Associations of Depressive Symptoms with Subjective Cognitive Decline in Elderly People—A Cross-Sectional Analysis from the AgeWell.de-Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
- ▪
- Nutritional advice
- ▪
- An enhancement of physical activity
- ▪
- Cognitive training
- ▪
- An optimization of the individuals’ medication
- ▪
- Managing the individuals’ vascular risk factors
- ▪
- Improving the individuals’ social engagement
- ▪
- Interventions for depressive symptoms, bereavement, and grief
2.2. Participants
2.3. Instruments
2.3.1. Mild Cognitive Impairment-Score (MCI-Score)
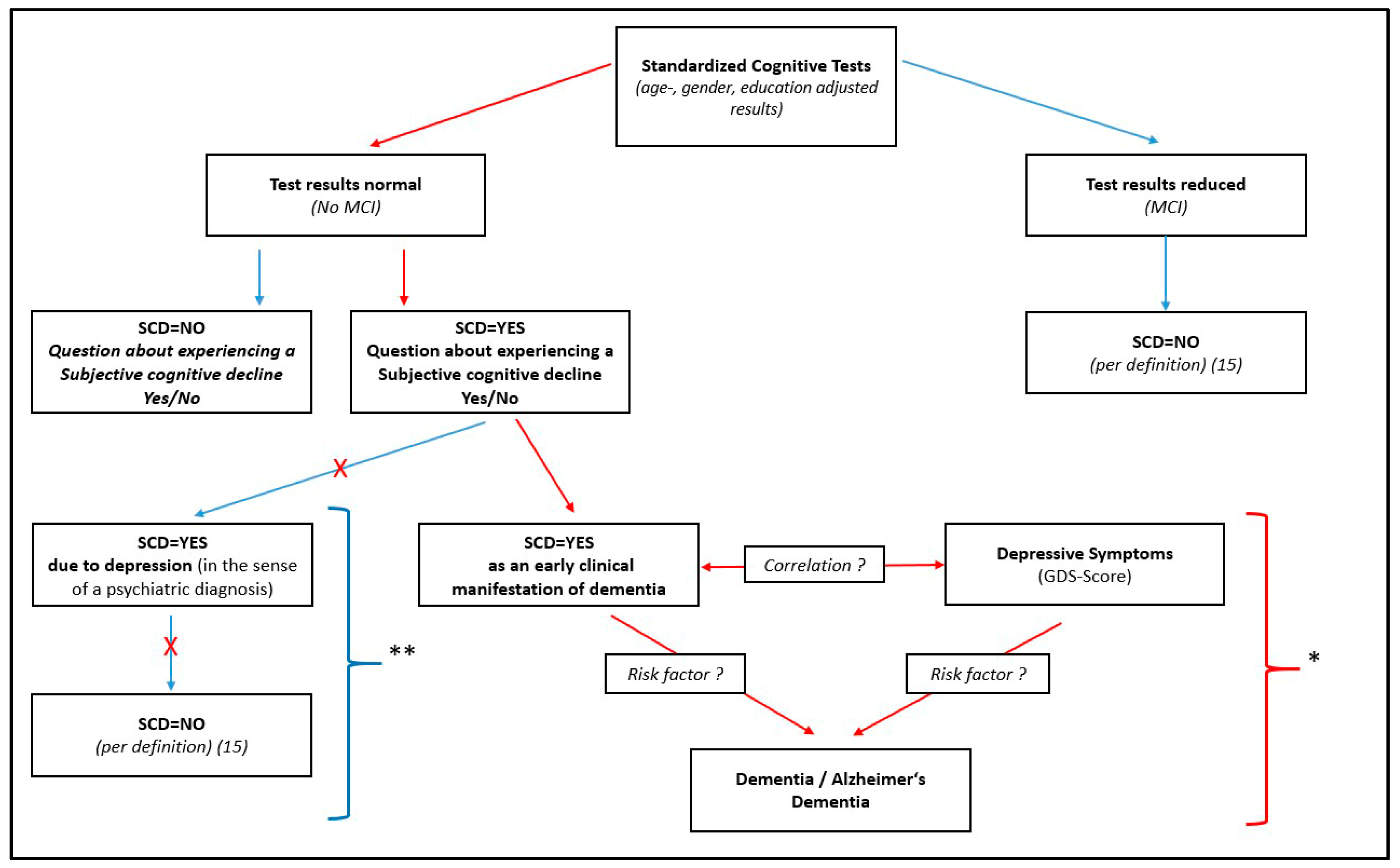
2.3.2. Calculation of the SCD
2.3.3. Calculation of the Lubben Social Network Scale
2.3.4. Calculation of the Education Groups According to CASMIN
2.3.5. Presence of Sleeping Problems
2.3.6. Presence of Depressive Symptoms
2.3.7. Selection of Variables for the Descriptive Analysis of Participants with and without Depressive Symptoms
2.4. Trial Registration and Ethical Clearance
2.5. Statistical Analyses and Procedure
3. Results
3.1. Prevalence of Depressive Symptoms and Description of the Differences between Study Participants with and without Depressive Symptoms
3.2. Prevalence of SCD and Description of the Differences between Study Participants with and without SCD
3.3. Prevalence of Depressive Symptoms and SCD
3.4. Multivariate Analysis of Variables That Influence SCD
4. Discussion
4.1. SCD-Regression Model
4.2. Descriptive Analysis of Depressive Symptoms
4.3. Strengths
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CAIDE | Cardiovascular risk factors, aging, and incidence of dementia |
| CASMIN | Comparative analysis of social mobility in industrial nations |
| GDS | Geriatric depression scale |
| SCD | Subjective cognitive decline |
| MCI | Mild cognitive impairment |
| MoCA | Montreal cognitive assessment |
| LSNS-6 | Lubben social network scale 6-items |
References
- Prince, M.J.; Wimo, A.; Guerchet, M.M.; Ali, G.C.; Wu, Y.T.; Prina, M. World Alzheimer Report 2015—The Global Impact of Dementia: An Analysis of Prevalence, Incidence, Cost and Trends; Alzheimer’s Disease International: London, UK, 2015. [Google Scholar]
- Anders, W.; Prince, M. World Alzheimer Report 2010. The Global Economic Impact of Dementia; Alzheimer’s Disease International: London, UK, 2010. [Google Scholar]
- Prince, M.; Bryce, R.; Albanese, E.; Wimo, A.; Ribeiro, W.; Ferri, C.P. The global prevalence of dementia: A systematic review and metaanalysis. Alzheimer’s Dement. J. Alzheimer’s Assoc. 2013, 9, 63–75.e2. [Google Scholar] [CrossRef]
- WHO. Dementia: A Public Health Priority; World Health Organization: Geneva, Switzerland, 2012. [Google Scholar]
- Zülke, A.; Luck, T.; Pabst, A.; Hoffmann, W.; Thyrian, J.R.; Gensichen, J.; Kaduszkiewicz, H.; König, H.H.; Haefeli, W.E.; Czock, D.; et al. AgeWell.de—Study protocol of a pragmatic multi-center cluster-randomized controlled prevention trial against cognitive decline in older primary care patients. BMC Geriatr. 2019, 19, 203. [Google Scholar] [CrossRef]
- Luck, T.; Riedel-Heller, S.G. Prävention von Alzheimer-Demenz in Deutschland: Eine Hochrechnung des möglichen Potenzials der Reduktion ausgewählter Risikofaktoren [Prevention of Alzheimer’s dementia in Germany: A projection of the possible potential of reducing selected risk factors]. Der Nervenarzt 2016, 87, 1194–1200. [Google Scholar] [CrossRef]
- Norton, S.; Matthews, F.E.; Barnes, D.E.; Yaffe, K.; Brayne, C. Potential for primary prevention of Alzheimer’s disease: An analysis of population-based data. Lancet Neurol. 2014, 13, 788–794. [Google Scholar] [CrossRef]
- Livingston, G.; Huntley, J.; Sommerlad, A.; Ames, D.; Ballard, C.; Banerjee, S.; Brayne, C.; Burns, A.; Cohen-Mansfield, J.; Cooper, C.; et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet 2020, 396, 413–446. [Google Scholar] [CrossRef]
- Diniz, B.S.; Butters, M.A.; Albert, S.M.; Dew, M.A.; Reynolds, C.F., 3rd. Late-life depression and risk of vascular dementia and Alzheimer’s disease: Systematic review and meta-analysis of community-based cohort studies. Br. J. Psychiatry J. Ment. Sci. 2013, 202, 329–335. [Google Scholar] [CrossRef]
- da Silva, J.; Gonçalves-Pereira, M.; Xavier, M.; Mukaetova-Ladinska, E.B. Affective disorders and risk of developing dementia: Systematic review. Br. J. Psychiatry J. Ment. Sci. 2013, 202, 177–186. [Google Scholar] [CrossRef]
- Barnes, D.E.; Yaffe, K. The projected effect of risk factor reduction on Alzheimer’s disease prevalence. Lancet Neurol. 2011, 10, 819–828. [Google Scholar] [CrossRef]
- Jorm, A.F. Is depression a risk factor for dementia or cognitive decline? A review. Gerontology 2000, 46, 219–227. [Google Scholar] [CrossRef]
- Forsell, Y.; Winblad, B. Major depression in a population of demented and nondemented older people: Prevalence and correlates. J. Am. Geriatr. Soc. 1998, 46, 27–30. [Google Scholar] [CrossRef]
- Moussavi, S.; Chatterji, S.; Verdes, E.; Tandon, A.; Patel, V.; Ustun, B. Depression, chronic diseases, and decrements in health: Results from the World Health Surveys. Lancet 2007, 370, 851–858. [Google Scholar] [CrossRef]
- Liew, T.M. Depression, subjective cognitive decline, and the risk of neurocognitive disorders. Alzheimer’s Res. Ther. 2019, 11, 70. [Google Scholar] [CrossRef]
- Wang, S.M.; Han, K.D.; Kim, N.Y.; Um, Y.H.; Kang, D.W.; Na, H.R.; Lee, C.U.; Lim, H.K. Late-life depression, subjective cognitive decline, and their additive risk in incidence of dementia: A nationwide longitudinal study. PLoS ONE 2021, 16, e0254639. [Google Scholar] [CrossRef]
- Jessen, F.; Amariglio, R.E.; van Boxtel, M.; Breteler, M.; Ceccaldi, M.; Chételat, G.; Dubois, B.; Dufouil, C.; Ellis, K.A.; van der Flier, W.M.; et al. Subjective Cognitive Decline Initiative (SCD-I) Working Group (2014). A conceptual framework for research on subjective cognitive decline in preclinical Alzheimer’s disease. Alzheimer’s Dement. J. Alzheimer’s Assoc. 2014, 10, 844–852. [Google Scholar] [CrossRef]
- Schliep, K.C.; Barbeau, W.A.; Lynch, K.E.; Sorweid, M.K.; Varner, M.W.; Foster, N.L.; Qeadan, F. Overall and sex-specific risk factors for subjective cognitive decline: Findings from the 2015-2018 Behavioral Risk Factor Surveillance System Survey. Biol. Sex Differ. 2022, 13, 16. [Google Scholar] [CrossRef]
- Lin, L.H.; Wang, S.B.; Xu, W.Q.; Hu, Q.; Zhang, P.; Ke, Y.F.; Huang, J.H.; Ding, K.R.; Li, X.L.; Hou, C.L.; et al. Subjective cognitive decline symptoms and its association with socio-demographic characteristics and common chronic diseases in the southern Chinese older adults. BMC Public Health 2022, 22, 127. [Google Scholar] [CrossRef]
- O’Brien, J.T.; Lloyd, A.; McKeith, I.; Gholkar, A.; Ferrier, N. A longitudinal study of hippocampal volume, cortisol levels, and cognition in older depressed subjects. Am. J. Psychiatry 2004, 161, 2081–2090. [Google Scholar] [CrossRef]
- Burmester, B.; Leathem, J.; Merrick, P. Subjective Cognitive Complaints and Objective Cognitive Function in Aging: A Systematic Review and Meta-Analysis of Recent Cross-Sectional Findings. Neuropsychol. Rev. 2016, 26, 376–393. [Google Scholar] [CrossRef]
- Reid, L.M.; Maclullich, A.M. Subjective memory complaints and cognitive impairment in older people. Dement. Geriatr. Cogn. Disord. 2006, 22, 471–485. [Google Scholar] [CrossRef]
- Röhr, S.; Zülke, A.; Luppa, M.; Brettschneider, C.; Weißenborn, M.; Kühne, F.; Zöllinger, I.; Samos, F.Z.; Bauer, A.; Döhring, J.; et al. Recruitment and Baseline Characteristics of Participants in the AgeWell.de Study-A Pragmatic Cluster-Randomized Controlled Lifestyle Trial against Cognitive Decline. Int. J. Environ. Res. Public Health 2021, 18, 408. [Google Scholar] [CrossRef]
- Reitan, R.M. Trail Making Test: Manual for Administration and Scoring; Reitan Neuropsychology Laboratory: Tempe, AZ, USA, 1992. [Google Scholar]
- Satzger, W.; Hampel, H.; Padberg, F.; Bürger, K.; Nolde, T.; Ingrassia, G.; Engel, R.R. Zur praktischen Anwendung der CERAD-Testbatterie als neuropsychologisches Demenzscreening [Practical application of the CERAD test battery as a neuropsychological dementia screening test]. Der Nervenarzt 2001, 72, 196–203. [Google Scholar] [CrossRef]
- Morris, J.C.; Mohs, R.C.; Rogers, H.; Fillenbaum, G.; Heyman, A. Consortium to establish a registry for Alzheimer’s disease (CERAD) clinical and neuropsychological assessment of Alzheimer’s disease. Psychopharmacol. Bull. 1988, 24, 641–652. [Google Scholar]
- Morris, J.C.; Heyman, A.; Mohs, R.C.; Hughes, J.P.; van Belle, G.; Fillenbaum, G.; Mellits, E.D.; Clark, C. The Consortium to Establish a Registry for Alzheimer’s Disease (CERAD). Part I. Clinical and neuropsychological assessment of Alzheimer’s disease. Neurology 1989, 39, 1159–1165. [Google Scholar] [CrossRef]
- Isaacs, B.; Kennie, A.T. The set test as an aid to the detection of dementia in old people. Br. J. Psychiatry J. Ment. Sci. 1973, 123, 467–470. [Google Scholar] [CrossRef]
- Tombaugh, T.N.; Kozak, J.; Rees, L. Normative data stratified by age and education for two measures of verbal fluency: FAS and animal naming. Arch. Clin. Neuropsychol. Off. J. Natl. Acad. Neuropsychol. 1999, 14, 167–177. [Google Scholar]
- Rosen, W.G.; Mohs, R.C.; Davis, K.L. A new rating scale for Alzheimer’s disease. Am. J. Psychiatry 1984, 141, 1356–1364. [Google Scholar] [CrossRef] [PubMed]
- Baron-Cohen, S.; Wheelwright, S.; Hill, J.; Raste, Y.; Plumb, I. The “Reading the Mind in the Eyes” Test revised version: A study with normal adults, and adults with Asperger syndrome or high-functioning autism. J. Child Psychol. Psychiatry Allied Discip. 2001, 42, 241–251. [Google Scholar] [CrossRef]
- Bölte, S. Reading Mind in the Eyes Test für Erwachsene (dt. Fassung) von S. Baron-Cohen; Johann-Wolgang-Goethe-Universität: Frankfurt am Main, Germany, 2005. [Google Scholar]
- Mahony, F.I.; Barthel, D.W. Functional evaluation, the barthel index; A simple index of independence useful in scoring improvement in the rehabilitation of the chronically ill. Md. State Med. J. 1965, 14, 56–61. [Google Scholar]
- Lubben, J.; Blozik, E.; Gillmann, G.; Iliffe, S.; von Renteln Kruse, W.; Beck, J.C.; Stuck, A.E. Performance of an abbreviated version of the Lubben Social Network Scale among three European community-dwelling older adult populations. Gerontologist 2006, 46, 503–513. [Google Scholar] [CrossRef]
- König, W.; Lüttinger, P.; Müller, W. A Comparative Analysis of the Development and Structure of Educational Systems: Methodological Foundations and the Construction of a Comparative Educational Scale; Universität Mannheim, Institut für Sozialwissenschaften: Mannheim, Germany, 1988. [Google Scholar]
- Sheikh, J.I.; Yesavage, J.A. Geriatric Depression Scale (GDS): Recent evidence and development of a shorter version. Clin. Gerontol. J. Aging Ment. Health 1986, 5, 165–173. [Google Scholar]
- Gauggel, S.; Birkner, B. Validität und Reliabilität einer deutschen Version der Geriatrischen Depressionsskala (GDS). Z. Klin. Psychol. 1999, 28, 18–27. [Google Scholar] [CrossRef]
- Mannan, M.; Mamun, A.; Doi, S.; Clavarino, A. Prospective Associations between Depression and Obesity for Adolescent Males and Females—A Systematic Review and Meta-Analysis of Longitudinal Studies. PLoS ONE 2016, 11, e0157240. [Google Scholar] [CrossRef] [PubMed]
- Gan, Z.; Li, Y.; Xie, D.; Shao, C.; Yang, F.; Shen, Y.; Zhang, N.; Zhang, G.; Tian, T.; Yin, A.; et al. The impact of educational status on the clinical features of major depressive disorder among chinese women. J. Affect. Disord. 2012, 136, 988–992. [Google Scholar] [CrossRef] [PubMed]
- Gavin, A.R.; Walton, E.; Chae, D.H.; Alegria, M.; Jackson, J.S.; Takeuchi, D. The associations between socio-economic status and major depressive disorder among blacks, latinos, asians and non-hispanic whites: Findings from the Collaborative Psychiatric Epidemiology Studies. Psychol. Med. 2010, 40, 51–61. [Google Scholar] [CrossRef] [PubMed]
- Cacioppo, J.T.; Hughes, M.E.; Waite, L.J.; Hawkley, L.C.; Thisted, R.A. Loneliness as a specific risk factor for depressive symptoms: Cross-sectional and longitudinal analyses. Psychol. Aging 2006, 21, 140–151. [Google Scholar] [CrossRef] [PubMed]
- Beekman, A.T.; Deeg, D.J.; Geerlings, S.W.; Schoevers, R.A.; Smit, J.H.; van Tilburg, W. Emergence and persistence of late life depression: A 3-year follow-up of the Longitudinal Aging Study Amsterdam. J. Affect. Disord. 2001, 65, 131–138. [Google Scholar] [CrossRef]
- Domènech-Abella, J.; Lara, E.; Rubio-Valera, M.; Olaya, B.; Moneta, M.V.; Rico-Uribe, L.A.; Ayuso-Mateos, J.L.; Mundó, J.; Haro, J.M. Loneliness and depression in the elderly: The role of social network. Soc. Psychiatry Psychiatr. Epidemiol. 2017, 52, 381–390. [Google Scholar] [CrossRef]
- Schuch, F.B.; Stubbs, B. The Role of Exercise in Preventing and Treating Depression. Curr. Sports Med. Rep. 2019, 18, 299–304. [Google Scholar] [CrossRef]
- Pearce, M.; Garcia, L.; Abbas, A.; Strain, T.; Schuch, F.B.; Golubic, R.; Kelly, P.; Khan, S.; Utukuri, M.; Laird, Y.; et al. Association Between Physical Activity and Risk of Depression: A Systematic Review and Meta-analysis. JAMA Psychiatry 2022, 79, 550–559. [Google Scholar] [CrossRef]
- Fang, H.; Tu, S.; Sheng, J.; Shao, A. Depression in sleep disturbance: A review on a bidirectional relationship, mechanisms and treatment. J. Cell. Mol. Med. 2019, 23, 2324–2332. [Google Scholar] [CrossRef]
- Balash, Y.; Mordechovich, M.; Shabtai, H.; Giladi, N.; Gurevich, T.; Korczyn, A.D. Subjective memory complaints in elders: Depression, anxiety, or cognitive decline? Acta Neurol. Scand. 2013, 127, 344–350. [Google Scholar] [CrossRef]
- Lee, S.H.; Kang, Y.; Cho, S.J. Subjective cognitive decline in patients with migraine and its relationship with depression, anxiety, and sleep quality. J. Headache Pain 2017, 18, 77. [Google Scholar] [CrossRef] [PubMed]
- Xu, W.Q.; Lin, L.H.; Ding, K.R.; Ke, Y.F.; Huang, J.H.; Hou, C.L.; Jia, F.J.; Wang, S.B. The role of depression and anxiety in the relationship between poor sleep quality and subjective cognitive decline in Chinese elderly: Exploring parallel, serial, and moderated mediation. J. Affect. Disord. 2021, 294, 464–471. [Google Scholar] [CrossRef] [PubMed]
- Gutzmann, H.; Qazi, A. Depression associated with dementia. Z. Gerontol. Geriatr. 2015, 48, 305–311. [Google Scholar] [CrossRef]
- Kessing, L.V. Depression and the risk for dementia. Curr. Opin. Psychiatry 2012, 25, 457–461. [Google Scholar] [CrossRef] [PubMed]
- Neuvonen, E.; Lehtisalo, J.; Ngandu, T.; Levälahti, E.; Antikainen, R.; Hänninen, T.; Laatikainen, T.; Lindström, J.; Paajanen, T.; Soininen, H.; et al. Associations of Depressive Symptoms and Cognition in the FINGER Trial: A Secondary Analysis of a Randomised Clinical Trial. J. Clin. Med. 2022, 11, 1449. [Google Scholar] [CrossRef]
- Tzang, R.F.; Yang, A.C.; Yeh, H.L.; Liu, M.E.; Tsai, S.J. Association of depression and loneliness with specific cognitive performance in non-demented elderly males. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2015, 21, 100–104. [Google Scholar] [CrossRef]
- Xu, W.; Tan, L.; Wang, H.F.; Tan, M.S.; Tan, L.; Li, J.Q.; Zhao, Q.F.; Yu, J.T. Education and Risk of Dementia: Dose-Response Meta-Analysis of Prospective Cohort Studies. Mol. Neurobiol. 2016, 53, 3113–3123. [Google Scholar] [CrossRef]
- Lövdén, M.; Fratiglioni, L.; Glymour, M.M.; Lindenberger, U.; Tucker-Drob, E.M. Education and Cognitive Functioning Across the Life Span. Psychol. Sci. Public Interest A J. Am. Psychol. Soc. 2020, 21, 6–41. [Google Scholar] [CrossRef]
- Schwarz, R.; Gunzelmann, T.; Hinz, A.; Brähler, E. Angst und Depressivität in der über 60-jährigen Allgemeinbevölkerung [Anxiety and depression in the general population over 60 years old]. Dtsch. Med. Wochenschr. 2001, 126, 611–615. [Google Scholar] [CrossRef]
- Stek, M.L.; Gussekloo, J.; Beekman, A.T.; van Tilburg, W.; Westendorp, R.G. Prevalence, correlates and recognition of depression in the oldest old: The Leiden 85-plus study. J. Affect. Disord. 2004, 78, 193–200. [Google Scholar] [CrossRef] [PubMed]
| Absolute Number (n) | Relative Number (%) | ||
|---|---|---|---|
| No depression (GDS 0–5) | 956 | 94.1% | No Depressive Symptoms according to GDS-Score (GDS 0–5) |
| Light to moderate depressive symptoms (GDS 6–10) | 56 | 5.5% | Depressive Symptoms according to GDS-Score (GDS 6–15) |
| Severe depressive symptoms (GDS 11–15) | 4 | 0.4% | |
| Total | 1016 | 100.0% |
| Depressive Symptoms According to GDS-Score (n = 1016) | Subjective Cognitive Decline (n = 921) | All Participants (n = 1030) | ||||||
|---|---|---|---|---|---|---|---|---|
| Yes (n = 60) | No (n = 956) | p-Value | Yes (n = 320) | No (n = 601) | p-Value | |||
| Age | Median (IQR) [years] | 67.00 (10.00) | 69.00 (8.00) | 0.184 | 69.00 (9.00) | 69.00 (7.00) | 0.819 | 69.00 (8.00) |
| Sex | Male [n] | 27 (45.0%) | 457 (47.8%) | 0.673 | 152 (47.5%) | 293 (48.8%) | 0.717 | 493 (47.9%) |
| Female [n] | 33 (55.0%) | 499 (52.2%) | 168 (52.5%) | 308 (51.2%) | 537 (52.1%) | |||
| BMI | Median (IQR) [kg/m2] | 32.85 (6,50) | 30.50 (7.70) | 0.005 * | 30.60 (7.50) | 30.50 (7.70) | 0.652 | 30.40 (7.70) |
| Education group (CASMIN) | Low [n] | 21 (35.0%) | 224 (23.4%) | 0.022 * | 61 (19.0%) | 158 (26.3%) | 0.024 * | 251 (24.4%) |
| Medium [n] | 33 (55.0%) | 508 (53.2%) | 175 (54.7%) | 318 (52.9%) | 546 (53.0%) | |||
| High [n] | 6 (10.0%) | 224 (23.4%) | 84 (26.3%) | 125 (20.8%) | 233 (22.6%) | |||
| Lubben social network scale | Median (IQR) | 11.00 (7.00) | 18.00 (7.00) | <0.001 * | 17.00 (7.00) | 17.00 (8.00) | 0.513 | 17.00 (8.00) |
| Two times a week minimum of 30 min of sports | Yes [n] | 38 (64.4%) | 448 (46.9%) | <0.001 * | 144 (45.3%) | 296 (49.3%) | 0.408 | 489 (47.8%) |
| No [n] | 18 (30.5%) | 503 (52.6%) | 171 (53.8%) | 300 (49.9%) | 525 (51.3%) | |||
| Not specified [n] | 3 (5.1%) | 5 (0.5%) | 3 (0.9%) | 5 (0.8%) | 9 (0.9%) | |||
| Hypertension | No [n] | 9 (15.0%) | 118 (12.4%) | 0.676 | 46 (14.4%) | 66 (11.0%) | 0.140 | 128 (12.4%) |
| Yes [n] | 51 (85.0%) | 831 (86.9%) | 270 (84.4%) | 532 (88.5%) | 895 (86.9%) | |||
| Not specified [n] | - | 7 (0.7%) | 4 (1.2%) | 3 (0.5%) | 7 (0.7%) | |||
| MoCA-Score | Median (IQR) | 24.00 (7.00) | 25.00 (4.00) | 0.146 | 25.00 (4.00) | 25.00 (5.00) | 0.069 | 25.00 (4.00) |
| Sleeping problems | No [n] | 41 (68.3%) | 779 (81.5%) | 0.026 * | 241 (75.3%) | 509 (84.7%) | 0.002 * | 833 (80.9%) |
| Yes [n] | 19 (31.7%) | 171 (17.9%) | 76 (23.8%) | 90 (15.0%) | 191 (18.5%) | |||
| Not specified [n] | - | 6 (0.6%) | 3 (0.9%) | 2 (0.3%) | 6 (0.6%) | |||
| Daily alcohol consumption | Median (IQR) [g/day] | 0.00 (9.53) | 7.49 (18.26) | 0.173 | 7.49 (17.47) | 4.08 (17.47) | 0.472 | 7.49 (17.47) |
| Packyears | Median (IQR) [py] | 7.00 (30.00) | 2.00 (26.45) | 0.275 | 0.99 (24.25) | 3.60 (27.00) | 0.413 | 2.40 (26.50) |
| Subjective cognitive decline | No [n] | 20 (41.7%) | 578 (66.8%) | <0.001 * | - | 601 (65.3%) | ||
| Yes [n] | 28 (58.3%) | 287 (33.2%) | 320 (34.7%) | |||||
| Depressive symptoms according to GDS-Score | No [n] | - | 287 (91.1%) | 578 (96.7%) | <0.001 * | 956 (94.1%) | ||
| Yes [n] | 28 (8.9%) | 20 (3.3%) | 60 (5.9%) | |||||
| No MCI | MCI | Total | |
|---|---|---|---|
| No self-experienced memory problems | 601 (58.8%) | 13 (1.3%) | 614 (60.1%) |
| Self-experienced memory problems | 320 (31.3%) # | 88 (8.6%) | 408 (39.9%) |
| Total | 921 (90.1%) | 101 (9.9%) | 1022 (100.0%) |
| Subjective Cognitive Decline (n = 921) | ||
|---|---|---|
| OR (95% CI) | p-Value | |
| Age | 1.008 (0.979–1.038) | 0.584 |
| Sex (female) | 0.939 (0.701–1.257) | 0.670 |
| Sleeping problems * | 1.550 (1.080–2.225) | 0.017 * |
| GDS-Score * | 1.219 (1.127–1.318) | <0.001 * |
| Education group CASMIN (low) * | Reference group | 0.014 * |
| Education group CASMIN (medium) * | 1.474 (1.024–2–123) | 0.037 * |
| Education group CASMIN (high) * | 1.875 (1.224–2.872) | 0.004 * |
| Lubben social network scale | 1.023 (0.996–1.050) | 0.097 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zöllinger, I.; Bauer, A.; Blotenberg, I.; Brettschneider, C.; Buchholz, M.; Czock, D.; Döhring, J.; Escales, C.; Fankhaenel, T.; Frese, T.; et al. Associations of Depressive Symptoms with Subjective Cognitive Decline in Elderly People—A Cross-Sectional Analysis from the AgeWell.de-Study. J. Clin. Med. 2023, 12, 5205. https://doi.org/10.3390/jcm12165205
Zöllinger I, Bauer A, Blotenberg I, Brettschneider C, Buchholz M, Czock D, Döhring J, Escales C, Fankhaenel T, Frese T, et al. Associations of Depressive Symptoms with Subjective Cognitive Decline in Elderly People—A Cross-Sectional Analysis from the AgeWell.de-Study. Journal of Clinical Medicine. 2023; 12(16):5205. https://doi.org/10.3390/jcm12165205
Chicago/Turabian StyleZöllinger, Isabel, Alexander Bauer, Iris Blotenberg, Christian Brettschneider, Maresa Buchholz, David Czock, Juliane Döhring, Catharina Escales, Thomas Fankhaenel, Thomas Frese, and et al. 2023. "Associations of Depressive Symptoms with Subjective Cognitive Decline in Elderly People—A Cross-Sectional Analysis from the AgeWell.de-Study" Journal of Clinical Medicine 12, no. 16: 5205. https://doi.org/10.3390/jcm12165205
APA StyleZöllinger, I., Bauer, A., Blotenberg, I., Brettschneider, C., Buchholz, M., Czock, D., Döhring, J., Escales, C., Fankhaenel, T., Frese, T., Hoffmann, W., Kaduszkiewicz, H., König, H.-H., Luppa, M., Oey, A., Pabst, A., Sanftenberg, L., Thyrian, J. R., Weiss, J., ... Gensichen, J. (2023). Associations of Depressive Symptoms with Subjective Cognitive Decline in Elderly People—A Cross-Sectional Analysis from the AgeWell.de-Study. Journal of Clinical Medicine, 12(16), 5205. https://doi.org/10.3390/jcm12165205







