Triage of Critically Ill Patients: Characteristics and Outcomes of Patients Refused as Too Well for Intensive Care
Abstract
:1. Introduction
2. Materials and Methods
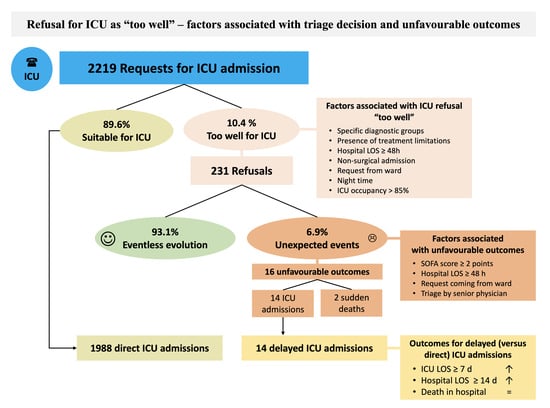
3. Results
3.1. Comparison of Included Patients According to ICU Triage Decision
3.1.1. Baseline Characteristics
3.1.2. Outcomes
3.2. Characteristics of Patients Deemed “Too Well” According to Event Occurrence
3.3. Outcomes According to Delay in ICU Admission
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Edbrooke, D.L.; Minelli, C.; Mills, G.H.; Iapichino, G.; Pezzi, A.; Corbella, D.; Jacobs, P.; Lippert, A.; Wiis, J.; Pesenti, A.; et al. Implications of ICU Triage Decisions on Patient Mortality: A Cost-Effectiveness Analysis. Crit. Care Lond. Engl. 2011, 15, R56. [Google Scholar] [CrossRef] [PubMed]
- Anesi, G.L.; Admon, A.J.; Halpern, S.D.; Kerlin, M.P. Understanding Irresponsible Use of Intensive Care Unit Resources in the USA. Lancet Respir. Med. 2019, 7, 605–612. [Google Scholar] [CrossRef] [PubMed]
- Society of Critical Care Medicine Ethics Committee. Consensus Statement on the Triage of Critically Ill Patients. JAMA 1994, 271, 1200–1203. [Google Scholar] [CrossRef]
- Teres, D. Civilian Triage in the Intensive Care Unit: The Ritual of the Last Bed. Crit. Care Med. 1993, 21, 598–606. [Google Scholar] [CrossRef]
- White, D.B.; Lo, B. Mitigating Inequities and Saving Lives with ICU Triage during the COVID-19 Pandemic. Am. J. Respir. Crit. Care Med. 2021, 203, 287–295. [Google Scholar] [CrossRef]
- Vinay, R.; Baumann, H.; Biller-Andorno, N. Ethics of ICU Triage during COVID-19. Br. Med. Bull. 2021, 138, 5–15. [Google Scholar] [CrossRef] [PubMed]
- Swiss Academy Of Medical Sciences. COVID-19 Pandemic: Triage for Intensive-Care Treatment under Resource Scarcity (3rd, Updated Version). Swiss Med. Wkly. 2020, 150, w20401. [Google Scholar] [CrossRef]
- Sprung, C.L.; Danis, M.; Iapichino, G.; Artigas, A.; Kesecioglu, J.; Moreno, R.; Lippert, A.; Curtis, J.R.; Meale, P.; Cohen, S.L.; et al. Triage of Intensive Care Patients: Identifying Agreement and Controversy. Intensive Care Med. 2013, 39, 1916–1924. [Google Scholar] [CrossRef]
- Blanch, L.; Abillama, F.F.; Amin, P.; Christian, M.; Joynt, G.M.; Myburgh, J.; Nates, J.L.; Pelosi, P.; Sprung, C.; Topeli, A.; et al. Triage Decisions for ICU Admission: Report from the Task Force of the World Federation of Societies of Intensive and Critical Care Medicine. J. Crit. Care 2016, 36, 301–305. [Google Scholar] [CrossRef]
- Nates, J.L.; Nunnally, M.; Kleinpell, R.; Blosser, S.; Goldner, J.; Birriel, B.; Fowler, C.S.; Byrum, D.; Miles, W.S.; Bailey, H.; et al. ICU Admission, Discharge, and Triage Guidelines: A Framework to Enhance Clinical Operations, Development of Institutional Policies, and Further Research. Crit. Care Med. 2016, 44, 1553–1602. [Google Scholar] [CrossRef]
- Guidelines for Intensive Care Unit Admission, Discharge, and Triage. Task Force of the American College of Critical Care Medicine, Society of Critical Care Medicine. Crit. Care Med. 1999, 27, 633–638. [Google Scholar]
- Levin, P.D.; Sprung, C.L. The Process of Intensive Care Triage. Intensive Care Med. 2001, 27, 1441–1445. [Google Scholar] [CrossRef] [PubMed]
- Sprung, C.L.; Baras, M.; Iapichino, G.; Kesecioglu, J.; Lippert, A.; Hargreaves, C.; Pezzi, A.; Pirracchio, R.; Edbrooke, D.L.; Pesenti, A.; et al. The Eldicus Prospective, Observational Study of Triage Decision Making in European Intensive Care Units: Part I--European Intensive Care Admission Triage Scores. Crit. Care Med. 2012, 40, 125–131. [Google Scholar] [CrossRef] [PubMed]
- Bassford, C.R.; Krucien, N.; Ryan, M.; Griffiths, F.E.; Svantesson, M.; Fritz, Z.; Perkins, G.D.; Quinton, S.; Slowther, A.-M.U.K. Intensivists’ Preferences for Patient Admission to ICU: Evidence From a Choice Experiment. Crit. Care Med. 2019, 47, 1522–1530. [Google Scholar] [CrossRef] [PubMed]
- Cohen, R.I.; Eichorn, A.; Silver, A. Admission Decisions to a Medical Intensive Care Unit Are Based on Functional Status Rather than Severity of Illness. A Single Center Experience. Minerva Anestesiol. 2012, 78, 1226–1233. [Google Scholar] [PubMed]
- Cohen, R.I.; Eichorn, A.; Motschwiller, C.; Laktikova, V.; La Torre, G.; Ginsberg, N.; Steinberg, H. Medical Intensive Care Unit Consults Occurring within 48 Hours of Admission: A Prospective Study. J. Crit. Care 2015, 30, 363–368. [Google Scholar] [CrossRef]
- Escher, M.; Cullati, S.; Hudelson, P.; Nendaz, M.; Ricou, B.; Perneger, T.; Dayer, P. Admission to Intensive Care: A Qualitative Study of Triage and Its Determinants. Health Serv. Res. 2019, 54, 474–483. [Google Scholar] [CrossRef]
- Garrouste-Orgeas, M.; Montuclard, L.; Timsit, J.-F.; Misset, B.; Christias, M.; Carlet, J. Triaging Patients to the ICU: A Pilot Study of Factors Influencing Admission Decisions and Patient Outcomes. Intensive Care Med. 2003, 29, 774–781. [Google Scholar] [CrossRef]
- Garrouste-Orgeas, M.; Montuclard, L.; Timsit, J.-F.; Reignier, J.; Desmettre, T.; Karoubi, P.; Moreau, D.; Montesino, L.; Duguet, A.; Boussat, S.; et al. Predictors of Intensive Care Unit Refusal in French Intensive Care Units: A Multiple-Center Study. Crit. Care Med. 2005, 33, 750–755. [Google Scholar] [CrossRef]
- Iapichino, G.; Corbella, D.; Minelli, C.; Mills, G.H.; Artigas, A.; Edbooke, D.L.; Pezzi, A.; Kesecioglu, J.; Patroniti, N.; Baras, M.; et al. Reasons for Refusal of Admission to Intensive Care and Impact on Mortality. Intensive Care Med. 2010, 36, 1772–1779. [Google Scholar] [CrossRef]
- Sprung, C.L.; Geber, D.; Eidelman, L.A.; Baras, M.; Pizov, R.; Nimrod, A.; Oppenheim, A.; Epstein, L.; Cotev, S. Evaluation of Triage Decisions for Intensive Care Admission. Crit. Care Med. 1999, 27, 1073–1079. [Google Scholar] [CrossRef] [PubMed]
- Sinuff, T.; Kahnamoui, K.; Cook, D.J.; Luce, J.M.; Levy, M.M. Values Ethics and Rationing in Critical Care Task Force Rationing Critical Care Beds: A Systematic Review. Crit. Care Med. 2004, 32, 1588–1597. [Google Scholar] [CrossRef] [PubMed]
- Escher, M.; Nendaz, M.; Scherer, F.; Cullati, S.; Perneger, T. Physicians’ Predictions of Long-Term Survival and Functional Outcomes Do Not Influence the Decision to Admit Patients with Advanced Disease to Intensive Care: A Prospective Study. Palliat. Med. 2021, 35, 161–168. [Google Scholar] [CrossRef] [PubMed]
- Gopalan, P.D.; Pershad, S. Decision-Making in ICU—A Systematic Review of Factors Considered Important by ICU Clinician Decision Makers with Regard to ICU Triage Decisions. J. Crit. Care 2019, 50, 99–110. [Google Scholar] [CrossRef]
- Valley, T.S.; Schutz, A.; Miller, J.; Miles, L.; Lipman, K.; Eaton, T.L.; Kinni, H.; Cooke, C.R.; Iwashyna, T.J. Hospital Factors That Influence ICU Admission Decision-Making: A Qualitative Study of Eight Hospitals. Intensive Care Med. 2023, 49, 505–516. [Google Scholar] [CrossRef] [PubMed]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. STROBE Initiative The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. Ann. Intern. Med. 2007, 147, 573–577. [Google Scholar] [CrossRef]
- Howe, D.C. Observational Study of Admission and Triage Decisions for Patients Referred to a Regional Intensive Care Unit. Anaesth. Intensive Care 2011, 39, 650–658. [Google Scholar] [CrossRef]
- Robert, R.; Coudroy, R.; Ragot, S.; Lesieur, O.; Runge, I.; Souday, V.; Desachy, A.; Gouello, J.-P.; Hira, M.; Hamrouni, M.; et al. Influence of ICU-Bed Availability on ICU Admission Decisions. Ann. Intensive Care 2015, 5, 55. [Google Scholar] [CrossRef]
- Andersen, F.H.; Flaatten, H.; Klepstad, P.; Follestad, T.; Strand, K.; Krüger, A.J.; Hahn, M.; Buskop, C.; Rime, A.-K.; Kvåle, R. Long-Term Outcomes After ICU Admission Triage in Octogenarians. Crit. Care Med. 2017, 45, e363–e371. [Google Scholar] [CrossRef]
- Pintado, M.-C.; Villa, P.; González-García, N.; Luján, J.; Molina, R.; Trascasa, M.; López-Ramos, E.; Martínez, C.; Cambronero, J.-A.; de Pablo, R. Characteristics and Outcomes of Elderly Patients Refused to ICU. Sci. World J. 2013, 2013, 590837. [Google Scholar] [CrossRef]
- Sprung, C.L.; Artigas, A.; Kesecioglu, J.; Pezzi, A.; Wiis, J.; Pirracchio, R.; Baras, M.; Edbrooke, D.L.; Pesenti, A.; Bakker, J.; et al. The Eldicus Prospective, Observational Study of Triage Decision Making in European Intensive Care Units. Part II: Intensive Care Benefit for the Elderly. Crit. Care Med. 2012, 40, 132–138. [Google Scholar] [CrossRef] [PubMed]
- van der Zee, E.N.; Benoit, D.D.; Hazenbroek, M.; Bakker, J.; Kompanje, E.J.O.; Kusadasi, N.; Epker, J.L. Outcome of Cancer Patients Considered for Intensive Care Unit Admission in Two University Hospitals in the Netherlands: The Danger of Delayed ICU Admissions and off-Hour Triage Decisions. Ann. Intensive Care 2021, 11, 125. [Google Scholar] [CrossRef] [PubMed]
- Garrouste-Orgeas, M.; Timsit, J.-F.; Montuclard, L.; Colvez, A.; Gattolliat, O.; Philippart, F.; Rigal, G.; Misset, B.; Carlet, J. Decision-Making Process, Outcome, and 1-Year Quality of Life of Octogenarians Referred for Intensive Care Unit Admission. Intensive Care Med. 2006, 32, 1045–1051. [Google Scholar] [CrossRef] [PubMed]
- Mery, E.; Kahn, J.M. Does Space Make Waste? The Influence of ICU Bed Capacity on Admission Decisions. Crit. Care Lond. Engl. 2013, 17, 315. [Google Scholar] [CrossRef]
- Cohen, R.I.; Lisker, G.N.; Eichorn, A.; Multz, A.S.; Silver, A. The Impact of Do-Not-Resuscitate Order on Triage Decisions to a Medical Intensive Care Unit. J. Crit. Care 2009, 24, 311–315. [Google Scholar] [CrossRef]
- Todorov, A.; Kaufmann, F.; Arslani, K.; Haider, A.; Bengs, S.; Goliasch, G.; Zellweger, N.; Tontsch, J.; Sutter, R.; Buddeberg, B.; et al. Gender Differences in the Provision of Intensive Care: A Bayesian Approach. Intensive Care Med. 2021, 47, 577–587. [Google Scholar] [CrossRef]
- Hill, A.; Ramsey, C.; Dodek, P.; Kozek, J.; Fransoo, R.; Fowler, R.; Doupe, M.; Wong, H.; Scales, D.; Garland, A. Examining Mechanisms for Gender Differences in Admission to Intensive Care Units. Health Serv. Res. 2020, 55, 35–43. [Google Scholar] [CrossRef]
- Hinds, N.; Borah, A.; Yoo, E.J. Outcomes of Nighttime Refusal of Admission to the Intensive Care Unit: The Role of the Intensivist in Triage. J. Crit. Care 2017, 39, 214–219. [Google Scholar] [CrossRef]
- Vanhecke, T.E.; Gandhi, M.; McCullough, P.A.; Lazar, M.H.; Ravikrishnan, K.P.; Kadaj, P.; Begle, R.L. Outcomes of Patients Considered for, but Not Admitted to, the Intensive Care Unit. Crit. Care Med. 2008, 36, 812–817. [Google Scholar] [CrossRef]
- Naser, W.; Schwartz, N.; Finkelstein, R.; Bisharat, N. Outcome of Mechanically Ventilated Patients Initially Denied Admission to an Intensive Care Unit and Subsequently Admitted. Eur. J. Intern. Med. 2016, 35, 100–105. [Google Scholar] [CrossRef]
- Chalfin, D.B.; Trzeciak, S.; Likourezos, A.; Baumann, B.M.; Dellinger, R.P. DELAY-ED study group Impact of Delayed Transfer of Critically Ill Patients from the Emergency Department to the Intensive Care Unit. Crit. Care Med. 2007, 35, 1477–1483. [Google Scholar] [CrossRef] [PubMed]
- Mathews, K.S.; Durst, M.S.; Vargas-Torres, C.; Olson, A.D.; Mazumdar, M.; Richardson, L.D. Effect of Emergency Department and ICU Occupancy on Admission Decisions and Outcomes for Critically Ill Patients. Crit. Care Med. 2018, 46, 720–727. [Google Scholar] [CrossRef]
- Kiekkas, P.; Tzenalis, A.; Gklava, V.; Stefanopoulos, N.; Voyagis, G.; Aretha, D. Delayed Admission to the Intensive Care Unit and Mortality of Critically Ill Adults: Systematic Review and Meta-Analysis. BioMed Res. Int. 2022, 2022, 4083494. [Google Scholar] [CrossRef] [PubMed]
- Mardini, L.; Lipes, J.; Jayaraman, D. Adverse Outcomes Associated with Delayed Intensive Care Consultation in Medical and Surgical Inpatients. J. Crit. Care 2012, 27, 688–693. [Google Scholar] [CrossRef]
- Guan, G.; Lee, C.M.Y.; Begg, S.; Crombie, A.; Mnatzaganian, G. The Use of Early Warning System Scores in Prehospital and Emergency Department Settings to Predict Clinical Deterioration: A Systematic Review and Meta-Analysis. PLoS ONE 2022, 17, e0265559. [Google Scholar] [CrossRef] [PubMed]
- Ramos, J.G.R.; Ranzani, O.T.; Perondi, B.; Dias, R.D.; Jones, D.; Carvalho, C.R.R.; Velasco, I.T.; Forte, D.N. A Decision-Aid Tool for ICU Admission Triage Is Associated with a Reduction in Potentially Inappropriate Intensive Care Unit Admissions. J. Crit. Care 2019, 51, 77–83. [Google Scholar] [CrossRef] [PubMed]
- Zimmerman, J.E.; Kramer, A.A. A Model for Identifying Patients Who May Not Need Intensive Care Unit Admission. J. Crit. Care 2010, 25, 205–213. [Google Scholar] [CrossRef]
- Nicola, R.; Dogra, V. Ultrasound: The Triage Tool in the Emergency Department: Using Ultrasound First. Br. J. Radiol. 2016, 89, 20150790. [Google Scholar] [CrossRef]
- Guzmán-García, M.B.; Mohedano-Moriano, A.; González-González, J.; Morales-Cano, J.M.; Campo-Linares, R.; Lozano-Suárez, C.; Estrada-Álvarez, T.P.; Romero-Fernández, M.M.; Aguilar-Galán, E.V.; Criado-Álvarez, J.J. Lung Ultrasound as a Triage Method in Primary Care for Patients with Suspected SARS-CoV-2 Pneumonia. J. Clin. Med. 2022, 11, 6420. [Google Scholar] [CrossRef]
- Yin, W.; Li, Y.; Zeng, X.; Qin, Y.; Wang, D.; Zou, T.; Su, L.; Kang, Y. The Utilization of Critical Care Ultrasound to Assess Hemodynamics and Lung Pathology on ICU Admission and the Potential for Predicting Outcome. PLoS ONE 2017, 12, e0182881. [Google Scholar] [CrossRef]

| Admitted to ICU | Refused as Too Well | p Value | |
|---|---|---|---|
| (N = 1988) | (N = 231) | ||
| Patient characteristics | |||
| Age distribution—no. (%) | 0.82 | ||
| 14–64 y | 840 (42.3) | 102 (44.2) | |
| 65–79 y | 754 (37.9) | 83 (35.9) | |
| 80–98 y | 394 (19.8) | 46 (19.9) | |
| Sex–no. (%) | 0.36 | ||
| Male | 1224 (61.6) | 135 (58.4) | |
| Female | 764 (38.4) | 96 (41.6) | |
| Diagnosis for ICU request–no. (%) | <0.01 | ||
| Acute coronary syndrome | 313 (15.7) | 27 (11.7) | |
| Arrhythmia | 89 (4.5) | 14 (6.1) | |
| Cardiovascular, other | 230 (11.6) | 42 (18.2) | |
| Respiratory, any | 268 (13.5) | 48 (20.8) | |
| Stroke | 248 (12.4) | 4 (1.7) | |
| Neurologic, other | 189 (9.5) | 23 (10.0) | |
| Sepsis | 114 (5.7) | 22 (9.5) | |
| Gastrointestinal, any | 181 (9.1) | 13 (5.6) | |
| Metabolic imbalance | 77 (3.9) | 20 (8.7) | |
| Intoxication | 73 (3.7) | 5 (2.1) | |
| Trauma | 41 (2.1) | 3 (1.3) | |
| Other reason 1 | 165 (8.3) | 10 (4.3) | |
| Oncologic disease—no. (%) | 0.51 | ||
| None or limited disease | 1786 (89.8) | 209 (90.5) | |
| Metastatic cancer | 126 (6.3) | 18 (7.8) | |
| Leukaemia/Lymphoma | 53 (2.7) | 4 (1.7) | |
| Missing | 23 (1.2) | 0 (0.0) | |
| Limitations of life-sustaining treatments—no. (%) | 0.02 | ||
| No limitation | 1711 (86.1) | 181 (78.3) | |
| Any limitation 2 | 277 (13.9) | 45 (19.5) | |
| Order “no ICU” 3 | 0 (0.0) | 5 (2.2) | |
| Time since hospital admission—no. (%) | 0.04 | ||
| <2 d | 1636 (82.3) | 174 (75.3) | |
| 2 to <7 d | 174 (8.7) | 28 (12.1) | |
| 7 to 114 d | 178 (9.0) | 29 (12.6) | |
| Organisational factors | |||
| Admission status—no. (%) | <0.01 | ||
| Medical | 1469 (73.9) | 211 (91.3) | |
| Surgical, urgent | 243 (12.2) | 14 (6.1) | |
| Surgical, elective | 272 (13.7) | 6 (2.6) | |
| Missing | 4 (0.2) | 0 (0.0) | |
| Location at time of ICU demand—no. (%) | <0.01 | ||
| Emergency room | 1141 (57.4) | 148 (64.1) | |
| Ward | 273 (13.7) | 68 (29.4) | |
| Postoperative recovery room | 117 (5.9) | 9 (3.9) | |
| Operating theatre | 394 (19.8) | 6 (2.6) | |
| Other location 1 | 63 (3.2) | 0 (0.0) | |
| Time of demand for ICU admission—no. (%) | <0.01 | ||
| 00:00–05:59 | 263 (13.2) | 50 (21.6) | |
| 06:00–11:59 | 292 (14.7) | 34 (14.7) | |
| 12:00–17:59 | 820 (41.3) | 81 (35.1) | |
| 18:00–23:59 | 613 (30.8) | 66 (28.6) | |
| Availability of ICU beds at time of ICU demand—no. (%) | <0.01 | ||
| >4 beds | 1046 (52.6) | 97 (42.0) | |
| 3–4 beds | 573 (28.8) | 73 (31.6) | |
| 0–2 beds | 369 (18.6) | 61 (26.4) |
| Admitted to ICU | Refused as Too Well | p Value | |
|---|---|---|---|
| (N = 1988) | (N = 231) | ||
| Death in ICU—no. (%) 1 | 90 (4.5) | 7 (3.0) | 0.29 |
| Death in hospital, all—no. (%) | 150 (7.5) | 16 (6.9) | 0.74 |
| Death in hospital, according to treatment limitations at time of ICU demand—no./total of subgroup [%] | |||
| No limitation | 108/1711 [6.3] | 9/181 [5.0] | 0.48 |
| Any limitation 2 | 42/277 [15.2] | 6/45 [13.3] | 0.75 |
| Order “no ICU” | - | 1/5 [20.0] | n.a. |
| Death within 7 days—no. (%) | 85 (4.3) | 4 (1.7) | 0.06 |
| No therapeutic limitations, no. (%) 3 | - | 2 (0.9) | n.a. |
| Therapeutic limitations, no. (%) 4 | - | 2 (0.9) | n.a. |
| ICU admission within 7 days, no. (%) | - | 17 (7.4) | n.a. |
| No obviously new reason, no. (%) 3 | - | 14 (6.1) | n.a. |
| Other reason than at time of refusal 5 | - | 3 (1.3) | n.a. |
| Eventless Evolution | Unexpected Event 1 | p Value | |
|---|---|---|---|
| (N = 215) | (N = 16) | ||
| Patient characteristics | |||
| Age distribution—no. (%) | 0.16 | ||
| 14–64 y | 96 (44.7) | 6 (37.5) | |
| 65–79 y | 74 (34.4) | 9 (56.2) | |
| 80–98 y | 45 (20.9) | 1 (6.3) | |
| Sex—no. (%) | 0.73 | ||
| Male | 125 (58.1) | 10 (62.5) | |
| Female | 90 (41.9) | 6 (37.5) | |
| Diagnosis for ICU request—no. (%) | 0.15 | ||
| Acute coronary syndrome | 26 (12.1) | 1 (6.2) | |
| Arrhythmia | 12 (5.6) | 2 (12.5) | |
| Cardiovascular, other | 42 (19.5) | 0 (0.0) | |
| Respiratory, any | 42 (19.5) | 6 (37.5) | |
| Stroke | 4 (1.9) | 0 (0.0) | |
| Neurologic, other | 23 (10.7) | 0 (0.0) | |
| Sepsis | 21 (9.8) | 1 (6.3) | |
| Gastrointestinal, any | 11 (5.1) | 2 (12.5) | |
| Metabolic imbalance | 18 (8.4) | 2 (12.5) | |
| Intoxication | 5 (2.3) | 0 (0.0) | |
| Trauma | 3 (1.4) | 0 (0.0) | |
| Other reason 2 | 8 (3.7) | 2 (12.5) | |
| Oncologic disease—no. (%) | 0.53 | ||
| None or limited disease | 195 (90.7) | 14 (87.5) | |
| Metastatic cancer | 16 (7.4) | 2 (12.5) | |
| Leukaemia/Lymphoma | 4 (1.9) | 0 (0.0) | |
| Limitations of life-sustaining treatments—no. (%) | 1.00 | ||
| No limitation | 168 (78.1) | 13 (81.2) | |
| Any limitation 3 | 42 (19.6) | 3 (18.8) | |
| Order “no ICU” | 5 (2.3) | 0 (0.0) | |
| Time since hospital admission—no. (%) | 0.04 | ||
| <2 d | 165 (76.7) | 9 (56.2) | |
| 2 to <7 d | 23 (10.7) | 5 (31.3) | |
| 7 to 114 d | 27 (12.6) | 2 (12.5) | |
| SOFA Score, points | <0.01 | ||
| 0–1 | 121 (56.3) | 2 (12.5) | |
| 2–3 | 63 (29.3) | 8 (50.0) | |
| 4–5 | 26 (12.1) | 4 (25.0) | |
| 6–24 | 5 (2.3) | 2 (12.5) | |
| Organisational factors | |||
| Admission status—no. (%) | 0.75 | ||
| Medical | 195 (90.7) | 16 (100.0) | |
| Surgical, urgent | 14 (6.5) | 0 (0.0) | |
| Surgical, elective | 6 (2.8) | 0 (0.0) | |
| Location at time of ICU demand—no. (%) | 0.04 | ||
| Emergency room | 142 (66.0) | 6 (37.5) | |
| Ward | 58 (27.0) | 10 (62.5) | |
| Postoperative recovery room | 9 (4.2) | 0 (0.0) | |
| Operating theatre | 6 (2.8) | 0 (0.0) | |
| Time of demand for ICU admission—no. (%) | 0.25 | ||
| 00:00–05:59 | 48 (22.3) | 2 (12.5) | |
| 06:00–11:59 | 29 (13.5) | 5 (31.3) | |
| 12:00–17:59 | 77 (35.8) | 4 (25.0) | |
| 18:00–23:59 | 61 (28.4) | 5 (31.3) | |
| Availability of ICU beds at time of ICU demand—no. (%) | 0.55 | ||
| >4 beds | 92 (42.8) | 5 (31.2) | |
| 3–4 beds | 66 (30.7) | 7 (43.8) | |
| 0–2 beds | 57 (26.5) | 4 (25.0) | |
| Physician’s grade of experience—no. (%) | 0.047 | ||
| ICU specialist | 171 (79.5) | 16 (100.0) | |
| ICU fellow | 44 (20.5) | 0 (0.0) | |
| Written documentation of ICU refusal—no. (%) | 0.40 | ||
| Present | 139 (64.7) | 12 (75.0) | |
| Absent | 76 (35.3) | 4 (25.0) | |
| Duration of ICU consultation—no. (%) | 0.78 | ||
| 1–15 min | 132 (61.4) | 10 (62.5) | |
| 16–30 min | 65 (30.2) | 4 (25.0) | |
| 31–90 min | 18 (8.4) | 2 (12.5) | |
| Consultation, type—no. (%) | 0.71 | ||
| At bedside | 191 (88.8) | 14 (87.5) | |
| By phone and chart | 23 (10.7) | 2 (12.5) | |
| By phone only | 1 (0.5) | 0 (0.0) |
| Direct Admission | Delayed Admission 1 | p Value | |
|---|---|---|---|
| (N = 1988) | (N = 14) | ||
| Deaths in ICU—no. (%) | 90 (4.5) | 3 (21.4) | 0.02 |
| Deaths in hospital—no. (%) | 150 (7.5) | 3 (21.4) | 0.09 |
| Deaths in hospital within 7 days—no. (%) | 85 (4.3) | 0 (0.0) | 1.00 |
| Death in hospital, according to treatment limitations at time of ICU demand—no./total of subgroup [%] | |||
| No limitation | 108/1711 [6.3] | 2/11 [18.2] | 0.13 |
| Any limitation 2 | 42/277 [15.2] | 1/3 [33.3] | 0.24 |
| Time between refusal and ICU admission—no. (%) | n.a. | ||
| <2 d | - | 9 (64.3) | |
| 2 to <4 d | - | 4 (28.6) | |
| 4 to 7 d | - | 1 (7.1) | |
| ICU LOS—no. (%) | <0.01 | ||
| <2 d | 1442 (72.5) | 7 (50.0) | |
| 2 to <7 d | 439 (22.1) | 2 (14.3) | |
| 7 to 60 d | 107 (5.4) | 5 (35.7) | |
| LOS in hospital after first ICU demand—no. (%) | 0.02 | ||
| <7 d | 939 (47.2) | 2 (14.3) | |
| 7 to <14 d | 542 (27.3) | 5 (35.7) | |
| 14 to 147 d | 507 (25.5) | 7 (50.0) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sridharan, G.; Fleury, Y.; Hergafi, L.; Doll, S.; Ksouri, H. Triage of Critically Ill Patients: Characteristics and Outcomes of Patients Refused as Too Well for Intensive Care. J. Clin. Med. 2023, 12, 5513. https://doi.org/10.3390/jcm12175513
Sridharan G, Fleury Y, Hergafi L, Doll S, Ksouri H. Triage of Critically Ill Patients: Characteristics and Outcomes of Patients Refused as Too Well for Intensive Care. Journal of Clinical Medicine. 2023; 12(17):5513. https://doi.org/10.3390/jcm12175513
Chicago/Turabian StyleSridharan, Govind, Yvan Fleury, Leila Hergafi, Sébastien Doll, and Hatem Ksouri. 2023. "Triage of Critically Ill Patients: Characteristics and Outcomes of Patients Refused as Too Well for Intensive Care" Journal of Clinical Medicine 12, no. 17: 5513. https://doi.org/10.3390/jcm12175513
APA StyleSridharan, G., Fleury, Y., Hergafi, L., Doll, S., & Ksouri, H. (2023). Triage of Critically Ill Patients: Characteristics and Outcomes of Patients Refused as Too Well for Intensive Care. Journal of Clinical Medicine, 12(17), 5513. https://doi.org/10.3390/jcm12175513