Simplifying Forehead and Temple Reconstruction: A Narrative Review
Abstract
1. Introduction
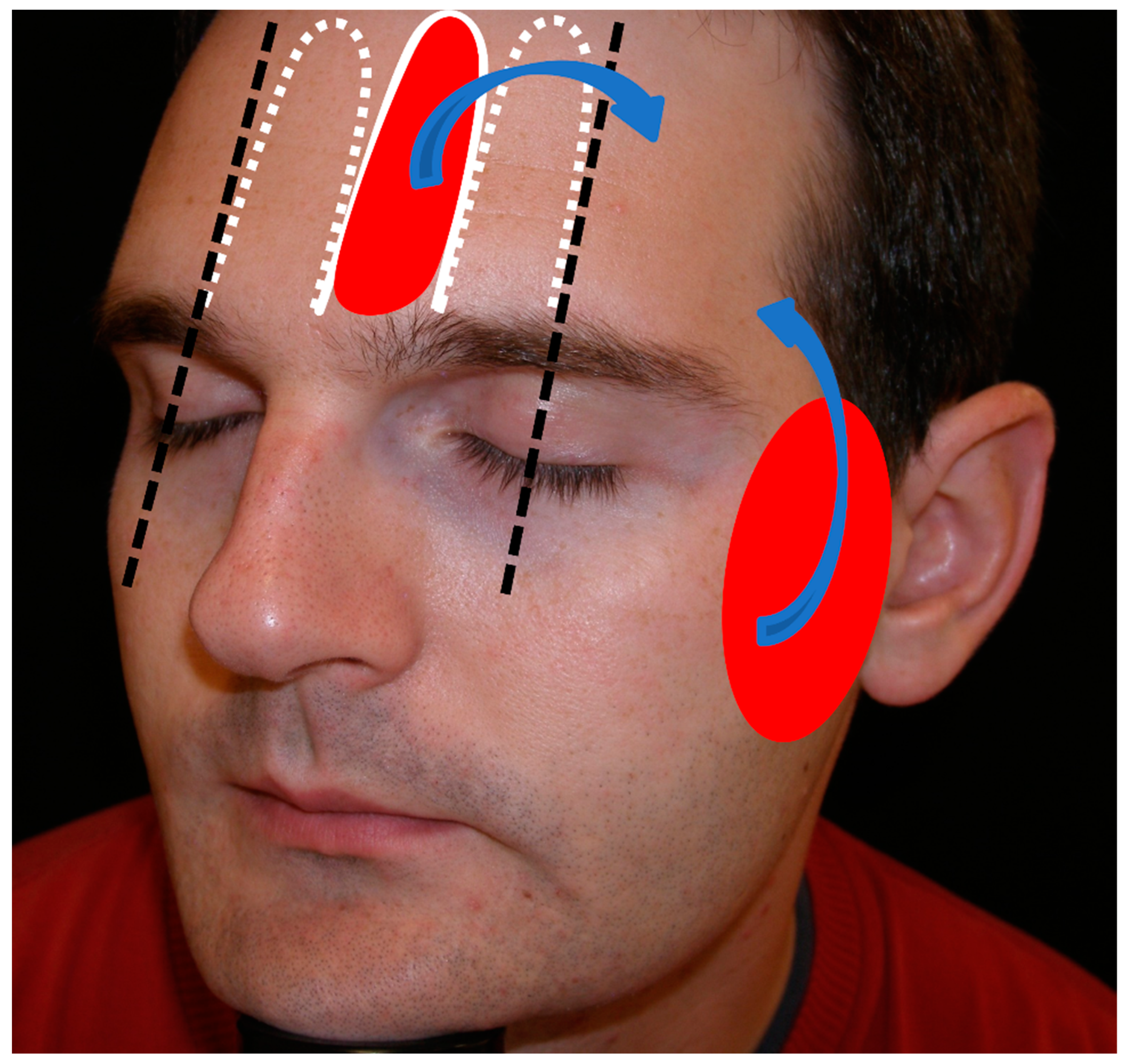
2. Anatomy
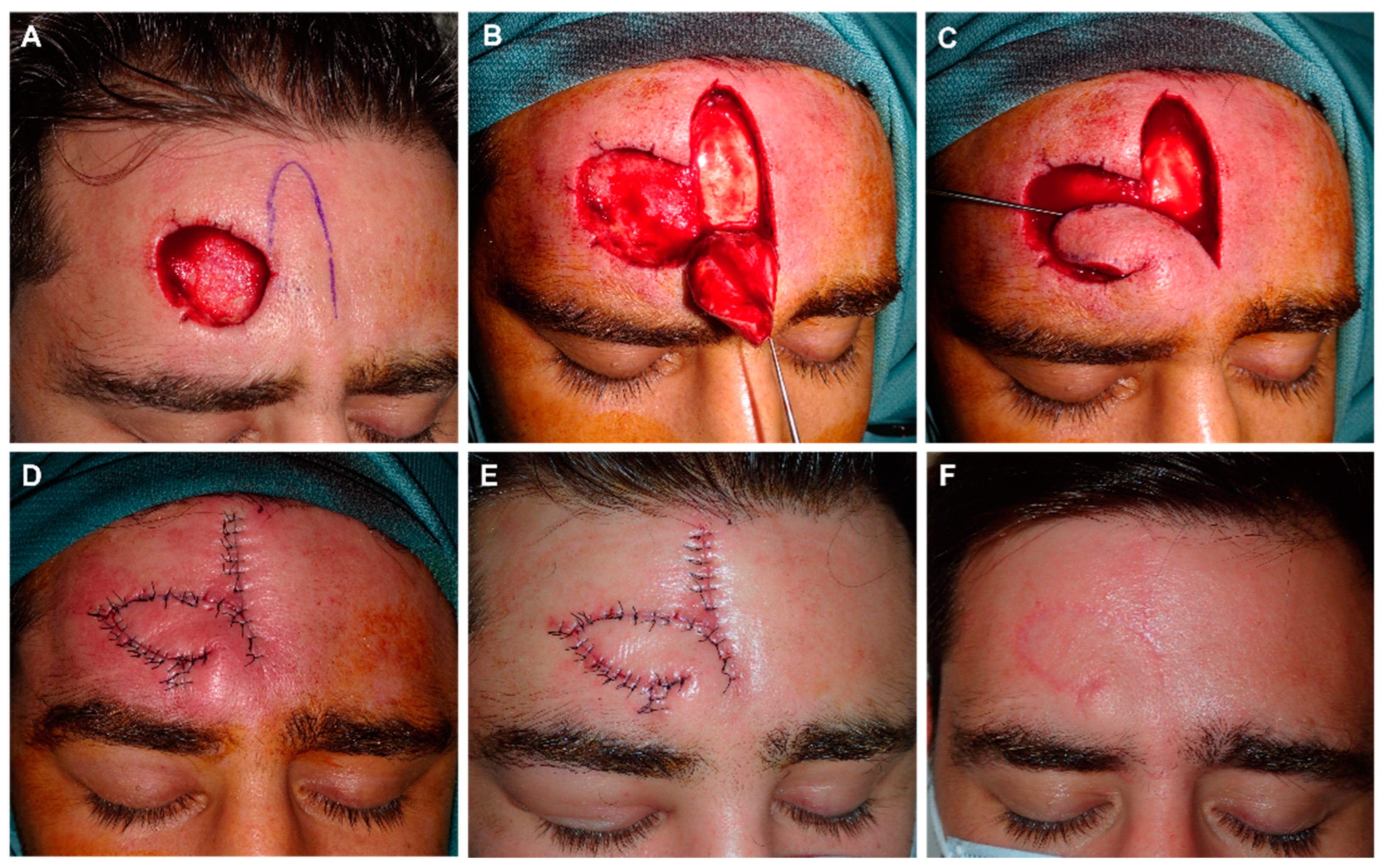
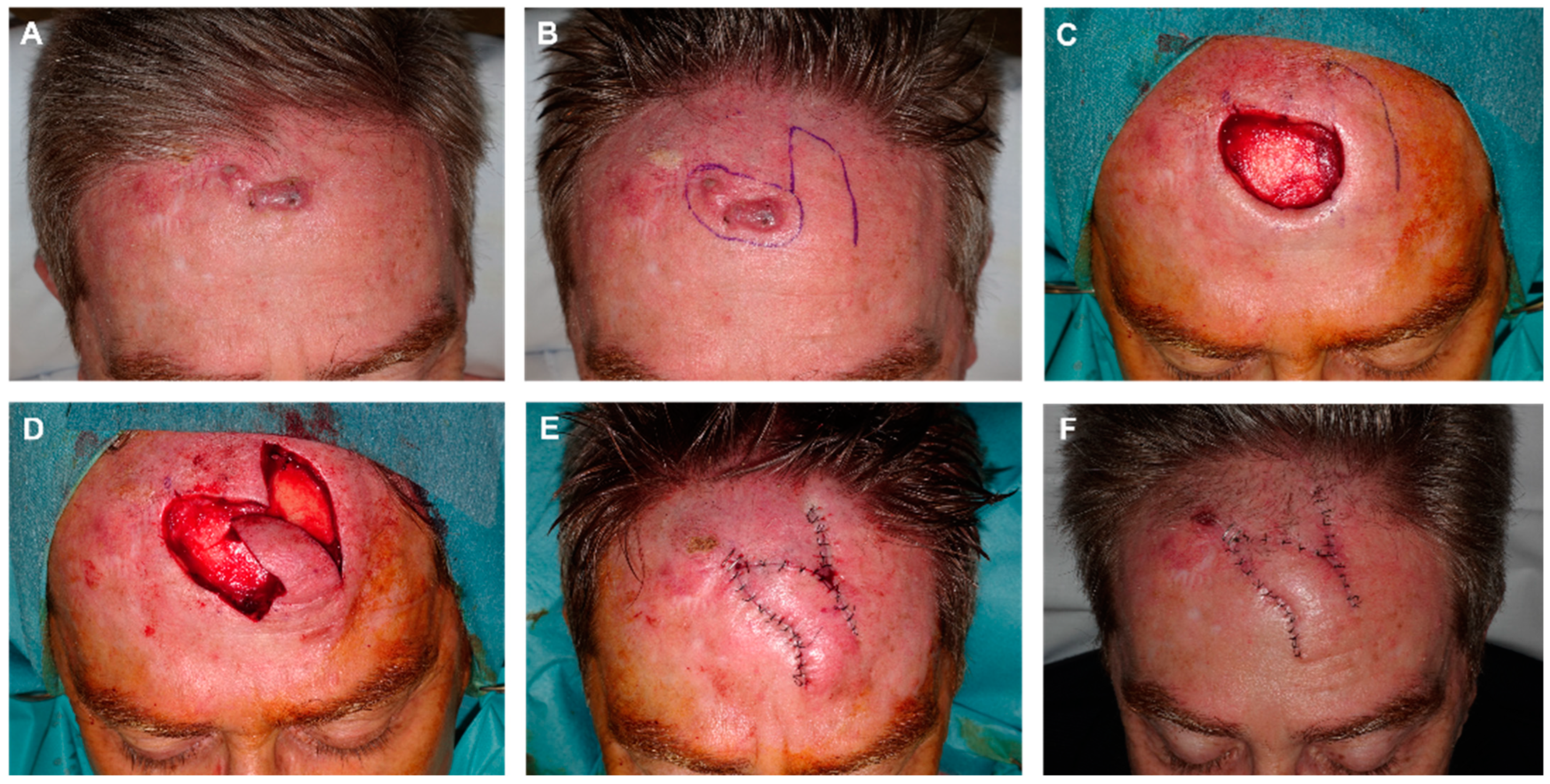
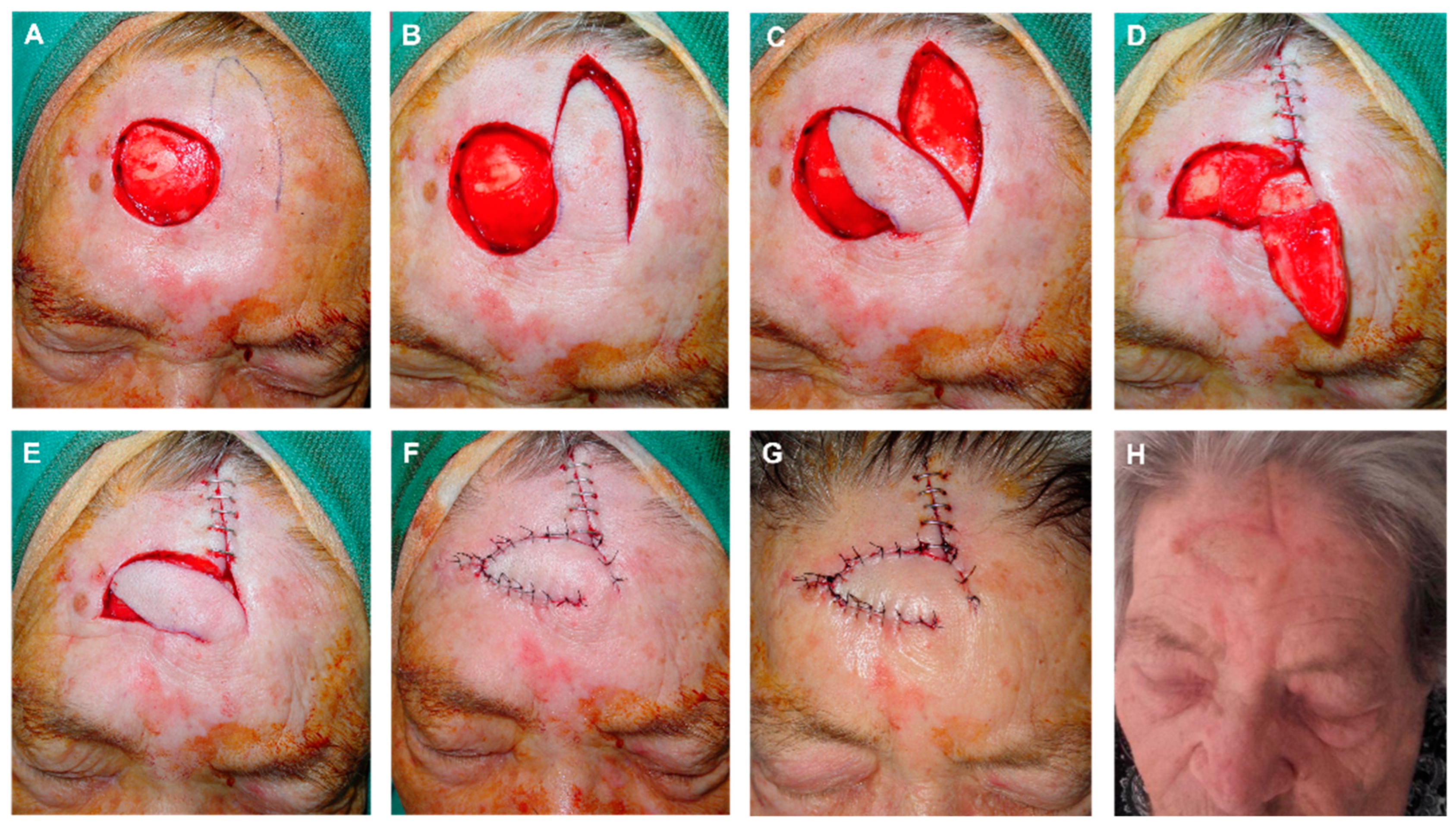
3. Median and Lateral Forehead Reconstruction
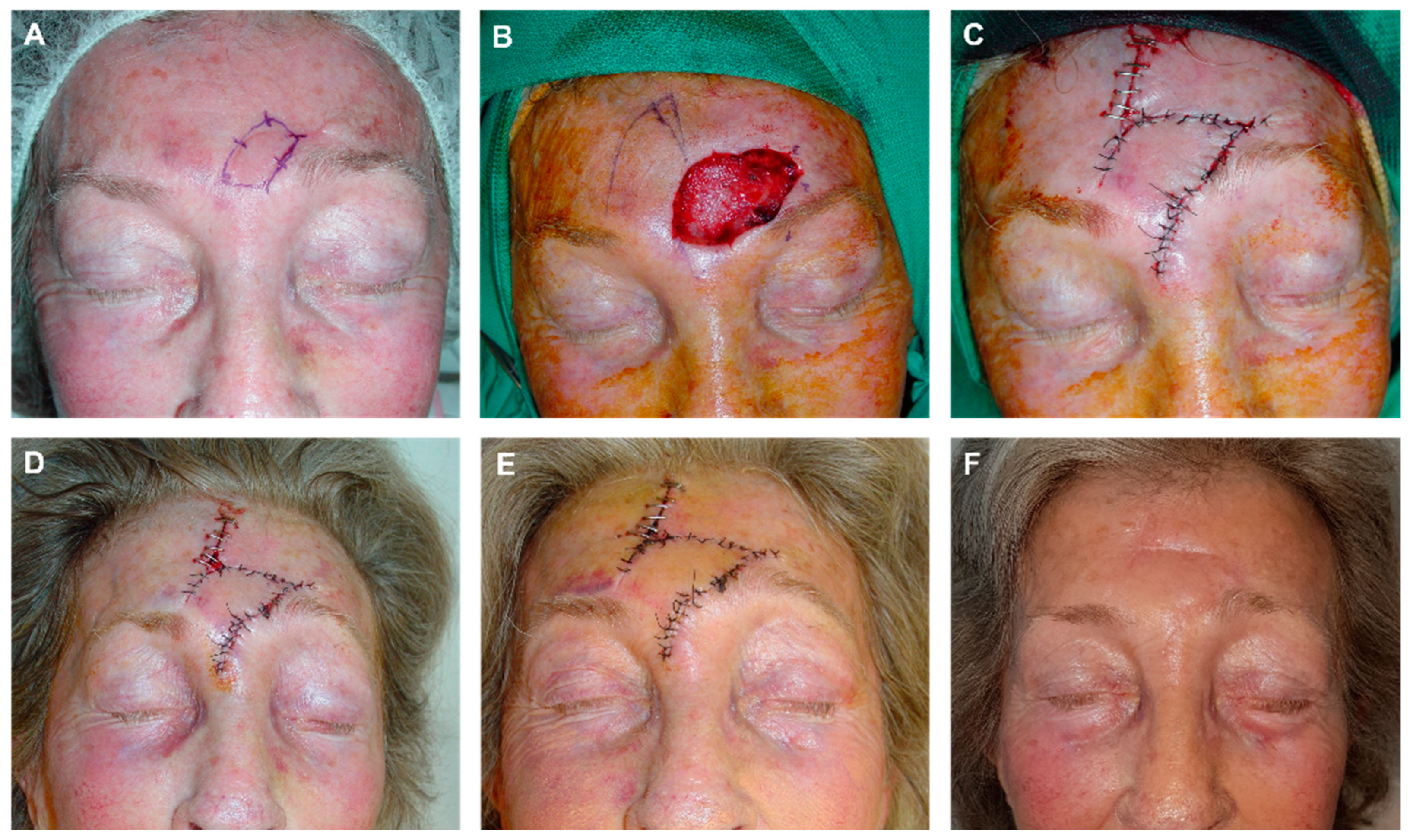
3.1. Advancement Flaps
3.2. Rotation Flaps
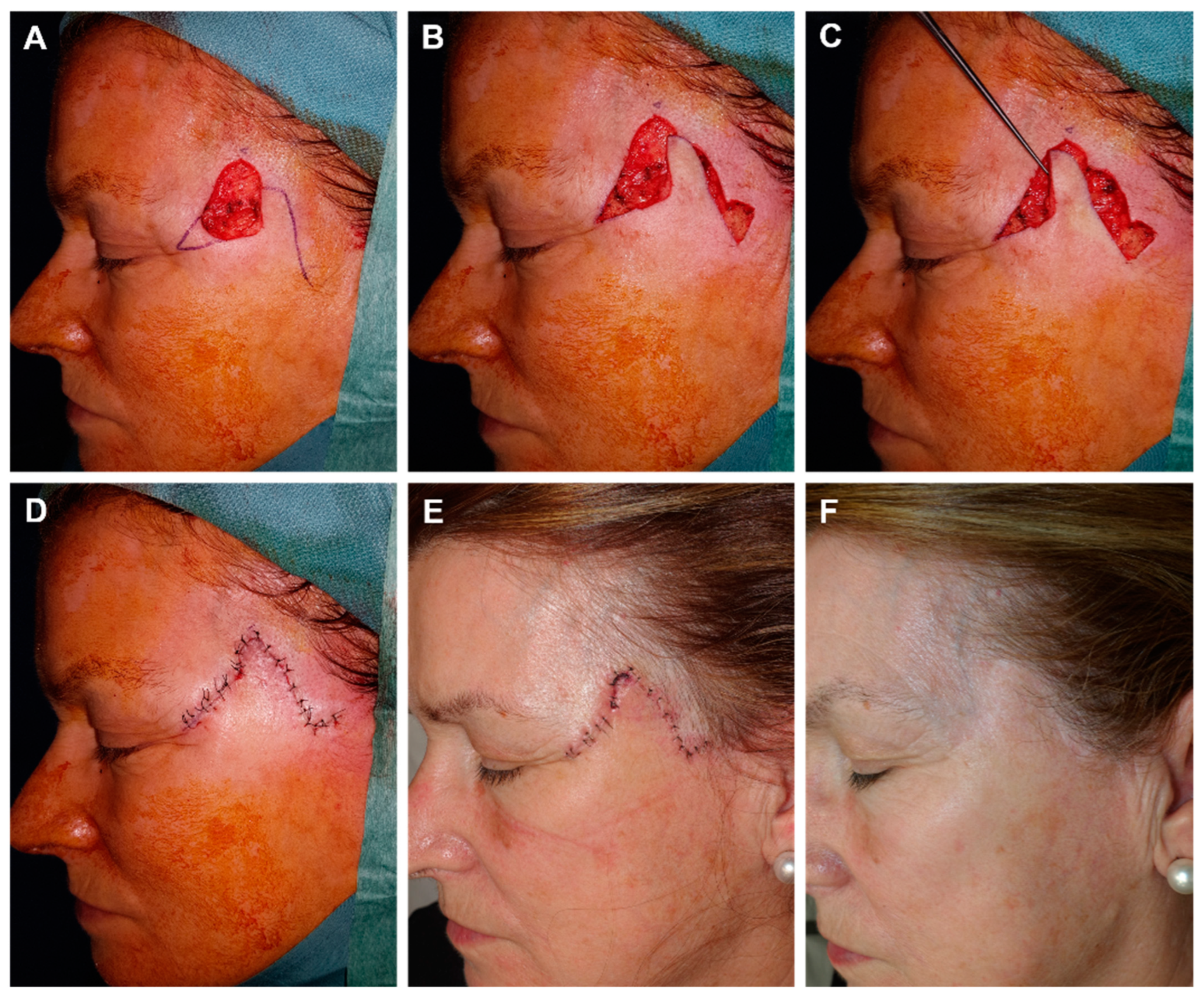
3.3. Transposition Flaps
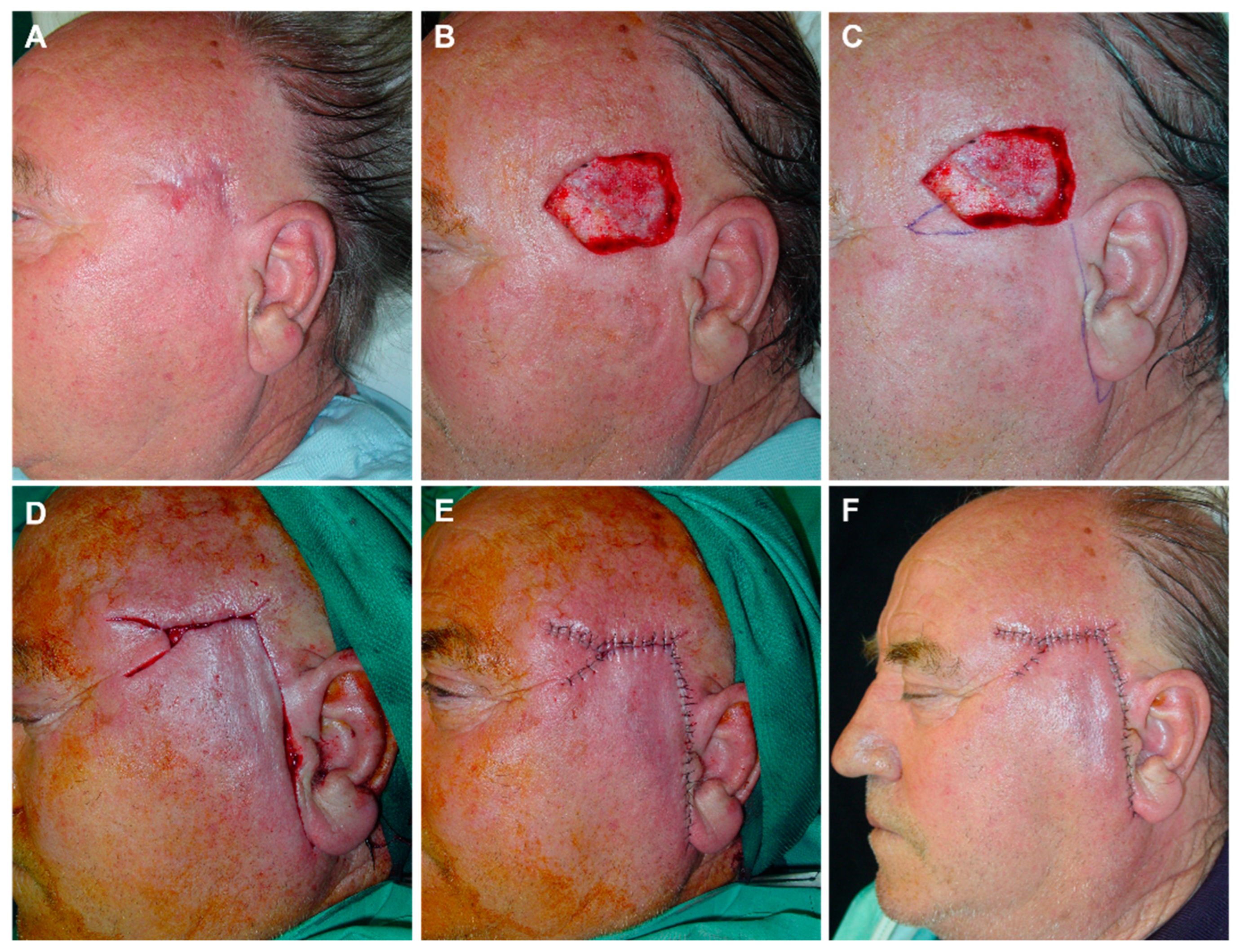
4. Temple Reconstruction
4.1. Rotation Flaps
4.2. Advancement Flaps
4.3. Transposition Flaps
5. Eyebrows Reconstruction
6. Glabella Reconstruction
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Garritano, F.G.; Quatela, V.C. Surgical Anatomy of the Upper Face and Forehead. Facial Plast. Surg. 2018, 34, 109–113. [Google Scholar] [CrossRef]
- Seline, P.C.; Siegle, R.J. Forehead reconstruction. Dermatol. Clin. 2005, 23, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Freund, R.M.; Nolan, W.B.I.I.I. Correlation between brow lift outcomes and aesthetic ideals for eyebrow height and shape in females. Plast. Reconstr. Surg. 1996, 97, 1343–1348. [Google Scholar] [CrossRef] [PubMed]
- Martinovic, M.; Lupi-Ferandin, S.; Tokic, D.; Usljebrka, M.; Rados, A.; Pojatina, A.; Kadic, S.; Puizina, E.; Mihovilovic, A.; Kumric, M.; et al. Objective skin quality assessment after reconstructive procedures for facial skin defects. J. Clin. Med. 2022, 11, 4471. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.S.; Kim, J.O.; Kim, N.G.; Lee, Y.J.; Park, Y.J.; Kim, J.S. A comparison of the cocal flap and skin graft by Location of face in reconstruction after resection of facial skin cancer. Arch. Craniofacial Surg. 2017, 18, 255–260. [Google Scholar] [CrossRef] [PubMed]
- Quatrano, N.A.; Dawli, T.B.; Park, A.J.; Samie, F.H. Simplifying Forehead Reconstruction: A Review of More Than 200 Cases. Facial Plast. Surg. 2016, 32, 309–314. [Google Scholar] [PubMed]
- Arnaud, D.; Beuzeboc, M.; Huguier, V.; Darsonval, V.; Rousseau, P. Forehead and temple aesthetic reconstruction. Ann. Chir. Plast. Esthet. 2013, 58, 389–427. [Google Scholar] [CrossRef] [PubMed]
- Pomaranski, M.R.; Krull, E.A.; Balle, M.R. Use of the Z-plasty technique for forehead defects. Dermatol. Surg. 2005, 31, 1720–1723. [Google Scholar] [PubMed]
- Jackson, I.T. (Ed.) Forehead reconstruction. In Local Flaps in Head and Neck Reconstruction; Mosby: St. Louis, MO, USA, 1985; pp. 43–85. [Google Scholar]
- Siegle, R.J. Reconstruction of the forehead. In Local Flaps in Facial Reconstruction; Baker, S.R., Swanson, N.A., Eds.; Mosby Year Book: St. Louis, MO, USA, 1995; pp. 422–442. [Google Scholar]
- Redondo, P. Geometric reconstructive surgery of the temple and lateral forehead: The best election for avoiding a graft. Dermatol. Surg. 2008, 34, 1553–1560. [Google Scholar] [CrossRef]
- Babakurban, S.T.; Cakmak, O.; Kendir, S.; Elhan, A.; Quatela, V.C. Temporal branch of the facial nerve and its relationship to fascial layers. Arch. Facial Plast. Surg. 2010, 12, 16–23. [Google Scholar] [CrossRef] [PubMed]
- Rose, V.; Overstall, S.; Moloney, D.M.; Powell, B.W. The H-flap: A useful flap for forehead reconstruction. Br. J. Plast. Surg. 2001, 54, 705–707. [Google Scholar] [CrossRef]
- Ghosh, A.; Chakrabarti, S.; Rai, A.K.; Choubey, T.; Panuganti, A.; Bhukar, S. O to T Flap for Central Forehead Defect Reconstruction. J. Maxillofac. Oral. Surg. 2020, 19, 523–526. [Google Scholar] [CrossRef] [PubMed]
- Gurunluoglu, R.; Shafighi, M.; Williams, S.A.; Glasgow, M. Reconstruction of large supra-eyebrow and forehead defects using the hatchet flap principle and sparing sensory nerve branches. Ann. Plast. Surg. 2012, 68, 37–42. [Google Scholar] [CrossRef]
- Gargano, F.; Alfanco, C. Versatility of the hatchet flap in facial reconstruction. Acta Chir. Plast. 2005, 47, 67. [Google Scholar] [PubMed]
- LeVasseur, J.G.; Mellette, J.R. Applications of the double O to Z flap repair for facial reconstruction. Dermatol. Surg. 2001, 27, 79–81. [Google Scholar] [PubMed]
- Tomás-Velázquez, A.; Redondo, P. Assessment of frontalis myocutaneous transposition flap for forehead reconstruction after Mohs surgery. JAMA Dermatol. 2018, 154, 708–711. [Google Scholar] [CrossRef] [PubMed]
- Redondo, P.; Rodriguez-Garijo, N.; Tomás-Velázquez, A. Forehead and frontal scalp reconstruction after resection of subcutaneous dermatofibrosarcoma protuberans. Dermatol. Surg. 2022, 48, 867–869. [Google Scholar] [CrossRef] [PubMed]
- Hussain, W. The contralateral subgaleal sliding flap for the single-stage reconstruction of large defects of the temple and lateral forehead. Br. J. Dermatol. 2014, 170, 952–955. [Google Scholar] [CrossRef] [PubMed]
- Salmon, P.J.M. Bridge flaps: A hybrid family of bipedicled flaps for the forehead, temple, and scalp: Experience with 103 cases. Dermatol. Surg. 2020, 46, 890–896. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, L.H.; Silapunt, S.; Alam, M.; Peterson, S.R.; Jih, M.H.; Kimyai-Asadi, A. Surgical repair of temple defects after Mohs micrographic surgery. J. Am. Acad. Dermatol. 2005, 52, 631–636. [Google Scholar] [CrossRef]
- Hicks, D.L.; Watson, D. Soft tissue reconstruction of the forehead and temple. Facial Plast. Surg. Clin. N. Am. 2005, 13, 243–251. [Google Scholar] [CrossRef] [PubMed]
- Figueira, E.; Wasserbauer, S.; Wu, A.; Huilgol, S.C.; Marzola, M.; Selva, D. Eyebrow reconstruction. Orbit 2017, 36, 273–284. [Google Scholar] [CrossRef] [PubMed]
- Silapunt, S.; Goldberg, L.H.; Peterson, S.R.; Gardner, E.S. Eyebrow reconstruction: Options for reconstruction of cutaneous defects of the eyebrow. Dermatol. Surg. 2004, 30, 530–535. [Google Scholar] [CrossRef] [PubMed]
- Manuel, R.; Faulhaber, J.; Johannes, B.; Moritz, F. A novel approach to reconstruct defects of the lower forehead without eyebrow shortening. J. Dtsch. Dermatol. Ges. 2021, 19, 637–640. [Google Scholar] [PubMed]
- Alonso-Martínez, S.; Masa, I.; Salinas-Velasco, V. Nasal root island flap for reconstruction of glabellar defects. Ann. Plast. Surg. 2015, 74, 34–36. [Google Scholar] [CrossRef] [PubMed]






Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Redondo, P. Simplifying Forehead and Temple Reconstruction: A Narrative Review. J. Clin. Med. 2023, 12, 5399. https://doi.org/10.3390/jcm12165399
Redondo P. Simplifying Forehead and Temple Reconstruction: A Narrative Review. Journal of Clinical Medicine. 2023; 12(16):5399. https://doi.org/10.3390/jcm12165399
Chicago/Turabian StyleRedondo, Pedro. 2023. "Simplifying Forehead and Temple Reconstruction: A Narrative Review" Journal of Clinical Medicine 12, no. 16: 5399. https://doi.org/10.3390/jcm12165399
APA StyleRedondo, P. (2023). Simplifying Forehead and Temple Reconstruction: A Narrative Review. Journal of Clinical Medicine, 12(16), 5399. https://doi.org/10.3390/jcm12165399





