Association of TNF-α (-308G/A) Gene Polymorphism with Changes in Circulating TNF-α Levels in Response to CPAP Treatment in Adults with Coronary Artery Disease and Obstructive Sleep Apnea
Abstract
1. Introduction
2. Materials and Methods
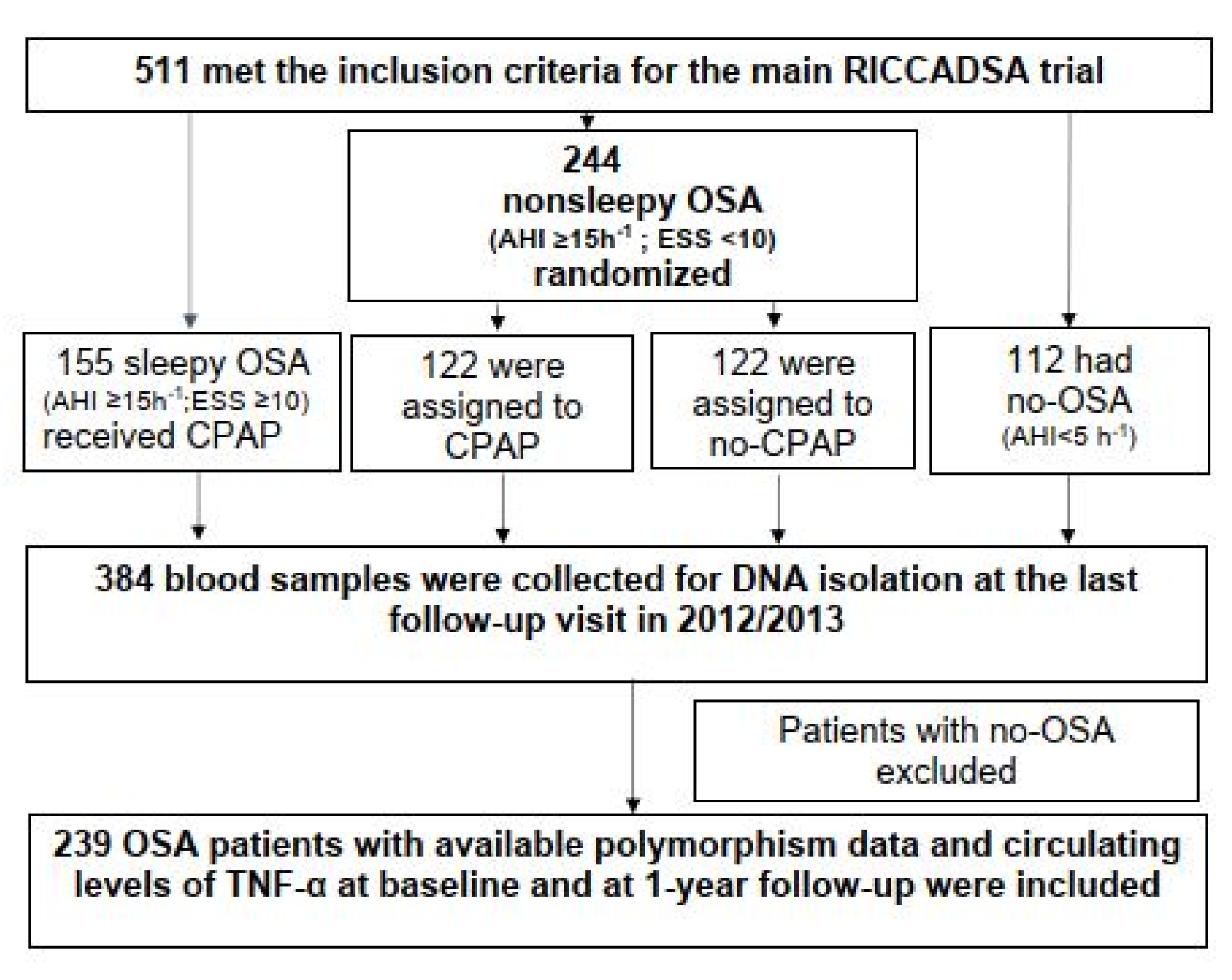
2.1. Study Participants
2.2. Study Oversight
2.3. Sleep Studies
2.4. Epworth Sleepiness Scale
2.5. Comorbidities
2.6. TNF-α Circulating Concentration
2.7. TNF-α Promotor -308G/A (Rs1800629) SNA Genotyping
2.8. Statistical Analysis
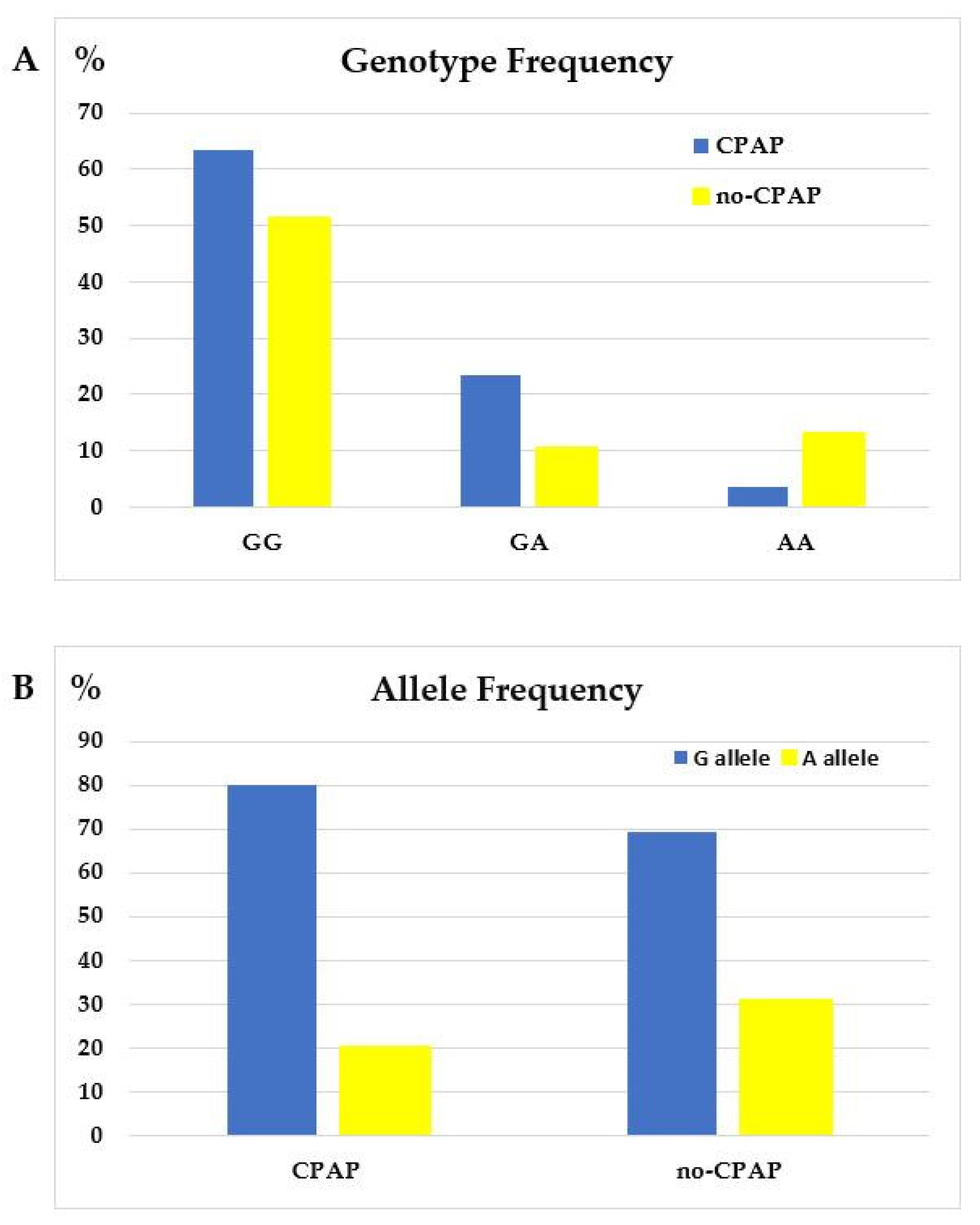
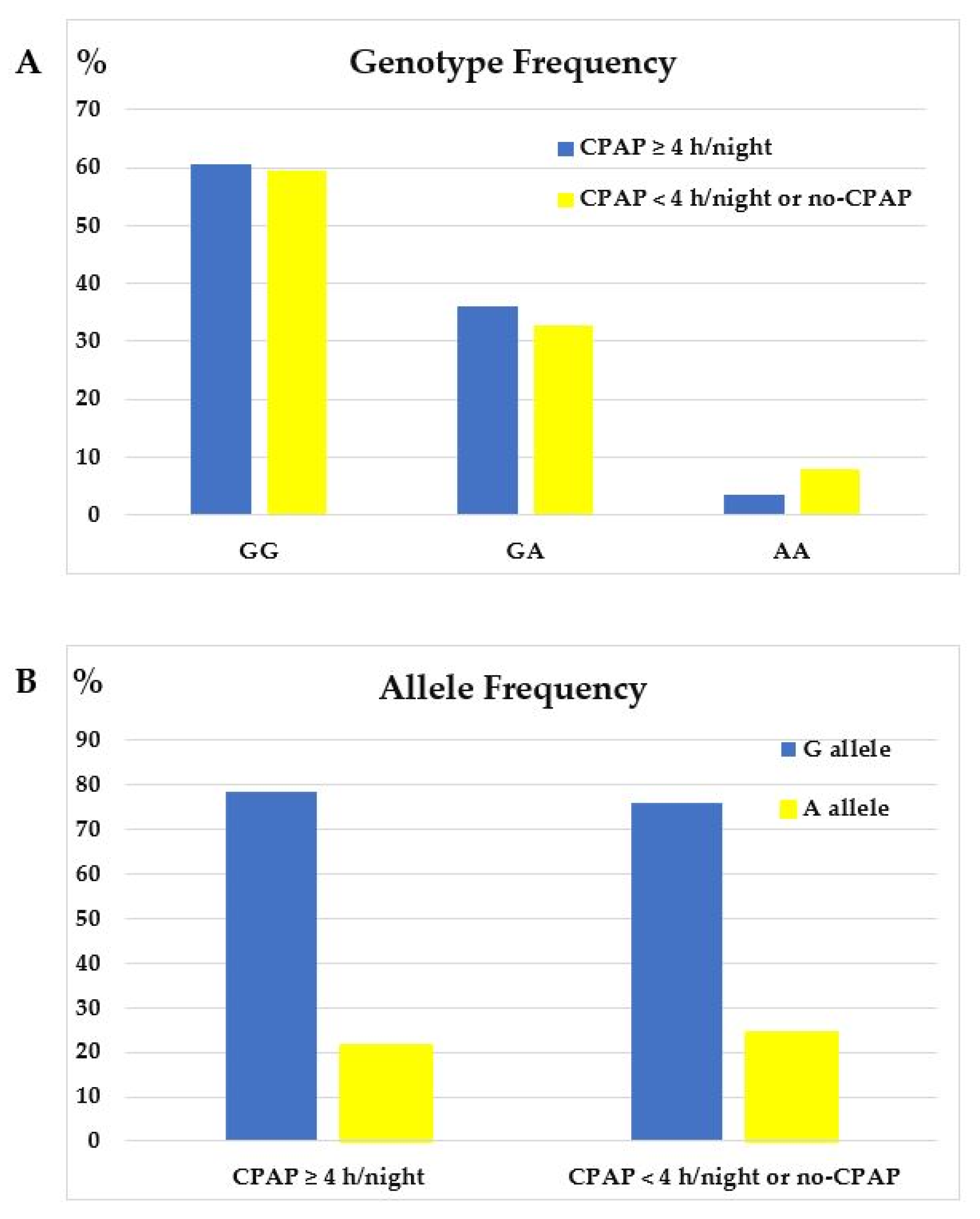
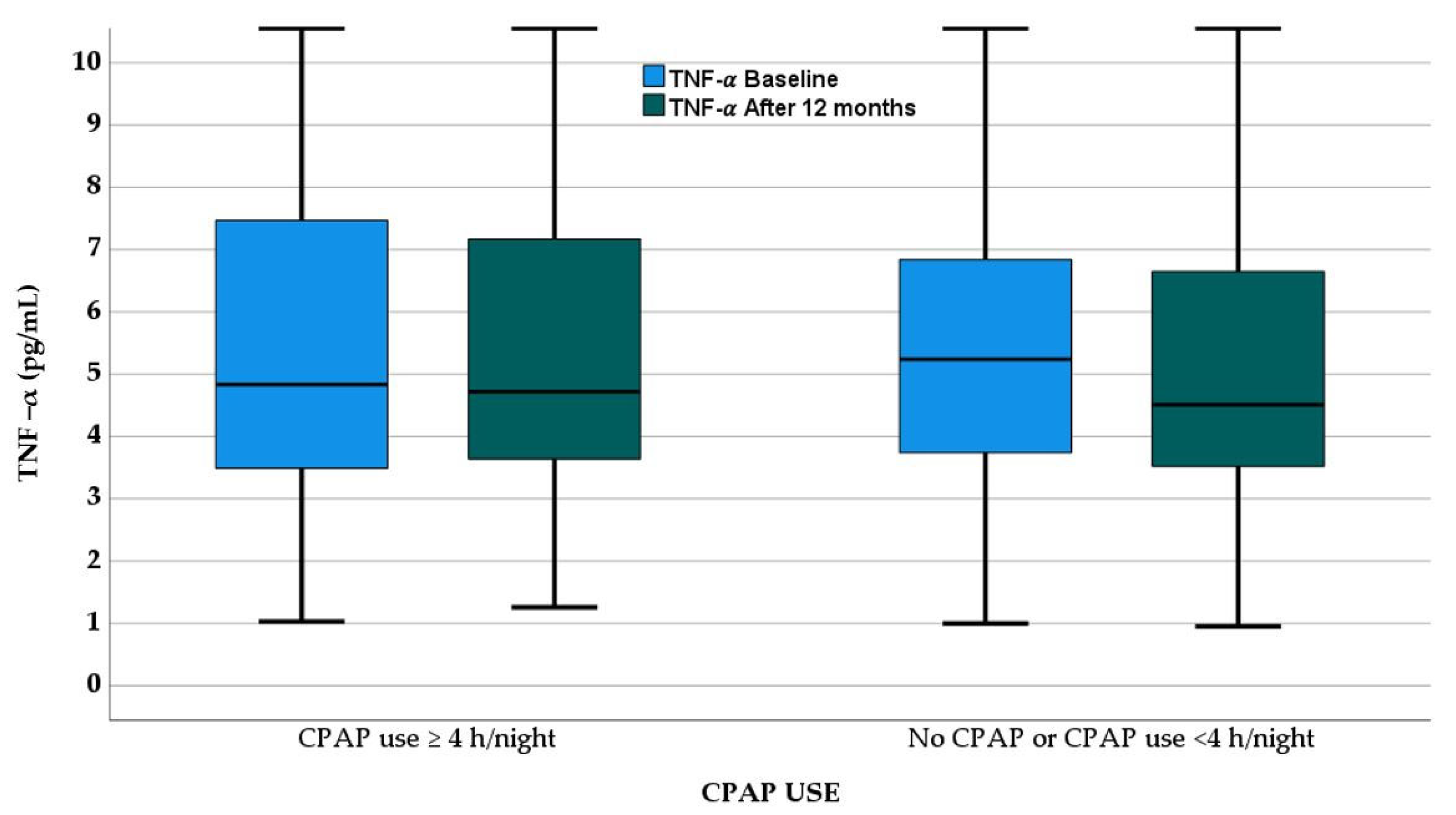
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Redline, S.; Azarbarzin, A.; Peker, Y. Obstructive sleep apnoea heterogeneity and cardiovascular disease. Nat. Rev. Cardiol. 2023, 20, 560–573. [Google Scholar] [CrossRef] [PubMed]
- Musunuru, K.; Kathiresan, S. Genetics of Common, Complex Coronary Artery Disease. Cell 2019, 177, 132–145. [Google Scholar] [CrossRef]
- Khera, A.V.; Kathiresan, S. Genetics of coronary artery disease: Discovery, biology and clinical translation. Nat. Rev. Genet. 2017, 18, 331–344. [Google Scholar] [CrossRef]
- Young, T.; Palta, M.; Dempsey, J.; Peppard, P.E.; Nieto, F.J.; Hla, K.M. Burden of sleep apnea: Rationale, design, and major findings of the Wisconsin Sleep Cohort study. WMJ Off. Publ. State Med. Soc. Wis. 2009, 108, 246–249. [Google Scholar]
- Peker, Y.; Franklin, K.; Hedner, J. Coronary artery disease and sleep apnea. In Principles and Practice of Sleep Medicine, 7th ed.; Roth, K., Goldtstein, Dement, W.T., Eds.; Elsevier Inc.: Philadelphia, PA, USA, 2022; pp. 1453–1461. ISBN 978-0-323-66189-8. [Google Scholar]
- Turgut Çelen, Y.; Peker, Y. Cardiovascular consequences of sleep apnea: II-Cardiovascular mechanisms. Anatol. J. Cardiol. 2010, 10, 168–175. [Google Scholar] [CrossRef] [PubMed]
- Hansson, G.K. Inflammation, atherosclerosis, and coronary artery disease. N. Engl. J. Med. 2005, 352, 1685–1695. [Google Scholar] [CrossRef] [PubMed]
- Cesari, M.; Penninx, B.W.; Newman, A.B.; Kritchevsky, S.B.; Nicklas, B.J.; Sutton-Tyrrell, K.; Pahor, M. Inflammatory markers and onset of cardiovascular events: Results from the Health ABC study. Circulation 2003, 108, 2317–2322. [Google Scholar] [CrossRef]
- He, L.P.; Tang, X.Y.; Ling, W.H.; Chen, W.Q.; Chen, Y.M. Early C-reactive protein in the prediction of long-term outcomes after acute coronary syndromes: A meta-analysis of longitudinal studies. Heart 2010, 96, 339–346. [Google Scholar] [CrossRef]
- Patt, B.T.; Jarjoura, D.; Haddad, D.N.; Sen, C.K.; Roy, S.; Flavahan, N.A.; Khayat, R.N. Endothelial dysfunction in the microcirculation of patients with obstructive sleep apnea. Am. J. Respir. Crit. Care Med. 2010, 182, 1540–1545. [Google Scholar] [CrossRef]
- Arnardottir, E.S.; Mackiewicz, M.; Gislason, T.; Teff, K.L.; Pack, A.I. Molecular signatures of obstructive sleep apnea in adults: A review and perspective. Sleep 2009, 32, 447–470. [Google Scholar] [CrossRef]
- Gabryelska, A.; Łukasik, Z.M.; Makowska, J.S.; Białasiewicz, P. Obstructive Sleep Apnea: From Intermittent Hypoxia to Cardiovascular Complications via Blood Platelets. Front. Neurol. 2018, 9, 635. [Google Scholar] [CrossRef]
- Reid, M.B.; Lännergren, J.; Westerblad, H. Respiratory and limb muscle weakness induced by tumor necrosis factor-alpha: Involvement of muscle myofilaments. Am. J. Respir. Crit. Care Med. 2002, 166, 479–484. [Google Scholar] [CrossRef]
- Boyd, J.H.; Petrof, B.J.; Hamid, Q.; Fraser, R.; Kimoff, R.J. Upper airway muscle inflammation and denervation changes in obstructive sleep apnea. Am. J. Respir. Crit. Care Med. 2004, 170, 541–546. [Google Scholar] [CrossRef] [PubMed]
- Huang, T.; Goodman, M.; Li, X.; Sands, S.A.; Li, J.; Stampfer, M.J.; Saxena, R.; Tworoger, S.S.; Redline, S. C-reactive Protein and Risk of OSA in Four US Cohorts. Chest 2021, 159, 2439–2448. [Google Scholar] [CrossRef] [PubMed]
- Nadeem, R.; Molnar, J.; Madbouly, E.M.; Nida, M.; Aggarwal, S.; Sajid, H.; Naseem, J.; Loomba, R. Serum inflammatory markers in obstructive sleep apnea: A meta-analysis. J. Clin. Sleep Med. 2013, 9, 1003–1012. [Google Scholar] [CrossRef]
- Kheirandish-Gozal, L.; Gozal, D. Obstructive Sleep Apnea and Inflammation: Proof of Concept Based on Two Illustrative Cytokines. Int. J. Mol. Sci. 2019, 20, 459. [Google Scholar] [CrossRef]
- Ming, H.; Tian, A.; Liu, B.; Hu, Y.; Liu, C.; Chen, R.; Cheng, L. Inflammatory cytokines tumor necrosis factor-α, interleukin-8 and sleep monitoring in patients with obstructive sleep apnea syndrome. Exp. Ther. Med. 2019, 17, 1766–1770. [Google Scholar] [CrossRef]
- Mukherjee, S.; Saxena, R.; Palmer, L.J. The genetics of obstructive sleep apnoea. Respirology 2018, 23, 18–27. [Google Scholar] [CrossRef] [PubMed]
- Kent, B.D.; Ryan, S.; McNicholas, W.T. The genetics of obstructive sleep apnoea. Curr. Opin. Pulm. Med. 2010, 16, 536–542. [Google Scholar] [CrossRef]
- Popko, K.; Gorska, E.; Potapinska, O.; Wasik, M.; Stoklosa, A.; Plywaczewski, R.; Winiarska, M.; Gorecka, D.; Sliwinski, P.; Popko, M.; et al. Frequency of distribution of inflammatory cytokines IL-1, IL-6 and TNF-alpha gene polymorphism in patients with obstructive sleep apnea. J. Physiol. Pharmacol. 2008, 59 (Suppl. S6), 607–614. [Google Scholar]
- Bhushan, B.; Guleria, R.; Misra, A.; Luthra, K.; Vikram, N.K. TNF-alpha gene polymorphism and TNF-alpha levels in obese Asian Indians with obstructive sleep apnea. Respir. Med. 2009, 103, 386–392. [Google Scholar] [CrossRef]
- Bhatt, S.P.; Guleria, R.; Vikram, N.K.; Vivekanandhan, S.; Singh, Y.; Gupta, A.K. Association of inflammatory genes in obstructive sleep apnea and non alcoholic fatty liver disease in Asian Indians residing in north India. PLoS ONE 2018, 13, e0199599. [Google Scholar] [CrossRef] [PubMed]
- Riha, R.L.; Brander, P.; Vennelle, M.; Mcardle, N.; Kerr, S.M.; Anderson, N.H.; Douglas, N.J. Tumour necrosis factor-α (−308) gene polymorphism in obstructive sleep apnoea–hypopnoea syndrome. Eur. Respir. J. 2005, 26, 673–678. [Google Scholar] [CrossRef] [PubMed]
- Khalyfa, A.; Serpero, L.D.; Kheirandish-Gozal, L.; Capdevila, O.S.; Gozal, D. TNF-α gene polymorphisms and excessive daytime sleepiness in pediatric obstructive sleep apnea. J. Pediatr. 2011, 158, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Pawlik, A.; Domanski, L.; Rozanski, J.; Florczak, M.; Dabrowska-Zamojcin, E.; Dutkiewicz, G.; Gawronska-Szklarz, B. IL-2 and TNF-alpha promoter polymorphisms in patients with acute kidney graft rejection. Transplant. Proc. 2005, 37, 2041–2043. [Google Scholar] [CrossRef]
- Aoki, T.; Hirota, T.; Tamari, M.; Ichikawa, K.; Takeda, K.; Arinami, T.; Shibasaki, M.; Noguchi, E. An association between asthma and TNF-308G/A polymorphism: Meta-analysis. J. Hum. Genet. 2006, 51, 677–685. [Google Scholar] [CrossRef]
- Zang, S.; Wang, C.; Xi, B.; Li, X. Association between the tumour necrosis factor-α-308G/A polymorphism and chronic obstructive pulmonary disease: An update. Respirology 2011, 16, 107–115. [Google Scholar] [CrossRef]
- Song, D.; Cheng, D. Associations of TNFα-308G/A and TNFα-238G/A Polymorphisms with Ischemic Stroke in East Asians and Non-East Asians: A Meta-Analysis. Genet. Test Mol. Biomarkers 2017, 21, 10–16. [Google Scholar] [CrossRef]
- O’Rielly, D.D.; Roslin, N.M.; Beyene, J.; Pope, A. Rahman PTNF-alpha-308G/A polymorphism responsiveness to TNF-alpha blockade therapy in moderate to severe rheumatoid arthritis: A systematic review meta-analysis. Pharmacogenom. J. 2009, 9, 161–167. [Google Scholar] [CrossRef]
- Guarnizo-Zuccardi, P.; Lopez, Y.; Giraldo, M.; Garcia, N.; Rodriguez, L.; Ramirez, L.; Uribe, O.; Garcia, L.; Vasquez, G. Cytokine gene polymorphisms in Colombian patients with systemic lupus erythematosus. Tissue Antigens 2007, 70, 376–382. [Google Scholar] [CrossRef]
- Antonicelli, R.; Olivieri, F.; Cavallone, L.; Spazzafumo, L.; Bonaf, M.; Marchegiani, F.; Cardelli, M.; Galeazzi, R.; Giovagnetti, S.; Perna, G.P.; et al. Tumor necrosis factor-alpha gene-308G>A polymorphism is associated with ST-elevation myocardial infarction and with high plasma levels of biochemical ischemia markers. Coron. Artery Dis. 2005, 16, 489–493. [Google Scholar] [CrossRef] [PubMed]
- Hua, X.P.; Qian, J.; Cao, C.B.; Xie, J.; Zeng, X.T.; Zhang, Z.J. Association between TNF-α rs1800629 polymorphism and the risk of myocardial infarction: A meta-analysis. Genet. Mol. Res. 2016, 13, gmr.15037292. [Google Scholar] [CrossRef]
- Huang, R.; Zhao, S.R.; Li, Y.; Liu, F.; Gong, Y.; Xing, J.; Xu, Z.S. Association of tumor necrosis factor-α gene polymorphisms and coronary artery disease susceptibility: A systematic review and meta-analysis. BMC Med. Genet. 2020, 21, 29. [Google Scholar] [CrossRef]
- Behboudi, A.; Thelander, T.; Yazici, D.; Celik, Y.; Yucel-Lindberg, T.; Thunström, E.; Peker, Y. Association of TNF-α (-308G/A) Gene Polymorphism with Circulating TNF-α Levels and Excessive Daytime Sleepiness in Adults with Coronary Artery Disease and Concomitant Obstructive Sleep Apnea. J. Clin. Med. 2021, 10, 3413. [Google Scholar] [CrossRef]
- Peker, Y.; Glantz, H.; Eulenburg, C.; Wegscheider, K.; Herlitz, J.; Thunstrom, E. Effect of Positive Airway Pressure on Cardiovascular Outcomes in Coronary Artery Disease Patients with Nonsleepy Obstructive Sleep Apnea. The RICCADSA Randomized Controlled Trial. Am. J. Respir. Crit. Care Med. 2016, 194, 613–620. [Google Scholar] [CrossRef]
- American Academy of Sleep Medicine Task Force. Sleep-related breathing disorders in adults: Recommendations for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force. Sleep 1999, 22, 667–689. [Google Scholar] [CrossRef]
- Johns, M.W. A new method for measuring daytime sleepiness: The Epworth sleepiness scale. Sleep 1991, 14, 540–545. [Google Scholar] [CrossRef] [PubMed]
- World Health Organ. Obesity: Preventing and Managing the Global Epidemic. Report of a WHO Consultation; World Health Organ: Geneva, Switzerland, 2000; Volume 894, pp. i–xii.
- Thunström, E.; Glantz, H.; Fu, M.; Yucel-Lindberg, T.; Petzold, M.; Lindberg, K.; Peker, Y. Increased inflammatory activity in nonobese patients with coronary artery disease and obstructive sleep apnea. Sleep 2015, 38, 463–471. [Google Scholar] [CrossRef] [PubMed]
- Lederer, D.J.; Bell, S.C.; Branson, R.; Chalmers, J.D.; Marshall, R.; Maslove, D.M.; Ost, D.E.; Punjabi, N.M.; Schatz, M.; Smyth, A.R.; et al. Control of Confounding and Reporting of Results in Causal Inference Studies. Guidance for Authors from Editors of Respiratory, Sleep, and Critical Care Journals. Ann. Am. Thorac. Soc. 2019, 16, 22–28. [Google Scholar] [CrossRef]
- Karkucak, M.; Ursavaş, A.; Ocakoğlu, G.; Görükmez, O.; Yakut, T.; Ercan, I.; Karadağ, M. Analysis of TNF-alpha G308A and C857T Gene Polymorphisms in Turkish Patients with Obstructive Sleep Apnea Syndrome. Turk. Klin. J. Med. Sci. 2012, 32, 1368–1373. [Google Scholar] [CrossRef][Green Version]
- Huang, J.; Liao, N.; Huang, Q.P.; Xie, Z.F. Association between tumor necrosis factor-α-308G/A polymorphism and obstructive sleep apnea: A meta-analysis. Genet. Test Mol. Biomark. 2012, 16, 246–251. [Google Scholar] [CrossRef]
- Wu, Y.; Cao, C.; Wu, Y.; Zhang, C.; Zhu, C.; Ying, S.; Li, W. TNF-α-308G/A Polymorphism Contributes to Obstructive Sleep Apnea Syndrome Risk: Evidence Based on 10 Case-Control Studies. PLoS ONE 2014, 9, e106183. [Google Scholar] [CrossRef]
- Kazemi, E.; Jamialahmadi, K.; Avan, A.; Mirhafez, S.R.; Mohiti, J.; Pirhoushiaran, M.; Hosseini, N.; Mohammadi, A.; Ferns, G.A.; Pasdar, A.; et al. Association of tumor necrosis factor-α-308G/A gene polymorphism with coronary artery diseases: An evidence-based study. J. Clin. Lan. Anal. 2018, 32, e22153. [Google Scholar] [CrossRef]
- Nejati, P.; Naeimipour, S.; Salehi, A.; Shahbazi, M. Association of tumor necrosis factor-alpha gene promoter polymorphism and its mRNA expression level in coronary artery disease. Meta Gene 2018, 18, 122–126. [Google Scholar] [CrossRef]
- Yuepeng, J.; Zhao, X.; Zhao, Y.; Li, L. Gene polymorphism associated with TNF-α (G308A) IL-6 (C174G) and susceptibility to coronary atherosclerotic heart disease: A meta-analysis. Medicine 2019, 98, e13813. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Zheng, X. Tumor necrosis factor alpha is a promising circulating biomarker for the development of obstructive sleep apnea syndrome: A meta-analysis. Oncotarget 2017, 8, 27616–27626. [Google Scholar] [CrossRef] [PubMed]
- Thunström, E.; Glantz, H.; Yucel-Lindberg, T.; Lindberg, K.; Saygin, M.; Peker, Y. CPAP Does Not Reduce Inflammatory Biomarkers in Patients with Coronary Artery Disease and Nonsleepy Obstructive Sleep Apnea: A Randomized Controlled Trial. Sleep 2017, 40, zsx157. [Google Scholar] [CrossRef]
- Kroeger, K.M.; Carville, K.S.; Abraham, L.J. The-308 tumor necrosis factor-alpha promoter polymorphism effects transcription. Mol. Immunol. 1997, 34, 391–399. [Google Scholar] [CrossRef]
| OSA on CPAP n = 169 | OSA no-CPAP n = 70 | p-Value | |
|---|---|---|---|
| Age, yrs | 64.1 (59.8–69.3) | 67.4 (62.7–72.4) | 0.019 |
| Male sex, % | 86.4 | 85.7 | 0.890 |
| BMI, kg/m2 | 28.3 (25.9–31.1) | (28.7 (26.2–30.0) | 0.548 |
| Obesity, % | 32.0 | 24.3 | 0.238 |
| WHR | 0.96 (0.93–1.00) | 0.96 (0.91–0.99) | 0.153 |
| Abdominal obesity, % | 93.2 | 95.7 | 0.470 |
| Current smoking, % | 16.0 | 15.7 | 0.960 |
| ESS score | 10.0 (6.0–12.0) | 6.0 (4.0–7.0) | <0.001 |
| EDS (ESS score ≥ 10), % | 56.8 | 0.0 | <0.001 |
| AHI, events/h | 27.7 (18.7–39.2) | 22.9 (17.8–35.7) | 0.128 |
| ODI, events/h | 15.7 (9.4–24.8) | 12.6 (7.2–22.9) | 0.101 |
| Hypertension | 60.9 | 54.3 | 0.341 |
| AMI at baseline | 54.4 | 44.3 | 0.153 |
| Lung disease, % | 5.3 | 4.3 | 0.738 |
| Diabetes, % | 26.0 | 12.9 | 0.026 |
| Stroke, % | 4.8 | 10.1 | 0.121 |
| Plasma TNF-α (pg/mL) | 4.87 (3.43–6.99) | 5.15 (3.92–6.54) | 0.856 |
| CPAP ≥ 4 h/Night (Adherent) n = 86 | CPAP < 4 h/Night or no CPAP n = 153 | p-Value | |
|---|---|---|---|
| Age, yrs | 64.4 (60.1–70.6) | 65.2 (59.9–70.6) | 0.602 |
| Male sex, % | 84.9 | 86.9 | 0.660 |
| BMI, kg/m2 | 28.2 (25.7–31.1) | 28.7 (26.2–30.2) | 0.875 |
| Obesity, % | 32.6 | 28.1 | 0.470 |
| WHR | 0.96 (0.92–1.02) | 0.97 (0.93–1.01) | 0.609 |
| Abdominal obesity, % | 92.8 | 94.6 | 0.586 |
| Current smoking, % | 12.8 | 17.6 | 0.324 |
| ESS score | 10.0 (6.0–11.0) | 7.0 (4.0–10.0) | 0.007 |
| EDS (ESS score ≥ 10), % | 53.5 | 32.7 | 0.002 |
| AHI, events/h | 28.2 (18.3–40.1) | 25.3 (18.6–36.2) | 0.293 |
| ODI, events/h | 17.2 (10.1–25.7) | 14.2 (7.9–23.1) | 0.052 |
| Hypertension | 60.5 | 58.2 | 0.729 |
| AMI at baseline | 54.7 | 49.7 | 0.460 |
| Lung disease, % | 5.3 | 4.3 | 0.738 |
| Diabetes, % | 27.9 | 19.0 | 0.110 |
| Stroke, % | 5.8 | 4.6 | 0.674 |
| Plasma TNF-α (pg/mL) | 4.87 (3.48–7.53) | 5.24 (3.59–6.85) | 0.631 |
| Standardized | 95% Confidence Interval for | p-Values | |||
|---|---|---|---|---|---|
| Coefficients β | Lower Bound | Upper Bound | |||
| Entire Cohort | Genotypes * | −0.129 | −1.82 | −0.12 | 0.025 |
| Age | 0.018 | −0.05 | 0.07 | 0.762 | |
| Male sex | −0.035 | −1.91 | 1.00 | 0.540 | |
| BMI | −0.005 | −0.15 | 0.14 | 0.942 | |
| AHI | −0.035 | −0.04 | 0.02 | 0.573 | |
| ESS | −0.115 | −0.28 | 0.00 | 0.056 | |
| Diabetes | 0.017 | −1.13 | 1.53 | 0.768 | |
| CPAP use ≥4 h/night | Genotypes * | −2.979 | −6.11 | −1.21 | 0.004 |
| Age | −0.057 | −0.25 | 0.15 | 0.607 | |
| Male sex | 0.128 | −1.61 | 6.21 | 0.246 | |
| BMI | 0.029 | −0.29 | 0.38 | 0.803 | |
| AHI | −0.183 | −0.16 | 0.01 | 0.096 | |
| ESS | −0.078 | −0.46 | 0.22 | 0.481 | |
| Diabetes | 0.006 | −3.03 | 3.21 | 0.955 | |
| CPAP use <4 h/night or no-CPAP | Genotypes * | −0.019 | −0.93 | 0.73 | 0.816 |
| Age | 0.026 | −0.58 | 0.79 | 0.765 | |
| Male sex | −0.079 | −2.36 | 0.84 | 0.349 | |
| BMI | −0.078 | −0.23 | 0.09 | 0.368 | |
| AHI | 0.124 | −0.01 | 0.07 | 0.149 | |
| ESS | −0.055 | −0.19 | 0.10 | 0.507 | |
| Diabetes | −0.055 | −1.82 | 0.91 | 0.509 | |
| Standardized | 95% Confidence Interval for | p-Values | |||
|---|---|---|---|---|---|
| Coefficients β | Lower Bound | Upper Bound | |||
| Entire Cohort | TNF-α A Allele | −0.098 | −2.08 | −0.08 | 0.034 |
| Age | 0.020 | −0.04 | 0.07 | 0.676 | |
| Male sex | 0.027 | −0.88 | 1.60 | 0.568 | |
| BMI | −0.009 | −0.13 | 0.11 | 0.858 | |
| AHI | −0.060 | −0.05 | 0.10 | 0.202 | |
| CPAP h/night | 0.011 | −0.14 | 0.18 | 0.827 | |
| ESS | −0.061 | −0.19 | 0.41 | 0.208 | |
| Diabetes | −0.017 | −1.24 | 0.85 | 0.714 | |
| CPAP use ≥4 h/night | TNF-α A Allele | −0.212 | −5.66 | −1.01 | 0.005 |
| Age | −0.038 | −0.18 | 0.11 | 0.627 | |
| Male sex | 0.102 | −0.90 | 4.58 | 0.187 | |
| BMI | 0.018 | −0.21 | 0.26 | 0.823 | |
| AHI | −0.189 | −0.14 | −0.02 | 0.015 | |
| ESS | −0.061 | −0.34 | 0.15 | 0.434 | |
| Diabetes | 0.012 | −2.03 | 2.38 | 0.876 | |
| CPAP use <4 h/night or no-CPAP | TNF-α A Allele | −0.014 | −0.96 | 0.75 | 0.805 |
| Age | 0.025 | −0.04 | 0.06 | 0.670 | |
| Male sex | −0.079 | −1.87 | 0.35 | 0.180 | |
| BMI | −0.078 | −0.18 | 0.04 | 0.197 | |
| AHI | 0.123 | −0.01 | 0.06 | 0.039 | |
| ESS | −0.055 | −0.15 | 0.05 | 0.347 | |
| Diabetes | −0.055 | −1.40 | 0.49 | 0.346 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Celik, Y.; Peker, Y.; Yucel-Lindberg, T.; Thelander, T.; Behboudi, A. Association of TNF-α (-308G/A) Gene Polymorphism with Changes in Circulating TNF-α Levels in Response to CPAP Treatment in Adults with Coronary Artery Disease and Obstructive Sleep Apnea. J. Clin. Med. 2023, 12, 5325. https://doi.org/10.3390/jcm12165325
Celik Y, Peker Y, Yucel-Lindberg T, Thelander T, Behboudi A. Association of TNF-α (-308G/A) Gene Polymorphism with Changes in Circulating TNF-α Levels in Response to CPAP Treatment in Adults with Coronary Artery Disease and Obstructive Sleep Apnea. Journal of Clinical Medicine. 2023; 12(16):5325. https://doi.org/10.3390/jcm12165325
Chicago/Turabian StyleCelik, Yeliz, Yüksel Peker, Tülay Yucel-Lindberg, Tilia Thelander, and Afrouz Behboudi. 2023. "Association of TNF-α (-308G/A) Gene Polymorphism with Changes in Circulating TNF-α Levels in Response to CPAP Treatment in Adults with Coronary Artery Disease and Obstructive Sleep Apnea" Journal of Clinical Medicine 12, no. 16: 5325. https://doi.org/10.3390/jcm12165325
APA StyleCelik, Y., Peker, Y., Yucel-Lindberg, T., Thelander, T., & Behboudi, A. (2023). Association of TNF-α (-308G/A) Gene Polymorphism with Changes in Circulating TNF-α Levels in Response to CPAP Treatment in Adults with Coronary Artery Disease and Obstructive Sleep Apnea. Journal of Clinical Medicine, 12(16), 5325. https://doi.org/10.3390/jcm12165325







