Evaluation of Retinal Blood Flow in Patients with Monoclonal Gammopathy Using OCT Angiography
Abstract
1. Introduction
2. Materials and Methods
Statistical Analysis
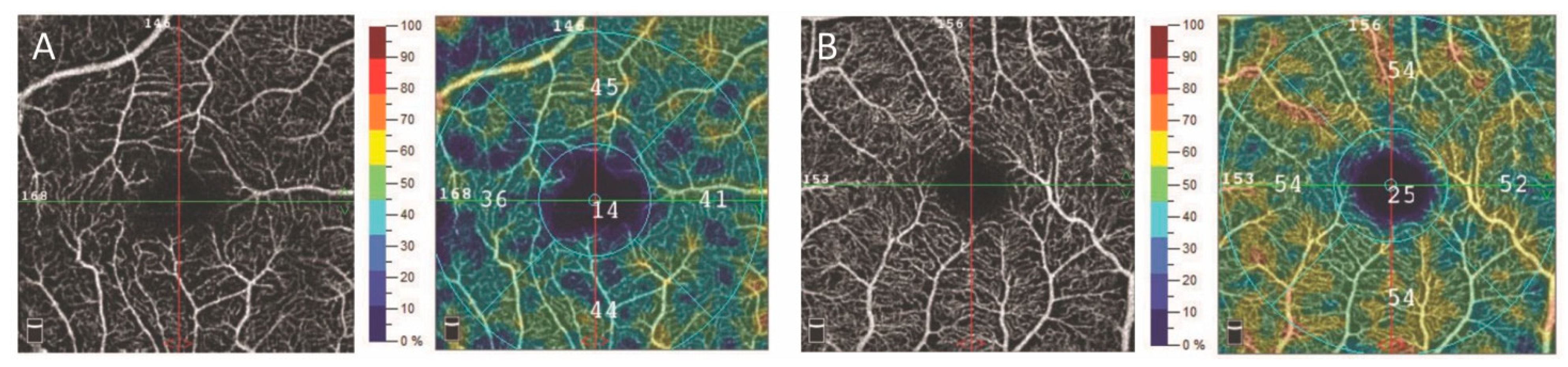
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kyle, R.A. Monoclonal gammopathy of undetermined significance. Natural history in 241 cases. Am. J. Med. 1978, 64, 814–826. [Google Scholar] [CrossRef]
- Kyle, R.A.; Therneau, T.M.; Rajkumar, S.V.; Larson, D.R.; Plevak, M.F.; Offord, J.R.; Dispenzieri, A.; Katzmann, J.A.; Melton, J.L. Prevalence of monoclonal gammopathy of undetermined significance. N. Engl. J. Med. 2006, 354, 1362–1369. [Google Scholar] [CrossRef] [PubMed]
- Rajkumar, S.V.; Dimopoulos, M.A.; Palumbo, A.; Blade, J.; Merlini, G.; Mateos, M.V.; Kumar, S.; Hillengass, J.; Kastritis, E.; Richardson, P.; et al. International Myeloma Working Group updated criteria for the diagnosis of multiple myeloma. Lancet Oncol. 2014, 15, 538–548. [Google Scholar] [CrossRef] [PubMed]
- Kyle, R.A.; Larson, D.R.; Therneau, T.M.; Dispenzieri, A.; Kumar, S.; Cerhan, J.R.; Rajkumar, S.V. Long-Term Follow-up of Monoclonal Gammopathy of Undetermined Significance. N. Engl. J. Med. 2018, 378, 241–249. [Google Scholar] [CrossRef] [PubMed]
- Omoti, A.E.; Omoti, C.E. Ophthalmic manifestations of multiple myeloma. West Afr. J. Med. 2007, 26, 265–268. [Google Scholar]
- Agorogiannis, E.I.; Kotamarthi, V. Paraproteinemia and central retinal vein occlusion. Hippokratia 2015, 19, 92. [Google Scholar]
- Kormányos, K.; Kovács, K.; Németh, O.; Tóth, G.; Sándor, G.L.; Csorba, A.; Czakó, C.N.; Langenbucher, A.; Nagy, Z.Z.; Varga, G.; et al. Ocular Signs and Ocular Comorbidities in Monoclonal Gammopathy: Analysis of 80 Subjects. J. Ophthalmol. 2021, 2021, 9982875. [Google Scholar] [CrossRef]
- Kormányos, K.; Kovács, K.; Németh, O.; Tóth, G.; Sándor, G.L.; Csorba, A.; Czakó, C.N.; Módis, L., Jr.; Langenbucher, A.; Nagy, Z.Z.; et al. Corneal Densitometry and In Vivo Confocal Microscopy in Patients with Monoclonal Gammopathy-Analysis of 130 Eyes of 65 Subjects. J. Clin. Med. 2022, 11, 1848. [Google Scholar] [CrossRef]
- Menke, M.N.; Feke, G.T.; McMeel, J.W.; Branagan, A.; Hunter, Z.; Treon, S.P. Hyperviscosity-related retinopathy in waldenstrom macroglobulinemia. Arch. Ophthalmol. 2006, 124, 1601–1606. [Google Scholar] [CrossRef]
- Eton, E.A.; Abrams, G.; Khan, N.W.; Fahim, A.T. Autoimmune retinopathy associated with monoclonal gammopathy of undetermined significance: A case report. BMC Ophthalmol. 2020, 20, 153. [Google Scholar] [CrossRef]
- Garibaldi, D.C.; Gottsch, J.; de la Cruz, Z.; Haas, M.; Green, W.R. Immunotactoid keratopathy: A clinicopathologic case report and a review of reports of corneal involvement in systemic paraproteinemias. Surv. Ophthalmol. 2005, 50, 61–80. [Google Scholar] [CrossRef]
- Smith, S.J.; Johnson, M.W.; Ober, M.D.; Comer, G.M.; Smith, B.D. Maculopathy in Patients with Monoclonal Gammopathy of Undetermined Significance. Ophthalmol. Retin. 2020, 4, 300–309. [Google Scholar] [CrossRef]
- Coscas, F.; Sellam, A.; Glacet-Bernard, A.; Jung, C.; Goudot, M.; Miere, A.; Souied, E.H. Normative data for vascular density in superficial and deep capillary plexuses of healthy adults assessed by optical coherence tomography angiography. Investig. Ophthalmol. Vis. Sci. 2016, 57, 211–223. [Google Scholar] [CrossRef]
- Watson, J.A.; Olson, D.J.; Zhang, A.Y. Hyperviscosity Retinopathy Due to Waldenström Macroglobulinemia: A Case Report and Literature Review. J. VitreoRetinal Dis. 2021, 5, 520–524. [Google Scholar] [CrossRef]
- Li, J.; Zhang, R.; Gu, F.; Liu, Z.L.; Sun, P. Optical coherence tomography angiography characteristics in Waldenström macroglobulinemia retinopathy: A case report. World J. Clin. Cases 2020, 8, 6071–6079. [Google Scholar] [CrossRef]
- Dursun, M.E.; Erdem, S.; Karahan, M.; Ava, S.; Hazar, L.; Dursun, B.; Karakas, A.; Demircan, V.; Keklikci, U. Retinal Microvascular Changes in Patients with Multiple Myeloma: A Study Based on Optical Coherence Tomography Angiography. Curr. Eye Res. 2022, 47, 874–881. [Google Scholar] [CrossRef] [PubMed]
- Kwaan, H.C. Hyperviscosity in plasma cell dyscrasias. Clin. Hemorheol. Microcirc. 2013, 55, 75–83. [Google Scholar] [CrossRef]
- Dumas, G.; Merceron, S.; Zafrani, L.; Canet, E.; Lemiale, V.; Kouatchet, A.; Azoulay, E. Syndrome d’hyperviscosité plasmatique [Hyperviscosity syndrome]. Rev. Med. Interne 2015, 36, 588–595. [Google Scholar] [CrossRef] [PubMed]
- Caimi, G.; Hopps, E.; Carlisi, M.; Montana, M.; Gallà, E.; Lo Presti, R.; Siragusa, S. Hemorheological parameters in Monoclonal Gammopathy of Undetermined Significance (MGUS). Clin. Hemorheol. Microcirc. 2018, 68, 51–59. [Google Scholar] [CrossRef]
- Uggla, B.; Nilsson, T.K. Whole blood viscosity in plasma cell dyscrasias. Clin. Biochem. 2015, 48, 122–124. [Google Scholar] [CrossRef] [PubMed]
- Kashani, A.H.; Chen, C.L.; Gahm, J.K.; Zheng, F.; Richter, G.M.; Rosenfeld, P.J.; Shi, Y.; Wang, R.K. Optical coherence tomography angiography: A comprehensive review of current methods and clinical applications. Prog. Retin. Eye Res. 2017, 60, 66–100. [Google Scholar] [CrossRef] [PubMed]
- Tokayer, J.; Jia, Y.; Dhalla, A.H.; Huang, D. Blood flow velocity quantification using split-spectrum amplitude-decorrelation angiography with optical coherence tomography. Biomed. Opt. Express 2013, 4, 1909–1924. [Google Scholar] [CrossRef] [PubMed]
- Pascual-Prieto, J.; Burgos-Blasco, B.; Ávila Sánchez-Torija, M.; Fernández-Vigo, J.I.; Arriola-Villalobos, P.; Barbero Pedraz, M.A.; García-Feijoo, J.; Martínez-de-la-Casa, J.M. Utility of optical coherence tomography angiography in detecting vascular retinal damage caused by arterial hypertension. Eur. J. Ophthalmol. 2020, 30, 579–585. [Google Scholar] [CrossRef] [PubMed]
- Tan, W.; Yao, X.; Le, T.T.; Tan, A.C.S.; Cheung, C.Y.; Chin, C.W.L.; Schmetterer, L.; Chua, J. The Application of Optical Coherence Tomography Angiography in Systemic Hypertension: A Meta-Analysis. Front. Med. 2021, 8, 778330. [Google Scholar] [CrossRef]
- Czakó, C.; Sándor, G.; Ecsedy, M.; Récsán, Z.; Horváth, H.; Szepessy, Z.; Nagy, Z.Z.; Kovács, I. Decreased retinal capillary density is associated with a higher risk of diabetic retinopathy in patients with diabetes. Retina 2019, 39, 1710–1719. [Google Scholar] [CrossRef]
- István, L.; Czakó, C.; Benyó, F.; Élő, Á.; Mihály, Z.; Sótonyi, P.; Varga, A.; Nagy, Z.Z.; Kovács, I. The effect of systemic factors on retinal blood flow in patients with carotid stenosis: An optical coherence tomography angiography study. Geroscience 2022, 44, 389–401. [Google Scholar] [CrossRef]
- Lee, C.W.; Cheng, H.C.; Chang, F.C.; Wang, A.G. Optical Coherence Tomography Angiography Evaluation of Retinal Microvasculature Before and After Carotid Angioplasty and Stenting. Sci. Rep. 2019, 9, 14755. [Google Scholar] [CrossRef]
- Lahme, L.; Storp, J.J.; Marchiori, E.; Esser, E.; Eter, N.; Mihailovic, N.; Alnawaiseh, M. Evaluation of Ocular Perfusion in Patients with End-Stage Renal Disease Receiving Hemodialysis Using Optical Coherence Tomography Angiography. J. Clin. Med. 2023, 12, 3836. [Google Scholar] [CrossRef]
- Sampson, D.M.; Dubis, A.M.; Chen, F.K.; Zawadzki, R.J.; Sampson, D.D. Towards standardizing retinal optical coherence tomography angiography: A review. Light Sci. Appl. 2022, 11, 63. [Google Scholar] [CrossRef]
- Rakusiewicz, K.; Kanigowska, K.; Hautz, W.; Ziółkowska, L. Usefulness of retinal optical coherence tomography angiography evolution in cases of systemic diseases. Klin. Oczna. 2021, 123, 166–172. [Google Scholar] [CrossRef]
- Czakó, C.; István, L.; Ecsedy, M.; Récsán, Z.; Sándor, G.; Benyó, F.; Horváth, H.; Papp, A.; Resch, M.; Borbándy, Á.; et al. The effect of image quality on the reliability of OCT angiography measurements in patients with diabetes. Int. J. Retin. Vitr. 2019, 5, 46. [Google Scholar] [CrossRef] [PubMed]
- Czakó, C.; István, L.; Benyó, F.; Élő, Á.; Erdei, G.; Horváth, H.; Nagy, Z.Z.; Kovács, I. The Impact of Deterministic Signal Loss on OCT Angiography Measurements. Transl. Vis. Sci. Technol. 2020, 9, 10. [Google Scholar] [CrossRef]
- Greipp, P.R.; San Miguel, J.; Durie, B.G.; Crowley, J.J.; Barlogie, B.; Bladé, J.; Boccadoro, M.; Child, J.A.; Avet-Loiseau, H.; Kyle, R.A.; et al. International staging system for multiple myeloma. J. Clin. Oncol. 2005, 23, 3412–3420. [Google Scholar] [CrossRef] [PubMed]
- Palumbo, A.; Avet-Loiseau, H.; Oliva, S.; Lokhorst, H.M.; Goldschmidt, H.; Rosinol, L.; Richardson, P.; Caltagirone, S.; Lahuerta, J.J.; Facon, T.; et al. Revised International Staging System for Multiple Myeloma: A Report from International Myeloma Working Group. J. Clin. Oncol. 2015, 33, 2863–2869. [Google Scholar] [CrossRef] [PubMed]
| Monoclonal Gammopathy (n = 44) | Healthy Controls (n = 62) | p | |
|---|---|---|---|
| VD SVP—3 × 3 mm central macular area (%) | 44.54 ± 3.22 | 46.62 ± 2.84 | 0.04 |
| VD DVP—3 × 3 mm central macular area (%) | 48.59 ± 3.23 | 49.76 ± 3.99 | 0.77 |
| VD SVP—parafoveal area (%) | 47.54 ± 3.60 | 49.57 ± 2.95 | 0.08 |
| VD DVP—parafoveal area (%) | 51.13 ± 3.24 | 52.00 ± 3.99 | 0.93 |
| FAZ (mm2) | 0.293 | 0.289 | 0.91 |
| CRT (µm) | 263.73 | 254.95 | 0.22 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Czakó, C.; Gerencsér, D.; Kormányos, K.; Kéki-Kovács, K.; Németh, O.; Tóth, G.; Sándor, G.L.; Csorba, A.; Langenbucher, A.; Nagy, Z.Z.; et al. Evaluation of Retinal Blood Flow in Patients with Monoclonal Gammopathy Using OCT Angiography. J. Clin. Med. 2023, 12, 5227. https://doi.org/10.3390/jcm12165227
Czakó C, Gerencsér D, Kormányos K, Kéki-Kovács K, Németh O, Tóth G, Sándor GL, Csorba A, Langenbucher A, Nagy ZZ, et al. Evaluation of Retinal Blood Flow in Patients with Monoclonal Gammopathy Using OCT Angiography. Journal of Clinical Medicine. 2023; 12(16):5227. https://doi.org/10.3390/jcm12165227
Chicago/Turabian StyleCzakó, Cecilia, Dóra Gerencsér, Kitti Kormányos, Klaudia Kéki-Kovács, Orsolya Németh, Gábor Tóth, Gábor László Sándor, Anita Csorba, Achim Langenbucher, Zoltán Zsolt Nagy, and et al. 2023. "Evaluation of Retinal Blood Flow in Patients with Monoclonal Gammopathy Using OCT Angiography" Journal of Clinical Medicine 12, no. 16: 5227. https://doi.org/10.3390/jcm12165227
APA StyleCzakó, C., Gerencsér, D., Kormányos, K., Kéki-Kovács, K., Németh, O., Tóth, G., Sándor, G. L., Csorba, A., Langenbucher, A., Nagy, Z. Z., Varga, G., Gopcsa, L., Mikala, G., Kovács, I., & Szentmáry, N. (2023). Evaluation of Retinal Blood Flow in Patients with Monoclonal Gammopathy Using OCT Angiography. Journal of Clinical Medicine, 12(16), 5227. https://doi.org/10.3390/jcm12165227






