Response to Immunization against SARS-CoV-2 and Risk of Omicron Infection in Dialysis Patients: A Prospective Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
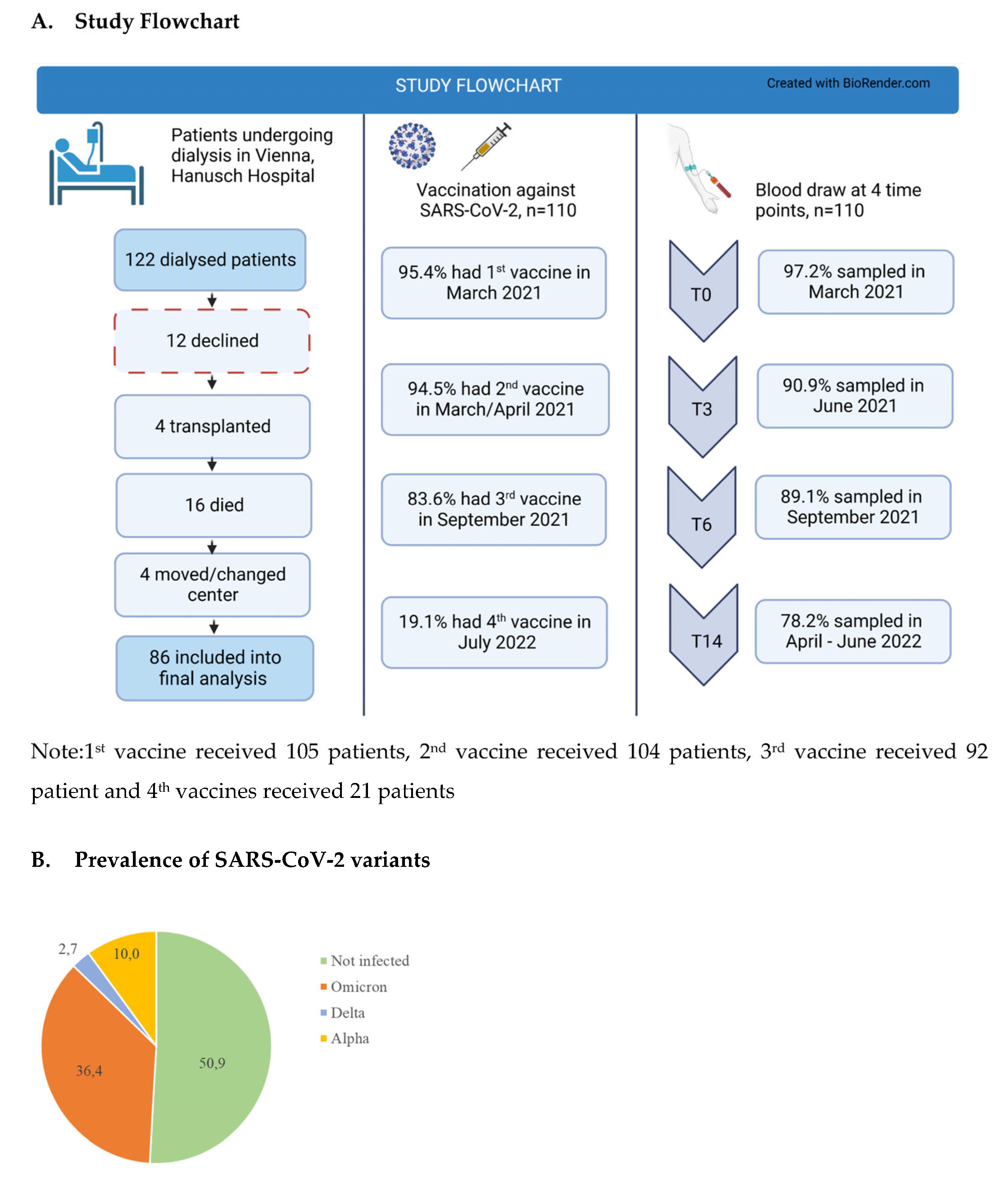
2.1. Study Design
2.2. Study Size
2.3. Cell Lines and Viruses
2.4. Chemiluminescent Microparticle Immunoassay (CMIA)
2.5. Interferon-γ Release Assay (IGRA)
2.6. Virus Neutralization Test
2.7. Statistical Methods
3. Results
3.1. Patient Characteristics
3.2. Antibody Titer over Time
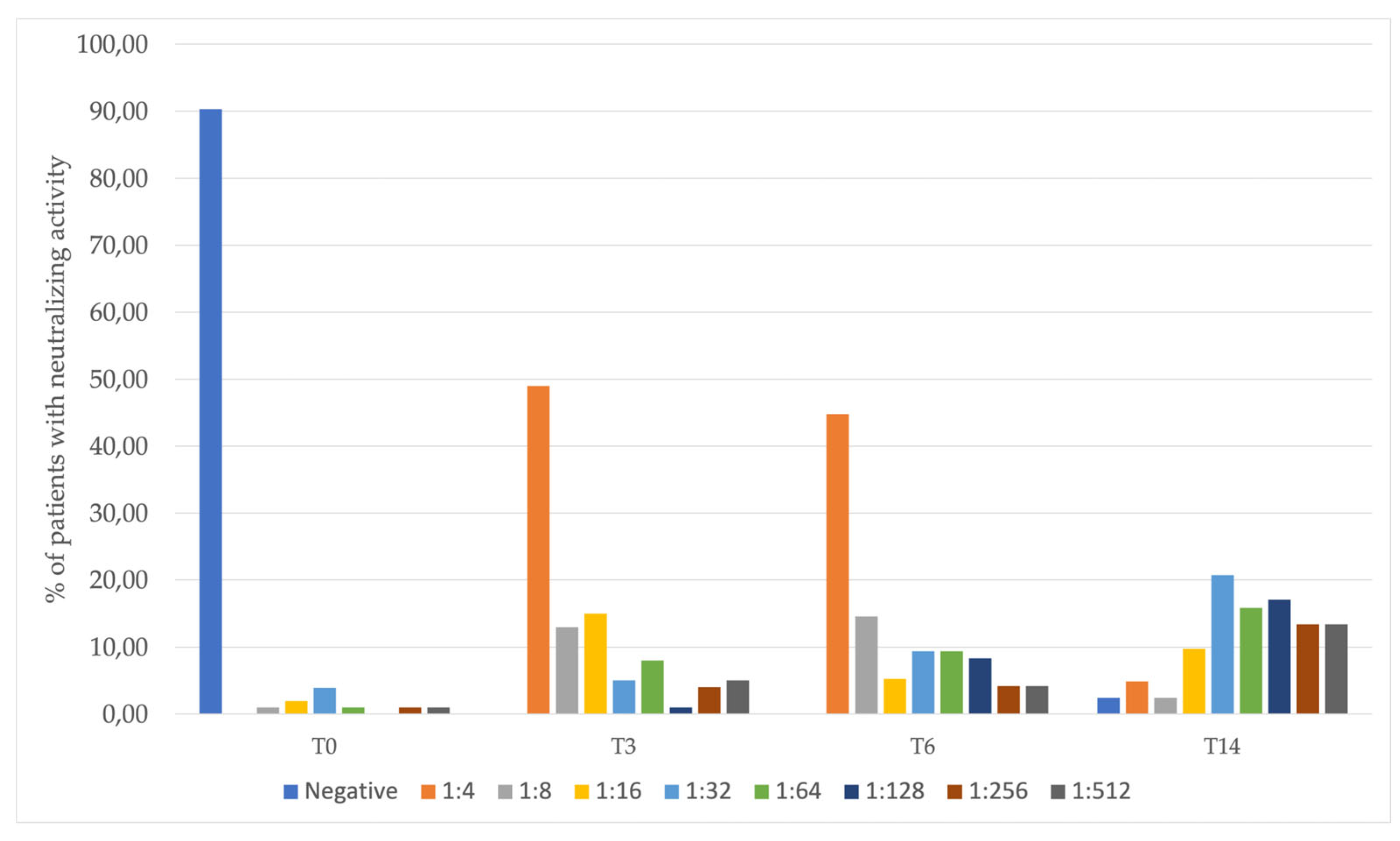
3.3. Validity of Antibody Tests and Titers
3.4. Differences in Antibody Levels over Time
3.5. Difference in the Prevalence of an Omicron Infection by Selected Risk Factors
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Liu, J.; Wei, H.; He, D. Differences in case-fatality-rate of emerging SARS-CoV-2 variants. Public Health Pr. 2023, 5, 100350. [Google Scholar] [CrossRef]
- Jager, K.J.; Kramer, A.; Chesnaye, N.C.; Couchoud, C.; Sanchez-Alvarez, J.E.; Garneata, L.; Collart, F.; Hemmelder, M.H.; Ambuhl, P.; Kerschbaum, J.; et al. Results from the ERA-EDTA Registry indicate a high mortality due to COVID-19 in dialysis patients and kidney transplant recipients across Europe. Kidney Int. 2020, 98, 1540–1548. [Google Scholar] [CrossRef] [PubMed]
- Simon, B.; Rubey, H.; Treipl, A.; Gromann, M.; Hemedi, B.; Zehetmayer, S.; Kirsch, B. Haemodialysis patients show a highly diminished antibody response after COVID-19 mRNA vaccination compared to healthy controls. Nephrol. Dial. Transpl. 2021, 36, 1709–1716. [Google Scholar] [CrossRef]
- Hilbrands, L.B.; Duivenvoorden, R.; Vart, P.; Franssen, C.F.M.; Hemmelder, M.H.; Jager, K.J.; Kieneker, L.M.; Noordzij, M.; Pena, M.J.; Vries, H.; et al. COVID-19-related mortality in kidney transplant and dialysis patients: Results of the ERACODA collaboration. Nephrol. Dial. Transpl. 2020, 35, 1973–1983. [Google Scholar] [CrossRef]
- Sigal, A.; Milo, R.; Jassat, W. Estimating disease severity of Omicron and Delta SARS-CoV-2 infections. Nat. Rev. 2022, 22, 267–269. [Google Scholar] [CrossRef]
- Chow, K.M.; Chan, J.Y.H.; Wong, S.S.H.; Yuen, S.K.; Wong, P.N.; Cheng, Y.L.; Szeto, C.C. Impact of COVID-19 on the mortality of dialysis patients and kidney transplant recipients during the Omicron fifth wave in Hong Kong. Hong Kong Med. J. 2023, 29, 82–83. [Google Scholar] [CrossRef] [PubMed]
- Solante, R.; Alvarez-Moreno, C.; Burhan, E.; Chariyalertsak, S.; Chiu, N.C.; Chuenkitmongkol, S.; Dung, D.V.; Hwang, K.P.; Ortiz Ibarra, J.; Kiertiburanakul, S.; et al. Expert review of global real-world data on COVID-19 vaccine booster effectiveness and safety during the omicron-dominant phase of the pandemic. Expert Rev. Vaccines 2023, 22, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef] [PubMed]
- AGES. Monitoring of SARS-CoV-2 Variants in Austria; AGES: Vienna, Austria, 2023. [Google Scholar]
- Hoffmann, M.; Kleine-Weber, H.; Schroeder, S.; Kruger, N.; Herrler, T.; Erichsen, S.; Schiergens, T.S.; Herrler, G.; Wu, N.H.; Nitsche, A.; et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell 2020, 181, 271–280.e8. [Google Scholar] [CrossRef]
- Reed, L.J.; Muench, H.A. A simple method of estimating fiftypercent endpoints. Am. J. Hyg. 1938, 27, 493–497. [Google Scholar]
- Zimmermann, P.; Curtis, N. Factors That Influence the Immune Response to Vaccination. Clin. Microbiol. Rev. 2019, 32, e00084-18. [Google Scholar] [CrossRef] [Green Version]
- Kato, S.; Chmielewski, M.; Honda, H.; Pecoits-Filho, R.; Matsuo, S.; Yuzawa, Y.; Tranaeus, A.; Stenvinkel, P.; Lindholm, B. Aspects of Immune Dysfunction in End-stage Renal Disease. Clin. J. Am. Soc. Nephrol. 2008, 3, 1526–1533. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kausz, A.; Pahari, D. The value of vaccination in chronic kidney disease. Semin. Dial. 2004, 17, 9–11. [Google Scholar] [CrossRef]
- Zitt, E.; Hafner-Giessauf, H.; Wimmer, B.; Herr, A.; Horn, S.; Friedl, C.; Sprenger-Mähr, H.; Kramar, R.; Rosenkranz, A.R.; Lhotta, K. Response to active hepatitis B vaccination and mortality in incident dialysis patients. Vaccine 2017, 35, 814–820. [Google Scholar] [CrossRef]
- Mavrovouniotis, I.; Fylaktou, A.; Stagou, M.; Ouranos, K.; Lioulios, G.; Evgenikaki, E.; Exindari, M.; Gioula, G. Cellular and Humoral Responses in Dialysis Patients after Vaccination with the BNT162b2 or mRNA-1273 Vaccines. Life 2023, 13, 474. [Google Scholar] [CrossRef]
- Kohmer, N.; Rabenau, H.F.; Ciesek, S.; Krämer, B.K.; Göttmann, U.; Keller, C.; Rose, D.; Blume, C.; Thomas, M.; Lammert, A.; et al. Heterologous immunization with BNT162b2 followed by mRNA-1273 in dialysis patients: Seroconversion and presence of neutralizing antibodies. Nephrol. Dial. Transpl. 2022, 37, 1132–1139. [Google Scholar] [CrossRef] [PubMed]
- Simon, B.; Rubey, H.; Gromann, M.; Knopf-Völkerer, A.; Hemedi, B.; Zehetmayer, S.; Kirsch, B. SARS-CoV-2 Antibody and T Cell Response after a Third Vaccine Dose in Hemodialysis Patients Compared with Healthy Controls. Vaccines 2022, 10, 694. [Google Scholar] [CrossRef] [PubMed]
- Melin, J.; Svensson, M.K.; Albinsson, B.; Winqvist, O.; Pauksens, K. A third dose SARS-CoV-2 BNT162b2 mRNA vaccine results in improved immune response in hemodialysis patients. Ups. J. Med. Sci. 2022, 127. [Google Scholar] [CrossRef]
- Dulovic, A.; Strengert, M.; Ramos, G.M.; Becker, M.; Griesbaum, J.; Junker, D.; Lürken, K.; Beigel, A.; Wrenger, E.; Lonnemann, G.; et al. Diminishing Immune Responses against Variants of Concern in Dialysis Patients 4 Months after SARS-CoV-2 mRNA Vaccination. Emerg. Infect Dis. 2022, 28, 743–750. [Google Scholar] [CrossRef]
- Schrezenmeier, E.; Bergfeld, L.; Hillus, D.; Lippert, J.D.; Weber, U.; Tober-Lau, P.; Landgraf, I.; Schwarz, T.; Kappert, K.; Stefanski, A.L.; et al. Immunogenicity of COVID-19 Tozinameran Vaccination in Patients on Chronic Dialysis. Front. Immunol. 2021, 12, 690698. [Google Scholar] [CrossRef]
- Strengert, M.; Becker, M.; Ramos, G.M.; Dulovic, A.; Gruber, J.; Juengling, J.; Lürken, K.; Beigel, A.; Wrenger, E.; Lonnemann, G.; et al. Cellular and humoral immunogenicity of a SARS-CoV-2 mRNA vaccine in patients on haemodialysis. EBioMedicine 2021, 70, 103524. [Google Scholar] [CrossRef] [PubMed]
- Becker, M.; Cossmann, A.; Lürken, K.; Junker, D.; Gruber, J.; Juengling, J.; Ramos, G.M.; Beigel, A.; Wrenger, E.; Lonnemann, G.; et al. Longitudinal cellular and humoral immune responses after triple BNT162b2 and fourth full-dose mRNA-1273 vaccination in haemodialysis patients. Front. Immunol. 2022, 13, 1004045. [Google Scholar] [CrossRef] [PubMed]
- Jahn, M.; Korth, J.; Dorsch, O.; Anastasiou, O.E.; Krawczyk, A.; Brochhagen, L.; van de Sand, L.; Sorge-Hadicke, B.; Tyczynski, B.; Witzke, O.; et al. Decline of Humoral Responses 6 Months after Vaccination with BNT162b2 (Pfizer-BioNTech) in Patients on Hemodialysis. Vaccines 2022, 10, 327. [Google Scholar] [CrossRef] [PubMed]
- Agur, T.; Zingerman, B.; Ben-Dor, N.; Alkeesh, W.; Steinmetz, T.; Rachamimov, R.; Korzets, A.; Rozen-Zvi, B.; Herman-Edelstein, M. Humoral Response to the Third Dose of BNT162b2 COVID-19 Vaccine among Hemodialysis Patients. Nephron 2023, 147, 185–192. [Google Scholar] [CrossRef] [PubMed]
- Verdier, J.-F.; Boyer, S.; Chalmin, F.; Jeribi, A.; Egasse, C.; Maggi, M.F.; Auvray, P.; Yalaoui, T. Response to three doses of the Pfizer/BioNTech BNT162b2 COVID-19 vaccine: A retrospective study of a cohort of haemodialysis patients in France. BMC Nephrol. 2022, 23, 189. [Google Scholar] [CrossRef]
- Bichara, C.D.A.; da Silva Graca Amoras, E.; Vaz, G.L.; da Silva Torres, M.K.; Queiroz, M.A.F.; do Amaral, I.P.C.; Vallinoto, I.; Bichara, C.N.C.; Vallinoto, A.C.R. Dynamics of anti-SARS-CoV-2 IgG antibodies post-COVID-19 in a Brazilian Amazon population. BMC Infect. Dis. 2021, 21, 443. [Google Scholar] [CrossRef]
- Karakizlis, H.; Nahrgang, C.; Strecker, K.; Chen, J.; Aly, M.; Slanina, H.; Schüttler, C.G.; Esso, I.; Wolter, M.; Todorova, D.; et al. Data on immunogenicity and reactogenicity to COVID-19 vaccination among patients receiving maintenance dialysis. Data Brief 2022, 42, 108271. [Google Scholar] [CrossRef]
- Pajon, R.; Doria-Rose, N.A.; Shen, X.; Schmidt, S.D.; O’Dell, S.; McDanal, C.; Feng, W.; Tong, J.; Eaton, A.; Maglinao, M.; et al. SARS-CoV-2 Omicron Variant Neutralization after mRNA-1273 Booster Vaccination. N. Engl. J. Med. 2022, 386, 1088–1091. [Google Scholar] [CrossRef]
- Paul, P.; El-Naas, A.; Hamad, O.; Salameh, M.A.; Mhaimeed, N.; Laswi, I.; Abdelati, A.A.; AlAnni, J.; Khanjar, B.; Al-Ali, D.; et al. Effectiveness of the pre-Omicron COVID-19 vaccines against Omicron in reducing infection, hospitalization, severity, and mortality compared to Delta and other variants: A systematic review. Hum. Vaccin. Immunother. 2023, 19, 2167410. [Google Scholar] [CrossRef]
- Wing, S.; Thomas, D.; Balamchi, S.; Ip, J.; Naylor, K.; Dixon, S.N.; McArthur, E.; Kwong, J.C.; Perl, J.; Atiquzzaman, M.; et al. Effectiveness of Three Doses of mRNA COVID-19 Vaccines in the Hemodialysis Population during the Omicron Period. Clin. J. Am. Soc. Nephrol. 2023, 18, 491–498. [Google Scholar] [CrossRef]
- Montez-Rath, M.E.; Garcia, P.; Han, J.; Cadden, L.; Hunsader, P.; Morgan, C.; Kerschmann, R.; Beyer, P.; Dittrich, M.; Block, G.A.; et al. SARS-CoV-2 Infection during the Omicron Surge among Patients Receiving Dialysis: The Role of Circulating Receptor-Binding Domain Antibodies and Vaccine Doses. J. Am. Soc. Nephrol. 2022, 33, 1832–1839. [Google Scholar] [CrossRef] [PubMed]
- Chinnadurai, R.; Wu, H.H.L.; Cox, E.; Moore, J.; Clough, T.; Lamerton, E.; Donne, R.; O’Riordan, E.; Poulikakos, D. Humoral Response in Hemodialysis Patients Following COVID-19 Vaccination and Breakthrough Infections during Delta and Omicron Variant Predominance. Vaccines 2022, 10, 498. [Google Scholar] [CrossRef] [PubMed]
- Patnaik, A.P.; Rout, N.K.; Ahmed, S.; Dash, K.A.; Praharaj, A.K.; Patro, A.R.K. Correlation of Breakthrough Infection During the Omicron Wave With Seropositivity of Vaccinated Patients Undergoing Hemodialysis. Cureus 2022, 14, e29296. [Google Scholar] [CrossRef] [PubMed]


| Readout | Unit | |
|---|---|---|
| RT-PCR | Presence of viral particles in upper respiratory tract | Positive or negative |
| CMIA | Levels of anti-SARS-CoV IgG | BAU/mL |
| Neutralization test | Virus-neutralizing activity of antibodies | Titer |
| IGRA | Interferon-γ release in response to virus (“cellular response”) | IU/mL |
| Missing Values, n (%) | ||
|---|---|---|
| Age, Mean (SD) | 68.4 (13.7) | |
| Sex, n (%) | ||
| Male | 67 (60.9) | |
| Female | 43 (39.1) | |
| BMI category, n (%) | 9 (8.2) | |
| Underweight | 1 (0.9) | |
| Normal | 37 (33.6) | |
| Overweight | 37 (33.6) | |
| Obesity | 26 (23.6) | |
| Smoking status, n (%) | 7 (6.4) | |
| Current smoker | 21 (19.1) | |
| Ex-smoker | 29 (26.4) | |
| Non-smoker | 53 (48.2) | |
| Diabetes mellitus, n (%) | 4 (3.6) | |
| Yes | 50 (45.5) | |
| No | 56 (50.9) | |
| Charlson Comorbidity Index, Mean (SD) | 6.9 (2.5) | |
| CKD origin, n (%) | ||
| Tubulointerstitial | 2 (1.8) | |
| Glomerular disease | 22 (20.0) | |
| Hereditary nephropathy | 7 (6.4) | |
| Hypertension | 17 (15.5) | |
| Diabetes mellitus | 15 (13.6) | |
| Other systematic disease | 3 (2.7) | |
| Miscellaneous renal disease | 4 (3.6) | |
| Unknown | 40 (36.4) | |
| Dialysis frequency, n (%) | ||
| Once a week | 1 (0.9) | |
| Twice a week | 18 (16.4) | |
| Three times a week | 86 (78.2) | |
| Peritoneal dialysis | 5 (4.5) | |
| History of kidney transplant, n (%) | ||
| Yes | 12 (10.9) | |
| No | 98 (89.1) | |
| Current immunosuppressive therapy, n (%) | ||
| Yes | 10 (9.1) | |
| No | 100 (90.9) | |
| Vaccination doses against SARS-CoV-2, n (%) | ||
| 0 | 5 (4.5) | |
| 1 | 1 (0.9) | |
| 2 | 12 (10.9) | |
| 3 | 71 (64.5) | |
| 4 or more | 21 (19.1) | |
| First infection with SARS-CoV-2, n (%) | 54 (49.1) | |
| Severity of first infection | 1 (1.9) | |
| Mild | 39 (72.2) | |
| Severe | 11 (20.4) | |
| Death | 3 (5.6) | |
| Second infection with SARS-CoV-2, n (%) | 5 (4.5) | |
| Severity of second infection | ||
| Mild | 5 (100) | |
| Severe | 0 (0) | |
| Death | 0 (0) | |
| Infected during Omicron wave, n (%) | 40 (36.4) | |
| Positive neutralization test n (%) | ||
| T0 | 10 (9.1) | 7 (6.4) |
| T3 | 54 (49.1) | 20 (18.2) |
| T6 | 56 (50.9) | 25 (22.7) |
| T14 | 77 (70.0) | 29 (26.4) |
| Parameter | Estimate | SE | df | t | p-Value | 95% Confidence Interval | ||
|---|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | |||||||
| Intercept | 3149.2 | 321.5 | 84.8 | 9.8 | <0.001 | 2509.9 | 3788.5 | |
| T0 | −3145.7 | 315.8 | 82.8 | −10.0 | <0.001 | −3773.8 | −2517.7 | |
| T3 | −2879.4 | 329.6 | 90.6 | −8.7 | <0.001 | −3534.2 | −2224.6 | |
| T6 | −2889.0 | 297.5 | 83.1 | −9.7 | <0.001 | −3480.6 | −2297.4 | |
| T14 | Ref. | |||||||
| No Omicron event | −1571.7 | 424.8 | 86.1 | −3.7 | <0.001 | −2416.1 | −727.2 | |
| Omicron event | Ref. | |||||||
| T0 * No Omicron event | 1679.4 | 417.6 | 83.7 | 4.0 | <0.001 | 848.9 | 2509.8 | |
| T3 * No Omicron event | 2001.7 | 435.4 | 91.7 | 4.6 | <0.001 | 1136.9 | 2866.5 | |
| T6 * No Omicron event | 1825.4 | 394.5 | 83.8 | 4.6 | <0.001 | 1040.8 | 2609.9 | |
| 95% Confidence Interval for Difference | ||||||||
| Time | Mean Difference (I-J) | SE | df | p-value | Lower Bound | Upper Bound | ||
| T0 | T3 | −427.5 | 117.1 | 91.2 | 0.000 | −660.1 | −194.9 | |
| T6 | −329.8 | 119.2 | 104.4 | 0.007 | −566.1 | −93.4 | ||
| T14 | −2306.0 | 208.8 | 83.7 | 0.000 | −2721.3 | −1890.8 | ||
| T3 | T6 | 97.7 | 98.7 | 89.09 | 0.325 | −98.3 | 293.8 | |
| T14 | −1878.5 | 217.7 | 91.7 | <0.001 | −2310.9 | −1446.1 | ||
| T6 | T14 | −1976.3 | 197.2 | 83.8 | <0.001 | −2368.5 | −1584.0 | |
| Time by Omicron infection | Mean values of Abbott | SE | df | 95% Confidence Interval | ||||
| Lower Bound | Upper Bound | |||||||
| T0 | not infected | 111.2 | 59.2 | 104.9 | −6.2 | 228.6 | ||
| infected | 3.5 | 78.5 | 105.7 | −152.1 | 159.1 | |||
| T3 | not infected | 699.8 | 142.5 | 89.4 | 416.7 | 982.9 | ||
| infected | 269.8 | 175.2 | 88.4 | −78.4 | 618.0 | |||
| T6 | not infected | 513.9 | 138.8 | 102.0 | 238.7 | 789.2 | ||
| infected | 260.2 | 167.9 | 99.1 | −72.9 | 593.3 | |||
| T14 | not infected | 1577.5 | 277.6 | 87.6 | 1025.8 | 2129.3 | ||
| infected | 3149.2 | 321.5 | 84.8 | 2509.9 | 3788.5 | |||
| Parameter | Estimate | SE | df | t | p-Value | 95% Confidence Interval | ||
|---|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | |||||||
| Intercept | 0.71 | 0.27 | 99.45 | 2.67 | 0.01 | 0.18 | 1.24 | |
| T0 | −0.67 | 0.24 | 97.61 | −2.81 | 0.01 | −1.14 | −0.20 | |
| T3 | −0.37 | 0.20 | 88.71 | −1.84 | 0.07 | −0.77 | 0.03 | |
| T6 | −0.52 | 0.17 | 82.66 | −3.13 | 0.00 | −0.85 | −0.19 | |
| T14 | Ref. | |||||||
| No Omicron event | 0.25 | 0.35 | 103.69 | 0.71 | 0.48 | −0.44 | 0.93 | |
| Omicron event | Ref. | |||||||
| T0 * No Omicron event | −0.09 | 0.31 | 99.74 | −0.29 | 0.77 | −0.71 | 0.53 | |
| T3 * No Omicron event | 0.04 | 0.27 | 90.46 | 0.14 | 0.89 | −0.49 | 0.56 | |
| T6 * No Omicron event | 0.17 | 0.22 | 84.61 | 0.77 | 0.45 | −0.27 | 0.61 | |
| 95% Confidence Interval for Difference | ||||||||
| Time | Mean Difference (I-J) | SE | df | p-value | Lower Bound | Upper Bound | ||
| T0 | T3 | −0.36 | 0.14 | 101.3 | 0.013 | −0.64 | −0.08 | |
| T6 | −0.28 | 0.12 | 103.6 | 0.029 | −0.53 | −0.03 | ||
| T14 | −0.71 | 0.16 | 99.74 | <0.001 | −1.02 | −0.41 | ||
| T3 | T6 | 0.08 | 0.07 | 91.76 | 0.219 | −0.05 | 0.22 | |
| T14 | −0.35 | 0.13 | 90.46 | 0.009 | −0.62 | −0.09 | ||
| T6 | T14 | −0.44 | 0.11 | 84.61 | <0.001 | −0.66 | −0.22 | |
| Time by Omicron infection | Mean values of QuantiFERON Ag1 | SE | df | 95% Confidence Interval | ||||
| Lower Bound | Upper Bound | |||||||
| T0 | not infected | 0.20 | 0.11 | 105.72 | −0.02 | 0.42 | ||
| infected | 0.04 | 0.14 | 107.52 | −0.24 | 0.33 | |||
| T3 | not infected | 0.63 | 0.18 | 103.01 | 0.27 | 0.98 | ||
| infected | 0.34 | 0.22 | 102.6 | −0.10 | 0.79 | |||
| T6 | not infected | 0.61 | 0.16 | 105.26 | 0.30 | 0.92 | ||
| infected | 0.19 | 0.19 | 100.78 | −0.19 | 0.57 | |||
| T14 | not infected | 0.96 | 0.22 | 109.71 | 0.52 | 1.40 | ||
| Infected | 0.71 | 0.27 | 99.45 | 0.18 | 1.24 | |||
| Variable | Prevalence of Omicron Infection | p-Value | |
|---|---|---|---|
| Sex | Male | 45.5% (30/66) | 0.03 |
| Female | 24.4% (10/41) | ||
| Smoking | Never smoker | 37.7% (20/53) | 0.92 |
| Current or ex-smoker | 36.7 (18/49) | ||
| Diabetes mellitus | No | 40.0% (22/55) | 0.48 |
| Yes | 33.3% (16/48) | ||
| Glucocorticoid | No | 36.4% (36/99) | 0.44 |
| Yes | 50.0% (4/8) | ||
| Immunosuppressive therapy | No | 37.8% (37/98) | 0.79 |
| Yes | 33.3% (3/9) | ||
| Kidney transplant | No | 40.0% (38/95) | 0.11 |
| Yes | 16.7% (2/12) | ||
| Age a | 0.71 | ||
| Charlson Comorbidity Index b | 0.10 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Werzowa, J.; Behanova, M.; Handisurya, A.; Heger, F.; Indra, A.; Holzer, B.; Dechat, T.; Spitzer, S.; Lederer, S.; Kraus, D.A.; et al. Response to Immunization against SARS-CoV-2 and Risk of Omicron Infection in Dialysis Patients: A Prospective Cohort Study. J. Clin. Med. 2023, 12, 4983. https://doi.org/10.3390/jcm12154983
Werzowa J, Behanova M, Handisurya A, Heger F, Indra A, Holzer B, Dechat T, Spitzer S, Lederer S, Kraus DA, et al. Response to Immunization against SARS-CoV-2 and Risk of Omicron Infection in Dialysis Patients: A Prospective Cohort Study. Journal of Clinical Medicine. 2023; 12(15):4983. https://doi.org/10.3390/jcm12154983
Chicago/Turabian StyleWerzowa, Johannes, Martina Behanova, Ammon Handisurya, Florian Heger, Alexander Indra, Barbara Holzer, Thomas Dechat, Silvia Spitzer, Sandra Lederer, Daniel A. Kraus, and et al. 2023. "Response to Immunization against SARS-CoV-2 and Risk of Omicron Infection in Dialysis Patients: A Prospective Cohort Study" Journal of Clinical Medicine 12, no. 15: 4983. https://doi.org/10.3390/jcm12154983
APA StyleWerzowa, J., Behanova, M., Handisurya, A., Heger, F., Indra, A., Holzer, B., Dechat, T., Spitzer, S., Lederer, S., Kraus, D. A., Zwerina, J., & Fritsch-Stork, R. D. E. (2023). Response to Immunization against SARS-CoV-2 and Risk of Omicron Infection in Dialysis Patients: A Prospective Cohort Study. Journal of Clinical Medicine, 12(15), 4983. https://doi.org/10.3390/jcm12154983






