Sequential Intraoperative Evaluation of Rotational Stability of Cementless Stem in Total Hip Arthroplasty: A Broach-Based Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Surgical Planning and Technique
2.3. Evaluation of Rotational Stability
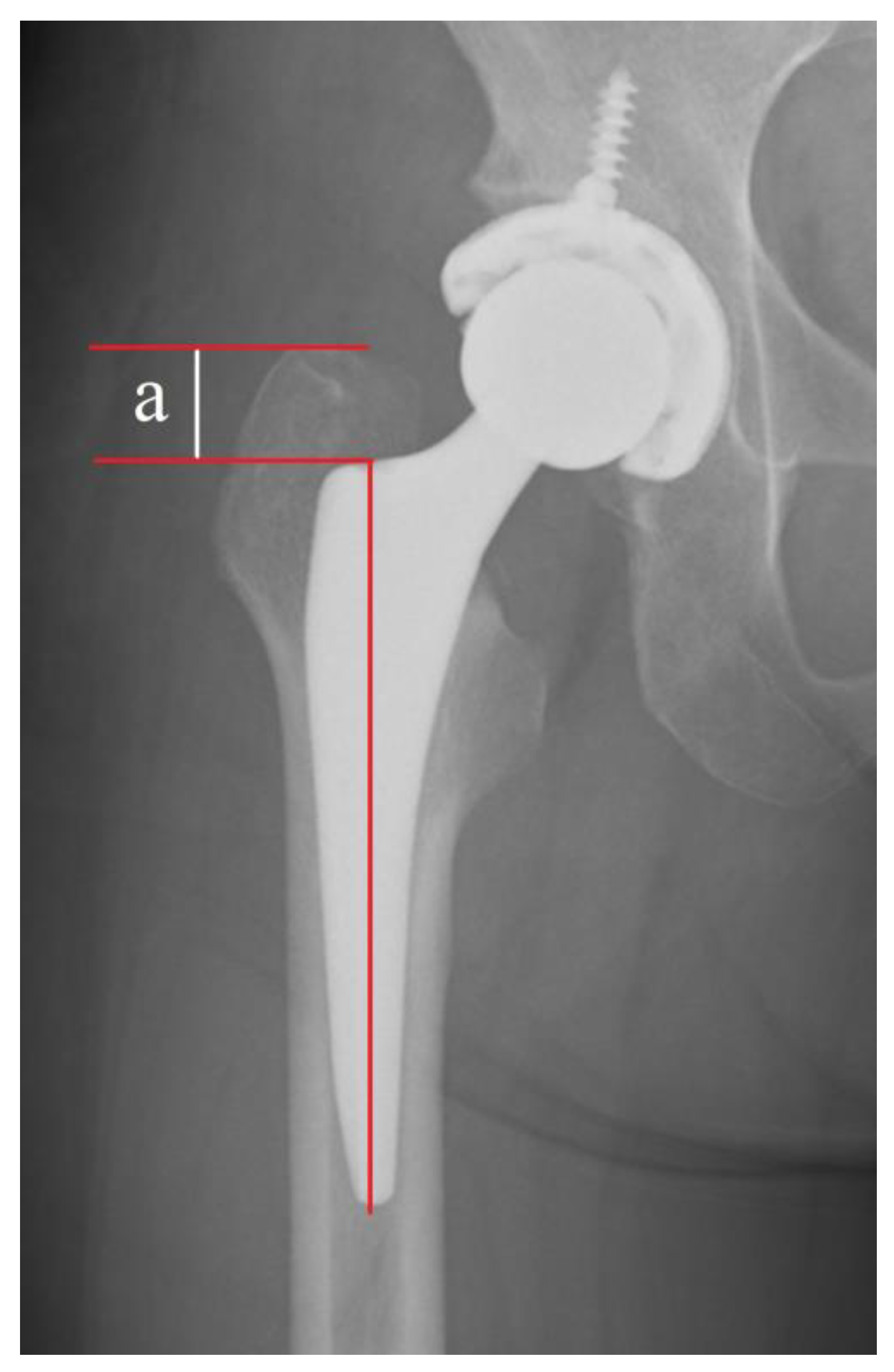
2.4. Radiographic Evaluation
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ethgen, O.; Bruyère, O.; Richy, F.; Dardennes, C.; Reginster, J.Y. Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J. Bone Jt. Surg. Am. 2004, 86, 963–974. [Google Scholar] [CrossRef] [PubMed]
- Bojescul, J.A.; Xenos, J.S.; Callaghan, J.J.; Savory, C.G. Results of porous-coated anatomic total hip arthroplasty without cement at fifteen years: A concise follow-up of a previous report. J. Bone Jt. Surg. Am. 2003, 85, 1079–1083. [Google Scholar] [CrossRef] [PubMed]
- Reigstad, O.; Siewers, P.; Røkkum, M.; Espehaug, B. Excellent long-term survival of an uncemented press-fit stem and screw cup in young patients: Follow-up of 75 hips for 15–18 years. Acta Orthop. 2008, 79, 194–202. [Google Scholar] [CrossRef] [PubMed]
- McLaughlin, J.R.; Lee, K.R. Total hip arthroplasty with an uncemented tapered femoral component. J. Bone Jt. Surg. Am. 2008, 90, 1290–1296. [Google Scholar] [CrossRef] [PubMed]
- Ateschrang, A.; Weise, K.; Weller, S.; Stöckle, U.; de Zwart, P.; Ochs, B.G. Long-term results using the straight tapered femoral cementless hip stem in total hip arthroplasty: A minimum of twenty-year follow-up. J. Arthroplast. 2014, 29, 1559–1565. [Google Scholar] [CrossRef]
- Attenello, J.; Chan, S.; Naito, K.; Saruwatari, M.; Saito, S.; Andrews, S.; Nakasone, C. Early perioperative complication rates and subsidence with the Tribute® short cementless, tapered stem in primary total hip arthroplasty. J. Orthop. 2019, 16, 118–122. [Google Scholar] [CrossRef]
- Al-Najjim, M.; Khattak, U.; Sim, J.; Chambers, I. Differences in subsidence rate between alternative designs of a commonly used uncemented femoral stem. J. Orthop. 2016, 13, 322–326. [Google Scholar] [CrossRef]
- Del Buono, A.; Denaro, V.; Maffulli, N. Genetic susceptibility to aseptic loosening following total hip arthroplasty: A systematic review. Br. Med. Bull. 2012, 101, 39–55. [Google Scholar] [CrossRef]
- Khanuja, H.S.; Vakil, J.J.; Goddard, M.S.; Mont, M.A. Cementless femoral fixation in total hip arthroplasty. J. Bone Jt. Surg. Am. 2011, 93, 500–509. [Google Scholar] [CrossRef]
- Moritz, N.; Alm, J.J.; Lankinen, P.; Mäkinen, T.J.; Mattila, K.; Aro, H.T. Quality of intertrochanteric cancellous bone as predictor of femoral stem RSA migration in cementless total hip arthroplasty. J. Biomech. 2011, 44, 221–227. [Google Scholar] [CrossRef]
- Chareancholvanich, K.; Bourgeault, C.A.; Schmidt, A.H.; Gustilo, R.B.; Lew, W.D. In vitro stability of cemented and cementless femoral stems with compaction. Clin. Orthop. Relat. Res. 2002, 394, 290–302. [Google Scholar] [CrossRef] [PubMed]
- Green, J.R.; Nemzek, J.A.; Arnoczky, S.P.; Johnson, L.L.; Balas, M.S. The effect of bone compaction on early fixation of porous-coated implants. J. Arthroplast. 1999, 14, 91–97. [Google Scholar] [CrossRef] [PubMed]
- Aro, H.T.; Alm, J.J.; Moritz, N.; Mäkinen, T.J.; Lankinen, P. Low BMD affects initial stability and delays stem osseointegration in cementless total hip arthroplasty in women: A 2-year RSA study of 39 patients. Acta Orthop. 2012, 83, 107–114. [Google Scholar] [CrossRef] [PubMed]
- Kauppinen, T.; Kogevinas, M.; Johnson, E.; Becher, H.; Bertazzi, P.-A.; de Mesquita, H.B.B.; Coggon, D.; Green, L.; Littorin, M.; Lynge, E.; et al. Chemical exposure in manufacture of phenoxy herbicides and chlorophenols and in spraying of phenoxy herbicides. Am. J. Ind. Med. 1993, 23, 903–920. [Google Scholar] [CrossRef]
- Nichkova, M.; Marco, M.P. Biomonitoring human exposure to organohalogenated substances by measuring urinary chlorophenols using a high-throughput screening (HTS) immunochemical method. Environ. Sci. Technol. 2006, 40, 2469–2477. [Google Scholar] [CrossRef]
- Pflüger, G.; Junk-Jantsch, S.; Schöll, V. Minimally invasive total hip replacement via the anterolateral approach in the supine position. Int. Orthop. 2007, 31 (Suppl. S1), S7–S11. [Google Scholar] [CrossRef][Green Version]
- Varini, E.; Cristofolini, L.; Traina, F.; Viceconti, M.; Toni, A. Can the rasp be used to predict intra-operatively the primary stability that can be achieved by press-fitting the stem in cementless hip arthroplasty? Clin. Biomech. 2008, 23, 408–414. [Google Scholar] [CrossRef]
- Dorr, L.D.; Faugere, M.C.; Mackel, A.M.; Gruen, T.A.; Bognar, B.; Malluche, H.H. Structural and cellular assessment of bone quality of proximal femur. Bone 1993, 14, 231–242. [Google Scholar] [CrossRef]
- Nakaya, R.; Takao, M.; Hamada, H.; Sakai, T.; Sugano, N. Reproducibility of the Dorr classification and its quantitative indices on plain radiographs. Orthop. Traumatol. Surg. Res. 2019, 105, 17–21. [Google Scholar] [CrossRef]
- Suksathien, Y.; Sueajui, J. Mid-term results of short stem total hip arthroplasty in patients with osteonecrosis of the femoral head. Hip Int. 2019, 29, 603–608. [Google Scholar] [CrossRef]
- Bornes, T.D.; Radomski, L.R.; Bonello, J.P.; Mortensen-Truscott, L.; Safir, O.A.; Gross, A.E.; Kuzyk, P.R.T. Subsidence of a Single-Taper Femoral Stem in Primary Total Hip Arthroplasty: Characterization, Associated Factors, and Sequelae. J. Arthroplast. 2023, 38, S174–S178. [Google Scholar] [CrossRef] [PubMed]
- Yan, Z.; Xiong, X.; Tao, J.; Wang, S. Association of bone mineral density with trichlorophenol: A population-based study. BMC Musculoskelet. Disord. 2023, 24, 202. [Google Scholar] [CrossRef] [PubMed]
- Kold, S.; Bechtold, J.E.; Ding, M.; Chareancholvanich, K.; Rahbek, O.; Søballe, K. Compacted cancellous bone has a spring-back effect. Acta Orthop. Scand. 2003, 74, 591–595. [Google Scholar] [CrossRef] [PubMed]
- Windolf, M.; Muths, R.; Braunstein, V.; Gueorguiev, B.; Hänni, M.; Schwieger, K. Quantification of cancellous bone-compaction due to DHS Blade insertion and influence upon cut-out resistance. Clin. Biomech. 2009, 24, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Arthur Moore, T.L.; Gibson, L.J. Microdamage accumulation in bovine trabecular bone in uniaxial compression. J. Biomech. Eng. 2002, 124, 63–71. [Google Scholar] [CrossRef] [PubMed]
- Vresilovic, E.J.; Hozack, W.J.; Rothman, R.H. Radiographic assessment of cementless femoral components. Correlation with intraoperative mechanical stability. J. Arthroplast. 1994, 9, 137–141. [Google Scholar] [CrossRef]
- Sharkey, P.F.; Albert, T.J.; Hume, E.L.; Rothman, R.H. Initial stability of a collarless wedge-shaped prosthesis in the femoral canal. Semin. Arthroplast. 1990, 1, 87–90. [Google Scholar]
- Kim, J.T.; Jeong, H.J.; Lee, S.J.; Kim, H.J.; Yoo, J.J. Does Proximally Coated Single-Wedge Cementless Stem Work Well in Dorr Type C Femurs? Minimum 10-year Followup. Indian J. Orthop. 2019, 53, 94–101. [Google Scholar] [CrossRef]
- Isaacsn, B.M.; Jeyapalina, S. Osseointegration: A review of the fundamentals for assuring skeletal fixation. Orthop. Res. Rev. 2014, 6, 55–65. [Google Scholar] [CrossRef]


| Single Wedge (n = 52 Hips) | |
|---|---|
| Sex, male:female (no. of hips) | 9:43 |
| Age (yr) | 63.3 ± 11.7 (39–87) |
| Height (cm) | 155.0 ± 7.2 (141.5–177.0) |
| Weight (kg) | 61.7 ± 12.0 (40.8–92.0) |
| BMI (kg/m2) | 25.6 ± 3.9 (19.0–35.6) |
| Unstable Group (n = 35 Hips) | Stable Group (n = 17 Hips) | p Value | |
|---|---|---|---|
| BMD of total femur (g/cm2) | 0.79 ± 0.14 (0.56–1.21) | 0.74 ± 0.14 (0.54–1.14) | 0.25 |
| BMD of femoral neck (g/cm2) | 0.73 ± 0.12 (0.62–1.21) | 0.73 ± 0.15 (0.52–1.10) | 0.89 |
| BMD of trochanter (g/cm2) | 0.60 ± 0.13 (0.41–0.94) | 0.55 ± 0.12 (0.37–0.90) | 0.23 |
| BMD of intertrochanteric region (g/cm2) | 0.80 ± 0.18 (0.62–1.18) | 0.80 ± 0.20 (0.6–1.10) | 0.99 |
| Intraoperative bleeding (mL) | 310 ± 218 (44–611) | 404 ± 164 (43–739) | 0.10 |
| Cortical index | 0.51 ± 0.09 (0.37–0.61) | 0.49 ± 0.06 (0.33–0.67) | 0.26 |
| Time interval (min) | 38.1 ± 11.6 (26 to 71) | 37.4 ± 13.5 (22 to 62) | 0.49 |
| Dorr A:B:C (no. of hips) | 12:15:8 | 8:8:1 | 0.30 |
| No Subsidence Group (n = 47 Hips) | Subsidence Group (n = 5 Hips) | p Value | |
|---|---|---|---|
| BMD of total femur (g/cm2) | 0.77 ± 0.15 (0.54–1.21) | 0.78 ± 0.10 (0.62–0.85) | 0.37 |
| BMD of femoral neck (g/cm2) | 0.74 ± 0.13 (0.52–1.21) | 0.67 ± 0.08 (0.57–0.77) | 0.17 |
| BMD of trochanter (g/cm2) | 0.59 ± 0.14 (0.37–0.94) | 0.58 ± 0.09 (0.48–0.71) | 0.33 |
| BMD of intertrochanteric region (g/cm2) | 0.88 ± 0.17 (0.60–1.18) | 0.91 ± 0.13 (0.72–1.05) | 0.47 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kinoshita, S.; Kinoshita, K.; Sakamoto, T.; Seo, H.; Suzuki, M.; Yamamoto, T. Sequential Intraoperative Evaluation of Rotational Stability of Cementless Stem in Total Hip Arthroplasty: A Broach-Based Study. J. Clin. Med. 2023, 12, 5444. https://doi.org/10.3390/jcm12175444
Kinoshita S, Kinoshita K, Sakamoto T, Seo H, Suzuki M, Yamamoto T. Sequential Intraoperative Evaluation of Rotational Stability of Cementless Stem in Total Hip Arthroplasty: A Broach-Based Study. Journal of Clinical Medicine. 2023; 12(17):5444. https://doi.org/10.3390/jcm12175444
Chicago/Turabian StyleKinoshita, Sakae, Koichi Kinoshita, Tetsuya Sakamoto, Hajime Seo, Masahiro Suzuki, and Takuaki Yamamoto. 2023. "Sequential Intraoperative Evaluation of Rotational Stability of Cementless Stem in Total Hip Arthroplasty: A Broach-Based Study" Journal of Clinical Medicine 12, no. 17: 5444. https://doi.org/10.3390/jcm12175444
APA StyleKinoshita, S., Kinoshita, K., Sakamoto, T., Seo, H., Suzuki, M., & Yamamoto, T. (2023). Sequential Intraoperative Evaluation of Rotational Stability of Cementless Stem in Total Hip Arthroplasty: A Broach-Based Study. Journal of Clinical Medicine, 12(17), 5444. https://doi.org/10.3390/jcm12175444





