Pain Management and Functional Recovery after Pericapsular Nerve Group (PENG) Block for Total Hip Arthroplasty: A Prospective, Randomized, Double-Blinded Clinical Trial
Abstract
1. Introduction
2. Patients and Methods
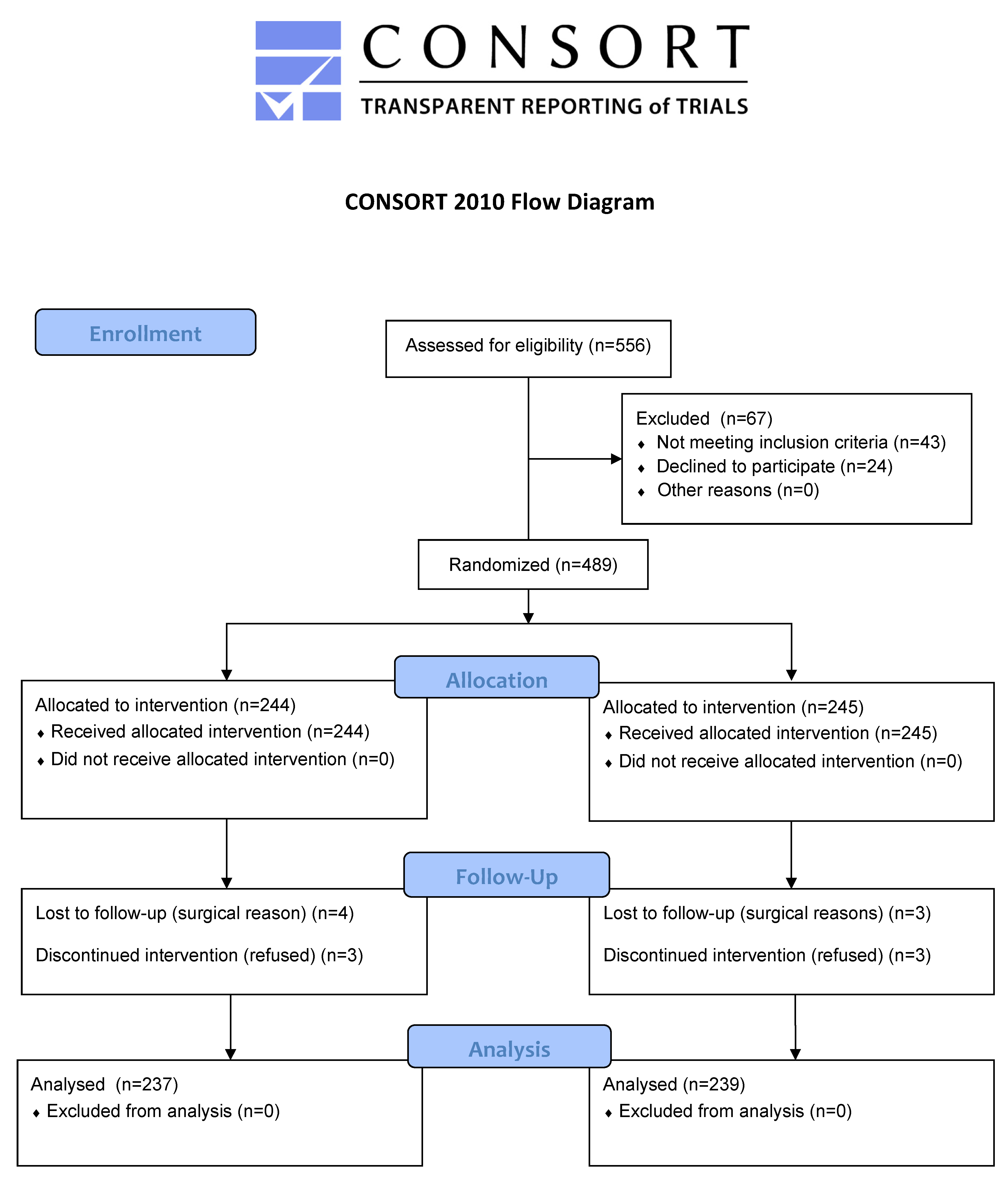
2.1. Study Design and Participants
2.2. Randomization
2.3. Perioperative Management and Spinal Anesthesia Procedure
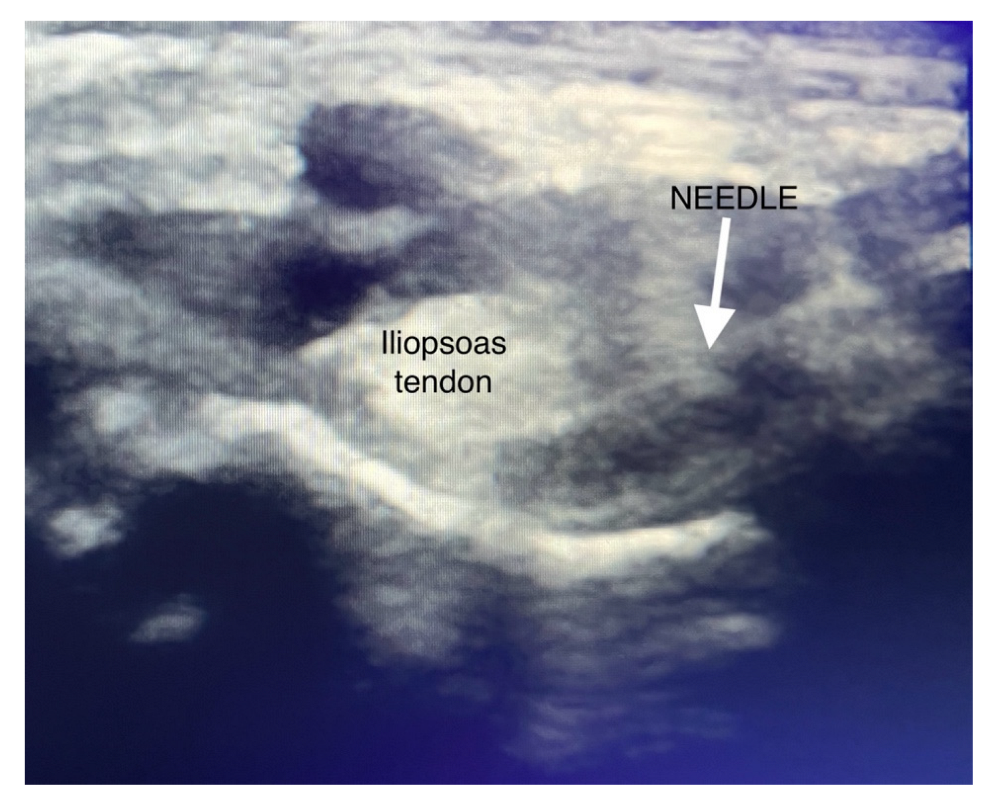
2.4. PENG Block Procedure
2.5. Postoperative Analgesia Management and Evaluation of Outcomes
2.6. Outcome Assessments
2.7. Statistical Analyses and Sample Size Calculation
3. Results
Patients and Operation Characteristics
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fontalis, A.; Epinette, J.-A.; Thaler, M.; Zagra, L.; Khanduja, V.; Haddad, F.S. Advances and innovations in total hip arthroplasty. SICOT-J 2021, 7, 26. [Google Scholar] [CrossRef] [PubMed]
- Surace, P.; Sultan, A.A.; George, J.; Samuel, L.T.; Khlopas, A.; Molloy, R.M.; Stearns, K.L.; Mont, M.A. The association between operative time and short-term complications in total hip arthroplasty: An analysis of 89,802 surgeries. J. Arthroplast. 2019, 34, 426–432. [Google Scholar] [CrossRef] [PubMed]
- Wu, V.J.; Ross, B.J.; Sanchez, F.L.; Billings, C.R.; Sherman, W.F. Complications following total hip arthroplasty: A nationwide database study comparing elective vs hip fracture cases. J. Arthroplast. 2020, 35, 2144–2148. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Davis, S.P. An integrative review of multimodal pain management on patient recovery after total hip and knee arthroplasty. Int. J. Nurs. Stud. 2019, 98, 94–106. [Google Scholar] [CrossRef]
- Laigaard, J.; Pedersen, C.; Rønsbo, T.N.; Mathiesen, O.; Karlsen, A.P.H. Minimal clinically important differences in randomised clinical trials on pain management after total hip and knee arthroplasty: A systematic review. Br. J. Anaesth. 2021, 126, 1029–1037. [Google Scholar] [CrossRef]
- Marty, P.; Chassery, C.; Rontes, O.; Vuillaume, C.; Basset, B.; Merouani, M.; Marquis, C.; De Lussy, A.; Ferré, F.; Naudin, C. Combined proximal or distal nerve blocks for postoperative analgesia after total knee arthroplasty: A randomised controlled trial. Br. J. Anaesth. 2022, 129, 427–434. [Google Scholar] [CrossRef]
- Sousa, I.P.; da Silva Peixoto, C.L.; Coimbra, L.F.; da Costa Rodrigues, F. Comparison of pericapsular nerve group (PENG) block and epidural analgesia following total hip arthroplasty: A retrospective analysis. Rev. Española Anestesiol. Y Reanim. 2022, 69, 632–639. [Google Scholar] [CrossRef]
- Angers, M.; Belzile, É.L.; Vachon, J.; Beauchamp-Chalifour, P.; Pelet, S. Negative influence of femoral nerve block on quadriceps strength recovery following total knee replacement: A prospective randomized trial. Orthop. Traumatol. Surg. Res. 2019, 105, 633–637. [Google Scholar] [CrossRef]
- Memtsoudis, S.G.; Cozowicz, C.; Bekeris, J.; Bekere, D.; Liu, J.; Soffin, E.M.; Mariano, E.R.; Johnson, R.L.; Go, G.; Hargett, M.J. Peripheral nerve block anesthesia/analgesia for patients undergoing primary hip and knee arthroplasty: Recommendations from the International Consensus on Anesthesia-Related Outcomes after Surgery (ICAROS) group based on a systematic review and meta-analysis of current literature. Reg. Anesth. Pain Med. 2021, 46, 971–985. [Google Scholar]
- Girón-Arango, L.; Peng, P.W.; Chin, K.J.; Brull, R.; Perlas, A. Pericapsular nerve group (PENG) block for hip fracture. Reg. Anesth. Pain Med. 2018, 43, 859–863. [Google Scholar] [CrossRef] [PubMed]
- Aliste, J.; Layera, S.; Bravo, D.; Jara, Á.; Muñoz, G.; Barrientos, C.; Wulf, R.; Brañez, J.; Finlayson, R.J.; Tran, D.Q. Randomized comparison between pericapsular nerve group (PENG) block and suprainguinal fascia iliaca block for total hip arthroplasty. Reg. Anesth. Pain Med. 2021, 46, 874–878. [Google Scholar] [CrossRef] [PubMed]
- Allard, C.; Pardo, E.; de la Jonquière, C.; Wyniecki, A.; Soulier, A.; Faddoul, A.; Tsai, E.S.; Bonnet, F.; Verdonk, F. Comparison between femoral block and PENG block in femoral neck fractures: A cohort study. PLoS ONE 2021, 16, e0252716. [Google Scholar] [CrossRef]
- Hua, H.; Xu, Y.; Jiang, M.; Dai, X. Evaluation of pericapsular nerve group (PENG) block for analgesic effect in elderly patients with femoral neck fracture undergoing hip arthroplasty. J. Healthc. Eng. 2022, 2022, 7452716. [Google Scholar] [CrossRef]
- Pascarella, G.; Costa, F.; Del Buono, R.; Pulitanò, R.; Strumia, A.; Piliego, C.; De Quattro, E.; Cataldo, R.; Agrò, F.; Carassiti, M. Impact of the pericapsular nerve group (PENG) block on postoperative analgesia and functional recovery following total hip arthroplasty: A randomised, observer-masked, controlled trial. Anaesthesia 2021, 76, 1492–1498. [Google Scholar] [CrossRef] [PubMed]
- Bilal, B.; Öksüz, G.; Boran, Ö.F.; Topak, D.; Doğar, F. High volume pericapsular nerve group (PENG) block for acetabular fracture surgery: A new horizon for novel block. J. Clin. Anesth. 2020, 62, 109702. [Google Scholar] [CrossRef] [PubMed]
- Lin, D.-Y.; Morrison, C.; Brown, B.; Saies, A.A.; Pawar, R.; Vermeulen, M.; Anderson, S.R.; Lee, T.S.; Doornberg, J.; Kroon, H.M. Pericapsular nerve group (PENG) block provides improved short-term analgesia compared with the femoral nerve block in hip fracture surgery: A single-center double-blinded randomized comparative trial. Reg. Anesth. Pain Med. 2021, 46, 398–403. [Google Scholar] [CrossRef]
- Peng, P.W.; Perlas, A.; Chin, K.J. Reply to Dr Nielsen: Pericapsular nerve group (PENG) block for hip fracture. Reg. Anesth. Pain Med. 2019, 44, 415–416. [Google Scholar] [CrossRef]
- Tran, J.; Agur, A.; Peng, P. Is pericapsular nerve group (PENG) block a true pericapsular block? Reg. Anesth. Pain Med. 2019, 44, 257. [Google Scholar] [CrossRef]
- Thallaj, A. Combined PENG and LFCN blocks for postoperative analgesia in hip surgery—A case report. Saudi J. Anaesth. 2019, 13, 381. [Google Scholar]
- Pagano, T.; Scarpato, F.; Chicone, G.; Carbone, D.; Bussemi, C.B.; Albano, F.; Ruotolo, F. Analgesic evaluation of ultrasound-guided Pericapsular Nerve Group (PENG) block for emergency hip surgery in fragile patients: A case series. Arthroplasty 2019, 1, 18. [Google Scholar] [CrossRef]
- Kukreja, P.; Schuster, B.; Northern, T.; Sipe, S.; Naranje, S.; Kalagara, H. Pericapsular nerve group (PENG) block in combination with the quadratus lumborum block analgesia for revision total hip arthroplasty: A retrospective case series. Cureus 2020, 12, e12233. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Ahmed, W. Continuous pericapsular nerve group block for hip surgery: A case series. A&A Pract. 2020, 14, e01320. [Google Scholar]
- Zheng, J.; Pan, D.; Zheng, B.; Ruan, X. Preoperative pericapsular nerve group (PENG) block for total hip arthroplasty: A randomized, placebo-controlled trial. Reg. Anesth. Pain Med. 2022, 47, 155–160. [Google Scholar] [PubMed]
- Et, T.; Korkusuz, M. Comparison of pericapsular nerve group (peng) block with intra-articular and quadratus lumborum block in primary total hip arthroplasty: A randomized controlled trial. Korean J. Anesthesiol. 2023. ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.S.; Park, K.K.; Lee, B.; Nam, W.S.; Kim, D.-H. Pericapsular Nerve Group (PENG) block versus supra-inguinal fascia iliaca compartment block for total hip arthroplasty: A randomized clinical trial. J. Pers. Med. 2022, 12, 408. [Google Scholar] [CrossRef]
- Senthil, K.; Kumar, P.; Ramakrishnan, L. Comparison of pericapsular nerve group block versus fascia iliaca compartment block as postoperative pain management in hip fracture surgeries. Anesth. Essays Res. 2021, 15, 352. [Google Scholar]
- Yu, H.C.; Moser, J.J.; Chu, A.Y.; Montgomery, S.H.; Brown, N.; Endersby, R.V.W. Inadvertent quadriceps weakness following the pericapsular nerve group (PENG) block. Reg. Anesth. Pain Med. 2019. [Google Scholar] [CrossRef]
- Pascarella, G.; Costa, F.; Del Buono, R.; Strumia, A.; Cataldo, R.; Felice, E.A.; Carassiti, M. Defining the optimal spread of local anesthetic during pericapsular nerve group (PENG) block may help to avoid short-term motor block (reply to Aliste et al.). Reg. Anesth. Pain Med. 2022, 47, 200–201. [Google Scholar] [CrossRef]
- Çiftçi, B.; Ahıskalıoğlu, A.; Altıntaş, H.M.; Tekin, B.; Şakul, B.U.; Alıcı, H.A. A possible mechanism of motor blockade of high volume pericapsular nerve group (PENG) block: A cadaveric study. J. Clin. Anesth. 2021, 74, 110407. [Google Scholar] [CrossRef]
- Yeoh, S.-R.; Chou, Y.; Chan, S.-M.; Hou, J.-D.; Lin, J.-A. Pericapsular nerve group block and iliopsoas plane block: A scoping review of quadriceps weakness after two proclaimed motor-sparing Hip blocks. Healthcare 2022, 10, 1565. [Google Scholar]
- Hu, J.; Wang, Q.; Hu, J.; Kang, P.; Yang, J. Efficacy of ultrasound-guided pericapsular nerve group (PENG) block combined with local infiltration analgesia on postoperative pain after total hip arthroplasty: A prospective, double-blind, randomized controlled trial. J. Arthroplast. 2023, 38, 1096–1103. [Google Scholar] [CrossRef]
- Bravo, D.; Aliste, J.; Layera, S.; Fernández, D.; Erpel, H.; Aguilera, G.; Arancibia, H.; Barrientos, C.; Wulf, R.; León, S. Randomized clinical trial comparing pericapsular nerve group (PENG) block and periarticular local anesthetic infiltration for total hip arthroplasty. Reg. Anesth. Pain Med. 2023. [Google Scholar] [CrossRef] [PubMed]
- Nobre, L.V.; Cunha, G.P.; Sousa, P.C.C.B.D.; Takeda, A.; Ferraro, L.H.C. Peripheral nerve block and rebound pain: Literature review. Rev. Bras. Anestesiol. 2020, 69, 587–593. [Google Scholar] [CrossRef] [PubMed]
- Dada, O.; Gonzalez Zacarias, A.; Ongaigui, C.; Echeverria-Villalobos, M.; Kushelev, M.; Bergese, S.D.; Moran, K. Does rebound pain after peripheral nerve block for orthopedic surgery impact postoperative analgesia and opioid consumption? A narrative review. Int. J. Environ. Res. Public Health 2019, 16, 3257. [Google Scholar]
- Baeriswyl, M.; Kirkham, K.; Jacot-Guillarmod, A.; Albrecht, E. Efficacy of perineural vs systemic dexamethasone to prolong analgesia after peripheral nerve block: A systematic review and meta-analysis. BJA Br. J. Anaesth. 2017, 119, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Talawar, P.; Tandon, S.; Tripathy, D.; Kaushal, A. Combined pericapsular nerve group and lateral femoral cutaneous nerve blocks for surgical anaesthesia in hip arthroscopy. Indian J. Anaesth. 2020, 64, 638. [Google Scholar] [CrossRef]


| Sham Block Group n = 237 | Pericapsular Nerve Group (PENG) Block Group n = 239 | p Value | |
|---|---|---|---|
| ASA | 2 (SD = 0.5) | 2 (SD = 0.5) | 0.8508 |
| Age (years) | 66 (SD = 5.1) | 66 (SD = 5.8) | 0.1001 |
| Sex (F/M) | 115/122 | 99/140 | 0.1429 |
| BMI (kg/m2) | 31 (SD = 2.9) | 31 (SD = 3.2) | 0.2108 |
| NRS at rest—before surgery | 4.1 (SD = 1.3) | 4.3 (SD = 1.1) | 0.2741 |
| Spinal anesthesia needle level (L2/3 vs. L3/4) | 31 (13%) vs. 206 (87%) | 34 (14%) vs. 205 (86%) | 0.7898 |
| Surgery duration (min) | 63 (SD = 7.6) | 61 (SD = 8.3) | 0.3211 |
| Sham Block Group n = 237 | Pericapsular Nerve Group (PENG) Block Group n = 239 | p Value | |
|---|---|---|---|
| NRS postoperative | |||
| 24 h | 5.3 (SD = 1.0) | 3.1 (SD = 1.0) | <0.0001 |
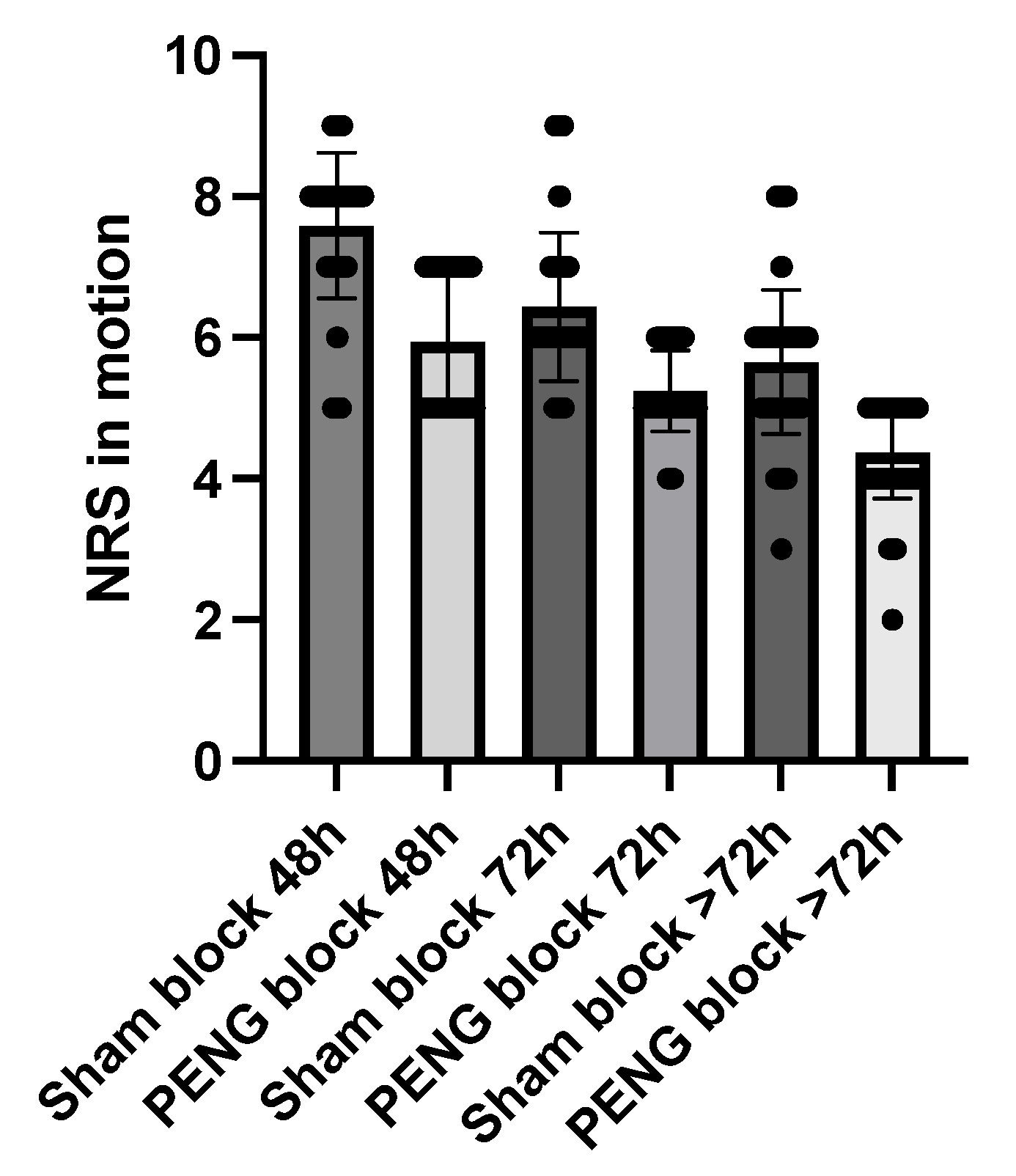
| NRS in motion | |||
| 48 h | 7.6 (SD = 1.0) | 5.9 (SD = 1.0) | <0.0001 |
| 72 h | 6.4 (SD = 1.1) | 5.2 (SD = 0.6) | <0.0001 |
| >72 h | 5.7 (SD = 1.0) | 4.4 (SD = 0.6) | <0.0001 |
| NRS at rest | |||
| 48 h | 3.7 (SD = 0.7) | 2.8 (SD = 0.8) | <0.0001 |
| 72 h | 2.8 (SD = 0.6) | 2.5 (SD = 0.8) | <0.0001 |
| >72 h | 0.4 (SD = 0.8) | 0 | 0.0004 |
| Postoperative opioid consumption | |||
| yes | 237 (100%) | 182 (76%) | <0.0001 |
| no | 0 (0%) | 57 (24%) | |
| Time to first opioid | |||
| hours | 4.5 (SD = 1.6) | 9.5 (SD = 5.5) | <0.0001 |
| Total opioid consumption(Intravenous morphine equivalents; mg) | |||
| 0–24 h | 8.4 (SD = 3.7) | 2.3 (SD = 1.6) | <0.0001 |
| 24–48 h | 2.5 (SD = 2.0) | 0.5 (SD = 1.1) | <0.0001 |
| 48–72 h | 0.3 (SD = 0.7) | 0 | <0.0001 |
| Functional recovery | |||
| Active elevation of operated limb | 25 (11%) | 127 (53%) | <0.0001 |
| Walking by the balcony | 108 (46%) | 239 (100%) | <0.0001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Domagalska, M.; Ciftci, B.; Reysner, T.; Kolasiński, J.; Wieczorowska-Tobis, K.; Kowalski, G. Pain Management and Functional Recovery after Pericapsular Nerve Group (PENG) Block for Total Hip Arthroplasty: A Prospective, Randomized, Double-Blinded Clinical Trial. J. Clin. Med. 2023, 12, 4931. https://doi.org/10.3390/jcm12154931
Domagalska M, Ciftci B, Reysner T, Kolasiński J, Wieczorowska-Tobis K, Kowalski G. Pain Management and Functional Recovery after Pericapsular Nerve Group (PENG) Block for Total Hip Arthroplasty: A Prospective, Randomized, Double-Blinded Clinical Trial. Journal of Clinical Medicine. 2023; 12(15):4931. https://doi.org/10.3390/jcm12154931
Chicago/Turabian StyleDomagalska, Małgorzata, Bahadir Ciftci, Tomasz Reysner, Jerzy Kolasiński, Katarzyna Wieczorowska-Tobis, and Grzegorz Kowalski. 2023. "Pain Management and Functional Recovery after Pericapsular Nerve Group (PENG) Block for Total Hip Arthroplasty: A Prospective, Randomized, Double-Blinded Clinical Trial" Journal of Clinical Medicine 12, no. 15: 4931. https://doi.org/10.3390/jcm12154931
APA StyleDomagalska, M., Ciftci, B., Reysner, T., Kolasiński, J., Wieczorowska-Tobis, K., & Kowalski, G. (2023). Pain Management and Functional Recovery after Pericapsular Nerve Group (PENG) Block for Total Hip Arthroplasty: A Prospective, Randomized, Double-Blinded Clinical Trial. Journal of Clinical Medicine, 12(15), 4931. https://doi.org/10.3390/jcm12154931





