Unraveling Acute and Post-COVID Cytokine Patterns to Anticipate Future Challenges
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Cytokine/Chemokine Analysis
2.3. Statistics
3. Results
3.1. Demographic and Baseline Characteristics
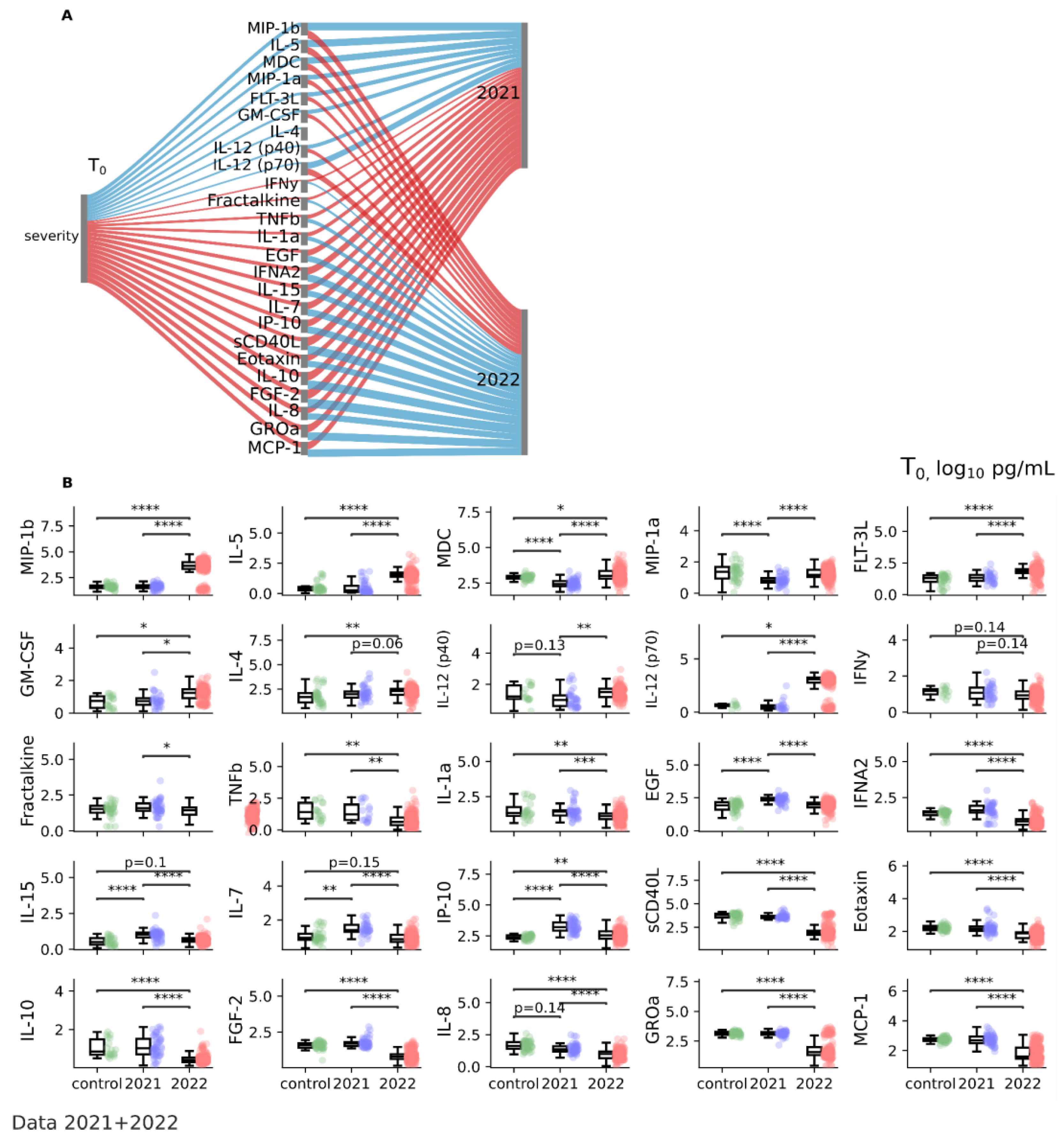
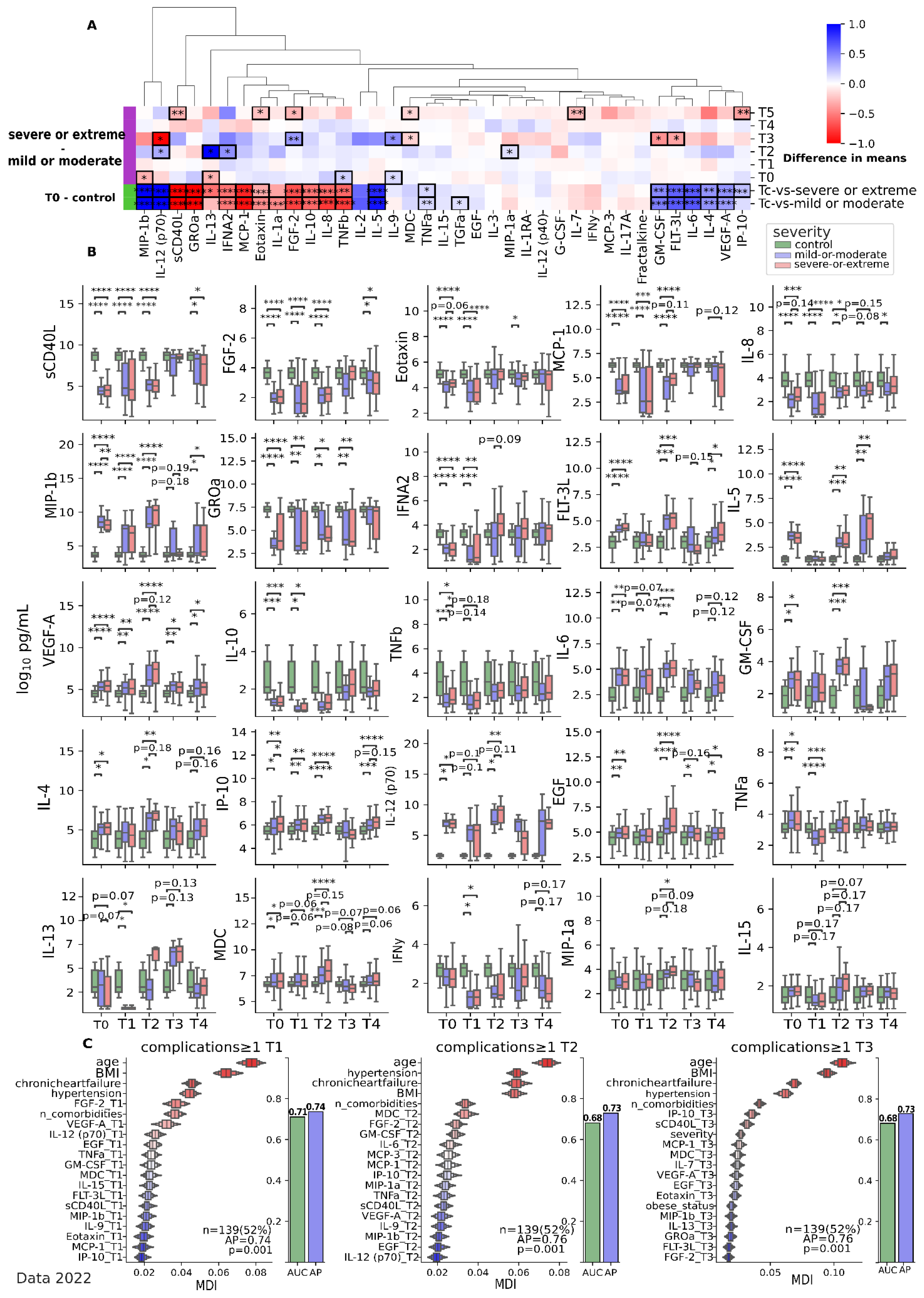
3.2. Cytokines Features of Acute COVID-19
3.3. Cytokines Pattern of Post-COVID Syndrome or Post-Acute Sequelae of SARS-CoV-2 Infection (PASC)
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Stoian, M.; Procopiescu, B.; Șeitan, S.; Scarlat, G. Post-COVID-19 syndrome: Insights into a novel post-infectious systemic disorder. J. Med. Life 2023, 16, 195–202. [Google Scholar] [CrossRef]
- Mehandru, S.; Merad, M. Pathological sequelae of long-haul COVID. Nat. Immunol. 2022, 23, 194–202. [Google Scholar] [CrossRef] [PubMed]
- Davis, H.E.; McCorkell, L.; Vogel, J.M.; Topol, E.J. Long COVID: Major findings, mechanisms and recommendations. Nat. Rev. Microbiol. 2023, 21, 133–146. [Google Scholar] [CrossRef] [PubMed]
- Ray, A.; Gulati, S.G.K.; Joshi, N.R.J. Cytokines and their Role in Health and Disease: A Brief Overview. MOJ Immunol. 2016, 4, 00121. [Google Scholar] [CrossRef]
- Liu, C.; Chu, D.; Kalantar-Zadeh, K.; George, J.; Young, H.A.; Liu, G. Cytokines: From Clinical Significance to Quantification. Adv. Sci. 2021, 8, 2004433. [Google Scholar] [CrossRef]
- Kao, C.-Y.; Mills, J.A.; Burke, C.J.; Morse, B.; Marques, B.F. Role of Cytokines and Growth Factors in the Manufacturing of iPSC-Derived Allogeneic Cell Therapy Products. Biology 2023, 12, 677. [Google Scholar] [CrossRef]
- Morán, G.A.G.; Parra-Medina, R.; Cardona, A.G.; Quintero-Ronderos, P.; Rodríguez, É.G. Chapter 9 Cytokines, chemokines and growth factors. In Autoimmunity: From Bench to Bedside; Anaya, J.-M., Shoenfeld, Y., Rojas-Villarraga, A., Levy, R.A., Cervera, R., Eds.; El Rosario University Press: Bogota, Colombia, 2013; p. 855. [Google Scholar]
- Xiao, T.; Yan, Z.; Xiao, S.; Xia, Y. Proinflammatory cytokines regulate epidermal stem cells in wound epithelialization. Stem Cell Res. Ther. 2020, 11, 232. [Google Scholar] [CrossRef]
- McInnes, I.B.; Schett, G. Cytokines in the pathogenesis of rheumatoid arthritis. Nat. Rev. Immunol. 2007, 7, 429–442. [Google Scholar] [CrossRef]
- O’Neill, L.A.; Kishton, R.J.; Rathmell, J. A guide to immunometabolism for immunologists. Nat. Rev. Immunol. 2016, 16, 553–565. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Deng, H.; Cui, H.; Fang, J.; Zuo, Z.; Deng, J.; Li, Y.; Wang, X.; Zhao, L. Inflammatory responses and inflammation-associated diseases in organs. Oncotarget 2018, 9, 7204–7218. [Google Scholar] [CrossRef]
- Bustamante, J.; Boisson-Dupuis, S.; Abel, L.; Casanova, J.-L. Mendelian susceptibility to mycobacterial disease: Genetic, immunological, and clinical features of inborn errors of IFN-γ immunity. Semin. Immunol. 2014, 26, 454–470. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, N.B.; Bastos, M.D.L.; Souza, A.S.; Netto, E.M.; Arruda, S.; Santos, S.B.; Carvalho, E.M. Impaired TNF, IL-1β, and IL-17 production and increased susceptibility to Mycobacterium tuberculosis infection in HTLV-1 infected individuals. Tuberculosis 2018, 108, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Abdollahi-Roodsaz, S.; Joosten, L.A.; Koenders, M.I.; Devesa, I.; Roelofs, M.F.; Radstake, T.R.; Heuvelmans-Jacobs, M.; Akira, S.; Nicklin, M.J.; Ribeiro-Dias, F.; et al. Stimulation of TLR2 and TLR4 differentially skews the balance of T cells in a mouse model of arthritis. J. Clin. Investig. 2008, 118, 205–216. [Google Scholar] [CrossRef] [PubMed]
- Munguía, L.; Nájera, N.; Martínez, F.d.J.; Díaz-Chiguer, D.; Jiménez-Ponce, F.; Ortiz-Flores, M.; Villarreal, F.; Ceballos, G. Correlation of Biomarkers of Endothelial Injury and Inflammation to Outcome in Hospitalized COVID-19 Patients. J. Clin. Med. 2022, 11, 7436. [Google Scholar] [CrossRef]
- Binayke, A.; Zaheer, A.; Dandotiya, J.; Gupta, S.K.; Mani, S.; Tripathy, M.R.; Madan, U.; Shrivastava, T.; Kumar, Y.; Pandey, A.K.; et al. Proinflammatory Innate Cytokines and Distinct Metabolomic Signatures Shape the T Cell Response in Active COVID-19. Vaccines 2022, 10, 1762. [Google Scholar] [CrossRef]
- Clinical Protocol of Diagnosis and Treatment. Coronavirus Infection COVID-19 in Adults. Available online: https://online.zakon.kz/Document/?doc_id=36043894&pos=6;-106#pos=6;-106 (accessed on 2 July 2023).
- World Health Organization. Guideline Clinical Management of COVID-19 Patients: Living Guideline; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Biswas, B.; Chattopadhyay, S.; Hazra, S.; Hansda, A.K.; Goswami, R. COVID-19 pandemic: The delta variant, T-cell responses, and the efficacy of developing vaccines. Inflamm. Res. 2022, 71, 377–396. [Google Scholar] [CrossRef]
- Fan, Y.; Li, X.; Zhang, L.; Wan, S.; Zhang, L.; Zhou, F. SARS-CoV-2 Omicron variant: Recent progress and future perspectives. Signal Transduct. Target. Ther. 2022, 7, 141. [Google Scholar] [CrossRef]
- Xu, P.; Zhang, S.; Kan, X.; Shen, X.; Mao, J.; Fang, C.; Wu, X.; Qiu, J.; Qu, P.; Qian, P.; et al. Changes and roles of IL-17A, VEGF-A and TNF-α in patients with cerebral infarction during the acute phase and early stage of recovery. Clin. Biochem. 2022, 107, 67–72. [Google Scholar] [CrossRef]
- Schultheiß, C.; Willscher, E.; Paschold, L.; Gottschick, C.; Klee, B.; Henkes, S.-S.; Bosurgi, L.; Dutzmann, J.; Sedding, D.; Frese, T.; et al. The IL-1β, IL-6, and TNF cytokine triad is associated with post-acute sequelae of COVID-19. Cell Rep. Med. 2022, 3, 100663. [Google Scholar] [CrossRef]
- Verbist, K.C.; Klonowski, K.D. Functions of IL-15 in anti-viral immunity: Multiplicity and variety. Cytokine 2012, 59, 467–478. [Google Scholar] [CrossRef]
- Singh, A.K.; Kasarpalkar, N.; Bhowmick, S.; Paradkar, G.; Talreja, M.; Shah, K.; Tiwari, A.; Palav, H.; Kaginkar, S.; Kulkarni, R.; et al. Opposing roles for sMAdCAM and IL-15 in COVID-19 associated cellular immune pathology. J. Leukoc. Biol. 2022, 111, 1287–1295. [Google Scholar] [CrossRef] [PubMed]
- Perpiñan, C.; Bertran, L.; Terra, X.; Aguilar, C.; Binetti, J.; Lopez-Dupla, M.; Rull, A.; Reverté, L.; Yeregui, E.; Gómez-Bertomeu, F.; et al. Resistin and IL-15 as Predictors of Invasive Mechanical Ventilation in COVID-19 Pneumonia Irrespective of the Presence of Obesity and Metabolic Syndrome. J. Pers. Med. 2022, 12, 391. [Google Scholar] [CrossRef] [PubMed]
- Kleymenov, D.A.; Bykonia, E.N.; Popova, L.I.; Mazunina, E.P.; Gushchin, V.A.; Kolobukhina, L.V.; Burgasova, O.A.; Kruzhkova, I.S.; Kuznetsova, N.A.; Shidlovskaya, E.V.; et al. A Deep Look Into COVID-19 Severity Through Dynamic Changes in Blood Cytokine Levels. Front. Immunol. 2021, 12, 771609. [Google Scholar] [CrossRef]
- Cabaro, S.; D’esposito, V.; Di Matola, T.; Sale, S.; Cennamo, M.; Terracciano, D.; Parisi, V.; Oriente, F.; Portella, G.; Beguinot, F.; et al. Cytokine signature and COVID-19 prediction models in the two waves of pandemics. Sci. Rep. 2021, 11, 20793. [Google Scholar] [CrossRef] [PubMed]
- Rivas-Fuentes, S.; Valdés, V.J.; Espinosa, B.; Gorocica-Rosete, P.; Salgado-Aguayo, A. Could SARS-CoV-2 blocking of ACE2 in endothelial cells result in upregulation of CX3CL1, promoting thrombosis in COVID-19 patients? Med. Hypotheses 2021, 151, 110570. [Google Scholar] [CrossRef]
- Monserrat, J.; Gómez-Lahoz, A.; Ortega, M.A.; Sanz, J.; Muñoz, B.; Arévalo-Serrano, J.; Rodríguez, J.M.; Gasalla, J.M.; Gasulla, Ó.; Arranz, A.; et al. Role of Innate and Adaptive Cytokines in the Survival of COVID-19 Patients. Int. J. Mol. Sci. 2022, 23, 10344. [Google Scholar] [CrossRef]
- Mohammadhosayni, M.; Mohammadi, F.S.; Ezzatifar, F.; Gorabi, A.M.; Khosrojerdi, A.; Aslani, S.; Hemmatzadeh, M.; Yazdani, S.; Arabi, M.; Marofi, F.; et al. Matrix metalloproteinases are involved in the development of neurological complications in patients with Coronavirus disease 2019. Int. Immunopharm. 2021, 100, 108076. [Google Scholar] [CrossRef]
- Tong, M.; Jiang, Y.; Xia, D.; Xiong, Y.; Zheng, Q.; Chen, F.; Zou, L.; Xiao, W.; Zhu, Y. Elevated Expression of Serum Endothelial Cell Adhesion Molecules in COVID-19 Patients. J. Infect. Dis. 2020, 222, 894–898. [Google Scholar] [CrossRef]
- Hsu, R.-J.; Yu, W.-C.; Peng, G.-R.; Ye, C.-H.; Hu, S.; Chong, P.C.T.; Yap, K.Y.; Lee, J.Y.C.; Lin, W.-C.; Yu, S.-H. The Role of Cytokines and Chemokines in Severe Acute Respiratory Syndrome Coronavirus 2 Infections. Front. Immunol. 2022, 13, 832394. [Google Scholar] [CrossRef]
- Du, F.; Liu, B.; Zhang, S. COVID-19: The role of excessive cytokine release and potential ACE2 down-regulation in promoting hypercoagulable state associated with severe illness. J. Thromb. Thrombolysis 2021, 51, 313–329. [Google Scholar]
- Brojakowska, A.; Eskandari, A.; Bisserier, M.; Bander, J.; Garikipati, V.N.S.; Hadri, L.; Goukassian, D.A.; Fish, K.M. Comorbidities, sequelae, blood biomarkers and their associated clinical outcomes in the Mount Sinai Health System COVID-19 patients. PLoS ONE 2021, 16, e0253660. [Google Scholar] [CrossRef]
- Sciacchitano, S.; De Vitis, C.; D’Ascanio, M.; Giovagnoli, S.; De Dominicis, C.; Laghi, A.; Anibaldi, P.; Petrucca, A.; Salerno, G.; Santino, I.; et al. Gene signature and immune cell profiling by high-dimensional, single-cell analysis in COVID-19 patients, presenting Low T3 syndrome and coexistent hematological malignancies. J. Transl. Med. 2021, 19, 139. [Google Scholar] [CrossRef] [PubMed]
- Witkowski, J.M.; Fulop, T.; Bryl, E. Immunosenescence and COVID-19. Mech. Ageing Dev. 2022, 204, 111672. [Google Scholar] [CrossRef]
- Goldberg, E.M.; Southerland, L.T.; Meltzer, A.C.; Pagenhardt, J.; Hoopes, R.; Camargo, C.A.; Kline, J.A. Age-related differences in symptoms in older emergency department patients with COVID-19: Prevalence and outcomes in a multicenter cohort. J. Am. Geriatr. Soc. 2022, 70, 1918–1930. [Google Scholar] [CrossRef]
- Liu, Y.; Mao, B.; Liang, S.; Yang, J.-W.; Lu, H.-W.; Chai, Y.-H.; Wang, L.; Zhang, L.; Li, Q.-H.; Zhao, L.; et al. Association between age and clinical characteristics and outcomes of COVID-19. Eur. Respir. J. 2020, 55, 2001112. [Google Scholar] [CrossRef]
- Yokota, S.; Miyamae, T.; Kuroiwa, Y.; Nishioka, K. Novel Coronavirus Disease 2019 (COVID-19) and Cytokine Storms for More Effective Treatments from an Inflammatory Pathophysiology. J. Clin. Med. 2021, 10, 801. [Google Scholar] [CrossRef]
- Berry, A.; Balard, P.; Coste, A.; Olagnier, D.; Lagane, C.; Authier, H.; Benoit-Vical, F.; Lepert, J.-C.; Séguéla, J.-P.; Magnaval, J.-F.; et al. IL-13 induces expression of CD36 in human monocytes through PPARγ activation. Eur. J. Immunol. 2007, 37, 1642–1652. [Google Scholar] [CrossRef] [PubMed]
- Zha, L.-F.; Nie, S.-F.; Chen, Q.-W.; Liao, Y.-H.; Zhang, H.-S.; Dong, J.-T.; Xie, T.; Wang, F.; Tang, T.-T.; Xia, N.; et al. IL-13 may be involved in the development of CAD via different mechanisms under different conditions in a Chinese Han population. Sci. Rep. 2018, 8, 6182. [Google Scholar] [CrossRef] [PubMed]
- Kang, K.; Reilly, S.M.; Karabacak, V.; Gangl, M.R.; Fitzgerald, K.; Hatano, B.; Lee, C.-H. Adipocyte-Derived Th2 Cytokines and Myeloid PPARδ Regulate Macrophage Polarization and Insulin Sensitivity. Cell Metab. 2008, 7, 485–495. [Google Scholar] [CrossRef]






| Parameter M ± Sd (IQR)/Counts | Control (n = 40) | Mild (n = 38) | Moderate (n = 165) | Severe (n = 71) | Extremely Severe (n = 20) | p-Value |
|---|---|---|---|---|---|---|
| Age (IQR) 1 | 53.0 ± 8.4 (48.2–59.0) | 51.6 ± 16.1 (39.5–65.0) | 54.1 ± 15.0 (45.0–66.0) | 61.7 ± 13.2 (56.5–70.0) | 65.3 ± 14.1 (58.0–73.0) | 0.007 a |
| Gender, M/F (M%) 2 | 21/19 (52.5%) | 16/22 (42.1%) | 64/101 (38.9%) | 22/49 (31.5%) | 13/7 (65%) | 0.036 b |
| BMI (IQR) 1 | 26.3 ± 4.4 (23.6–28.6) | 27.4 ± 5.4 (24.0–30.2) | 28.8 ± 6.8 (24.2–32.4) | 29.1 ± 6.1 (24.8–32.4) | 30.2 ± 5.2 (25.9–33.4) | 0.028 a |
| Year of observation 2021/2022 (2021%) 2 | - | 0/38 (0%) | 0/165 (0%) | 35/36 (49.29%) | 15/5 (75%) | ≤0.0001 b, 0.046 c |
| Pneumonia (Yes%) 2 | - | 4/34 (10.5%) | 162/3 (98.2%) | 68/3 (95.7%) | 20/0 (100%) | ≤0.0001 b |
| PCR+/− (Positive%) 2 | - | 23/15 (60.5%) | 121/44 (73.3%) | 23/48 (32%) | 5/15 (25%) | ≤0.0001 b |
| Normal/Overweight/Obesity (Overweight or Obese%) 2 | - | 13/10/15 (65.7%) | 48/66/51 (70.1%) | 20/27/24 (71.8%) | 5/10/5 (75%) | 0.007 b |
| Hyper-/Normotension (Yes%) 2 | - | 21/17 (55.3%) | 85/80 (51.5%) | 20/51 (28.2%) | 5/15 (25%) | 0.001 b |
| Type II diabetes Yes/No (Yes%) 2 | - | 3/35 (7.9%) | 22/143 (13.3%) | 12/59 (16.9%) | 4/16 (20%) | 0.51 b |
| Chronic heart failure (Yes%) 2 | - | 5/33 (13.2%) | 22/143 (13.3%) | 15/56 (21.2%) | 3/17 (15%) | 0.48 b |
| Comorbidities ≥ 1 (Yes%) 2 | - | 35/3 (92.1%) | 143/22 (86.7%) | 61/10 (85.9%) | 17/3 (85%) | 0.79 b |
| Control vs. T0 a | Control vs. T0 a | Pneumonia-No vs. Pneumonia-Yes in T0 b | ||||
|---|---|---|---|---|---|---|
| p-Value2021 | p-Value2022 | p-Value | p-Value | |||
| pro-inflammatory, 2021 + 2022 (↑) | 2021 (↑)–2022 (↓), 2022 (↓): | pro-inflammatory, pneumonia-yes (↑) | ||||
| TNFa | 0.034 | 0.0007 | FGF-2 | <0.0001 | IFNA2 | 0.0051 |
| IL-6 | 0.14 | 0.0009 | IFNA2 | <0.0001 | IL-15 | 0.0087 |
| IL-1RA | 0.0051 | 0.73 | IL-1a | <0.0001 | IL-7 | 0.0333 |
| IL-15 | <0.0001 | 0.1 | IL-7 | <0.0001 | sCD40L | 0.0336 |
| IL-2 | 0.5 | 0.4 | IL-10 | <0.0001 | MCP-1 | 0.0001 |
| IL-5 | 0.51 | <0.0001 | 2021 (↓)–2022 (↑), 2021 (↓): | anti-inflammatory, pneumonia-yes (↑) | ||
| MIP-1b | 0.85 | <0.0001 | IL-1b | 0.0548 | FGF-2 | 0.0066 |
| anti-inflammatory, 2021 + 2022 (↑) | IL-12 | 0.0001 | pro-inflammatory, pneumonia-yes (↓) | |||
| IL-4 | 0.25 | 0.0033 | MDC | <0.0001 | MIP-1b | 0.049 |
| IP-10 | <0.0001 | 0.0051 | 2021 (=)–2022 (↓), 2022 (↓): | MIP-1a | 0.0093 | |
| TGFa | 0.0002 | 0.069 | Fractalkin | 0.0023 | MDC | 0.055 |
| EGF | <0.0001 | 0.45 | GM-CSF | <0.0001 | GM-CSF | 0.0045 |
| VEGF-A | 0.0023 | 0.0001 | GROa | <0.0001 | ||
| 2021 + 2022 (↓) | IL-12 (p70) | <0.0001 | ||||
| MIP-1a | <0.0001 | 0.22 | ||||
| IL-8 | 0.13 | <0.0001 | ||||
| IL-9 | 0.29 | 0.74 | ||||
| MCP-1 | 0.75 | 0.0001 | ||||
| Eotaxin | 0.33 | <0.0001 | ||||
| IFNgamma | 0.53 | 0.14 | ||||
| sCD40L | 0.4 | <0.0001 | ||||
| TNFb | 0.82 | 0.0036 | ||||
| Severe or Extremely Severe vs. Mild/Moderate in T0 a | Severe/Extremely Severe in T0 vs. Severe/Extremely Severe in T1 b | Mild/Moderate in T2 vs. Severe/Extremely Severe in T2 b | ||||
|---|---|---|---|---|---|---|
| p-Value (Severe) | p-Value (Extremely Severe) | p-Value | p-Value | |||
| Pro-Inflammatory (↑) | (↓) | Severe/Extremely Severe (↑) | ||||
| MCP-1 | <0.0001 | 0.0007 | FGF-2 | <0.0001 | IL-13 | 0.0284 |
| IFNa2 | 0.0016 | 0.0001 | VEGF-A | 0.11 | IFNa2 | 0.01 |
| IL-7 | 0.0199 | 0.0008 | EGF | <0.0001 | MIP-1a | 0.0279 |
| IL-15 | 0.0073 | 0.0001 | IL-12(p70) | <0.0001 | IL-4 | 0.061 |
| EGF | 0.0002 | 0.0017 | IL-12(p70) | 0.0181 | ||
| IP-10 | <0.0001 | <0.0001 | MCP-1 | 0.0767 | ||
| IL-8 | <0.0001 | 0.17 | IL-1a | 0.0764 | ||
| Eotaxin | <0.0001 | 0.0031 | MDC | 0.12 | ||
| FGF-2 | <0.0001 | <0.0001 | IL-15 | 0.076 | ||
| GROa | <0.0001 | <0.0001 | VEGF-A | 0.076 | ||
| sCD40L | <0.0001 | 0.0001 | ||||
| IL-10 | <0.0001 | <0.0001 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bekbossynova, M.; Tauekelova, A.; Sailybayeva, A.; Kozhakhmetov, S.; Mussabay, K.; Chulenbayeva, L.; Kossumov, A.; Khassenbekova, Z.; Vinogradova, E.; Kushugulova, A. Unraveling Acute and Post-COVID Cytokine Patterns to Anticipate Future Challenges. J. Clin. Med. 2023, 12, 5224. https://doi.org/10.3390/jcm12165224
Bekbossynova M, Tauekelova A, Sailybayeva A, Kozhakhmetov S, Mussabay K, Chulenbayeva L, Kossumov A, Khassenbekova Z, Vinogradova E, Kushugulova A. Unraveling Acute and Post-COVID Cytokine Patterns to Anticipate Future Challenges. Journal of Clinical Medicine. 2023; 12(16):5224. https://doi.org/10.3390/jcm12165224
Chicago/Turabian StyleBekbossynova, Makhabbat, Ainur Tauekelova, Aliya Sailybayeva, Samat Kozhakhmetov, Karakoz Mussabay, Laura Chulenbayeva, Alibek Kossumov, Zhanagul Khassenbekova, Elizaveta Vinogradova, and Almagul Kushugulova. 2023. "Unraveling Acute and Post-COVID Cytokine Patterns to Anticipate Future Challenges" Journal of Clinical Medicine 12, no. 16: 5224. https://doi.org/10.3390/jcm12165224
APA StyleBekbossynova, M., Tauekelova, A., Sailybayeva, A., Kozhakhmetov, S., Mussabay, K., Chulenbayeva, L., Kossumov, A., Khassenbekova, Z., Vinogradova, E., & Kushugulova, A. (2023). Unraveling Acute and Post-COVID Cytokine Patterns to Anticipate Future Challenges. Journal of Clinical Medicine, 12(16), 5224. https://doi.org/10.3390/jcm12165224





