A Systematic Review of Telemedicine-Driven Pulmonary Rehabilitation after the Acute Phase of COVID-19
Abstract
1. Introduction
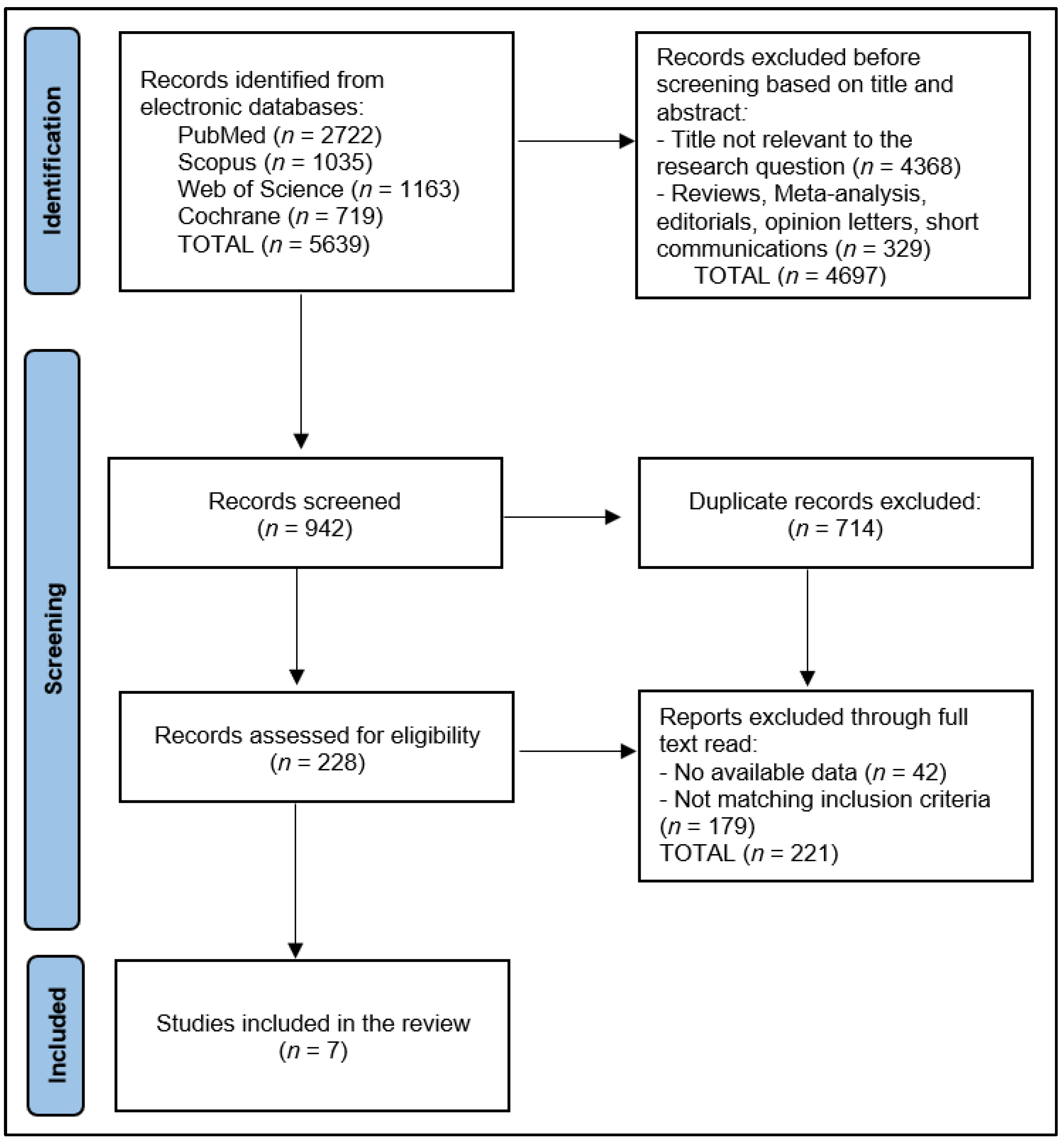
2. Materials and Methods
2.1. Protocol and Registration
2.2. Eligibility Criteria
2.3. Data Collection Process
2.4. Risk of Bias
3. Results
3.1. Study Characteristics
3.2. Rehabilitation Programs
3.3. Rehabilitation Measures and Outcomes
4. Discussion
4.1. Summary of Evidence
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Muralidar, S.; Ambi, S.V.; Sekaran, S.; Krishnan, U.M. The emergence of COVID-19 as a global pandemic: Understanding the epidemiology, immune response and potential therapeutic targets of SARS-CoV-2. Biochimie 2020, 179, 85–100. [Google Scholar] [CrossRef]
- Popescu, A.; Craina, M.; Pantea, S.; Pirvu, C.; Chiriac, V.D.; Marincu, I.; Bratosin, F.; Bogdan, I.; Hosin, S.; Citu, C.; et al. COVID-19 Pandemic Effects on Cervical Cancer Diagnosis and Management: A Population-Based Study in Romania. Diagnostics 2022, 12, 907. [Google Scholar] [CrossRef]
- Wang, F.; Kream, R.M.; Stefano, G.B. Long-Term Respiratory and Neurological Sequelae of COVID-19. Med. Sci. Monit. 2020, 26, e928996. [Google Scholar] [CrossRef]
- Citu, C.; Burlea, B.; Gorun, F.; Motoc, A.; Gorun, O.M.; Malita, D.; Ratiu, A.; Margan, R.; Grigoras, M.L.; Bratosin, F.; et al. Predictive Value of Blood Coagulation Parameters in Poor Outcomes in COVID-19 Patients: A Retrospective Observational Study in Romania. J. Clin. Med. 2022, 11, 2831. [Google Scholar] [CrossRef]
- Cerbu, B.; Grigoras, M.L.; Bratosin, F.; Bogdan, I.; Citu, C.; Bota, A.V.; Timircan, M.; Bratu, M.L.; Levai, M.C.; Marincu, I. Laboratory Profile of COVID-19 Patients with Hepatitis C-Related Liver Cirrhosis. J. Clin. Med. 2022, 11, 652. [Google Scholar] [CrossRef]
- Nalbandian, A.; Sehgal, K.; Gupta, A.; Madhavan, M.V.; McGroder, C.; Stevens, J.S.; Cook, J.R.; Nordvig, A.S.; Shalev, D.; Sehrawat, T.S.; et al. Post-acute COVID-19 syndrome. Nat. Med. 2021, 27, 601–615. [Google Scholar] [CrossRef] [PubMed]
- Bouteleux, B.; Henrot, P.; Ernst, R.; Grassion, L.; Raherison-Semjen, C.; Beaufils, F.; Zysman, M.; Delorme, M. Respiratory rehabilitation for Covid-19 related persistent dyspnoea: A one-year experience. Respir. Med. 2021, 189, 106648. [Google Scholar] [CrossRef] [PubMed]
- Fugazzaro, S.; Contri, A.; Esseroukh, O.; Kaleci, S.; Croci, S.; Massari, M.; Facciolongo, N.C.; Besutti, G.; Iori, M.; Salvarani, C.; et al. Reggio Emilia COVID-19 Working Group. Rehabilitation Interventions for Post-Acute COVID-19 Syndrome: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 5185. [Google Scholar] [CrossRef]
- Chen, H.; Shi, H.; Liu, X.; Sun, T.; Wu, J.; Liu, Z. Effect of Pulmonary Rehabilitation for Patients with Post-COVID-19: A Systematic Review and Meta-Analysis. Front. Med. 2022, 9, 837420. [Google Scholar] [CrossRef]
- Omboni, S.; Padwal, R.S.; Alessa, T.; Benczúr, B.; Green, B.B.; Hubbard, I.; Kario, K.; Khan, N.A.; Konradi, A.; Logan, A.G.; et al. The worldwide impact of telemedicine during COVID-19: Current evidence and recommendations for the future. Connect. Health 2022, 1, 7–35. [Google Scholar] [CrossRef] [PubMed]
- Kichloo, A.; Albosta, M.; Dettloff, K.; Wani, F.; El-Amir, Z.; Singh, J.; Aljadah, M.; Chakinala, R.C.; Kanugula, A.K.; Solanki, S.; et al. Telemedicine, the current COVID-19 pandemic and the future: A narrative review and perspectives moving forward in the USA. Fam. Med. Community Health 2020, 8, e000530. [Google Scholar] [CrossRef] [PubMed]
- Jaroń, K.; Jastrzębska, A.; Mąkosza, K.; Grajek, M.; Krupa-Kotara, K.; Kobza, J. Availability of Medical Services and Teleconsultation during COVID-19 Pandemic in the Opinion of Patients of Hematology Clinics—A Cross-Sectional Pilot Study (Silesia, Poland). Int. J. Environ. Res. Public Health 2023, 20, 4264. [Google Scholar] [CrossRef] [PubMed]
- Marotta, N.; Demeco, A.; Moggio, L.; Ammendolia, A. Why is telerehabilitation necessary? A pre-post COVID-19 comparative study of ICF activity and participation. J. Enabling Technol. 2021, 15, 117–121. [Google Scholar] [CrossRef]
- Cerdán-de-Las-Heras, J.; Balbino, F.; Løkke, A.; Catalán-Matamoros, D.; Hilberg, O.; Bendstrup, E. Effect of a New Tele-Rehabilitation Program versus Standard Rehabilitation in Patients with Chronic Obstructive Pulmonary Disease. J. Clin. Med. 2021, 11, 11. [Google Scholar] [CrossRef] [PubMed]
- Ora, J.; Prendi, E.; Attinà, M.L.; Cazzola, M.; Calzetta, L.; Rogliani, P. Efficacy of respiratory tele-rehabilitation in COPD patients: Systematic review and meta-analysis. Monaldi Arch. Chest Dis. Arch. Monaldi Mal. Torace 2022, 92. [Google Scholar] [CrossRef]
- Moher, D. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Schiavo, J.H. PROSPERO: An International Register of Systematic Review Protocols. Med. Ref. Serv. Q. 2019, 38, 171–180. [Google Scholar] [CrossRef]
- Foster, E.D.; Deardorff, A. Open Science Framework (OSF). J. Med. Libr. Assoc. 2017, 105, 203. [Google Scholar] [CrossRef]
- Institute of Medicine (US) Council on Health Care Technology. Medical Technology Assessment Directory: A Pilot Reference to Organizations, Assessments, and Information Resources; Goodman, C., Ed.; National Academies Press (US): Washington, DC, USA; National Heart, Lung, and Blood Institute: Bethesda, MA, USA, 1988. Available online: https://www.ncbi.nlm.nih.gov/books/NBK218529/ (accessed on 22 April 2023).
- Chambers, D.; Cantrell, A.; Johnson, M.; Preston, L.; Baxter, S.K.; Booth, A. Digital and Online Symptom Checkers and Assessment Services for Urgent Care to Inform a New Digital Platform: A Systematic Review; NIHR Journals Library: Southampton, UK, 2019; Health Services and Delivery Research, No. 7.29; Appendix 4, Quality Assessment Tools. Available online: https://www.ncbi.nlm.nih.gov/books/NBK545131/ (accessed on 22 April 2023).
- Dalbosco-Salas, M.; Torres-Castro, R.; Rojas Leyton, A.; Morales Zapata, F.; Henríquez Salazar, E.; Espinoza Bastías, G.; Beltrán Díaz, M.E.; Tapia Allers, K.; Mornhinweg Fonseca, D.; Vilaró, J. Effectiveness of a Primary Care Telerehabilitation Program for Post-COVID-19 Patients: A Feasibility Study. J. Clin. Med. 2021, 10, 4428. [Google Scholar] [CrossRef]
- Martin, I.; Braem, F.; Baudet, L.; Poncin, W.; Fizaine, S.; Aboubakar, F.; Froidure, A.; Pilette, C.; Liistro, G.; De Greef, J.; et al. Follow-up of functional exercise capacity in patients with COVID-19: It is improved by telerehabilitation. Respir. Med. 2021, 183, 106438. [Google Scholar] [CrossRef]
- Pehlivan, E.; Palalı, İ.; Atan, S.G.; Turan, D.; Çınarka, H.; Çetinkaya, E. The effectiveness of POST-DISCHARGE telerehabilitation practices in COVID-19 patients: Tele-COVID study-randomized controlled trial. Ann. Thorac. Med. 2022, 17, 110–117. [Google Scholar] [CrossRef]
- Hameed, F.; Palatulan, E.; Jaywant, A.; Said, R.; Lau, C.; Sood, V.; Layton, A.; Gellhorn, A. Outcomes of a COVID-19 recovery program for patients hospitalized with SARS-CoV-2 infection in New York City: A prospective cohort study. PM R 2021, 13, 609–617. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Xia, W.; Zhan, C.; Liu, S.; Yin, Z.; Wang, J.; Chong, Y.; Zheng, C.; Fang, X.; Cheng, W.; et al. A telerehabilitation programme in post-discharge COVID-19 patients (TERECO): A randomised controlled trial. Thorax 2022, 77, 697–706. [Google Scholar] [CrossRef]
- Capin, J.J.; Jolley, S.E.; Morrow, M.; Connors, M.; Hare, K.; MaWhinney, S.; Nordon-Craft, A.; Rauzi, M.; Flynn, S.; Stevens-Lapsley, J.E.; et al. Safety, feasibility and initial efficacy of an app-facilitated telerehabilitation (AFTER) programme for COVID-19 survivors: A pilot randomised study. BMJ Open 2022, 12, e061285. [Google Scholar] [CrossRef]
- Tanguay, P.; Marquis, N.; Gaboury, I.; Kairy, D.; Touchette, M.; Tousignant, M.; Décary, S. Telerehabilitation for Post-Hospitalized COVID-19 Patients: A Proof-of-Concept Study during a Pandemic. Int. J. Telerehabil. 2021, 13, e6383. [Google Scholar] [CrossRef]
- Büsching, G.; Zhang, Z.; Schmid, J.P.; Sigrist, T.; Khatami, R. Effectiveness of Pulmonary Rehabilitation in Severe and Critically Ill COVID-19 Patients: A Controlled Study. Int. J. Environ. Res. Public Health 2021, 18, 8956. [Google Scholar] [CrossRef] [PubMed]
- Hayden, M.C.; Limbach, M.; Schuler, M.; Merkl, S.; Schwarzl, G.; Jakab, K.; Nowak, D.; Schultz, K. Effectiveness of a Three-Week Inpatient Pulmonary Rehabilitation Program for Patients after COVID-19: A Prospective Observational Study. Int. J. Environ Res. Public Health 2021, 18, 9001. [Google Scholar] [CrossRef] [PubMed]
- Puchner, B.; Sahanic, S.; Kirchmair, R.; Pizzini, A.; Sonnweber, B.; Wöll, E.; Mühlbacher, A.; Garimorth, K.; Dareb, B.; Ehling, R.; et al. Beneficial effects of multi-disciplinary rehabilitation in postacute COVID-19: An observational cohort study. Eur. J. Phys. Rehabil. Med. 2021, 57, 189–198. [Google Scholar] [CrossRef]
- Spielmanns, M.; Pekacka-Egli, A.M.; Schoendorf, S.; Windisch, W.; Hermann, M. Effects of a Comprehensive Pulmonary Rehabilitation in Severe Post-COVID-19 Patients. Int. J. Environ. Res. Public Health 2021, 18, 2695. [Google Scholar] [CrossRef]
- Curci, C.; Negrini, F.; Ferrillo, M.; Bergonzi, R.; Bonacci, E.; Camozzi, D.M.; Ceravolo, C.; DEFranceschi, S.; Guarnieri, R.; Moro, P.; et al. Functional outcome after inpatient rehabilitation in postintensive care unit COVID-19 patients: Findings and clinical implications from a real-practice retrospective study. Eur. J. Phys. Rehabil. Med. 2021, 57, 443–450. [Google Scholar] [CrossRef]
- Zampogna, E.; Paneroni, M.; Belli, S.; Aliani, M.; Gandolfo, A.; Visca, D.; Bellanti, M.T.; Ambrosino, N.; Vitacca, M. Pulmonary Rehabilitation in Patients Recovering from COVID-19. Respiration 2021, 100, 416–422. [Google Scholar] [CrossRef] [PubMed]
- Official Recommendations of the American Thoracic Society and European Respiratory Society: Implementation, Use, and Dissemination of Respiratory Rehabilitation. Available online: https://www.ers-education.org/lrMedia/2015/pdf/393777.pdf (accessed on 22 April 2023).
- Gloeckl, R.; Leitl, D.; Jarosch, I.; Schneeberger, T.; Nell, C.; Stenzel, N.; Vogelmeier, C.F.; Kenn, K.; Koczulla, A.R. Benefits of pulmonary rehabilitation in COVID-19: A prospective observational cohort study. ERJ Open Res. 2021, 7, 00108–02021. [Google Scholar] [CrossRef] [PubMed]
- Hermann, M.; Pekacka-Egli, A.M.; Witassek, F.; Baumgaertner, R.; Schoendorf, S.; Spielmanns, M. Feasibility and Efficacy of Cardiopulmonary Rehabilitation After COVID-19. Am. J. Phys. Med. Rehabil. 2020, 99, 865–869. [Google Scholar] [CrossRef]
- Paneroni, M.; Vitacca, M.; Bernocchi, P.; Bertacchini, L.; Scalvini, S. Feasibility of tele-rehabilitation in survivors of COVID-19 pneumonia. Pulmonology 2021, 28, 152–154. [Google Scholar] [CrossRef] [PubMed]
- Nasserie, T.; Hittle, M.; Goodman, S.N. Assessment of the frequency and variety of persistent symptoms among patients with COVID-19: A systematic review. JAMA Netw. Open 2021, 4, e2111417. [Google Scholar] [CrossRef]
- Werneke, M.W.; Deutscher, D.; Grigsby, D.; Tucker, C.A.; Mioduski, J.E.; Hayes, D. Telerehabilitation during the COVID-19 Pandemic in Outpatient Rehabilitation Settings: A Descriptive Study. Phys. Ther. 2021, 101, pzab198. [Google Scholar] [CrossRef]
- Fioratti, I.; Fernandes, L.G.; Reis, F.J.; Saragiotto, B.T. Strategies for a safe and assertive telerehabilitation practice. Braz. J. Phys. Ther. 2021, 25, 113–116. [Google Scholar] [CrossRef]
- Houchen-Wolloff, L.; Steiner, M.C. Pulmonary rehabilitation at a time of social distancing: Prime time for tele-rehabilitation? Thorax 2020, 75, 446–447. [Google Scholar] [CrossRef]
- Rodriguez-Blanco, C.; Gonzalez-Gerez, J.J.; Bernal-Utrera, C.; Anarte-Lazo, E.; Perez-Ale, M.; Saavedra-Hernandez, M. Short-Term Effects of a Conditioning Telerehabilitation Program in Confined Patients Affected by COVID-19 in the Acute Phase. A Pilot Randomized Controlled Trial. Medicina 2021, 57, 684. [Google Scholar] [CrossRef]
- Barata, P.I.; Crisan, A.F.; Maritescu, A.; Negrean, R.A.; Rosca, O.; Bratosin, F.; Citu, C.; Oancea, C. Evaluating Virtual and Inpatient Pulmonary Rehabilitation Programs for Patients with COPD. J. Pers. Med. 2022, 12, 1764. [Google Scholar] [CrossRef]
- Hornsby, J.; Galbraith, F.; Brash, L.; Anderson, D. P104 Retrospective evaluation of ILD specific pulmonary rehabilitation program: Improvement in exercise capacity and quality of life scores. Thorax 2018, 73, A158–A159. [Google Scholar]

| Study and Author | Country | Study Year | Study Design | Study Quality |
|---|---|---|---|---|
| 1 Dalbosco-Salas et al. [21] | Chile | 2021 | Prospective Cohort | Good |
| 2 Martin et al. [22] | Belgium | 2021 | Prospective Cohort | Good |
| 3 Pehilvan et al. [23] | Turkey | 2022 | Randomized Trial | Good |
| 4 Hameed et al. [24] | USA | 2021 | Prospective Cohort | Good |
| 5 Li et al. [25] | China | 2022 | Randomized Trial | Excellent |
| 6 Capin et al. [26] | USA | 2022 | Randomized Trial | Excellent |
| 7 Tanguay et al. [27] | Canada | 2021 | Prospective Cohort | Good |
| Study Number | Number of Patients | Average Age (Years) | Gender (Men, %) | COVID-19 Severity | Length of Hospitalization |
|---|---|---|---|---|---|
| 1 Dalbosco-Salas et al. [21] | 115 (58 non-hospitalized vs. 57 hospitalized) | 52 vs. 59 | 43% (24% vs. 61%) | Severe—0.0% | 29.9 days |
| 2 Martin et al. [22] | 27 (14 telerehabilitation vs. 13 controls) | 61 vs. 62 | 62% (79% vs. 46%) | Severe—48.1% | 16.3 days vs. 16.1 days |
| 3 Pehilvan et al. [23] | 34 (17 telerehabilitation vs. 17 controls) | 51 vs. 43 | 74% (82% vs. 65%) | Severe—8.8% | NR |
| 4 Hameed et al. [24] | 69 (44 virtual rehabilitation vs. 25 in-person rehabilitation therapy) | 60 vs. 57 | 36% (57% vs. 24%) | Severe—31.8% | 14 days vs. 39 days |
| 5 Li et al. [25] | 119 (59 telerehabilitation vs. 60 controls) | 50 vs. 52 | 45% (46% vs. 43%) | Severe—31.9% | 28.6 days vs. 23.7 days |
| 6 Capin et al. [26] | 41 (28 virtual vs. 13 controls) | 52 vs. 54 | 54% (54% vs. 62%) | Severe—21.9% | 8 days vs. 5 days |
| 7 Tanguay et al. [27] | 7 (before vs. after rehabilitation) | 42 | 47% | Severe—0.0% | NR |
| Study Number | Program Exercises | Program Duration | Program Schedule | Rehabilitation Protocol Features |
|---|---|---|---|---|
| 1 Dalbosco-Salas et al. [21] | Aerobic, resistance training, and breathing exercise | 9 weeks | 3 sessions/week; duration: 40 min | Moderate- to high-intensity training. Resistance training was performed with elastic bands. |
| 2 Martin et al. [22] | Resistance training, muscle training | 6 weeks | 2 sessions/week; duration: 50 min | Fixed intensity of the endurance training on a 6-point intensity score. Muscle training was performed with materials available at home (2–3 series of 8–12 repetitions for each exercise). |
| 3 Pehilvan et al. [23] | Paced running/walking in the corridor, breathing exercises, active cycle of breathing technique, range of motion exercise, and standing squats. | 6 weeks | 3 sessions/week | 10 repetitions of each exercise or modified according to the level of fatigue. |
| 4 Hameed et al. [24] | Sit to stand, marching in place, shoulder scaption, standing heel raises, side stepping, wall pushups. | 4 weeks | 4 phases; duration: 30–60 min | Phase one required one workout cycle, four times a day, for seven days. Phase two required two workouts each day with a rest day on the fourth of seven days. Phase three required three workout cycles, twice daily for three days, followed by a day of rest and another three days. Phase four recommended community-level exercise. |
| 5 Li et al. [25] | Aerobic, resistance training, and breathing exercise. | 6 weeks | 4 sessions/week; duration: 40–60 min | Breathing control and thoracic expansion, aerobic exercises, lower-limb exercises (resistance training)—all exercises scheduled to increase in intensity. |
| 6 Capin et al. [26] | Aerobic, high-intensity training, breathing and clearance techniques, balance exercises, and functional activities. | 10 weeks | 12 sessions: 3/week in the first week, 2/week in weeks 2–4, 1/week in weeks 5–6, and 1 recall visit during weeks 9–10 | High-intensity strength training included breathing and compensating strategies. Balance, functional, and aerobic exercises were performed. Stretching ensured flexibility, while lifestyle counseling and motivational interviews kept participants engaged. Health in Motion enabled self-directed intervention outside of supervised sessions. Educational handouts were used to teach exercise, and weekly phone calls monitored progress and program adherence. |
| 7 Tanguay et al. [27] | Aerobic and resistance training | 8 weeks | 7 sessions/week; duration: 30 min | Aerobic training consisted of 15 min of intense cycling, steps, or walking. Resistance training followed, with 1–2 sets of 8–10 repetitions at 30%–80% of the repetition maximum. Balance training—walking with obstacles, changing direction, or stepping on unsteady surfaces—improved stability and coordination. |
| Study Number | Physical Health | Mental Health | QOL | Pulmonary Function |
|---|---|---|---|---|
| 1 Dalbosco-Salas et al. [21] | VAS fatigue score: 3 (0–5) non-hospitalized vs. 1 (0–3) hospitalized (p < 0.001) | SF-36 mental domain: 51.0 non-hospitalized vs. 63.7 hospitalized (p < 0.001) | SF-36 total score: 39.6 non-hospitalized vs. 58.9 hospitalized (p < 0.001) | mMRC dyspnea score: 2 (1–3) non-hospitalized vs. 1 (0–2) hospitalized (p < 0.001); STST: 18.9 vs. 29.2 (p < 0.001) |
| 2 Martin et al. [22] | NR | NR | NR | VAS dyspnea score: 5 (3–8) TR vs. 5 (1–10) controls (p = 0.966); STST change: 10 (5–19) TR vs. 5 (−4–11) controls (p = 0.004) |
| 3 Pehilvan et al. [23] | VAS pain score: 2.47 (0–8) TR vs. 1.76 (0–7) controls (p = 0.039) VAS fatigue score: 1.29 (0–3) TR vs. 1.47 (0–5) controls (p = 0.782) | BDI score: 3.2 TR vs. 4.1 controls (p = 0.623) | SGRQ total score: 31.5 TR vs. 16.9 controls (p = 0.033) | mMRC dyspnea score: 1 (0–2) TR vs. 0 (0–2) controls (p = 0.066) |
| 4 Hameed et al. [24] | Step test score: 73 ± 26 virtual vs. 71 ± 30 in-person (p < 0.001) | PHQ-4: 1 (4) virtual vs. 0 (1) in-person (p = 0.020) | NR | STST: 13 ± 3 virtual vs. 12 ± 1 in-person (p < 0.001) |
| 5 Li et al. [25] | 6MWD: 80.2 TR vs. 17.1 controls (p < 0.001) | SF-12 mental domain: 6.15 TR vs. 4.17 controls (p < 0.001) | SF-12 total score: 7.81 TR vs. 3.84 controls (p < 0.001) | MVV: 14.5 TR vs. 5.6 controls (p = 0.005); mMRC dyspnea: 90.4 TR vs. 61.7 controls (p < 0.001) |
| 6 Capin et al. [26] | 30 seconds chair stand: 11 (3) TR vs. 12 (3) controls (p = 0.730); TUG: 9 (3) TR vs. 10 (3) controls (p = 0.790) | 3-item LS: 4 (1) TR vs. 5 (2) controls (p = 0.510) | PHQ8 score: 6 (4) TR vs. 8 (6) controls (p = 0.370) | mMRC dyspnea score: 3 (1) TR vs. 3 (1) controls (p = 0.430) |
| 7 Tanguay et al. [27] | EQ-VAS: improvement between 10–45 points BPAQ: increase from low to moderate level | Anxiety/Depression: significant decrease | CAT score: increase by 30 points after 8 weeks | Borg dyspnea scale: average decrease by 4 points (from 7 to 3) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pescaru, C.C.; Crisan, A.F.; Marc, M.; Trusculescu, A.A.; Maritescu, A.; Pescaru, A.; Sumenkova, A.; Bratosin, F.; Oancea, C.; Vastag, E. A Systematic Review of Telemedicine-Driven Pulmonary Rehabilitation after the Acute Phase of COVID-19. J. Clin. Med. 2023, 12, 4854. https://doi.org/10.3390/jcm12144854
Pescaru CC, Crisan AF, Marc M, Trusculescu AA, Maritescu A, Pescaru A, Sumenkova A, Bratosin F, Oancea C, Vastag E. A Systematic Review of Telemedicine-Driven Pulmonary Rehabilitation after the Acute Phase of COVID-19. Journal of Clinical Medicine. 2023; 12(14):4854. https://doi.org/10.3390/jcm12144854
Chicago/Turabian StylePescaru, Camelia Corina, Alexandru Florian Crisan, Monica Marc, Ana Adriana Trusculescu, Adelina Maritescu, Andrei Pescaru, Anastasiia Sumenkova, Felix Bratosin, Cristian Oancea, and Emanuela Vastag. 2023. "A Systematic Review of Telemedicine-Driven Pulmonary Rehabilitation after the Acute Phase of COVID-19" Journal of Clinical Medicine 12, no. 14: 4854. https://doi.org/10.3390/jcm12144854
APA StylePescaru, C. C., Crisan, A. F., Marc, M., Trusculescu, A. A., Maritescu, A., Pescaru, A., Sumenkova, A., Bratosin, F., Oancea, C., & Vastag, E. (2023). A Systematic Review of Telemedicine-Driven Pulmonary Rehabilitation after the Acute Phase of COVID-19. Journal of Clinical Medicine, 12(14), 4854. https://doi.org/10.3390/jcm12144854






