The Impact of Non-Pharmacological Interventions on Delirium in Neurological Intensive Care Unit Patients: A Single-Center Interrupted Time Series Trial
Abstract
:1. Introduction
2. Methods
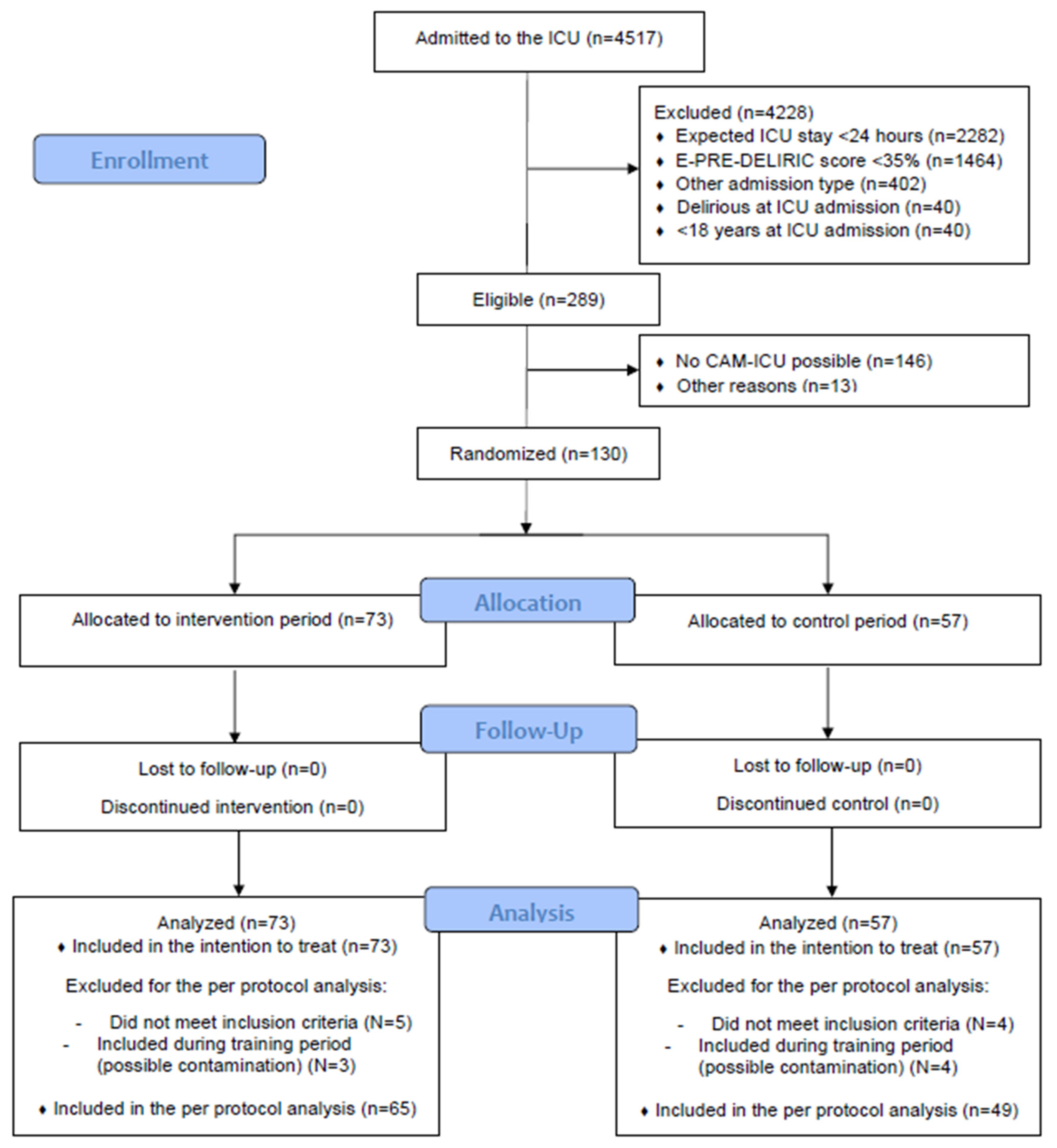
2.1. Design
2.2. Participants
2.3. Interventions and Implementation
2.4. Outcomes
2.5. Data Collection
2.6. Statistical Analyses
3. Results
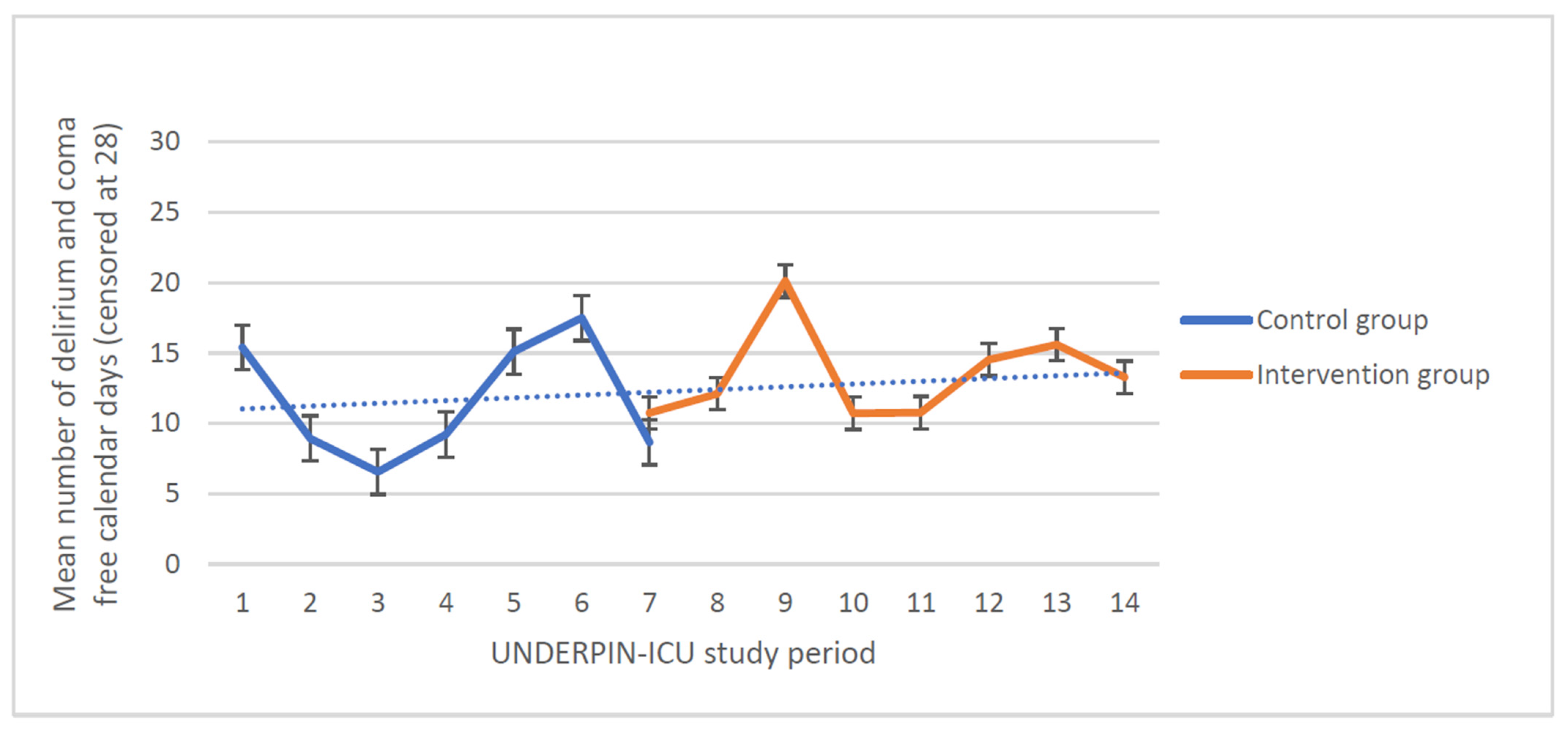
3.1. Primary Outcome
3.2. Secondary Outcomes
3.3. Process and Compliance Measures
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Slooter, A.J.C.; Otte, W.M.; Devlin, J.W.; Arora, R.C.; Bleck, T.P.; Claassen, J.; Duprey, M.S.; Ely, E.W.; Kaplan, P.W.; Latronico, N.; et al. Updated nomenclature of delirium and acute encephalopathy: Statement of ten Societies. Intensive Care Med. 2020, 46, 1020–1022. [Google Scholar] [CrossRef]
- Larsen, L.K.; Møller, K.; Petersen, M.; Egerod, I. Delirium prevalence and prevention in patients with acute brain injury: A prospective before-and-after intervention study. Intensive Crit. Care Nurs. 2020, 59, 102816. [Google Scholar] [CrossRef] [PubMed]
- Maldonado, J.R. Delirium pathophysiology: An updated hypothesis of the etiology of acute brain failure. Int. J. Geriatr. Psychiatry 2018, 33, 1428–1457. [Google Scholar] [CrossRef] [PubMed]
- Hughes, C.G.; Patel, M.B.; Pandharipande, P.P. Pathophysiology of acute brain dysfunction: What’s the cause of all this confusion? Curr. Opin. Crit. Care 2012, 18, 518–526. [Google Scholar] [CrossRef] [PubMed]
- Klimiec, E.; Dziedzic, T.; Kowalska, K.; Slowik, A.; Klimkowicz-Mrowiec, A. Knowns and Unknowns About Delirium in Stroke: A Review. Cogn. Behav. Neurol. 2016, 29, 174–189. [Google Scholar] [CrossRef] [PubMed]
- von Hofen-Hohloch, J.; Awissus, C.; Fischer, M.M.; Michalski, D.; Rumpf, J.J.; Classen, J. Delirium Screening in Neurocritical Care and Stroke Unit Patients: A Pilot Study on the Influence of Neurological Deficits on CAM-ICU and ICDSC Outcome. Neurocritical Care 2020, 33, 708–717. [Google Scholar] [CrossRef] [PubMed]
- Devlin, J.W.; Skrobik, Y.; Gelinas, C.; Needham, D.M.; Slooter, A.J.C.; Pandharipande, P.P.; Watson, P.L.; Weinhouse, G.L.; Nunnally, M.E.; Rochwerg, B.; et al. Clinical Practice Guidelines for the Prevention and Management of Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption in Adult Patients in the ICU. Crit. Care Med. 2018, 46, e825–e873. [Google Scholar] [CrossRef] [PubMed]
- Burry, L.; Mehta, S.; Perreault, M.M.; Luxenberg, J.S.; Siddiqi, N.; Hutton, B.; Fergusson, D.A.; Bell, C.; Rose, L. Antipsychotics for treatment of delirium in hospitalised non-ICU patients. Cochrane Database Syst. Rev. 2018, 6, Cd005594. [Google Scholar] [CrossRef] [PubMed]
- Lange, S.; Mędrzycka-Dąbrowska, W.; Friganovic, A.; Oomen, B.; Krupa, S. Non-Pharmacological Nursing Interventions to Prevent Delirium in ICU Patients-An Umbrella Review with Implications for Evidence-Based Practice. J. Pers. Med. 2022, 12, 760. [Google Scholar] [CrossRef] [PubMed]
- Kasapoğlu, E.S.; Enç, N. Role of multicomponent non-pharmacological nursing interventions on delirium prevention: A randomized controlled study. Geriatr. Nurs. 2022, 44, 207–214. [Google Scholar] [CrossRef] [PubMed]
- Matsuura, Y.; Ohno, Y.; Toyoshima, M.; Ueno, T. Effects of non-pharmacologic prevention on delirium in critically ill patients: A network meta-analysis. Nurs. Crit. Care 2022, 28, 727–737. [Google Scholar] [CrossRef] [PubMed]
- Rood, P.J.T.; Zegers, M.; Ramnarain, D.; Koopmans, M.; Klarenbeek, T.; Ewalds, E.; van der Steen, M.S.; Oldenbeuving, A.W.; Kuiper, M.A.; Teerenstra, S.; et al. The Impact of Nursing Delirium Preventive Interventions in the ICU: A Multicenter Cluster-randomized Controlled Clinical Trial. Am. J. Respir. Crit. Care Med. 2021, 204, 682–691. [Google Scholar] [CrossRef]
- Wassenaar, A.; Rood, P.; Schoonhoven, L.; Teerenstra, S.; Zegers, M.; Pickkers, P.; van den Boogaard, M. The impact of nUrsiNg DEliRium Preventive INnterventions in the Intensive Care Unit (UNDERPIN-ICU): A study protocol for a multi-centre, stepped wedge randomized controlled trial. Int. J. Nurs. Stud. 2017, 68, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Wassenaar, A.; van den Boogaard, M.; van Achterberg, T.; Slooter, A.J.C.; Kuiper, M.A.; Hoogendoorn, M.E.; Simons, K.S.; Maseda, E.; Pinto, N.; Jones, C.; et al. Multinational development and validation of an early prediction model for delirium in ICU patients. Intensive Care Med. 2015, 41, 1048–1056. [Google Scholar] [CrossRef] [PubMed]
- Hshieh, T.T.; Yue, J.; Oh, E.; Puelle, M.; Dowal, S.; Travison, T.; Inouye, S.K. Effectiveness of multicomponent nonpharmacological delirium interventions: A meta-analysis. JAMA Intern. Med. 2015, 175, 512–520. [Google Scholar] [CrossRef]
- Schweickert, W.D.; Pohlman, M.C.; Pohlman, A.S.; Nigos, C.; Pawlik, A.J.; Esbrook, C.L.; Spears, L.; Miller, M.; Franczyk, M.; Deprizio, D.; et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: A randomised controlled trial. Lancet 2009, 373, 1874–1882. [Google Scholar] [CrossRef] [PubMed]
- Inouye, S.K.; Bogardus, S.T., Jr.; Charpentier, P.A.; Leo-Summers, L.; Acampora, D.; Holford, T.R.; Cooney, L.M., Jr. A multicomponent intervention to prevent delirium in hospitalized older patients. N. Engl. J. Med. 1999, 340, 669–676. [Google Scholar] [CrossRef] [PubMed]
- Chaudoir, S.R.; Dugan, A.G.; Barr, C.H. Measuring factors affecting implementation of health innovations: A systematic review of structural, organizational, provider, patient, and innovation level measures. Implement Sci. 2013, 8, 22. [Google Scholar] [CrossRef] [PubMed]
- Ely, E.W.; Margolin, R.; Francis, J.; May, L.; Truman, B.; Dittus, R.; Speroff, T.; Gautam, S.; Bernard, G.R.; Inouye, S.K. Evaluation of delirium in critically ill patients: Validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). Crit. Care Med. 2001, 29, 1370–1379. [Google Scholar] [CrossRef] [PubMed]
- Sessler, C.; Gosnell, M.; Grap, M.; Brophy, G.; O'Neal, P.; Keane, K.; Tesoro, E.; Elswick, R. The Richmond Agitation-Sedation Scale: Validity and reliability in adult intensive care unit patients. Am. J. Respir. Crit. Care Med. 2002, 166, 1338–1344. [Google Scholar] [CrossRef] [PubMed]
- Rood, P.; Frenzel, T.; Verhage, R.; Bonn, M.; van der Hoeven, H.; Pickkers, P.; van den Boogaard, M. Development and daily use of a numeric rating score to assess sleep quality in ICU patients. J. Crit. Care 2019, 52, 68–74. [Google Scholar] [CrossRef] [PubMed]
- Miranda, D.R.; Nap, R.; de Rijk, A.; Schaufeli, W.; Iapichino, G. Nursing activities score. Crit. Care Med. 2003, 31, 374–382. [Google Scholar] [CrossRef] [PubMed]
- Zimmerman, J.E.; Kramer, A.A.; McNair, D.S.; Malila, F.M. Acute Physiology and Chronic Health Evaluation (APACHE) IV: Hospital mortality assessment for today's critically ill patients. Crit. Care Med. 2006, 34, 1297–1310. [Google Scholar] [CrossRef] [PubMed]
- Bannon, L.; McGaughey, J.; Verghis, R.; Clarke, M.; McAuley, D.F.; Blackwood, B. The effectiveness of non-pharmacological interventions in reducing the incidence and duration of delirium in critically ill patients: A systematic review and meta-analysis. Intensive Care Med. 2019, 45, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Martinez, F.; Donoso, A.M.; Marquez, C.; Labarca, E. Implementing a Multicomponent Intervention to Prevent Delirium Among Critically Ill Patients. Crit. Care Nurse 2017, 37, 36–46. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.J.; Traynor, V.; Wang, A.Y.; Shih, C.Y.; Tu, M.C.; Chuang, C.H.; Chiu, H.Y.; Chang, H.R. Comparative effectiveness of non-pharmacological interventions for preventing delirium in critically ill adults: A systematic review and network meta-analysis. Int. J. Nurs. Stud. 2022, 131, 104239. [Google Scholar] [CrossRef] [PubMed]
- Persico, I.; Cesari, M.; Morandi, A.; Haas, J.; Mazzola, P.; Zambon, A.; Annoni, G.; Bellelli, G. Frailty and Delirium in Older Adults: A Systematic Review and Meta-Analysis of the Literature. J. Am. Geriatr. Soc. 2018, 66, 2022–2030. [Google Scholar] [CrossRef] [PubMed]
- Zaal, I.J.; Devlin, J.W.; Peelen, L.M.; Slooter, A.J. A systematic review of risk factors for delirium in the ICU. Crit. Care Med. 2015, 43, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Kotfis, K.; van Diem-Zaal, I.; Williams Roberson, S.; Sietnicki, M.; van den Boogaard, M.; Shehabi, Y.; Ely, E.W. The future of intensive care: Delirium should no longer be an issue. Crit. Care 2022, 26, 200. [Google Scholar] [CrossRef]
- Berglund, B.; Lindvall, T.; Epidemiology, I.o.E.; Schwela, D.H.; Salut, O.M.d.l.; World Health Organization. Guidelines for Community Noise; World Health Organization: Geneva, Switzerland, 1999. [Google Scholar]
- Nostedt, S.; Joffe, A.R. Critical Care Randomized Trials Demonstrate Power Failure: A Low Positive Predictive Value of Findings in the Critical Care Research Field. J. Intensive Care Med. 2022, 37, 1082–1093. [Google Scholar] [CrossRef] [PubMed]
| Domain | Activities |
|---|---|
| 1. Visual and hearing impairment | Use of visual and hearing aids whenever awake Approach from the best side for vision and hearing Provision of material adapted to patients who have a visual impairment Prevention of cornea dehydration during sedation Attention to verbal communication when severely visually impaired Limiting background noise Use of special communication techniques as appropriate |
| 2. Sleep deprivation | Optimizing circadian rhythm Noise reduction Minimizing night-time procedures Providing optimal relaxation Restriction of sleep medication Improving staff awareness of sleep importance Striving to minimize sedation use |
| 3 Cognitive impairment | Providing a schedule, clock, and calendar for each patient Promotion of provision of personal objects by next of kin Promoting regular visits Optimizing and tailoring communication based on patients’ preferences Frequent reorientation Provision of cognitive training exercises |
| 4. Immobility | Encouraging setting and documenting of clear mobilization goals Minimizing sedation use Minimizing and optimally locating restraining lines Optimizing analgesia and establishing proper guidance for minimizing pain and fear during mobilization Frequent provision of physical therapy and/or mobilizationInvolving next of kin in stimulating early mobilization |
| A detailed description of activities can be found in Supplemental file S1 | |
| Intervention N = 73 | Control N = 53 | p-Value | |
|---|---|---|---|
| Male/female | 36/37 (49/51) | 36/21 (63/37) | 0.12 |
| Age in years, mean (SD) | 69 (11) | 67 (11) | 0.49 |
| Urgent admission | 70 (96) | 55 (97) | 0.11 |
| APACHE IV score per point, mean (SD) | 80 (25) | 78 (24) | 0.61 |
| History of cognitive disorders | 11 (15) | 11 (19) | 0.60 |
| History of alcohol abuse | 15 (21) | 11 (19) | 0.77 |
| Mean arterial pressure at admission (mmHg), mean (SD) | 91 (20) | 92 (20) | 0.68 |
| Corticosteroids at admission | 4 (6) | 6 (11) | 0.32 |
| Respiratory insufficiency | 65 (89) | 53 (93) | 0.98 |
| Serum urea level at admission (mmol/L), median [IQR] | 7 [5 to 9] | 5 [5 to 7] | 0.10 |
| E-PRE-DELIRIC score, mean (SD) | 41 (11) | 46 (10) | 0.01 |
| RASS score at admission, median [IQR] | −4 [−4 to −3] | −4 [−5 to −2] | 0.36 |
| Pre-admission use of visual or hearing aids | 18 (25) | 13 (23) | 0.34 |
| Intervention N = 73 | Control N = 57 | Level Change (95%CI) | p-Value | Slope Change (95%CI) | p-Value | |
|---|---|---|---|---|---|---|
| Delirium- and coma-free days alive | 15 [0–26] | 10 [0–24] | −0.48 (−7.07 to 6.10) | 0.87 | −0.95 (−2.41 to 0.52) | 0.18 |
| Delirium days | 0 [0–2] | 2 [0–4] | 1.02 (0.51 to 2.03) A | 0.96 | 1.11 (0.94 to 1.33) A | 0.19 |
| in delirious patients | 2 [1–7] | 2 [2–4] | 1.59 (0.72 to 3.49) A | 0.22 | 1.21 (1.00 to 1.48) | 0.05 |
| Coma days | 3 [1–5] | 2 [0–4] | 1.29 (0.69 to 2.43) A | 0.39 | 1.10 (0.94 to 1.29) A | 0.21 |
| Sedation days | 2 [1–4] | 2 [1–4] | 0.95 (0.47 to 1.91) A | 0.87 | 1.11 (0.93 to 1.33) A | 0.20 |
| Delirium medication days | 0 [0–1] | 0 [0–3] | 3.66 (0.75 to 17.78) A | 0.09 | 1.36 (0.81 to 2.31) A | 0.19 |
| Delirium incidence | 24 (33) | 42 (74) | 11.38 (<0.001 to 26647) B | 0.50 | 4.67 (0.66 to 32.75) B | 0.11 |
| Duration of mechanical ventilation | 5 [2–11] | 4 [2–13] | 1.46 (0.87 to 2.45) A | 0.13 | 1.06 (0.94 to 1.20) A | 0.28 |
| Incidence of re-intubation | 15 (21) | 9 (16) | 0.36 (<0.001 to 4727) B | 0.81 | 3.52 (0.48 to 26.03) B | 0.18 |
| Incidence of re-admission | 4 (6) | 8 (14) | 0.00 (0.00 to 0.00) B | <0.001 | 0.55 (0.23 to 1.30) B | 0.14 |
| Incidence of unplanned removal of tubes/catheters | 8 (14) | 5 (9) | 114.00 (<0.001 to >1000) B | 0.53 | 7.04 (0.11 to 431.40) B | 0.32 |
| Incidence of physical restraints | 33 (45) | 37 (65) | 1.53 (0.21 to 11.39) B | 0.65 | 1.07 (0.65 to 1.77) B | 0.77 |
| Duration of physical restraints | 0 [0–4] | 3 [0–8] | 1.18 (0.44 to 3.21) A | 0.71 | 1.08 (0.84 to 1.39) A | 0.50 |
| ICU length of stay | 8 [4–13] | 8 [5–18] | 1.75 (0.78 to 3.93) A | 0.16 | 1.77 (0.96 to 1.44) A | 0.10 |
| Hospital length of stay | 13 [6–22] | 18 [6–34] | 1.15 (0.45 to 2.96) A | 0.75 | 1.08 (0.85 to 1.36) A | 0.51 |
| Mortality, 28 days | 33 (45) | 25 (44) | 0.01 (<0.001 to 35.79) B | 0.24 | 0.16 (0.02 to 1.24) B | 0.07 |
| Mortality, 90 days | 39 (53) | 31 (54) | 0.006 (<0.001 to 18.28) B | 0.19 | 0.12 (0.02 to 0.89) B | 0.04 |
| Intervention | Control | p-Value | ||
|---|---|---|---|---|
| RASS score 1 | Night | −1 [−3–0] | −1 [−3–0] | 0.37 |
| Day | −1 [−3–0] | −1 [−3–0] | 0.86 | |
| Evening | −1 [−3–0] | −1 [−3–0] | 0.27 | |
| NRS Sleep 1 | 6 (2) | 6 (2) | 0.13 | |
| Light levels (LUX) 2 | Day | 86 [23–133] | 40 [21–109] | 0.64 |
| Night | 9 [9–10] | 15 [14–17] | <0.01 | |
| Noise levels (dB) 2 | Day | 40 [39–41] | 43 [43–44] | <0.01 |
| Night | 39 [38–39] | 42 [42–43] | <0.01 | |
| Nursing Activity Score—workload 1 | 50 [44–64] | 53 [44–62] | 0.45 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rood, P.J.T.; Ramnarain, D.; Oldenbeuving, A.W.; den Oudsten, B.L.; Pouwels, S.; van Loon, L.M.; Teerenstra, S.; Pickkers, P.; de Vries, J.; van den Boogaard, M. The Impact of Non-Pharmacological Interventions on Delirium in Neurological Intensive Care Unit Patients: A Single-Center Interrupted Time Series Trial. J. Clin. Med. 2023, 12, 5820. https://doi.org/10.3390/jcm12185820
Rood PJT, Ramnarain D, Oldenbeuving AW, den Oudsten BL, Pouwels S, van Loon LM, Teerenstra S, Pickkers P, de Vries J, van den Boogaard M. The Impact of Non-Pharmacological Interventions on Delirium in Neurological Intensive Care Unit Patients: A Single-Center Interrupted Time Series Trial. Journal of Clinical Medicine. 2023; 12(18):5820. https://doi.org/10.3390/jcm12185820
Chicago/Turabian StyleRood, Paul J. T., Dharmanand Ramnarain, Annemarie W. Oldenbeuving, Brenda L. den Oudsten, Sjaak Pouwels, Lex M. van Loon, Steven Teerenstra, Peter Pickkers, Jolanda de Vries, and Mark van den Boogaard. 2023. "The Impact of Non-Pharmacological Interventions on Delirium in Neurological Intensive Care Unit Patients: A Single-Center Interrupted Time Series Trial" Journal of Clinical Medicine 12, no. 18: 5820. https://doi.org/10.3390/jcm12185820
APA StyleRood, P. J. T., Ramnarain, D., Oldenbeuving, A. W., den Oudsten, B. L., Pouwels, S., van Loon, L. M., Teerenstra, S., Pickkers, P., de Vries, J., & van den Boogaard, M. (2023). The Impact of Non-Pharmacological Interventions on Delirium in Neurological Intensive Care Unit Patients: A Single-Center Interrupted Time Series Trial. Journal of Clinical Medicine, 12(18), 5820. https://doi.org/10.3390/jcm12185820








