1. Introduction
The COVID-19 pandemic is a global health crisis and a great challenge to our health system, as well as to almost the whole population of the entire world [
1]. Postponements of surgeries, strict regulations on examinations and hospital stays, social distancing, insecurity in general, and numerous individual restrictions burdened a large part of the world’s population from 2019 to 2023. Originating in December 2019 in Wuhan (a city in Hubei Province, China), this virus quickly spread all around the world, affecting almost every country [
2]. The WHO (World Health Organization) declared the spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) to be a pandemic on 11 March 2020 [
2]. In addition, many healthcare workers were affected by changes in their work location. During the pandemic, most healthcare workers around the world were assigned to other departments or areas in hospitals or clinics to treat the high number of COVID-19 patients [
1]. This job insecurity during the COVID-19 pandemic caused many healthcare workers to experience stress [
3]. In addition, frontline (i.e., in direct contact with COVID-19 patients) workers in the health sector (WHS) seemed to experience even higher stress levels while working in hospitals during the pandemic [
3,
4,
5]. In addition to higher stress levels, direct contact with COVID-19 patients has a negative impact on anxiety [
6], depression, and insomnia [
7], and quality of life was reported to decrease due to these factors [
8]. Mental health problems were shown to be more pronounced in WHS due to working directly with infected patients [
9].
There have been a few studies focusing on productivity (the amount of work-related output, compared to the tasks at hand) and motivation during the COVID-19 pandemic [
10]. For example, in Italy, 51 administrative officers who moved to WFH at the beginning of the COVID-19 pandemic were asked to self-assess their productivity. The results of this study revealed a decrease in productivity in 39.2% and an increase in productivity in 29.4% of participants. The authors suggested that the decrease in productivity could be explained by the presence of distractions in the domestic environment and impaired interactions with colleagues. Workers who reported higher productivity might have had reduced stress and/or reduced communication times [
11]. The diversity of the abovementioned results indicates that self-assessed productivity varies not only between but also within the different sectors of work.
In addition to changing work location within the hospital, working from home (WFH) was also an opportunity for several WHS. In some countries, staff who were not involved in direct care were asked to WFH. Due to the global COVID-19 pandemic, WHS were at a substantially increased risk of becoming infected with SARS-CoV-2 [
1]. To prevent high spread of the infection, some WHS were given the opportunity to WFH, such as WHS who could provide telemedicine services from home or WHS who perform scientific work in addition to their clinical care. Reducing those risk factors and their negative consequences by changing the workplace to WFH offered new possibilities to both employees and employers in healthcare. In addition to new opportunities, the change of work location to WFH was also found to be a challenge for employees. For example, the perception of productivity, which displays how productive one feels in one’s current workplace, was found to be altered when compared to the productivity before the COVID-19 pandemic, depending on the field of work [
10]. A Japanese study investigated the productivity changes of four manufacturing companies during the shift to WFH. They found that workers who engaged in WFH experienced more declining productivity than those who did not work from home. They reported that the main reasons for the differences were poor WFH setups and communication difficulties [
12].
An American study found that, for those who had previously been working in offices and transitioned to WFH, the perception of productivity was shown to remain equal during the COVID-19 pandemic in comparison to the perception of productivity before the COVID-19 pandemic. Female, older, and high-income workers were likely to report increased productivity [
10]. Another American study found that employees perceived WFH as having a strong and positive impact on their productivity and creativity at work. Productivity and creativity are enhanced when individuals identify their work and their organizations with deeper meaning in their lives and yet are still able to maintain boundaries between work and the non-work aspects of their lives [
13]. By this interpretation, productivity is supported best when work is close but not too close [
13]. Furthermore, an Austrian study investigating WHS found that more WHS (30.2%: men, 27.4%; women, 33.0%) felt less productive throughout the COVID-19 pandemic when WFH, whereas 12.7% (men, 13.4%; women, 11.9%) of the WHS reported higher productivity. WHS reporting decreased productivity were more frequently younger. Participants with a higher educational status reported improved productivity more frequently than those with less education [
14]. Another finding in the healthcare system reported that younger WHS felt very little decrease in their productivity. About 60% of the participants strongly disagreed that WFH interfered with their ability to complete work-related tasks. Only 4.5% of the participants reported interferences due to the switch to WFH [
15]. Compared to that, the focus of a similar study was to find gender disparities among researchers in the field of natural sciences. Women’s self-reported first/corresponding author’s and coauthor’s article submissions decreased significantly between the two time periods; men’s productivity metrics did not change [
16]. This occupational group was researched the most regarding WFH.
Both perceptions of productivity and symptoms of depression are associated with demographic aspects like sex and age. For example, research suggests that females suffer slightly more from mental health problems like stress, depression, anxiety, and insomnia [
17]. Furthermore, research also suggests that females reported additional burdens in household work [
18]. This is in line with the abovementioned finding on academic female researchers, who were found to have published less than their male colleagues during the pandemic [
16]. Females also reported a substantial decrease in time devoted to research [
14]. Furthermore, research on age differences compared to self-assessed productivity of WFH workers appears to be relatively rare. Awada et al. [
10] found higher productivity levels among older workers. Mental health problems seemed to be less prevalent in older individuals in this context [
14,
19,
20]. Moreover, research suggests that job satisfaction decreased with increasing age in the COVID-19 pandemic [
21], which might have also decreased self-assessed productivity [
22].
The purpose of this study was to determine how the COVID-19 pandemic affected the subjective perceived productivity of healthcare workers over the entire pandemic period, as a function of gender and age. In addition, the impact of the work environment (i.e., home office and hospital work) and the impact of perceived productivity on symptoms of depression were examined. In the present study, we investigated whether the perception of productivity was linked with changes in symptoms of depression in WHS over the course of the COVID-19 pandemic. As the perception of productivity is impacted by the location of work and the changes due to the COVID-19 pandemic [
23,
24], the current study investigated whether the perception of productivity (lower vs. equal. vs. higher productivity than before the COVID-19 pandemic) differed between workplace locations (WFH vs. working in hospitals). We hypothesized that a change in the perception of productivity might have a negative effect on symptoms of depression. We hypothesized that these effects would be even more dominant over a longer period during the COVID-19 pandemic. Since longitudinal studies are rare for this topic, the present study also focuses on that aspect. According to the recent literature, we hypothesized that WFH would have a more negative impact on the perception of productivity than working in a hospital or comparable healthcare facilities. Furthermore, we hypothesized that the COVID-19 pandemic would have effects on the perceptions of productivity in WHS, depending on sex, age, and work environment. Moreover, we hypothesized that direct contact with COVID-19 patients at the hospital as a working environment would have a more pronounced impact on the perception of productivity than indirect contact with COVID-19 patients [
23].
Examining these issues could help in designing prevention strategies to maintain the productivity levels and mental wellbeing of those WHS who engage in WFH, especially since this work modality seems to be persisting beyond the COVID-19 pandemic and will be part of future work in the healthcare sector.
2. Materials and Methods
2.1. Sample Description
The methods of this study were based on an online survey (using limesurvey.org) that was sent out to WHS in different Austrian hospitals and comparable healthcare facilities, like foster homes or rehabilitation facilities, at three different points in time (t1, t2, and t3). We included all facilities in Austria, with the request to send the questionnaires internally to the employees who treat patients in a clinical setting and provide a multi-professional service (medical, nursing, physiotherapeutic, psychological, etc.). The participants were informed about the study via internal mailings from the works councils or clinical management. Participation in the online questionnaire was then voluntary. We included all participants between the ages of 18 and 70 who reported active employment at a healthcare facility. This study was conducted in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of the Medical University Graz (EK-number: 32 329 ex 19/20). The participation in our questionnaire was anonymous and voluntary. Thus, for the present research question, we could not compare the results for WHS who participated in the survey more than once. All participants consented to the anonymous use of the collected data for scientific research.
2.2. Study Design/Procedure
This present study was a longitudinal observational study. An online survey to investigate workers in the health sector during the COVID-19 pandemic was conducted. This study was part of a large-scale study on the impact of COVID-19 on the mental health of WHS. During the first measurement in April 2020, essential institutions like hospitals and other medical facilities remained open. Healthcare workers were offered the opportunity, if possible, to partially work from home. Non-essential shops and institutions were closed in March 2020. In the first complete lockdown in Austria, there were new rules introduced, e.g., social distancing, wearing masks, and limiting contact with people from other households. During the second measurement period in winter 2020/2021, the restrictions imposed by the government on the citizens were loosened. In the third measurement period (winter 2021/2022), Austria was in its fourth lockdown. Therefore, the present study includes estimations of productivity over two years of the COVID-19 pandemic.
2.3. Materials
Workers in the health sector were asked about relevant sociodemographic data and their perceptions of their productivity via an online survey, containing self-designed questions as well as standardized questionnaires. The online survey contained the following sociodemographic items: sex, age (categorized into age groups), occupation, working hours, number of night duties in a month for certain occupations (e.g., medical doctors), number of inhabitants in the place of residence (grouped in various number brackets), living situation, inner size of the domicile, outer size of the domicile, workplace, and direct or indirect contact with COVID-19 patients. Furthermore, we compared frontline WHS (i.e., those working directly with COVID-19 patients) and non-frontline WHS (no direct contact with COVID-19 patients). The standardized psychometric measures included the Anhedonia Scale [
25], Patient Health Questionnaire (PHQ-9; [
26], Resilience Scale (RS13, [
27]), and Pittsburgh Sleep Quality Index (PSQI; [
28]). The Anhedonia Scale has a Cronbach’s alpha of 0.91 and has been validated for patients with mental disorders such as depression [
25]. The RS13 has been validated by factorial analyses and has a Cronbach’s alpha of 0.85 [
27]. In addition, the PSQI has a Cronbach’s alpha of 0.83, and all of its components have been validated in multiple studies examining both healthy individuals and patients with mental disorders [
28].
For the present study, the PHQ-9 was used for the further analyses. The PHQ-9 contains 9 questions about symptoms of depression and is used to measure the severity of depressive symptoms through questions about suicidality, mood, cognition, appetite, and self-esteem. The PHQ-9 has been continuously validated by structural clinical interviews for diagnosis (such as the SCID: Structured Clinical Interview for DSM) and has a Cronbach’s alpha of 0.79 [
26].
Additionally, self-designed COVID-19-related questions (e.g., COVID-19-related fears and productivity) were created at the beginning of the pandemic in an eye-valid manner, as there were no comparative questionnaires available at that time. Please see
Table 1 for the relevant questions, translated into English. The questions in the online survey were conceptualized and presented in German for WHS in Austria.
We formulated two different questions: one about the productivity changes based on the workplace of the hospital, and the other based on the productivity changes due to WFH (see
Table 1). Both questions were rated on a three-point Likert scale (“less productive”, “equally productive”, and “more productive” = 1–3, respectively). For this study, only data from the sociodemographic questionnaire, the questions regarding perceptions of productivity, and the PHQ-9 were used.
2.4. Statistical Analysis
For descriptive purposes, nominal and ordinal variables were described in absolute and relative quantities. Differences in the self-assessed productivity based on the nominal variables sex, age, groups, and contact with COVID-19 patients, as well as workplace, were calculated with χ2 tests. A one-way analysis of covariance (ANCOVA) was performed to test the differences between groups of different self-assessed productivity (low vs. equal. vs. higher productivity) and the means of symptoms of depression as measured by the PHQ-9 (controlled for age and sex). The requirements for conducting an ANCOVA were met. Data were analyzed using IBM SPSS Statistics 29 (SPSS version 26.0, IBM, Armonk, NY, USA). All hypotheses were tested at a significance level of p < 0.05. For our one-way analysis of variance (ANOVA), we used the depression score from the PHQ-9, where we compared the means of the PHQ-9 results of the different productivity groups (lower, equal, and higher productivity).
4. Discussion
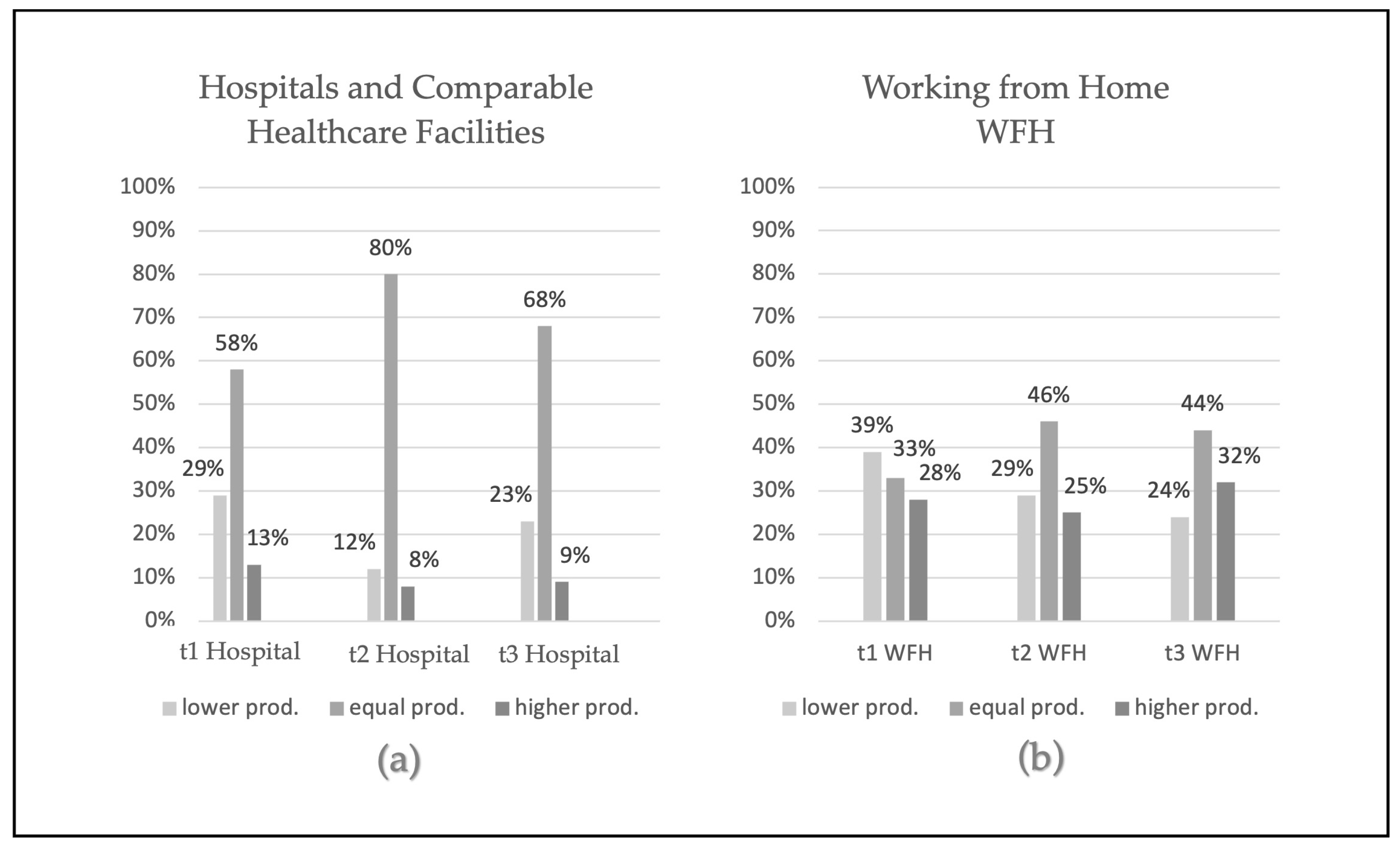
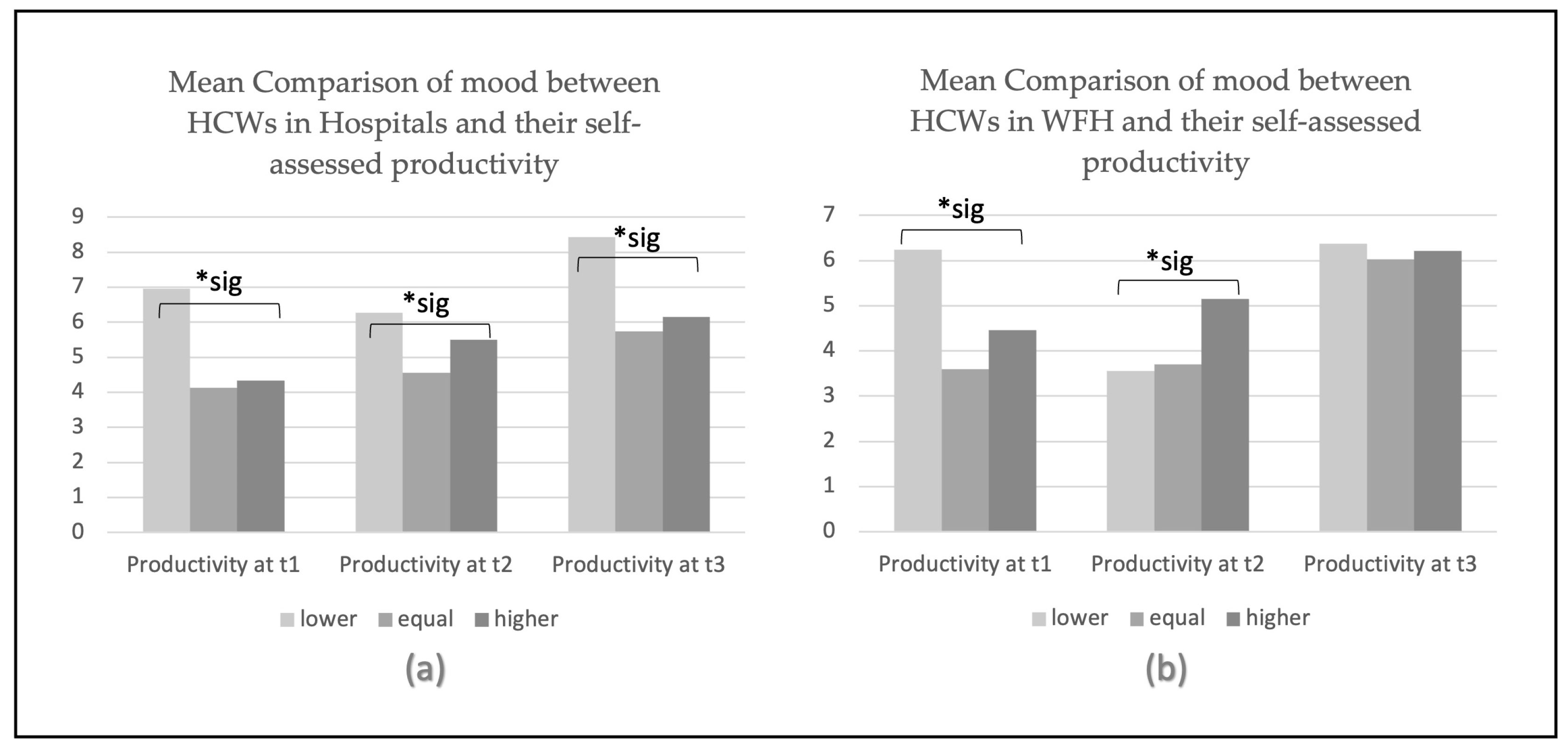
Our study focused on the differences in the perceptions of productivity in WHS working at a hospital or a comparable healthcare facility versus WHS in a WFH modus, resulting in significant differences between the two workplace modalities. In the present study, we additionally analyzed the differences in perceptions of productivity based on sex and age, but we could not find significant differences based on these factors. Furthermore, we investigated whether contact with COVID-19 patients had effects on the perception of productivity, finding no significant differences. Additionally, we looked at how changes in perceptions of productivity impacted the self-rating on the severity of depression symptoms, as measured by the PHQ-9, with significant outcomes revealing that most WHS who reported a decrease in their perception of productivity also reported the highest mean PHQ-9 depression scores, indicating that an increase in symptoms of depression is more prevalent in this category. It is already known that depression and anxiety were more pronounced in WHS during the COVID-19 pandemic and resulted in lower quality of life [
5,
6,
7,
8].
In addition, we hypothesized that WFH would have a more pronounced impact on the perception of productivity than working in a common workplace, e.g., a hospital or a comparable facility; this hypothesis was supported by the results of our study. This is in line with other research projects indicating that WHS engaging in WFH were more impacted by the pandemic and felt changes in their perceptions of productivity more often than WHS working in a hospital [
14].
We grouped our participants based on their perceptions of productivity, ranging from a decrease in the perception of productivity [
10,
15,
16], to mostly no changes [
10], and lastly to an increase in the perception of productivity [
1,
29], Overall, the data of workers who engaged in WFH do not point in just one direction [
13]. This supports our first hypothesis, which posited that the shift to WFH during the COVID-19 pandemic had a more pronounced impact on the perception of productivity. Possibly, changing working modalities like the workplace initiates distress that might affect the perception of productivity. Moreover, differences in environmental factors between these two modalities might have affected productivity. For example, parents with children at home could be distracted by their presence while working [
29]. In other cases, workers with increased perceptions of productivity also reported higher rates of creativity [
13]. Diving deeper into the causal mechanisms and further factors of these differences would be beneficial for both WHS and employers.
Assessing whether WFH could be beneficial, as well as to whom and under which circumstances, could have a significant impact on our work life in the decision of whether one might benefit from this change, especially since WFH might be relevant in the future of our work modalities. Further data and assessment would be needed to specifically determine which groups of workers would benefit the most from WFH, as well as how we can support workers who engage in WFH to feel more productive. Regarding our data, individuals who felt highly productive and were in the WFH group also experienced an increase in symptoms of depression in line with the three timepoints. One could speculate that individuals who feel more productive while WFH should be supported to have this opportunity.
The second hypothesis, which posited that the COVID-19 pandemic had effects on the perceptions of productivity among WHS, with a dependence on sex and age, showed significant results at the second measurement time in the hospital group. Perceptions of productivity in individuals WFH did not differ based on sex and age at any of the three measurement times. These results led to the conclusion that sex had no significant impact on the perception of productivity in our data. This was not consistent with other research suggesting that there are differences in perceptions of productivity based on sex [
16,
24], or age [
10]. Although current research shows differences between the sexes during the COVID-19 pandemic (e.g., a higher loss of productivity in female scientists [
16,
26] or a higher prevalence of mental health problems in females [
17], which might be partially connected to more additional burdens in household work [
18], our data did not show any significant differences between female and male WHS’s perceptions of productivity. The main purpose of this study was to find differences in the distribution of productivity between the sexes and age groups.
Thirdly, we theorized that direct contact with COVID-19 patients at the hospital as a working environment would have a bigger impact on the perception of productivity than indirect or no contact with COVID-19 patients. Contrary to our assumptions, there were no significant differences in perceptions of productivity between those in direct, indirect, or no contact with COVID-19 patients. This is consistent with recent research results indicating that direct contact with COVID-19 patients has effects on mental health, e.g., stress [
5], anxiety [
6], depression, insomnia [
7], and quality of life [
8]. Deteriorated mental health could, in turn, negatively influence one’s perception of productivity. The literature indeed indicates that contact with COVID-19 patients has an effect on mental health, but comparable studies investigating the perceptions of productivity among WHS working with COVID-19 patients are rare.
Finally, it was assumed that an improvement or decline in the perception of productivity would have a negative effect on symptoms of depression. The literature on the link between symptoms of depression and perceptions of productivity revealed a scarcity on this topic. Most studies investigated the link between general mental health and perceptions of productivity, reporting that worsening of the mental health status also increased the loss in perceptions of productivity [
4,
23]. As shown above, we observed that WHS working in the hospital who had an increased or decreased perceptions of productivity had worse PHQ-9 depression scores than WHS who described their productivity as being the same as it was before [
24]. The worst reported PHQ-9 depression score was at the third timepoint for WHS working in the hospital who self-assessed their productivity as lower than it was before the COVID-19 pandemic. These data suggest that WHS with an increased perception of productivity still reported higher depression scores than WHS who reported equal productivity at all three measurement times at the hospital. The lowest depression scores were found in WHS who reported an unchanged perception of productivity when working at a hospital or comparable healthcare facility at all three measurement times.
4.1. Limitations
The current study applied self-assessment questionnaires, which limits the objectivity of the impact of perceptions of productivity on objective measurements of productivity. Furthermore, it was sent out via an online survey, and the setting was not controllable. Furthermore, the distribution of the sexes in the questionnaire revealed a dominance of female WHS in this study, which might limit the generalizability of the current study. In addition, many healthcare workers changed their usual workplace at the beginning of the pandemic because healthcare was limited to essential treatments. This may have affected the comparison of productivity before and during COVID-19.
4.2. Implications
Researching the impacts of the COVID-19 pandemic on perceptions of productivity revealed differences in the perception of productivity between those working in a hospital as their usual workplace and those WFH due to the COVID-19 pandemic. Further research into the differences between these two working modalities and their benefits and downsides would be needed to broaden the knowledgebase of WFH to, on the one hand, be better prepared for similar pandemics that might occur in the future, and on the other hand, to explore new possibilities with this for many industries as a new working modality. Providing further research would be beneficial for the WHS as well as the employers. Assessing whether WFH could be beneficial, and to whom and under which circumstances, could have a big impact on our work life. The shift to WFH alters communication with other colleagues, changes the financial structures of workplaces and, thus, affects the mental health of WHS. Productivity gains from WFH would, of course, also prompt employers to consider home office options if the results of a related study confirm the benefits of WFH.