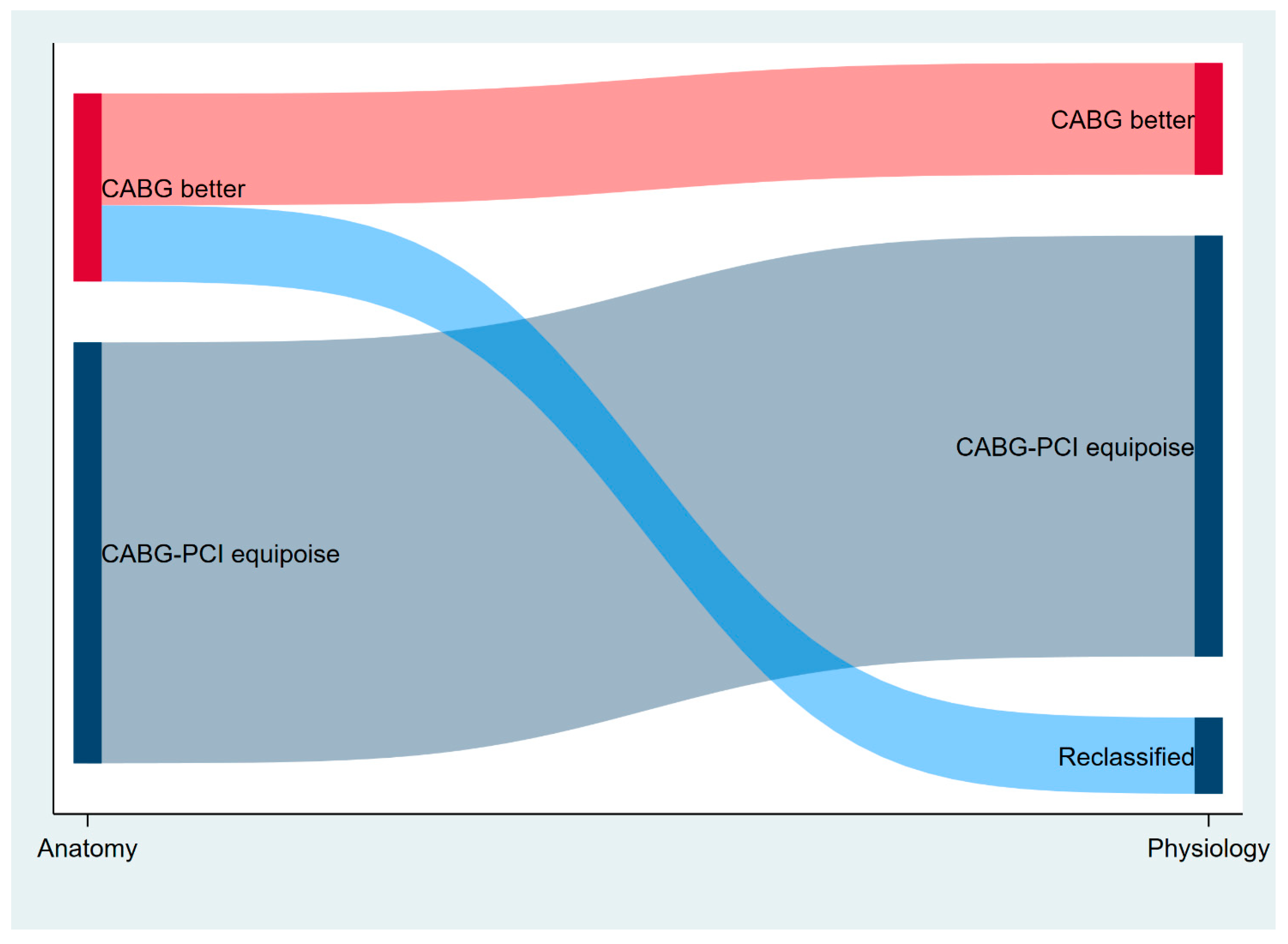
- The functional Syntax Score II 2020 reclassifies a significant portion of patients (≈40%) towards the equipoise between CABG and PCI, namely an ARD < 4.5% if compared to the anatomic Syntax Score II 2020.
- Kaplan–Meier curves showed no difference in survival estimates for the equipoise group based on anatomic Syntax Score II 2020 and those reclassified as equipoise after physiology assessment. In both cases, survival was greater if compared to the CABG better group.
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Neumann, F.-J.; Sousa-Uva, M.; Ahlsson, A.; Alfonso, F.; Banning, A.P.; Benedetto, U.; Byrne, R.A.; Collet, J.-P.; Falk, V.; Head, S.J.; et al. 2018 ESC/EACTS Guidelines on Myocardial Revascularization. Eur. Heart J. 2019, 40, 87–165. [Google Scholar] [CrossRef] [PubMed]
- Hlatky, M.A.; Boothroyd, D.B.; Bravata, D.M.; Boersma, E.; Booth, J.; Brooks, M.M.; Carrié, D.; Clayton, T.C.; Danchin, N.; Flather, M.; et al. Coronary Artery Bypass Surgery Compared with Percutaneous Coronary Interventions for Multivessel Disease: A Collaborative Analysis of Individual Patient Data from Ten Randomised Trials. Lancet 2009, 373, 1190–1197. [Google Scholar] [CrossRef] [PubMed]
- Farkouh, M.E.; Domanski, M.; Sleeper, L.A.; Siami, F.S.; Dangas, G.; Mack, M.; Fuster, V. Strategies for Multivessel Revascularization in Patients with Diabetes. N. Engl. J. Med. 2012, 367, 2375–2384. [Google Scholar] [CrossRef] [PubMed]
- Park, S.-J.; Ahn, J.-M.; Kim, Y.-H.; Park, D.-W.; Yun, S.-C.; Lee, J.-Y.; Kang, S.-J.; Lee, S.-W.; Lee, C.W.; Park, S.-W.; et al. Trial of Everolimus-Eluting Stents or Bypass Surgery for Coronary Disease. N. Engl. J. Med. 2015, 372, 1204–1212. [Google Scholar] [CrossRef] [PubMed]
- Fearon, W.F.; Zimmermann, F.M.; de Bruyne, B.; Piroth, Z.; van Straten, A.H.M.; Szekely, L.; Davidavičius, G.; Kalinauskas, G.; Mansour, S.; Kharbanda, R.; et al. Fractional Flow Reserve–Guided PCI as Compared with Coronary Bypass Surgery. N. Engl. J. Med. 2022, 386, 128–137. [Google Scholar] [CrossRef] [PubMed]
- Enezate, T.; Omran, J.; Al-Dadah, A.S.; Alpert, M.; White, C.J.; Abu-Fadel, M.; Aronow, H.; Cohen, M.; Aguirre, F.; Patel, M.; et al. Fractional flow reserve versus angiography guided percutaneous coronary intervention: An updated systematic review. Catheter. Cardiovasc. Interv. 2018, 92, 18–27. [Google Scholar] [CrossRef]
- Serruys, P.W.; Morice, M.-C.; Kappetein, A.P.; Colombo, A.; Holmes, D.R.; Mack, M.J.; Ståhle, E.; Feldman, T.E.; van den Brand, M.; Bass, E.J.; et al. Percutaneous Coronary Intervention versus Coronary-Artery Bypass Grafting for Severe Coronary Artery Disease. N. Engl. J. Med. 2009, 360, 961–972. [Google Scholar] [CrossRef] [PubMed]
- Banning, A.P.; Serruys, P.; de Maria, G.L.; Ryan, N.; Walsh, S.; Gonzalo, N.; Jan Van Geuns, R.; Onuma, Y.; Sabate, M.; Davies, J.; et al. Five-Year Outcomes after State-of-the-Art Percutaneous Coronary Revascularization in Patients with de Novo Three-Vessel Disease: Final Results of the SYNTAX II Study. Eur. Heart J. 2022, 43, 1307–1316. [Google Scholar] [CrossRef] [PubMed]
- Nam, C.W.; Mangiacapra, F.; Entjes, R.; Chung, I.S.; Sels, J.W.; Tonino, P.A.L.; de Bruyne, B.; Pijls, N.H.J.; Fearon, W.F. Functional SYNTAX Score for Risk Assessment in Multivessel Coronary Artery Disease. J. Am. Coll. Cardiol. 2011, 58, 1211–1218. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, K.; Serruys, P.W.; Fuster, V.; Farkouh, M.E.; Spertus, J.A.; Cohen, D.J.; Park, S.J.; Park, D.W.; Ahn, J.M.; Kappetein, A.P.; et al. Redevelopment and Validation of the SYNTAX Score II to Individualise Decision Making between Percutaneous and Surgical Revascularisation in Patients with Complex Coronary Artery Disease: Secondary Analysis of the Multicentre Randomised Controlled SYNTAXES Trial with External Cohort Validation. Lancet 2020, 396, 1399–1412. [Google Scholar] [PubMed]
- Hara, H.; Shiomi, H.; van Klaveren, D.; Kent, D.M.; Steyerberg, E.W.; Garg, S.; Onuma, Y.; Kimura, T.; Serruys, P.W. External Validation of the SYNTAX Score II 2020. J. Am. Coll. Cardiol. 2021, 78, 1227–1238. [Google Scholar] [CrossRef] [PubMed]
- Tebaldi, M.; Gallo, F.; Scoccia, A.; Durante, A.; Tedeschi, D.; Verdoliva, S.; Cortese, B.; Bilotta, F.; Watkins, S.; Ielasi, A.; et al. Clinical Outcome of FFR-Guided Revascularization Strategy of Coronary Lesions: The HALE-BOPP Study. Rev. Cardiovasc. Med. 2023, 24, 62. [Google Scholar] [CrossRef]
- Farooq, V.; Van Klaveren, D.; Steyerberg, E.W.; Meliga, E.; Vergouwe, Y.; Chieffo, A.; Kappetein, A.P.; Colombo, A.; Holmes, D.R.; MacK, M.; et al. Anatomical and Clinical Characteristics to Guide Decision Making between Coronary Artery Bypass Surgery and Percutaneous Coronary Intervention for Individual Patients: Development and Validation of SYNTAX Score II. Lancet 2013, 381, 639–650. [Google Scholar] [CrossRef] [PubMed]
- Park, S.-J.; Kim, Y.-H.; Park, D.-W.; Yun, S.-C.; Ahn, J.-M.; Song, H.G.; Lee, J.-Y.; Kim, W.-J.; Kang, S.-J.; Lee, S.-W.; et al. Randomized Trial of Stents versus Bypass Surgery for Left Main Coronary Artery Disease. N. Engl. J. Med. 2011, 364, 1718–1727. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, Y.; Lønborg, J.; Jong, A.; Nishi, T.; De Bruyne, B.; Høfsten, D.E.; Kelbæk, H.; Layland, J.; Nam, C.W.; Pijls, N.H.J.; et al. Prognostic Value of the Residual SYNTAX Score After Functionally Complete Revascularization in ACS. J. Am. Coll. Cardiol. 2018, 72, 1321–1329. [Google Scholar] [CrossRef] [PubMed]
- Ciccarelli, G.; Barbato, E.; Toth, G.G.; Gahl, B.; Xaplanteris, P.; Fournier, S.; Milkas, A.; Bartunek, J.; Vanderheyden, M.; Pijls, N.; et al. Angiography Versus Hemodynamics to Predict the Natural History of Coronary Stenoses: Fractional Flow Reserve Versus Angiography in Multivessel Evaluation 2 Substudy. Circulation 2018, 137, 1475–1485. [Google Scholar] [CrossRef] [PubMed]


| Patients (n = 1274) | |
|---|---|
| Age, years | 68 ± 10 |
| Female, no. (%) | 354 (28) |
| BMI, Kg/m2 | 28 ± 4 |
| Clinical history, no. (%) | |
| Hypertension | 1001 (78) |
| Hyperlipidemia | 886 (69) |
| Current smoking | 239 (18) |
| Diabetes mellitus | 324 (25) |
| NID-DM | 276 (21) |
| ID-DM | 48 (3) |
| Prior IHD | 472 (37) |
| Prior MI | 320 (25) |
| Prior PCI | 422 (33) |
| Prior CVA | 60 (4) |
| Peripheral artery disease | 357 (27) |
| COPD | 71 (5) |
| CKD | 332 (25) |
| Clinical presentation, no. (%) | |
| ACS | 650 (50) |
| STEMI | 169 (13) |
| NSTEMI | 465 (36) |
| UA | 16 (1) |
| CCS | 655 (50) |
| Stress test | 248 (44) |
| Imaging stress test | 88 (36) |
| Positive stress test | 226 (91) |
| LVEF, % | 53 ± 9 |
| LVEF < 40% | 180 (14) |
| Three Vessel Disease | 899 (68) |
| Discharge medication, no. (%) | |
| Aspirin | 1280 (98) |
| P2Y12 inhibitors | 1243 (95) |
| Oral anticoagulants | 20 (2) |
| ACE inhibitors or ARB | 1191 (91) |
| Beta blockers | 1128 (86) |
| Statin | 1189 (91) |
| High-dose statin | 892 (75) |
| Ezetimibe | 203 (16) |
| Lesions, n = 2422 | |
|---|---|
| Territory, no. (%) | |
| Left main | 89 (4) |
| LAD | 1112 (45) |
| LCx | 626 (25) |
| RCA | 595 (24) |
| Lesion features | |
| Type, no. (%) | |
| De novo | 2250 (92) |
| Instent restenosis | 167 (7) |
| Other | 5 (<1) |
| Serial lesions, no. (%) | 353 (14) |
| Location, no. (%) | |
| Proximal | 1294 (53) |
| Mid | 629 (26) |
| Distal | 499 (20) |
| AHA/ACC classification, no. (%) | |
| A or B1 | 850 (35) |
| B2 | 1076 (44) |
| C | 486 (20) |
| Severe calcification, no. (%) | 305 (12) |
| Bifurcation, no. (%) | 510 (21) |
| Severe tortuosity, no. (%) | 96 (3) |
| Quantitative coronary analysis | |
| RVD, mm | 2.6 ± 1.2 |
| Diameter stenosis, % | 66 ± 18 |
| Lesion length, mm | 15 ± 12 |
| MLD, mm | 1.27 ± 1.1 |
| Global anatomical Syntax Score | 15.5 ± 9.2 |
| Global functional Syntax Score | 9.5 ± 10 |
| Global Syntax Score II | 33.9 ± 12.5 |
| Global functional Syntax Score II | 32.2 ± 12.3 |
| SS-II 2020, predicted MACE, PCI, % | 26.1 ± 19 |
| SS-II 2020, predicted mortality, PCI, % | 37.4 ± 27.3 |
| Functional SS-II 2020, predicted MACE, PCI, % | 23.8 ± 17.9 |
| Functional SS-II 2020, predicted mortality, PCI, % | 35.3 ± 26.6 |
| Univariate | Multivariable | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p-Value | OR | 95% CI | p-Value | |
| Age | 1.08 | 1.06–1.11 | <0.0001 | 1.04 | 0.99–1.08 | 0.054 |
| LM-LAD versus others | 0.89 | 0.57–1.37 | 0.59 | |||
| MVD | 1.49 | 0.92–2.42 | 0.10 | 1.42 | 0.85–2.37 | 0.18 |
| Gender | 0.79 | 0.48–1.30 | 0.35 | |||
| BMI | 0.99 | 0.98–1.01 | 0.21 | |||
| Hypertension | 2.46 | 1.30–4.67 | 0.006 | 1.59 | 0.81–3.15 | 0.18 |
| Dyslipidemia | 1.23 | 0.77–1.94 | 0.39 | |||
| Smoking status: | ||||||
| Current | 1.29 | 0.81–2.04 | 0.29 | |||
| Former | 0.90 | 0.49–1.63 | 0.72 | |||
| Diabetes | 1.74 | 1.12–2.69 | 0.014 | |||
| Previous MI | 1.29 | 0.81–2.04 | 0.28 | |||
| IHD | 1.01 | 0.65–1.56 | 0.97 | |||
| COPD | 2.23 | 1.10–4.50 | 0.026 | |||
| PAD | 1.58 | 2.35–5.47 | 0.039 | 0.38 | 0.18–0.79 | 0.01 |
| CKD | 3.59 | 2.35–5.47 | <0.0001 | 1.37 | 1.02–2.94 | 0.04 |
| Previous stroke/TIA | 1.45 | 0.61–3.47 | 0.40 | |||
| LVEF | 0.95 | 0.93–0.97 | <0.0001 | 0.97 | 0.95–0.99 | 0.003 |
| Proximal disease | 1.20 | 0.78–1.84 | 0.41 | |||
| % DS | 1.01 | 0.99–1.03 | 0.43 | |||
| De novo vs. other | 0.53 | 0.29–0.99 | 0.047 | 0.57 | 0.30–1.11 | 0.10 |
| Functional SS-2020 | 1.03 | 1.02–1.03 | <0.0001 | 1.02 | 1.01–1.04 | 0.027 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scala, A.; Erriquez, A.; Verardi, F.M.; Marrone, A.; Scollo, E.; Trichilo, M.; Durante, A.; Tedeschi, D.; Cortese, B.; Ielasi, A.; et al. Functional (Re)Development of SYNTAX Score II 2020: Predictive Performance and Risk Assessment. J. Clin. Med. 2023, 12, 5844. https://doi.org/10.3390/jcm12185844
Scala A, Erriquez A, Verardi FM, Marrone A, Scollo E, Trichilo M, Durante A, Tedeschi D, Cortese B, Ielasi A, et al. Functional (Re)Development of SYNTAX Score II 2020: Predictive Performance and Risk Assessment. Journal of Clinical Medicine. 2023; 12(18):5844. https://doi.org/10.3390/jcm12185844
Chicago/Turabian StyleScala, Antonella, Andrea Erriquez, Filippo Maria Verardi, Andrea Marrone, Ennio Scollo, Michele Trichilo, Alessandro Durante, Delio Tedeschi, Bernardo Cortese, Alfonso Ielasi, and et al. 2023. "Functional (Re)Development of SYNTAX Score II 2020: Predictive Performance and Risk Assessment" Journal of Clinical Medicine 12, no. 18: 5844. https://doi.org/10.3390/jcm12185844
APA StyleScala, A., Erriquez, A., Verardi, F. M., Marrone, A., Scollo, E., Trichilo, M., Durante, A., Tedeschi, D., Cortese, B., Ielasi, A., Valentini, G., Tebaldi, M., Campo, G., Pavasini, R., & Biscaglia, S. (2023). Functional (Re)Development of SYNTAX Score II 2020: Predictive Performance and Risk Assessment. Journal of Clinical Medicine, 12(18), 5844. https://doi.org/10.3390/jcm12185844








