Robotic Total Mesorectal Excision for Low Rectal Cancer: A Narrative Review and Description of the Technique
Abstract
1. Introduction
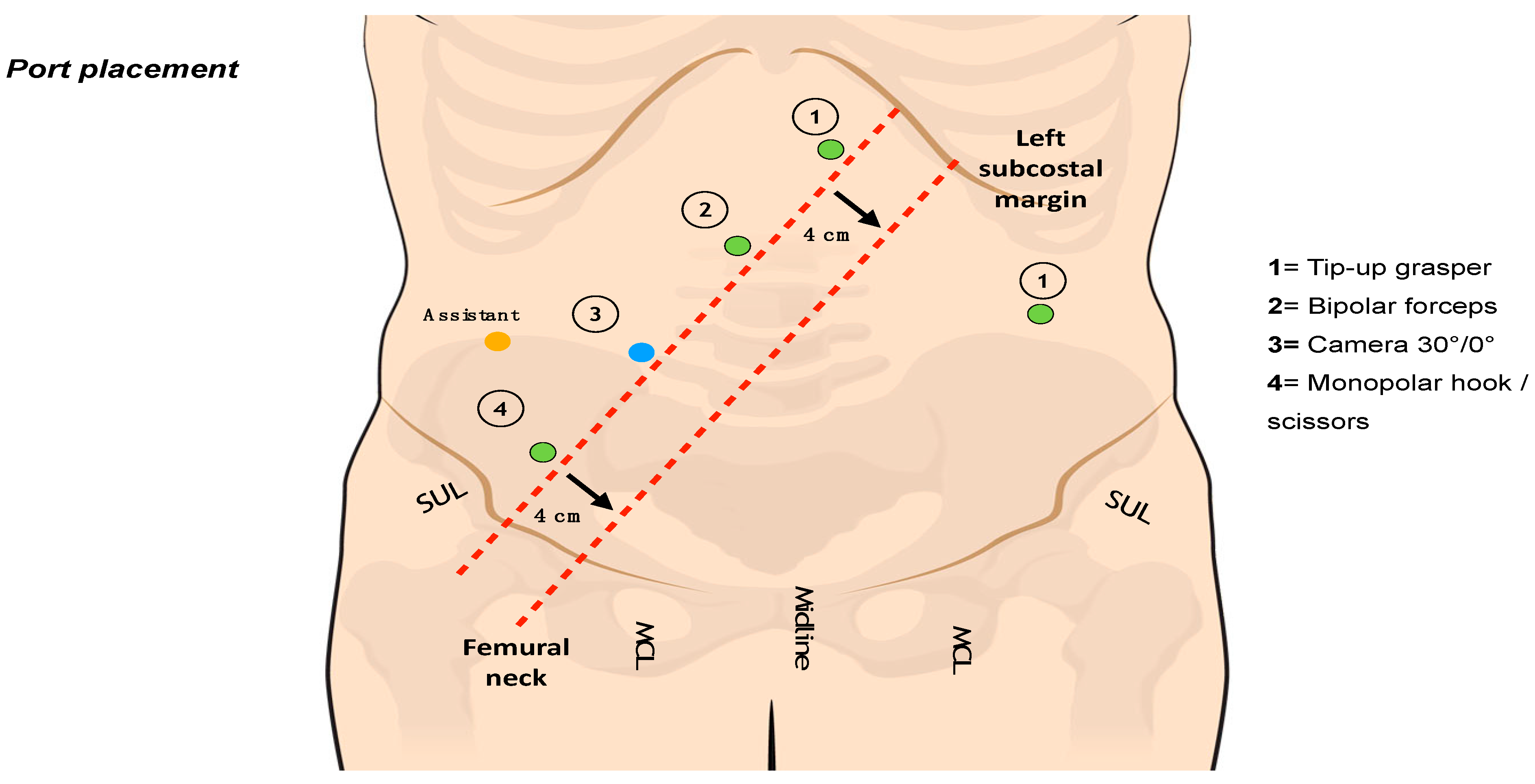
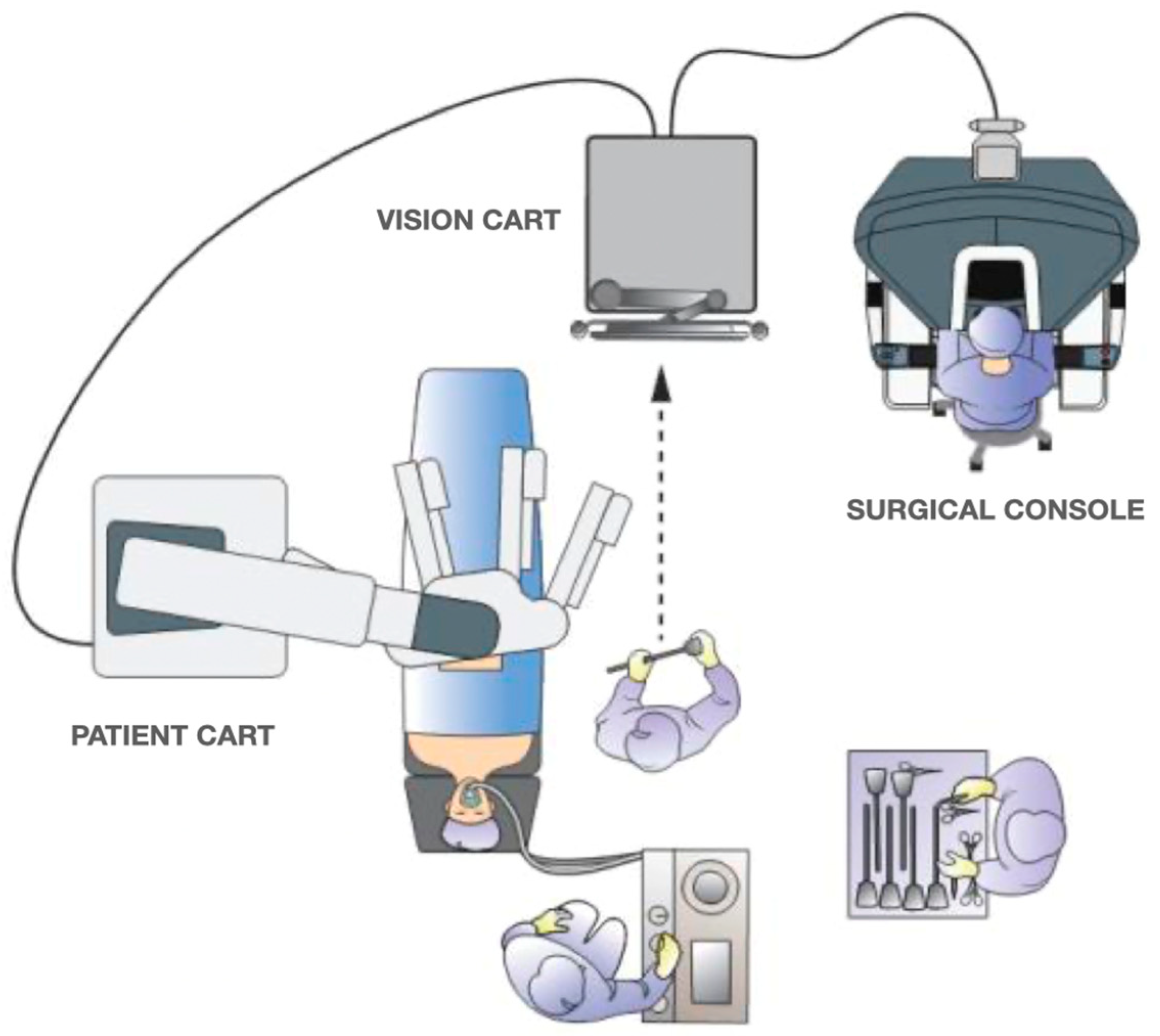
2. Surgical Technique
3. Laparoscopic versus Open Surgery: Long-Term Oncological Outcomes
4. Robotic versus Laparoscopic Surgery: Short-Term Outcomes and Pathological Outcomes
5. Robotic Surgery: Long-Term Oncological Outcomes
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Heald, R.J.; Ryall, R. Recurrent cancer after restorative resection of the rectum. Br. Med. J. (Clin. Res. Ed.) 1982, 284, 826–827. [Google Scholar] [CrossRef] [PubMed]
- Heald, R.J.; Moran, B.J.; Ryall, R.D.; Sexton, R.; MacFarlane, J.K. Rectal cancer: The Basingstoke experience of total mesorectal excision, 1978–1997. Arch. Surg. 1998, 133, 894–899. [Google Scholar] [CrossRef] [PubMed]
- Birbeck, K.F.; Macklin, C.P.; Tiffin, N.J.; Parsons, W.; Dixon, M.F.; Mapstone, N.P.; Abbott, C.R.; Scott, N.; Finan, P.J.; Johnston, D.; et al. Rates of circumferential resection margin involvement vary between surgeons and predict outcomes in rectal cancer surgery. Ann. Surg. 2002, 235, 449–457. [Google Scholar] [CrossRef] [PubMed]
- Green, B.L.; Marshall, H.C.; Collinson, F.; Quirke, P.; Guillou, P.; Jayne, D.G.; Brown, J.M. Long-term follow-up of the Medical Research Council CLASICC trial of conventional versus laparoscopically assisted resection in colorectal cancer. Br. J. Surg. 2013, 100, 75–82. [Google Scholar] [CrossRef] [PubMed]
- van der Pas, M.H.; Haglind, E.; Cuesta, M.A.; Fürst, A.; Lacy, A.M.; Hop, W.C.; Bonjer, H.J. COlorectal cancer Laparoscopic or Open Resection II (COLOR II) Study Group. Laparoscopic versus open surgery for rectal cancer (COLOR II): Short-term outcomes of a randomised, phase 3 trial. Lancet Oncol. 2013, 14, 210–218. [Google Scholar] [CrossRef]
- Park, J.W.; Kang, S.B.; Hao, J.; Lim, S.B.; Choi, H.S.; Kim, D.W.; Chang, H.J.; Kim, D.Y.; Jung, K.H.; Kim, T.Y.; et al. Open versus laparoscopic surgery for mid or low rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): 10-year follow-up of an open-label, non-inferiority, randomised controlled trial. Lancet Gastroenterol. Hepatol. 2021, 6, 569–577, Erratum in Lancet Gastroenterol. Hepatol. 2022, 7, e7. [Google Scholar] [CrossRef]
- Reibetanz, J.; Germer, C.T. Laparoskopische vs. offene Rektumkarzinomchirurgie: 3-Jahres-Ergebnisse der COLOR-II-Studie [Laparoscopic versus open surgery for rectal cancer: Results after 3 years of the COLOR II study]. Der Chir. 2015, 86, 802. [Google Scholar] [CrossRef]
- Stevenson, A.R.; Solomon, M.J.; Lumley, J.W.; Hewett, P.; Clouston, A.D.; Gebski, V.J.; Davies, L.; Wilson, K.; Hague, W.; Simes, J. ALaCaRT Investigators. Effect of Laparoscopic-Assisted Resection vs. Open Resection on Pathological Outcomes in Rectal Cancer: The ALaCaRT Randomized Clinical Trial. JAMA 2015, 314, 1356–1363. [Google Scholar] [CrossRef]
- Fleshman, J.; Branda, M.; Sargent, D.J.; Boller, A.M.; George, V.; Abbas, M.; Peters, W.R., Jr.; Maun, D.; Chang, G.; Herline, A.; et al. Effect of Laparoscopic-Assisted Resection vs. Open Resection of Stage II or III Rectal Cancer on Pathologic Outcomes: The ACOSOG Z6051 Randomized Clinical Trial. JAMA 2015, 314, 1346–1355. [Google Scholar] [CrossRef]
- Baek, S.J.; Kim, C.H.; Cho, M.S.; Bae, S.U.; Hur, H.; Min, B.S.; Baik, S.H.; Lee, K.Y.; Kim, N.K. Robotic surgery for rectal cancer can overcome difficulties associated with pelvic anatomy. Surg. Endosc. 2015, 29, 1419–1424. [Google Scholar] [CrossRef]
- Merola, G.; Sciuto, A.; Pirozzi, F.; Andreuccetti, J.; Pignata, G.; Corcione, F.; Milone, M.; De Palma, G.D.; Castaldo, R.; Pecchia, L.; et al. Is robotic right colectomy economically sustainable? A multicentre retrospective comparative study and cost analysis. Surg. Endosc. 2020, 34, 4041–4047. [Google Scholar] [CrossRef]
- Jayne, D.; Pigazzi, A.; Marshall, H.; Croft, J.; Corrigan, N.; Copeland, J.; Quirke, P.; West, N.; Rautio, T.; Thomassen, N.; et al. Effect of Robotic-Assisted vs. Conventional Laparoscopic Surgery on Risk of Conversion to Open Laparotomy Among Patients Undergoing Resection for Rectal Cancer: The ROLARR Randomized Clinical Trial. JAMA 2017, 318, 1569–1580. [Google Scholar] [CrossRef]
- Feng, Q.; Yuan, W.; Li, T.; Tang, B.; Jia, B.; Zhou, Y.; Zhang, W.; Zhao, R.; Zhang, C.; Cheng, L.; et al. REAL Study Group. Robotic versus laparoscopic surgery for middle and low rectal cancer (REAL): Short-term outcomes of a multicentre randomised controlled trial. Lancet Gastroenterol. Hepatol. 2022, 7, 991–1004. [Google Scholar] [CrossRef]
- Branda, M.E.; Sargent, D.J.; Boller, A.M.; George, V.V.; Abbas, M.A.; Peters, W.R., Jr.; Maun, D.C.; Chang, G.J.; Herline, A.; Fichera, A.; et al. Disease-free survival and local recurrence for laparo- scopic resection compared with open resection of stage II to III rectal cancer: Follow-up results of the ACOSOG Z6051 randomized controlled trial. Ann. Surg. 2019, 269, 589–595. [Google Scholar]
- Stevenson, A.R.L.; Solomon, M.J.; Brown, C.S.B.; Lumley, J.W.; Hewett, P.; Clouston, A.D.; Gebski, V.J.; Wilson, K.; Hague, W.; Simes, J. Disease-free survival and local recurrence after laparoscopic-assisted resection or open resection for rectal cancer: The Australasian laparoscopic cancer of the rectum randomized clinical trial. Ann. Surg. 2019, 269, 596–602. [Google Scholar] [CrossRef]
- Schnitzbauer, V.; Gerken, M.; Benz, S.; Völkel, V.; Draeger, T.; Fürst, A.; Klinkhammer-Schalke, M. Laparoscopic and open surgery in rectal cancer patients in Germany: Short and long-term results of a large 10-year population-based cohort. Surg. Endosc. 2020, 34, 1132–1141, Erratum in Surg. Endosc. 2020, 34, 1142. [Google Scholar] [CrossRef]
- Manchon-Walsh, P.; Aliste, L.; Biondo, S.; Espin, E.; Pera, M.; Targarona, E.; Pallarès, N.; Vernet, R.; Espinàs, J.A.; Guarga, A.; et al. A propensity-score-matched analysis of laparoscopic vs. open surgery for rectal cancer in a population-based study. Color. Dis. 2019, 21, 441–450. [Google Scholar] [CrossRef]
- Dehlaghi Jadid, K.; Cao, Y.; Petersson, J.; Angenete, E.; Matthiessen, P. Long term oncological outcomes for laparoscopic versus open surgery for rectal cancer—A population-based nationwide noninferiority study. Color. Dis. 2022, 24, 1308–1317. [Google Scholar] [CrossRef]
- Lee, G.C.; Bordeianou, L.G.; Francone, T.D.; Blaszkowsky, L.S.; Goldstone, R.N.; Ricciardi, R.; Kunitake, H.; Qadan, M. Superior pathologic and clinical outcomes after minimally invasive rectal cancer resection, compared to open resection. Surg. Endosc. 2020, 34, 3435–3448. [Google Scholar] [CrossRef]
- Villano, A.M.; Zeymo, A.; Houlihan, B.K.; Bayasi, M.; Al-Refaie, W.B.; Chan, K.S. Minimally Invasive Surgery for Colorectal Cancer: Hospital Type Drives Utilization and Outcomes. J. Surg. Res. 2020, 247, 180–189. [Google Scholar] [CrossRef]
- Myrseth, E.; Nymo, L.S.; Gjessing, P.F.; Kørner, H.; Kvaløy, J.T.; Norderval, S. Lower conversion rate with robotic assisted rectal resections compared with conventional laparoscopy; a national cohort study. Surg. Endosc. 2022, 236, 3574–3584. [Google Scholar] [CrossRef] [PubMed]
- Safiejko, K.; Tarkowski, R.; Koselak, M.; Juchimiuk, M.; Tarasik, A.; Pruc, M.; Smereka, J.; Szarpak, L. Robotic-Assisted vs. Standard Laparoscopic Surgery for Rectal Cancer Resection: A Systematic Review and Meta-Analysis of 19,731 Patients. Cancers 2021, 14, 180. [Google Scholar] [CrossRef] [PubMed]
- Phan, K.; Kahlaee, H.R.; Kim, S.H.; Toh, J.W.T. Laparoscopic vs. robotic rectal cancer surgery and the effect on conversion rates: A meta-analysis of randomized controlled trials and propensity-score-matched studies. Tech. Coloproctol. 2019, 23, 221–230. [Google Scholar] [CrossRef] [PubMed]
- Prete, F.P.; Pezzolla, A.; Prete, F.; Testini, M.; Marzaioli, R.; Patriti, A.; Jimenez-Rodriguez, R.M.; Gurrado, A.; Strippoli, G.F.M. Robotic Versus Laparoscopic Minimally Invasive Surgery for Rectal Cancer: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Ann. Surg. 2018, 267, 1034–1046. [Google Scholar] [CrossRef] [PubMed]
- Tang, B.; Lei, X.; Ai, J.; Huang, Z.; Shi, J.; Li, T. Comparison of robotic and laparoscopic rectal cancer surgery: A meta-analysis of randomized controlled trials. World J. Surg. Oncol. 2021, 19, 38. [Google Scholar] [CrossRef]
- Wang, X.; Cao, G.; Mao, W.; Lao, W.; He, C. Robot-assisted versus laparoscopic surgery for rectal cancer: A systematic review and meta-analysis. J. Cancer Res. Ther. 2020, 16, 979–989. [Google Scholar] [CrossRef]
- Trastulli, S.; Farinella, E.; Cirocchi, R.; Cavaliere, D.; Avenia, N.; Sciannameo, F.; Gullà, N.; Noya, G.; Boselli, C. Robotic resection compared with laparoscopic rectal resection for cancer: Systematic review and meta-analysis of short-term outcome. Color. Dis. 2012, 14, e134–e156. [Google Scholar] [CrossRef]
- Han, C.; Yan, P.; Jing, W.; Li, M.; Du, B.; Si, M.; Yang, J.; Yang, K.; Cai, H.; Guo, T. Clinical, pathological, and oncologic outcomes of robotic-assisted versus laparoscopic proctectomy for rectal cancer: A meta-analysis of randomized controlled studies. Asian J. Surg. 2020, 43, 880–890. [Google Scholar] [CrossRef]
- Corrigan, N.; Marshall, H.; Croft, J.; Copeland, J.; Jayne, D.; Brown, J. Exploring and adjusting for potential learning effects in ROLARR: A randomised controlled trial comparing robotic-assisted vs. standard laparoscopic surgery for rectal cancer resection. Trials 2018, 19, 339. [Google Scholar] [CrossRef]
- Rouanet, P.; Bertrand, M.M.; Jarlier, M.; Mourregot, A.; Traore, D.; Taoum, C.; de Forges, H.; Colombo, P.E. Robotic Versus Laparoscopic Total Mesorectal Excision for Sphincter-Saving Surgery: Results of a Single-Center Series of 400 Consecutive Patients and Perspectives. Ann. Surg. Oncol. 2018, 25, 3572–3579. [Google Scholar] [CrossRef]
- Bhama, A.R.; Obias, V.; Welch, K.B.; Vandewarker, J.F.; Cleary, R.K. A comparison of laparoscopic and robotic colorectal surgery outcomes using the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database. Surg. Endosc. 2015, 30, 1576–1584. [Google Scholar] [CrossRef]
- Al-Mazrou, A.M.; Chiuzan, C.; Kiran, R.P. The robotic approach significantly reduces length of stay after colectomy: A propensity score-matched analysis. Int. J. Color. Dis. 2017, 32, 1415–1421. [Google Scholar] [CrossRef]
- Altieri, M.S.; Yang, J.; Telem, D.A.; Zhu, J.; Halbert, C.; Talamini, M.; Pryor, A.D. Robotic approaches may offer benefit in colorectal procedures, more controversial in other areas: A review of 168,248 cases. Surg. Endosc. 2015, 30, 925–933. [Google Scholar] [CrossRef]
- Simillis, C.; Lal, N.; Thoukididou, S.N.; Kontovounisios, C.; Smith, J.J.; Hompes, R.; Adamina, M.; Tekkis, P.P. Open Versus Laparoscopic Versus Robotic Versus Transanal Mesorectal Excision for Rectal Cancer: A Systematic Review and Network Meta-analysis. Ann. Surg. 2019, 270, 59–68. [Google Scholar] [CrossRef]
- Giuratrabocchetta, S.; Formisano, G.; Salaj, A.; Opocher, E.; Ferraro, L.; Toti, F.; Bianchi, P.P. Update on Robotic Total Mesorectal Excision for Rectal Cancer. J. Pers. Med. 2021, 11, 900. [Google Scholar] [CrossRef]
- Hellan, M.; Ouellette, J.; Lagares-Garcia, J.A.; Rauh, S.M.; Kennedy, H.L.; Nicholson, J.D.; Nesbitt, D.; Johnson, C.S.; Pigazzi, A. Robotic Rectal Cancer Resection: A Retrospective Multicenter Analysis. Ann. Surg. Oncol. 2015, 22, 2151–2158. [Google Scholar] [CrossRef]
- Hara, M.; Sng, K.; Yoo, B.E.; Shin, J.W.; Lee, D.W.; Kim, S.H. Robotic-assisted surgery for rectal adenocarcinoma: Short-term and midterm outcomes from 200 consecutive cases at a single institution. Dis. Colon. Rectum. 2014, 57, 570–577. [Google Scholar] [CrossRef]
- Pai, A.; Marecik, S.J.; Park, J.J.; Melich, G.; Sulo, S.; Prasad, L.M. Oncologic and Clinicopathologic Outcomes of Robot-Assisted Total Mesorectal Excision for Rectal Cancer. Dis. Colon Rectum 2015, 58, 659–667. [Google Scholar] [CrossRef]
- Kwak, J.M.; Kim, S.H.; Kim, J.; Son, D.N.; Baek, S.J.; Cho, J.S. Robotic vs. laparoscopic resection of rectal cancer: Short-term outcomes of a case-control study. Dis. Colon Rectum 2011, 54, 151–156. [Google Scholar] [CrossRef]
- Ahmed, J.; Nasir, M.; Flashman, K.; Khan, J.; Parvaiz, A. Totally robotic rectal resection: An experience of the first 100 consecutive cases. Int. J. Color. Dis. 2016, 31, 869–876. [Google Scholar] [CrossRef]
- Ali, S.; Taylor, B.M.; Schlachta, C.M. Evaluation of pilot experience with robotic-assisted proctectomy and coloanal anastomosis for rectal cancer. Can. J. Surg. 2015, 58, 188–192. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sammour, T.; Malakorn, S.; Bednarski, B.K.; Kaur, H.; Shin, U.S.; Messick, C.; You, Y.N.; Chang, G.J. Oncological outcomes after robotic proctectomy for rectal cancer: Analysis of a prospective database. Ann. Surg. 2018, 267, 521–526. [Google Scholar] [CrossRef] [PubMed]
- Spanheimer, P.M.; Armstrong, J.G.; Fu, S.; Liao, J.; Regenbogen, S.E.; Byrn, J.C. Robotic proctectomy for rectal cancer: Analysis of 71 patients from a single institution. Int. J. Med. Robot. 2017, 13, e1841. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, T.; Kinugasa, Y.; Shiomi, A.; Tomioka, H.; Kagawa, H.; Yamakawa, Y. Robotic-assisted vs. conventional laparoscopic surgery for rectal cancer: Short-term outcomes at a single center. Surg. Today 2016, 46, 957–962. [Google Scholar] [CrossRef] [PubMed]
- Rullier, A.; Gourgou-Bourgade, S.; Jarlier, M.; Bibeau, F.; Chassagne-Clément, C.; Hennequin, C.; Tisseau, L.; Leroux, A.; Ettore, F.; Peoc’h, M.; et al. Predictive factors of positive circumferential resection margin after radiochemotherapy for rectal cancer: The French randomised trial ACCORD12/0405 PRODIGE 2. Eur. J. Cancer 2013, 49, 82–89. [Google Scholar] [CrossRef]
- Milone, M.; Manigrasso, M.; Velotti, N.; Torino, S.; Vozza, A.; Sarnelli, G.; Aprea, G.; Maione, F.; Gennarelli, N.; Musella, M.; et al. Completeness of total mesorectum excision of laparoscopic versus robotic surgery: A review with a meta-analysis. Int. J. Color. Dis. 2019, 34, 983–991. [Google Scholar] [CrossRef]
- Hopkins, M.B.; Geiger, T.M.; Bethurum, A.J.; Ford, M.M.; Muldoon, R.L.; Beck, D.E.; Stewart, T.G.; Hawkins, A.T. Comparing pathologic outcomes for robotic versus laparoscopic Surgery in rectal cancer resection: A propensity adjusted analysis of 7616 patients. Surg Endosc. 2020, 34, 2613–2622. [Google Scholar] [CrossRef]
- Yamaoka, Y.; Shiomi, A.; Kagawa, H.; Hino, H.; Manabe, S.; Kato, S.; Hanaoka, M. Robotic surgery for clinical T4 rectal cancer: Short- and long-term outcomes. Surg. Endosc. 2022, 36, 91–99. [Google Scholar] [CrossRef]
- Chang, T.P.; Chok, A.Y.; Tan, D.; Rogers, A.; Rasheed, S.; Tekkis, P.; Kontovounisios, C. The Emerging Role of Robotics in Pelvic Exenteration Surgery for Locally Advanced Rectal Cancer: A Narrative Review. J. Clin. Med. 2021, 10, 1518. [Google Scholar] [CrossRef]
- Aliyev, V.; Piozzi, G.N.; Bulut, A.; Guven, K.; Bakir, B.; Saglam, S.; Goksel, S.; Asoglu, O. Robotic vs. laparoscopic intersphincteric resection for low rectal cancer: A case matched study reporting a median of 7-year long-term oncological and functional outcomes. Updates Surg. 2022, 74, 1851–1860. [Google Scholar] [CrossRef]
- Lim, D.R.; Bae, S.U.; Hur, H.; Min, B.S.; Baik, S.H.; Lee, K.Y.; Kim, N.K. Long-term oncological outcomes of robotic versus laparoscopic total mesorectal excision of mid-low rectal cancer following neoadjuvant chemoradiation therapy. Surg. Endosc. 2017, 31, 1728–1737. [Google Scholar] [CrossRef]
- Park, S.Y.; Lee, S.M.; Park, J.S.; Kim, H.J.; Choi, G.S. Robot Surgery Shows Similar Long-term Oncologic Outcomes as Laparoscopic Surgery for Mid/Lower Rectal Cancer but Is Beneficial to ypT3/4 After Preoperative Chemoradiation. Dis. Colon Rectum 2021, 64, 812–821. [Google Scholar] [CrossRef]
- Huang, C.W.; Wei, P.L.; Chen, C.C.; Kuo, L.J.; Wang, J.Y. Clinical Safety and Effectiveness of Robotic-Assisted Surgery in Patients with Rectal Cancer: Real-World Experience over 8 Years of Multiple Institutions with High-Volume Robotic-Assisted Surgery. Cancers 2022, 14, 4175. [Google Scholar] [CrossRef]
| R-OS | L-OS | O-OS | R-DFS | L-DFS | O-DFS | R-LRR | L-LRR | O-LRR | R-LRFS | L-LRFS | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| COLOR II [5,7] | / | 86.7% (3y) | 83.6% (3y) | / | 74.8% (3y) | 70.8% (3y) | / | 5% (3y) | 5% (3y) | / | / |
| COREAN [6] | / | 76.8% (10y) | 74.1% (10y) | / | 64.3% (10y) | 59.3% (10y) | / | 3.4% (10y) | 8.9% (10y) | / | / |
| ALACART [14] | / | 94% (2y) | 93% (2y) | / | 80% (2y) | 82% (2y) | / | 5.4% (2y) | 3.1% (2y) | / | / |
| ACOSOG [15] | / | / | / | / | 79.5% (2y) | 83.2% (2y) | / | 4.6% (2y) | 4.5% (2y) | / | / |
| Aliyev et al. [50] | 90.4% (3y)– 86.3% (5y)– 76.9% (7y) | 88.6% (3y)–80.4% (5y)–73.4% (7y) | / | 84% (3y)–81% (5y)–80% (7y) | 80% (3y)–75% (5y)– 70% (7y) | / | / | / | / | 96% (3y)–94% (5y)–90% (7y) | 96% (3y)–92% (5y)–88% (7y) |
| Huang et al. [53] | 91.1% (5y) | / | / | 86.3% (5y) | / | / | 3.0% | / | / | / | / |
| Park er al. [52] | 92.8% (5y) | / | / | 81.9% (5y) | / | / | 2.3% (5y) | 1.2% (5y) | / | / | / |
| Lim et al. [51] | 90% (5y) | 93.3% (5y) | / | 76.8% (5y) | 76% (5y) | / | 2.7% (5y) | 6.3% (5y) | / | / |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Formisano, G.; Ferraro, L.; Salaj, A.; Giuratrabocchetta, S.; Piccolo, G.; Di Raimondo, G.; Bianchi, P.P. Robotic Total Mesorectal Excision for Low Rectal Cancer: A Narrative Review and Description of the Technique. J. Clin. Med. 2023, 12, 4859. https://doi.org/10.3390/jcm12144859
Formisano G, Ferraro L, Salaj A, Giuratrabocchetta S, Piccolo G, Di Raimondo G, Bianchi PP. Robotic Total Mesorectal Excision for Low Rectal Cancer: A Narrative Review and Description of the Technique. Journal of Clinical Medicine. 2023; 12(14):4859. https://doi.org/10.3390/jcm12144859
Chicago/Turabian StyleFormisano, Giampaolo, Luca Ferraro, Adelona Salaj, Simona Giuratrabocchetta, Gaetano Piccolo, Giulia Di Raimondo, and Paolo Pietro Bianchi. 2023. "Robotic Total Mesorectal Excision for Low Rectal Cancer: A Narrative Review and Description of the Technique" Journal of Clinical Medicine 12, no. 14: 4859. https://doi.org/10.3390/jcm12144859
APA StyleFormisano, G., Ferraro, L., Salaj, A., Giuratrabocchetta, S., Piccolo, G., Di Raimondo, G., & Bianchi, P. P. (2023). Robotic Total Mesorectal Excision for Low Rectal Cancer: A Narrative Review and Description of the Technique. Journal of Clinical Medicine, 12(14), 4859. https://doi.org/10.3390/jcm12144859





