Non-Pharmacological Interventions for Pain Management in Hemodialysis: A Narrative Review
Abstract
1. Introduction
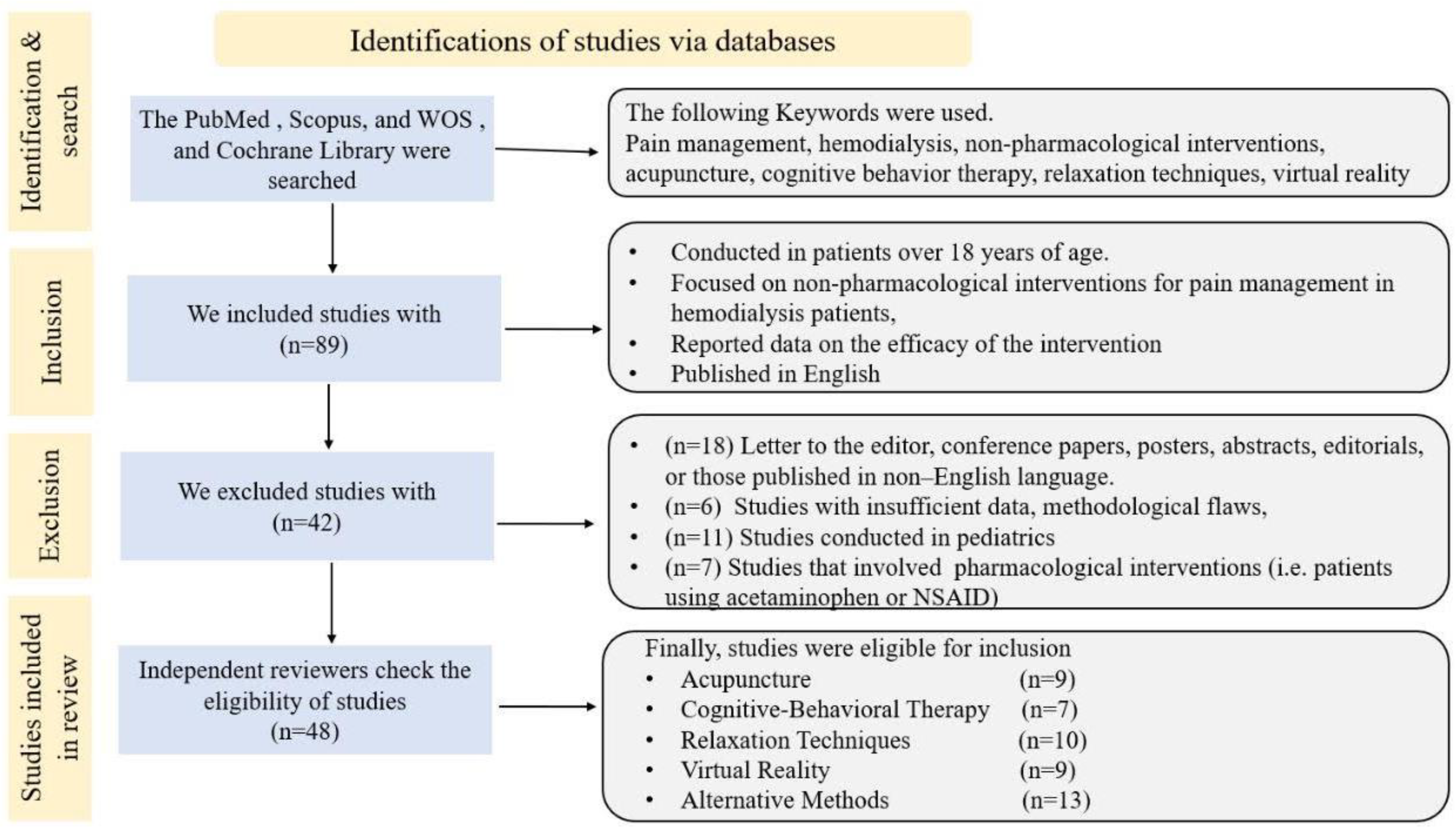
2. Methods
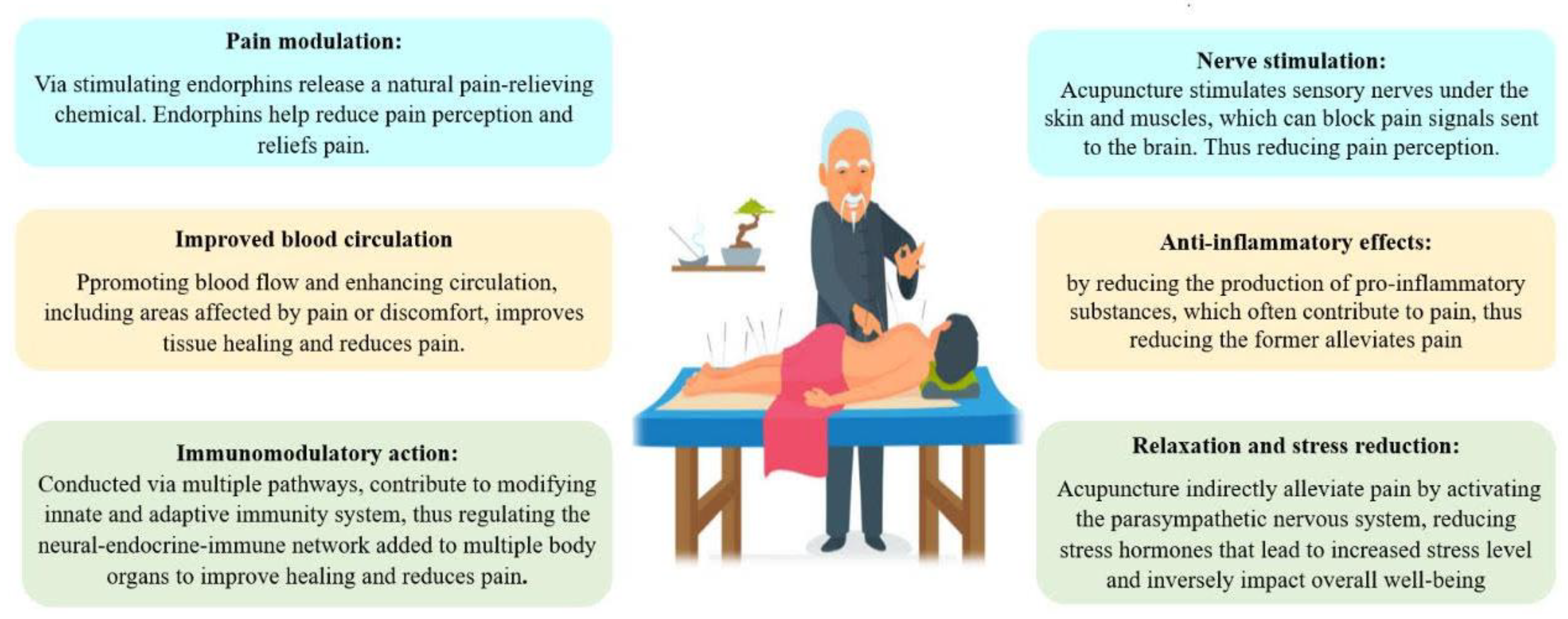
3. Acupuncture
4. Cognitive Behavioral Therapy (CBT)
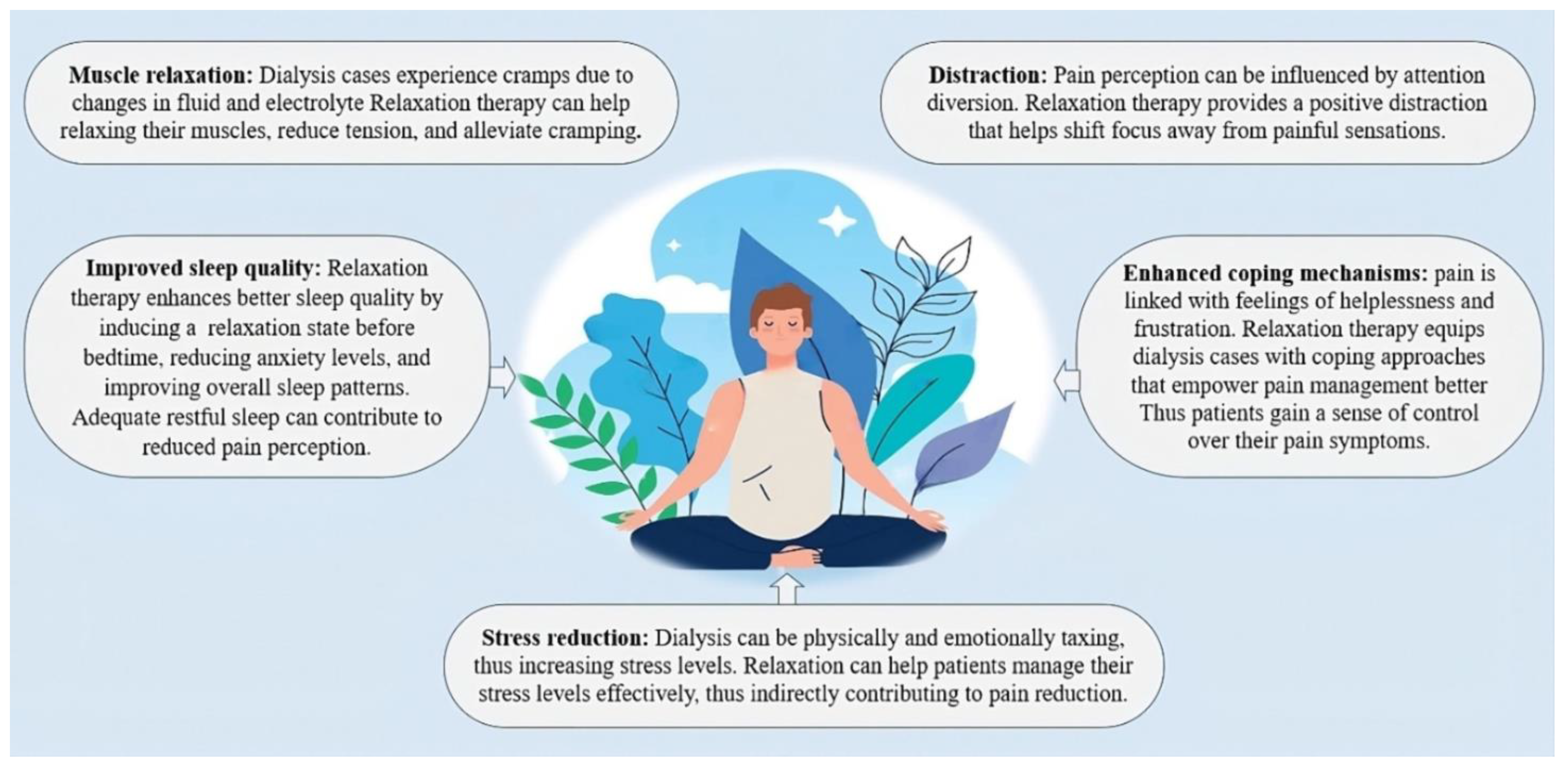
5. Relaxation Techniques
6. Virtual Reality
7. Other Alternative Methods
8. Discussion
9. Timing of Interventions
10. Side Effects of Non-Pharmacological Interventions
11. Study Limitations, Future Perspectives, and Further Research
12. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Davison, S.N. Pain in hemodialysis patients: Prevalence, cause, severity, and management. Am. J. Kidney Dis. 2003, 42, 1239–1247. [Google Scholar] [CrossRef] [PubMed]
- Thurlow, J.S.; Joshi, M.; Yan, G.; Norris, K.C.; Agodoa, L.Y.; Yuan, C.M.; Nee, R. Global Epidemiology of End-Stage Kidney Disease and Disparities in Kidney Replacement Therapy. Am. J. Nephrol. 2021, 52, 98–107. [Google Scholar] [CrossRef] [PubMed]
- Kafkia, T.; Chamney, M.; Drinkwater, A.; Pegoraro, M.; Sedgewick, J. Pain in Chronic Kidney Disease: Prevalence, Cause and Management. J. Ren. Care 2011, 37, 114–122. [Google Scholar] [CrossRef] [PubMed]
- dos Santos, P.R.; Mendonça, C.R.; Noll, M.; Borges, C.C.; Alves, P.M.; Dias, N.T.; Romeiro, A.M.d.S.; Barbosa, M.A.; Porto, C.C. Pain in Hemodialysis Patients: Prevalence, Intensity, Location, and Functional Interference in Daily Activities. Healthcare 2021, 9, 1375. [Google Scholar] [CrossRef] [PubMed]
- Davison, S.N.; Jhangri, G.S. Impact of Pain and Symptom Burden on the Health-Related Quality of Life of Hemodialysis Patients. J. Pain Symptom Manag. 2010, 39, 477–485. [Google Scholar] [CrossRef]
- Upadhyay, C.; Cameron, K.; Murphy, L.; Battistella, M. Measuring pain in patients undergoing hemodialysis: A review of pain assessment tools. Clin. Kidney J. 2014, 7, 367–372. [Google Scholar] [CrossRef]
- Kimmel, P.L.; Emont, S.L.; Newmann, J.M.; Danko, H.; Moss, A.H. ESRD patient quality of life: Symptoms, spiritual beliefs, psychosocial factors, and ethnicity. Am. J. Kidney Dis. 2003, 42, 713–721. [Google Scholar] [CrossRef]
- Theofilou, P. Quality of Life in Patients Undergoing Hemodialysis or Peritoneal Dialysis Treatment. J. Clin. Med. Res. 2011, 3, 132–138. [Google Scholar] [CrossRef]
- Hedayati, S.; Bosworth, H.; Kuchibhatla, M.; Kimmel, P.; Szczech, L. The predictive value of self-report scales compared with physician diagnosis of depression in hemodialysis patients. Kidney Int. 2006, 69, 1662–1668. [Google Scholar] [CrossRef]
- Dowell, D.; Haegerich, T.M.; Chou, R. CDC Guideline for Prescribing Opioids for Chronic Pain—United States, 2016. JAMA 2016, 315, 1624–1645. [Google Scholar] [CrossRef]
- Wilkinson, J.; Faleiro, R. Acupuncture in pain management. Contin. Educ. Anaesth. Crit. Care Pain 2007, 7, 135–138. [Google Scholar] [CrossRef]
- Dhond, R.P.; Yeh, C.; Park, K.; Kettner, N.; Napadow, V. Acupuncture modulates resting state connectivity in default and sensorimotor brain networks. Pain 2008, 136, 407–418. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Wang, X.; Ma, H.; Zhang, W. Mechanisms underlying acupuncture therapy in chronic kidney disease: A narrative overview of preclinical studies and clinical trials. Front. Nephrol. 2022, 2, 1006506. [Google Scholar] [CrossRef]
- Wang, M.; Liu, W.; Ge, J.; Liu, S. The immunomodulatory mechanisms for acupuncture practice. Front. Immunol. 2023, 14, 1147718. [Google Scholar] [CrossRef] [PubMed]
- Ma, Q. Somatotopic organization of autonomic reflexes by acupuncture. Curr. Opin. Neurobiol. 2022, 76, 102602. [Google Scholar] [CrossRef]
- Kim, K.H.; Lee, M.S.; Kim, T.-H.; Kang, J.W.; Choi, T.-Y.; Lee, J.D. Acupuncture and related interventions for symptoms of chronic kidney disease. Cochrane Database Syst. Rev. 2016, 2016, CD009440. [Google Scholar] [CrossRef]
- de Carvalho, M.C.; de Azevedo, J.N.; Azevedo, P.; Pires, C.; Laranjeira, M.; Machado, J.P. Effect of Acupuncture on Functional Capacity in Patients Undergoing Hemodialysis: A Patient-Assessor Blinded Randomized Controlled Trial. Healthcare 2022, 10, 1947. [Google Scholar] [CrossRef]
- Bullen, A.; Awdishu, L.; Lester, W.; Moore, T.; Trzebinska, D. Effect of Acupuncture or Massage on Health-Related Quality of Life of Hemodialysis Patients. J. Altern. Complement. Med. 2018, 24, 1069–1075. [Google Scholar] [CrossRef]
- de Carvalho, M.C.; de Azevedo, J.N.; Azevedo, P.; Pires, C.; Machado, J.P.; Laranjeira, M. Effectiveness of Acupuncture on Health-Related Quality of Life in Patients Receiving Maintenance Hemodialysis. Healthcare 2023, 11, 1355. [Google Scholar] [CrossRef]
- Tsai, L.-H.; Chen, C.-M.; Lin, L.-M.; Tsai, C.-C.; Han, Y.; See, L.-C. Acupressure reduces the severity of restless legs syndrome in hemodialysis patients: A cluster-randomized crossover pilot study. Biomed. J. 2022, 45, 533–541. [Google Scholar] [CrossRef]
- Zhang, L.; Li, Y.; Xiao, X.; Shi, Y.; Xu, D.; Li, N.; Deng, Y. Acupuncture for Uremic Pruritus: A Systematic Review and Meta-Analysis. J. Pain Symptom Manag. 2022, 65, e51–e62. [Google Scholar] [CrossRef] [PubMed]
- Çevik, B.; Taşcı, S. The effect of acupressure on upper extremity pain and quality of life in patients hemodialysis treatment: A Randomized Controlled Trial. Complement. Ther. Clin. Pr. 2020, 39, 101128. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.; Kim, T.; Kang, J.; Lee, M.; Kim, J.; Shin, M.; Jung, S.; Kim, A.; Kang, K.; Choi, S.; et al. P02.176. Acupuncture for symptom management in hemodialysis patients: A prospective, observational pilot study. BMC Complement. Altern. Med. 2012, 12, P232. [Google Scholar] [CrossRef]
- Lu, P.-H.; Lai, C.-C.; Chiu, L.-Y.; Wang, J.-Y.; Lu, P.-H. Comparative efficacy of Chinese herbal medicines for dialysis patients with uremic pruritus: A systematic review and network meta-analysis. Front. Pharmacol. 2023, 14, 1064926. [Google Scholar] [CrossRef]
- Melo, G.A.A.; Aguiar, L.L.; Silva, R.A.; Pereira, F.G.F.; da Silva, F.L.B.; Caetano, J. Effects of acupuncture in patients with chronic kidney disease: A systematic review. Rev. Bras. Enferm. 2020, 73, e20180784. [Google Scholar] [CrossRef]
- Xu, M.; Yang, C.; Nian, T.; Tian, C.; Zhou, L.; Wu, Y.; Li, Y.; Deng, X.; Li, X.; Yang, K. Adverse effects associated with acupuncture therapies: An evidence mapping from 535 systematic reviews. Chin. Med. 2023, 18, 1–10. [Google Scholar] [CrossRef]
- Zheng, H.; Li, J.; Li, Y.; Zhao, L.; Wu, X.; Chen, J.; Li, X.; Huang, Y.; Chang, X.; Liu, M.; et al. Acupuncture for patients with mild hypertension: A randomized controlled trial. J. Clin. Hypertens. 2019, 21, 412–420. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.-H.; Shih, C.-H.; Kaphle, K.; Wu, L.-S.; Tseng, W.-Y.; Chiu, J.-H.; Lee, T.-C.; Wu, Y.-L. Acupuncture Effects on Cardiac Functions Measured by Cardiac Magnetic Resonance Imaging in a Feline Model. Evid.-Based Complement. Altern. Med. 2010, 7, 169–176. [Google Scholar] [CrossRef] [PubMed]
- Ince, L.P. Cognitive Therapy and the Emotional Disorders. Am. J. Psychother. 1977, 31, 633–634. [Google Scholar] [CrossRef]
- Ehde, D.M.; Dillworth, T.M.; Turner, J.A. Cognitive-behavioral therapy for individuals with chronic pain: Efficacy, innovations, and directions for research. Am. Psychol. 2014, 69, 153–166. [Google Scholar] [CrossRef]
- Zegarow, P.; Manczak, M.; Rysz, J.; Olszewski, R. The influence of cognitive-behavioral therapy on depression in dialysis patients—Meta-analysis. Arch. Med. Sci. 2020, 16, 1271–1278. [Google Scholar] [CrossRef]
- Valsaraj, B.P.; Bhat, S.M.; Prabhu, R.; Kamath, A. Follow-Up Study on the Effect of Cognitive Behaviour Therapy on Haemodialysis Adherence: A randomised controlled trial. Sultan Qaboos Univ. Med. J. 2021, 21, e58–e65. [Google Scholar] [CrossRef]
- Jakubowski, K.P.; Jhamb, M.; Yabes, J.; Gujral, S.; Oberlin, L.E.; Bender, F.H.; Steel, J.L. Technology-assisted cognitive-behavioral therapy intervention for end-stage renal disease. Transl. Behav. Med. 2020, 10, 657–663. [Google Scholar] [CrossRef]
- Sohn, B.K.; Oh, Y.K.; Choi, J.-S.; Song, J.; Lim, A.; Lee, J.P.; An, J.N.; Choi, H.-J.; Hwang, J.Y.; Jung, H.-Y.; et al. Effectiveness of group cognitive behavioral therapy with mindfulness in end-stage renal disease hemodialysis patients. Kidney Res. Clin. Pr. 2018, 37, 77–84. [Google Scholar] [CrossRef] [PubMed]
- Cukor, D.; Halen, N.V.; Asher, D.R.; Coplan, J.D.; Weedon, J.; Wyka, K.E.; Saggi, S.J.; Kimmel, P.L. Psychosocial Intervention Improves Depression, Quality of Life, and Fluid Adherence in Hemodialysis. J. Am. Soc. Nephrol. 2014, 25, 196–206. [Google Scholar] [CrossRef] [PubMed]
- NCT01159197. Cognitive-Behavioral Therapy for Sleep Disturbance in Patients Undergoing Hemodialysis. Available online: https://clinicaltrials.gov/show/NCT01159197 (accessed on 18 July 2023).
- Principles and Practice of Stress Management, 3rd ed.; The Guilford Press: New York, NY, USA, 2007; Available online: https://psycnet.apa.org/record/2007-14796-000 (accessed on 1 May 2023).
- Whitehouse, W.; Orne, E.; Orne, M. Relaxation Techniques. In Encyclopedia of Stress, 2nd ed.; Elsevier: Amsterdam, The Netherlands, 2007; pp. 345–350. [Google Scholar] [CrossRef]
- Gorji, M.A.H.; Ardebil, M.D.; Mahdavi, A.; Gorji, A.M.H.; Yazdani, J. Implementing benson′s relaxation training in hemodialysis patients: Changes in perceived stress, anxiety, and depression. N. Am. J. Med. Sci. 2013, 5, 536–540. [Google Scholar] [CrossRef] [PubMed]
- Syam, N.M.; Desoky, G.M.; Ahmed, H.; Eldesoky, M. Effects of Progressive Muscle Relaxation Technique on Severity of Restless Legs Syndrome Among Patients on Maintenance Hemodialysis. Orig. Artic. Egypt. J. Health Care 2022, 13, 102–120. [Google Scholar] [CrossRef]
- Beizaee, Y.; Rejeh, N.; Heravi-Karimooi, M.; Tadrisi, S.D.; Griffiths, P.; Vaismoradi, M. The effect of guided imagery on anxiety, depression and vital signs in patients on hemodialysis. Complement. Ther. Clin. Pr. 2018, 33, 184–190. [Google Scholar] [CrossRef]
- Blouchi, T.; Kianmehr, M.; Tavakolizade, J.; Basiri-Moghadam, M.; Biabani, F. Effect of Muscle Relaxation on Hemodialysis Patients’ Pain. Intern. Med. Today 2015, 21, 75–80. [Google Scholar] [CrossRef][Green Version]
- Abu Maloh, H.I.A.; Chong, S.C.; Ismail, S.I.F.; Soh, K.G.; Abu Maloh, D.I.; Al Yateem, N.; AbuRuz, M.E. The Effectiveness of Benson’s Relaxation Technique on Pain and Perceived Stress Among Patients Undergoing Hemodialysis: A Double-Blind, Cluster-Randomized, Active Control Clinical Trial. Clin. Nurs. Res. 2023, 32, 288–297. [Google Scholar] [CrossRef]
- Rambod, M.; Sharif, F.; Pourali-Mohammadi, N.; Pasyar, N.; Rafii, F. Evaluation of the effect of Benson’s relaxation technique on pain and quality of life of haemodialysis patients: A randomized controlled trial. Int. J. Nurs. Stud. 2014, 51, 964–973. [Google Scholar] [CrossRef] [PubMed]
- Heidarigorji, A.; Davanloo, A.A. The efficacy of relaxation training on stress, anxiety, and pain perception in hemodialysis patients. Indian J. Nephrol. 2014, 24, 356–361. [Google Scholar] [CrossRef] [PubMed]
- Serin, E.K.; Ovayolu, N.; Ovayolu, Ö. The Effect of Progressive Relaxation Exercises on Pain, Fatigue, and Quality of Life in Dialysis Patients. Holist. Nurs. Pr. 2020, 34, 121–128. [Google Scholar] [CrossRef]
- Al Hasbi, H.; Chayati, N.; Makiyah, S.N.N. Progressive muscle relaxation to reduces chronic pain in hemodialysis patient. Medisains 2020, 17, 62. [Google Scholar] [CrossRef]
- Riva, G.; Wiederhold, B.K.; Mantovani, F. Neuroscience of Virtual Reality: From Virtual Exposure to Embodied Medicine. Cyberpsychol. Behav. Soc. Netw. 2019, 22, 82–96. [Google Scholar] [CrossRef]
- Hoffman, H.G.; Chambers, G.T.; Meyer, W.J.; Arceneaux, L.L.; Russell, W.J.; Seibel, E.J.; Richards, T.L.; Sharar, S.R.; Patterson, D.R. Virtual Reality as an Adjunctive Non-pharmacologic Analgesic for Acute Burn Pain During Medical Procedures. Ann. Behav. Med. 2011, 41, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Maddox, T.; Fitzpatrick, T. Virtual Reality in Chronic Kidney Disease Education and Training. Nephrol. Nurs. J. 2022, 49, 329–381. [Google Scholar] [CrossRef]
- Burrows, B.; Wilund, K.; Hernandez, R. Fully immersive virtual reality for hemodialysis patients: Is it safe? Blood Purif. 2020, 49, 250–251. [Google Scholar]
- Maynard, L.G.; de Menezes, D.L.; Lião, N.S.; de Jesus, E.M.; Andrade, N.L.S.; Santos, J.C.D.; Júnior, W.M.d.S.; Bastos, K.d.A.; Filho, J.A.S.B. Effects of Exercise Training Combined with Virtual Reality in Functionality and Health-Related Quality of Life of Patients on Hemodialysis. Games Health J. 2019, 8, 339–348. [Google Scholar] [CrossRef]
- Hernandez, R.; Burrows, B.; Browning, M.H.; Solai, K.; Fast, D.; Litbarg, N.O.; Wilund, K.R.; Moskowitz, J.T. Mindfulness-based Virtual Reality Intervention in Hemodialysis Patients: A Pilot Study on End-user Perceptions and Safety. Kidney360 2021, 2, 435–444. [Google Scholar] [CrossRef]
- Meléndez-Oliva, E.; Sánchez-Romero, E.A.; Segura-Ortí, E.; Gil-Gómez, J.-A.; Soto-Goñi, X.A.; Poveda-Pagán, E.J. Effect of a Virtual Reality Exercise on Patients Undergoing Haemodialysis: A Randomised Controlled Clinical Trial Research Protocol. Int. J. Environ. Res. Public Health 2023, 20, 4116. [Google Scholar] [CrossRef] [PubMed]
- Omonaiye, O.; Smyth, W.; Nagle, C. Impact of virtual reality interventions on haemodialysis patients: A scoping review. J. Ren. Care 2021, 47, 193–207. [Google Scholar] [CrossRef]
- Vance, C.G.T.; Dailey, D.L.; Chimenti, R.L.; Van Gorp, B.J.; Crofford, L.J.; Sluka, K.A. Using TENS for Pain Control: Update on the State of the Evidence. Medicina 2022, 58, 1332. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.Y.; Chen, H.M.; Su, Y.C.; Chin, C.C. The effect of transcutaneous electrical nerve stimulation on increasing salivary flow rate in hemodialysis patients. Oral Dis. 2019, 25, 133–141. [Google Scholar] [CrossRef] [PubMed]
- Linnemann, A.; Kappert, M.B.; Fischer, S.; Doerr, J.M.; Strahler, J.; Nater, U.M. The effects of music listening on pain and stress in the daily life of patients with fibromyalgia syndrome. Front. Hum. Neurosci. 2015, 9, 434. [Google Scholar] [CrossRef] [PubMed]
- Thakare, A.; Jallapally, A.; Agrawal, A.; Salkar, P. Music Therapy and Its Role in Pain Control. In Music in Health and Diseases; IntechOpen: Rijeka, Croatia, 2022. [Google Scholar] [CrossRef]
- Ginsberg, J.P.; Raghunathan, K.; Bassi, G.; Ulloa, L. Review of Perioperative Music Medicine: Mechanisms of Pain and Stress Reduction Around Surgery. Front. Med. 2022, 9, 821022. [Google Scholar] [CrossRef]
- Colebaugh, C.A.; Wilson, J.M.; Flowers, K.M.; Overstreet, D.; Wang, D.; Edwards, R.R.; Chai, P.R.; Schreiber, K.L. The Impact of Varied Music Applications on Pain Perception and Situational Pain Catastrophizing. J. Pain 2023, 24, 1181–1192. [Google Scholar] [CrossRef] [PubMed]
- Chai, P.R.; Gale, J.Y.; Patton, M.E.; Schwartz, E.; Jambaulikar, G.D.; Taylor, S.W.; Edwards, R.R.; Boyer, E.W.; Schreiber, K.L. The Impact of Music on Nociceptive Processing. Pain Med. 2020, 21, 3047–3054. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Jeong, H. Effects of Patient-Selected Music Listening on the Pain and Anxiety of Patients Undergoing Hemodialysis: A Randomized Controlled Trial. Healthcare 2021, 9, 1437. [Google Scholar] [CrossRef]
- Hagemann, P.M.S.; Martin, L.C.; Neme, C.M.B. The effect of music therapy on hemodialysis patients’ quality of life and depression symptoms. Braz. J. Nephrol. 2019, 41, 74–82. [Google Scholar] [CrossRef]
- Farrar, A.J.; Farrar, F.C. Clinical Aromatherapy. Nurs. Clin. N. Am. 2020, 55, 489–504. [Google Scholar] [CrossRef]
- Jankowska, M.; Rogalska, J.; Wyszkowska, J.; Stankiewicz, M. Molecular Targets for Components of Essential Oils in the Insect Nervous System—A Review. Molecules 2018, 23, 34. [Google Scholar] [CrossRef] [PubMed]
- Fung, T.K.H.; Lau, B.W.M.; Ngai, S.P.C.; Tsang, H.W.H. Therapeutic Effect and Mechanisms of Essential Oils in Mood Disorders: Interaction between the Nervous and Respiratory Systems. Int. J. Mol. Sci. 2021, 22, 4844. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, P.; Sebghatollahi, Z.; Kamal, M.; Dhyani, A.; Shrivastava, A.; Singh, K.K.; Sinha, M.; Mahato, N.; Mishra, A.K.; Baek, K.-H. Citrus Essential Oils in Aromatherapy: Therapeutic Effects and Mechanisms. Antioxidants 2022, 11, 2374. [Google Scholar] [CrossRef] [PubMed]
- Reyes, M.C.G.M.; Ribay, K.G.L.; Paragas, E.D. Effects of sweet orange aromatherapy on pain and anxiety during needle insertion among patients undergoing hemodialysis: A quasi-experimental study. Nurs. Forum 2020, 55, 425–432. [Google Scholar] [CrossRef]
- Mo, P.K.H.; Wong, E.L.Y.; Yeung, N.C.Y.; Wong, S.Y.S.; Chung, R.Y.; Tong, A.C.Y.; Ko, C.C.Y.; Li, J.; Yeoh, E.-K. Differential associations among social support, health promoting behaviors, health-related quality of life and subjective well-being in older and younger persons: A structural equation modelling approach. Health Qual. Life Outcomes 2022, 20, 38. [Google Scholar] [CrossRef]
- Cheng, J.; Zhang, H.; Bao, H.; Hong, H. Music-based interventions for pain relief in patients undergoing hemodialysis: A PRISMA-compliant systematic review and meta-analysis. Medicine 2021, 100, e24102. [Google Scholar] [CrossRef]
- Yıldız, A.; Şahan, S. Effect of aromatherapy on the pain of arteriovenous fistula puncture in patients on hemodialysis: A systematic review. J. Health Res. 2021, 36, 1187–1197. [Google Scholar] [CrossRef]
- Nielsen, A.; Dusek, J.A.; Taylor-Swanson, L.; Tick, H. Acupuncture Therapy as an Evidence-Based Nonpharmacologic Strategy for Comprehensive Acute Pain Care: The Academic Consortium Pain Task Force White Paper Update. Pain Med. 2022, 23, 1582–1612. [Google Scholar] [CrossRef] [PubMed]
- Dusek, J.A.; Kallenberg, G.A.; Hughes, R.M.D.; Storrow, A.B.; Coyne, C.J.; Vago, D.R.; Nielsen, A.; Karasz, A.; Kim, R.S.; Surdam, J.; et al. Acupuncture in the emergency department for pain management: A BraveNet multi-center feasibility study. Medicine 2022, 101, e28961. [Google Scholar] [CrossRef]
- Nees, T.A.; Riewe, E.; Waschke, D.; Schiltenwolf, M.; Neubauer, E.; Wang, H. Multidisciplinary Pain Management of Chronic Back Pain: Helpful Treatments from the Patients’ Perspective. J. Clin. Med. 2020, 9, 145. [Google Scholar] [CrossRef] [PubMed]
- Driscoll, M.A.; Edwards, R.R.; Becker, W.C.; Kaptchuk, T.J.; Kerns, R.D. Psychological Interventions for the Treatment of Chronic Pain in Adults. Psychol. Sci. Public Interest 2021, 22, 52–95. [Google Scholar] [CrossRef] [PubMed]
- Arcoraci, V.; Barbieri, M.A.; Rottura, M.; Nobili, A.; Natoli, G.; Argano, C.; Squadrito, G.; Squadrito, F.; Corrao, S.; on behalf of the REPOSI Investigators. Kidney Disease Management in the Hospital Setting: A Focus on Inappropriate Drug Prescriptions in Older Patients. Front. Pharmacol. 2021, 12, 749711. [Google Scholar] [CrossRef] [PubMed]
- Kesik, G.; Ersoy, N.A. The effect of nonpharmacologic interventions for muscle cramps and restless-leg syndrome in hemodialysis patients: A meta-analysis of randomized controlled trials. Ther. Apher. Dial. 2023, 27, 636–654. [Google Scholar] [CrossRef]
- Hargrove, N.; El Tobgy, N.; Zhou, O.; Pinder, M.; Plant, B.; Askin, N.; Bieber, L.; Collister, D.; Whitlock, R.; Tangri, N.; et al. Effect of Aerobic Exercise on Dialysis-Related Symptoms in Individuals Undergoing Maintenance Hemodialysis. Clin. J. Am. Soc. Nephrol. 2021, 16, 560–574. [Google Scholar] [CrossRef]
- Ghanbari, A.; Shahrbabaki, P.M.; Dehghan, M.; Mardanparvar, H.; Abadi, E.K.D.; Emami, A.; Sarikhani-Khorrami, E. Comparison of the Effect of Reflexology and Swedish Massage on Restless Legs Syndrome and Sleep Quality in Patients Undergoing Hemodialysis: A Randomized Clinical Trial. Int. J. Ther. Massage Bodyw. 2022, 15, 1–13. [Google Scholar] [CrossRef]
- Martin, J.L.; Saredakis, D.; Hutchinson, A.D.; Crawford, G.B.; Loetscher, T. Virtual Reality in Palliative Care: A Systematic Review. Healthcare 2022, 10, 1222. [Google Scholar] [CrossRef]
- Hsieh, C.-H.; Li, D. Understanding how virtual reality forest experience promote physiological and psychological health for patients undergoing hemodialysis. Front. Psychiatry 2022, 13, 1007396. [Google Scholar] [CrossRef]
- Gerogianni, G. Factors Affecting Pain in Hemodialysis and Non-pharmacological Management. Cureus 2023, 15, e35448. [Google Scholar] [CrossRef]
- Jira, L.; Weyessa, N.; Mulatu, S.; Alemayehu, A. Knowledge and Attitude Towards Non-Pharmacological Pain Management and Associated Factors Among Nurses Working in Benishangul Gumuz Regional State Hospitals in Western Ethiopia, 2018. J. Pain Res. 2020, 13, 2917–2927. [Google Scholar] [CrossRef]
- Bello, A.K.; Okpechi, I.G.; Osman, M.A.; Cho, Y.; Htay, H.; Jha, V.; Wainstein, M.; Johnson, D.W. Epidemiology of haemodialysis outcomes. Nat. Rev. Nephrol. 2022, 18, 378–395. [Google Scholar] [CrossRef] [PubMed]
- Andronis, L.; Kinghorn, P.; Qiao, S.; Whitehurst, D.G.T.; Durrell, S.; McLeod, H. Cost-Effectiveness of Non-Invasive and Non-Pharmacological Interventions for Low Back Pain: A Systematic Literature Review. Appl. Health Econ. Health Policy 2016, 15, 173–201. [Google Scholar] [CrossRef] [PubMed]
| Intervention | Authors; Year | Study Type | Participants | Perceived Benefits |
|---|---|---|---|---|
| Acupuncture | Kim et al. [16]; 2016 | Observational pilot | 24 hemodialysis patients | Reduction in pain related to hemodialysis |
| Correia et al. [17]; 2022 | Randomized control trial | 67 male and female adult patients who are experiencing decreased functional capacity associated with hemodialysis | Improvements in functional capacity and muscle strength | |
| Bullen et al. [18]; 2018 | Pre- and postintervention surveys | 101 patients who have end-stage renal disease | Improvement in the overall health-related quality of life | |
| Correia et al. [19]; 2023 | Randomized, controlled patient–assessor trial | 67 cases receiving maintenance HD | Enhancement of the health-related quality of life in individuals | |
| Çevik et al. [22]; 2020 | Randomized controlled trial | 50 patients divided into two groups of 25, each consisting of patients on hemodialysis [1] | Improved overall quality of life. Acupressure significantly reduces extremity pain according to the VAS pain score | |
| Melo et al. [25]; 2020 | Systematic review | Nine selected studies that examined patients with chronic kidney disease | Reduction in reported fatigue; reduced sleep problems and HRQOL in patients with CKD | |
| Cognitive behavioral therapy (CBT) | Zegarow et al. [31]; 2020 | Meta-analysis | 226 patients with hemodialysis | Reduced intensity of depressive symptoms |
| Valsaraj et al. [32]; 2021 | Randomized controlled trial | 67 patients with chronic kidney disease | Improved therapeutic adherence, as well as physiological and clinical parameters among CKD patients undergoing hemodialysis | |
| Jakbowski et al. [33]; 2020 | Pilot study | 10 ESRD undergoing hemodialysis was feasible and well accepted | No significant changes in depression, fatigue, or pain were observed | |
| Sohn et al. [34]; 2018 | Pilot study | Seven ESRD patients undergoing hemodialysis and experiencing depression | Significant improvements in quality of life, mood, anxiety, and perceived stress following the 12-week CBT program. In addition, serum creatinine levels significantly improved | |
| Cukor et al. [35]; 2014 | Randomized reciprocal trial | 59 patients undergoing dialysis treatments for three months | Reductions in depression scores, greater improvements in quality of life and interdialytic weight gain | |
| Relaxation techniques | Syam et al. [40]; 2022 | A quasi-experimental trial | 60 patients patients on maintenance hemodialysis | Reduced severity of restless leg syndrome and improvements observed in sleep patterns, physical activities, and social activities |
| Beizaee et al. [41]; 2018 | Clinical trial organized under randomized control | 80 patients undergoing hemodialysis | Reduced values of anxiety and depression | |
| Blouchi et al. [42]; 2015 | Random division into control and experimental groups | Ninety hemodialysis patients taking Benson muscle relaxation twice a day | A decrease in pain intensity in the intervention group compared to the control, suggesting that muscle relaxation can effectively reduce pain in hemodialysis patients | |
| Heidari et al. [45]; 2014 | Randomized controlled trial | 80 patients undergoing hemodialysis | Lowered anxiety and pain experienced in hemodialysis patients | |
| Kaplan et al. [46]; 2014 | Randomized controlled experimental investigation | 48 intervention and 48 control patients undergoing hemodialysis | Reduced fatigue score and average pain score and improved life quality | |
| Virtual reality | Maynard et al. [52]; 2019 | Randomized controlled trial | 20 intervention and 20 control patients undergoing hemodialysis | Improved functional capacity and some quality-of-life domains of hemodialysis patients |
| Hernandez et al. [53]; 2021 | Pilot study | 20 patients undergoing hemodialysis | Decrease in symptoms such as fatigue, nausea, lightheadedness, and headaches that often manifest during hemodialysis sessions | |
| Romero et al. [54]; 2023 | Randomized controlled trial | 40 intervention patients and 40 control patients | Improved adherence to exercise in hemodialysis patients leads to better outcomes, such as improved inflammatory state, functional capacity, psychological state, and cardiovascular health | |
| Transcutaneous electrical nerve stimulation | Yang et al. [57]; 2019 | Randomized controlled trial | 80 patients undergoing hemodialysis | Reduced pain intensity in hemodialysis patients with access-related pain and improved salivary flow rate |
| Music | Kim et al. [63]; 2021 | Randomized controlled trial | 32 intervention patients and 33 control patients | Reduced pain and anxiety levels of hemodialysis patients during vascular access operations |
| Hagemann et al. [64]; 2019 | Interventional study | 23 patients undergoing hemodialysis | Significant decrease in depression symptoms and improved quality of life across various dimensions, including functional capacity, pain, general health, vitality, mental health, and overall well-being | |
| Aromatherapy | Reyes et al. [69]; 2020 | A quasi-experimental | 50 patients undergoing hemodialysis | Sweet orange aromatherapy was effective in reducing pain and anxiety in hemodialysis patients |
| Yıldız et al. [72]; 2022 | Systematic review | Seven studies included in the review | Decreased pain during the fistula needle intervention |
| No. | Non-Pharmacological Intervention | Reported Side Effects | Supporting Reference: 1st Author Name and Year |
|---|---|---|---|
| 1 | Acupuncture | Usually safe, but it can have mild side effects like bruises, bleeding, or pain where the needles were put in. Rarely, more major side effects like infections or organ damage can happen if you do not follow the right hygiene and approach. | |
| 2 | Cognitive behavioral treatment | It is safe and well tolerated by most people and has few bad effects. Some people may feel temporary pain or mental distress during treatment meetings as they face and deal with problems linked to their pain. | |
| 3 | Relaxation techniques | These are generally safe and have no major side effects. But, some people may find it hard to fully relax or get frustrated if they do not reach the level of relaxation they aim for. | |
| 4 | Virtual reality | It is usually safe to use, but patients with motion sickness may feel dizzy or sick because of the way the virtual world moves. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kassim, M.A.K.; Pantazi, A.C.; Nori, W.; Tuta, L.A.; Balasa, A.L.; Mihai, C.M.; Mihai, L.; Frecus, C.E.; Lupu, V.V.; Lupu, A.; et al. Non-Pharmacological Interventions for Pain Management in Hemodialysis: A Narrative Review. J. Clin. Med. 2023, 12, 5390. https://doi.org/10.3390/jcm12165390
Kassim MAK, Pantazi AC, Nori W, Tuta LA, Balasa AL, Mihai CM, Mihai L, Frecus CE, Lupu VV, Lupu A, et al. Non-Pharmacological Interventions for Pain Management in Hemodialysis: A Narrative Review. Journal of Clinical Medicine. 2023; 12(16):5390. https://doi.org/10.3390/jcm12165390
Chicago/Turabian StyleKassim, Mustafa Ali Kassim, Alexandru Cosmin Pantazi, Wassan Nori, Liliana Ana Tuta, Adriana Luminita Balasa, Cristina Maria Mihai, Larisia Mihai, Corina Elena Frecus, Vasile Valeriu Lupu, Ancuta Lupu, and et al. 2023. "Non-Pharmacological Interventions for Pain Management in Hemodialysis: A Narrative Review" Journal of Clinical Medicine 12, no. 16: 5390. https://doi.org/10.3390/jcm12165390
APA StyleKassim, M. A. K., Pantazi, A. C., Nori, W., Tuta, L. A., Balasa, A. L., Mihai, C. M., Mihai, L., Frecus, C. E., Lupu, V. V., Lupu, A., Andrusca, A., Iorga, A. M., Litrin, R. M., Ion, I., Ciciu, E., Chirila, S. I., & Chisnoiu, T. (2023). Non-Pharmacological Interventions for Pain Management in Hemodialysis: A Narrative Review. Journal of Clinical Medicine, 12(16), 5390. https://doi.org/10.3390/jcm12165390









